Abstract
Background
Biomarkers that can accurately predict the efficacy of immune checkpoint inhibitors (ICIs) against programmed death 1 (PD-1) ligand in cancer immunotherapy are urgently needed. We have previously reported a novel formula that predicts the response to treatment with second-line nivolumab with high sensitivity and specificity in patients with non-small cell lung cancer (NSCLC) previously treated with chemotherapy. The formula was based on the percentages of CD62LlowCD4+ T cells (effector T cells; %Teff) and CD4+CD25+FOXP3+ T cells (regulatory T cells; %Treg) in the peripheral blood before treatment estimated using the peripheral blood mononuclear cell (PBMC) method. Here, we investigated the applicability of the formula (K-index) to predict the response to treatment with another ICI to expand its clinical applicability. Furthermore, we developed a simpler assay method based on whole blood (WB) samples to overcome the limitations of the PBMC method, such as technical difficulties, in obtaining the K-index.
Methods
The K-index was evaluated using the PBMC method in 59 patients with NSCLC who received first-line pembrolizumab treatment. We also assessed the K-index using the WB method and estimated the correlation between the measurements obtained using both methods in 76 patients with lung cancer.
Results
This formula consistently predicted the response to first-line pembrolizumab therapy in patients with NSCLC. The WB method correlated well with the PBMC method to obtain %Teff, %Treg, and the formula value. The WB method showed high repeatability (coefficient of variation, < 10%). The data obtained using WB samples collected in tubes containing either heparin or EDTA-2K and stored at room temperature (18–24 °C) for one day after blood sampling did not differ. Additionally, the performance of the WB method was consistent in different flow cytometry instruments.
Conclusions
The K-index successfully predicted the response to first-line therapy with pembrolizumab, as reported earlier for the second-line therapy with nivolumab in patients with NSCLC. The WB method established in this study can replace the cumbersome PBMC method in obtaining the K-index. Overall, this study suggests that the K-index can predict the response to anti-PD-1 therapy in various cancers, including NSCLC.
Similar content being viewed by others
Background
Immune checkpoint inhibitors (ICIs) targeting the anti-programmed death 1 (PD-1) ligand have shown epoch-making effects in several cancers, especially in terms of long-term survival [1,2,3,4,5,6,7,8]. However, a considerable number of patients do not achieve long-term antitumor efficacy because of the wide variations in their pre-existing antitumor immune status [1, 2, 4, 9,10,11,12,13]. Therefore, there is an urgent need to develop effective biomarkers that can accurately predict responses to anti-PD-1 therapies to ensure their appropriate clinical use [14].
In a previous study, we demonstrated that CD4+ T cell immunity in the peripheral blood before therapy predicted the antitumor efficacy of second-line nivolumab therapy in patients with non-small cell lung cancer (NSCLC). Furthermore, we developed a formula to predict non-responders to nivolumab based on the percentage of CD62LlowCD4+ and CD4+CD25+FOXP3+ T cells in CD4+ T cells of the peripheral blood, which demonstrated a sensitivity and specificity of 85.7 and 100%, respectively [15]. The formula value predicted long-term responders with progression-free survival (PFS) of > 500 days, referred to as the K-index in this study. The study indicated that the formula value could be potentially applied as a biomarker to predict response to anti-PD-1 therapies.
Owing to phase III clinical trials, such as Keynotes 024 and 042, the initial standard therapy for patients with advanced NSCLC with PD-L1 positive tumors has shifted from cytotoxic agents to PD-1 inhibitors [10, 16]. The long-term follow-up analysis of Keynote 024 showed that more than 30% of patients with advanced NSCLC with a PD-L1 tumor proportional score (TPS) ≥ 50% who received initial treatment with pembrolizumab achieved a 5-year survival. Therefore, in this study, we first investigated whether the K-index could predict the antitumor efficacy of first-line pembrolizumab therapy in patients with advanced NSCLC with a PD-L1 TPS of ≥50%.
To date, accurate analysis of T cell subset frequencies requires complicated experimental procedures of peripheral blood samples using flow cytometry (FCM) to obtain the K-index [15] Peripheral blood mononuclear cells (PBMCs) are separated from the blood samples over a Ficoll gradient, frozen at − 80 °C, and then transferred into a liquid nitrogen tank within a week for preservation. After thawing, the frozen cells are incubated in a culture medium for 32–48 h to restore molecular expression before FCM analysis. This method is known as the PBMC method. In our previous study, we applied this PBMC method to stably analyze specimens collected at various facilities and over different periods because the results were similar to those obtained at the time of collection. However, the PBMC method is not suitable for widespread clinical testing, such as in vitro diagnostics (IVD), because of the additional time required for culture and the complexity of rapid PBMC isolation and liquid nitrogen storage. Although it is crucial to maintain the initial expression of CD62L for IVD use, CD62L is rapidly lost by enzymatic degradation at the membrane-proximal site in T cells that are not isolated from PBMCs and stored as whole blood (WB) [17] Therefore, the present study also aimed to develop a method to obtain the K-index directly from WB without cumbersome procedures. Moreover, we analyzed the analytical performance of the WB method and compared it with that of the PBMC method. Our results revealed that the WB method correlated well with the PBMC method. This study confirms the wide applicability of the K-index in clinical laboratory settings.
Materials and methods
Clinical samples and determination of pembrolizumab therapy clinical efficacy
Fifty-nine consecutive patients with NSCLC who received fist-line pembrolizumab treatment between March 2017 and February 2019 at the Saitama Medical University International Medical Center (Saitama, Japan) were included in this study. This study was approved by ethical committee of Saitama Medical University International Medical Center. Written informed consent was obtained from all patients before sample collection, in accordance with the Declaration of Helsinki. One patient was excluded from all survival analyses because of a change in the pathological diagnosis after enrollment. Eight patients were excluded from the PFS analysis because the antitumor effect after pembrolizumab treatment could not be evaluated (Fig. 1a; Table 1). Informed consent was obtained from all participants prior to pembrolizumab treatment and blood samples were collected. K-index analysis was performed using the same procedure as previously reported [15]. Patients received a 200 mg dose of pembrolizumab every 3 weeks. Tumor response was assessed using the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1. The cutoff date for data collection was May 19, 2020. PD-L1 expression was assessed in formalin-fixed tumor samples at SRL Inc. (Tokyo, Japan) using an immunohistochemistry (IHC) assay, PD-L1 IHC 22C3 pharmDx assay (DAKO, Glostrup, Denmark). For clinical diagnosis, tumor samples were obtained via core needle biopsy, excisional biopsy, or endobronchial ultrasound-guided transbronchial needle aspiration.
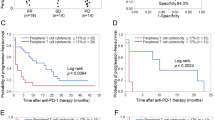
Correlation of the K-index with response to initial pembrolizumab therapy in patients with NSCLC. (a) PFS curves of patients receiving the first-line treatment. The blue line indicates K-index ≥192, and the red line indicates a K-index < 192. (b) OS curves of patients receiving first-line treatment. Statistical significance was assessed using the log-rank test. NSCLC, non-small cell lung cancer; OS, overall survival; mOS, median OS; PFS, progression-free survival; mPFS, median PFS
Clinical samples for establishing the WB method
Blood samples were collected from 76 patients with lung cancer at the Saitama Medical University International Medical Center (Saitama, Japan) from October 2020 to December 2021. This study was approved by ethical committee of Saitama Medical University International Medical Center. Written informed consent was obtained from all patients before sample collection, in accordance with the Declaration of Helsinki.
Blood samples were collected into heparinized CPT Vacutainer tubes (BD Biosciences, Franklin Lakes, NJ, USA) for PBMC isolation. Both heparin- and EDTA-2K-containing blood collection tubes were used to collect WB, and the samples were stored at room temperature (18–24 °C) before sample preparation for FCM.
Sample preparation for FCM
For the PBMC method, blood samples collected in heparinized CPT Vacutainer tubes were centrifuged at 1500×g for 20 min at room temperature (18–24 °C) to separate PBMCs from erythrocytes and granulocytes over a Ficoll gradient. The PBMCs were then frozen at − 80 °C in Cellbanker2 (Nippon Zenyaku Kogyo Co., Ltd., Fukushima, Japan) and transferred into a liquid nitrogen tank within a week. For T cell subset analyses, cells were incubated for 32–48 h in a culture medium comprising RPMI1640 and 10% fetal calf serum (FCS) before staining.
For the WB method, CD235ab-biotin (Clone HIR2; BioLegend, San Diego, CA, USA) and streptavidin magnetic beads (BioLegend) were added to the blood samples collected in heparin or EDTA-2K-containing blood collection tubes. Red blood cells (RBCs) were removed using cell separation magnets.
Cultured PBMC- and RBC-free WB cells were stained with CD4-FITC (Clone MEM-241; EXBIO Praha, a.s., Vestec, Czech Republic), CD25-PECy7 (Clone MEM-181, EXBIO), and CD62L-APC (Clone LT-TD180, EXBIO) at room temperature (18–24 °C). FOXP3 was then stained with a Foxp3/Transcription Factor Staining Buffer set (Thermo Fisher Scientific, Waltham, MA, USA) and anti-FOXP3-PE (Clone PCH101, Thermo Fisher Scientific or Clone 206D, BioLegend) according to the supplier’s protocol. The optimal dilution ratio of the antibodies and incubation time were determined in a pilot study and ensured in this study. The antibody panel in this study was confirmed to have the same performance as that of the panel in our previous study [15] (Supplementary Fig. 1).
Flow cytometry
The samples were measured using BD Accuri™ C6 Plus (BD Biosciences), BD FACSCanto™ II (BD), or Sysmex XF-1600 (Sysmex Corporation, Kobe, Japan) according to the manufacturer’s instructions. Fifteen thousand (15,000) CD4+ cells were analyzed in each measurement. The data were analyzed using FlowJo software version 10 (FlowJo, Ashland, OR, USA).
K-index calculation
The K-index was calculated using the prediction formula reported in a previous study [15]. The formula X2/Y was based on the percentages of CD62Llow cells (X) and CD25+FOXP3+ cells (Y) in the total population of CD4+ cells.
To evaluate the correlation of the K-index with the PBMC method, the formula was slightly modified from that reported in our previous study. In this study, we calculated the natural logarithm of X2/Y.
Statistical analysis
The data in Fig. 1 and Supplementary Fig. 2 were statistically analyzed at Saitama Medical University using Prism 9 (GraphPad Software, San Diego, CA, USA). Survival curves were estimated using the Kaplan-Meier method. All P-values were two-sided, and statistical significance was set as P < 0.05.
The data in Figs. 4–7 were statistically analyzed at Sysmex Corporation using StatFlex (Artech, Osaka, Japan). A correlation analysis was performed using a linear regression model.
Results
K-index to predict pembrolizumab response
As previously mentioned, the index obtained by dividing the square of the CD62Llow CD4+ T cell ratio by the CD4+CD25+FOXP3+ T cell ratio, analyzed using pretreatment peripheral blood, can be used to predict the response to nivolumab therapy in patients with previously treated NSCLC [15]. In this study, we prospectively evaluated whether the index obtained from pretreatment peripheral blood can be used as an accurate prognostic indicator in 59 consecutive patients with advanced or recurrent NSCLC who received initial pembrolizumab treatment. As this was an observational study of clinical treatment, it was performed following the Japanese insurance approval criteria. All patients were PD-L1 TPS positive, and 57 of the 59 patients had TPS ≥ 50%. The characteristics of the patients included in this study are listed in Table 1.
The overall analysis showed a median PFS (mPFS) of 206 days and a 12-month PFS of 37.1%, which was similar to the subgroup analysis of KEYNOTE-042 [16], which reported an mPFS of 207 days and a 12-month PFS of 37.1% in patients with a TPS ≥ 50% (Supplementary Fig. 2a and b). Moreover, PFS and overall survival (OS) were analyzed in the two groups using the index obtained from the analysis of pretreatment peripheral blood, and the index threshold was 192 (obtained in our previous study [15]). PFS analysis showed that the effect of pembrolizumab was significantly better in the group with an index ≥192 (hazard ratio [HR], 0.4065; P = 0.007 [log-rank test]). The mPFS was 363.0 days in the group with an index ≥192 and 122.5 days in the group with an index < 192 (Fig. 1a). OS was also significantly better in the group with an index ≥192; the median OS (mOS) was undefined in the group with index ≥192 and 324.0 days in the group with index < 192 (HR, 0.417; P = 0.19; Fig. 1b). These results indicate that our formula consistently predicted the response to first-line pembrolizumab in patients with NSCLC.
Development of the WB method to obtain the K-index
As the K-index was useful for predicting the response to pembrolizumab, and its significance was confirmed, we aimed to develop an easier method to measure the index. An outline of the PBMC and WB methods is shown in Fig. 2. The WB method was designed for automated sample preparation.
The data obtained from the FCM measurements were analyzed using the gating strategy illustrated in Fig. 3. Singlet cells were gated using an FSC-A/FSC-H dot plot (Fig. 3a and f). Lymphocytes were gated using an FSC-A/SSC-A dot plot (Fig. 3b and g). CD4+ T cells were gated using a CD4+/SSC-A dot plot (Fig. 3c and h). Cells with low CD62L expression were selected as CD4+ effector T cells (Teff; Fig. 3d and i). Cells expressing both CD25 and FOXP3 were selected as CD4+ regulatory T cells (Fig. 3e and j). Considering the future automation of WB method analysis, a rectangular fixed gate was adopted for the Treg gate setting, as shown in Fig. 3j.
Gating strategy for FCM data analysis. a, f Singlet cells gated using FSC-A/FSC-H dot plot. b, g Lymphocytes gated using FSC-A/SSC-A dot plot. c, h CD4+T cells gated using CD4+/SSC-A dot plot. d, i Cells with low CD62L expression are selected as CD4+Teff cells. e, j Cells expressing both CD25 and FOXP3 are selected as CD4+Treg cells. FCM, flow cytometry; Teff, effector T cells; Treg, regulatory T cells
Moreover, we investigated the correlation between the PBMC and WB measurements. The correlation coefficients for %Teff, %Treg, and the K-index between the two methods were 0.940, 0.705, and 0.908, respectively (Fig. 4a–c). The WB method correlated well with the PBMC method, with a sufficiently high K-index correlation. However, the %Treg value in the WB method was higher than that in the PBMC method, and subsequently, the K-index value in the WB method was lower than that in the PBMC method (Fig. 4b and c). These results suggest that the cutoff value to predict the response to anti-PD-1 therapy should be adjusted in future clinical studies.
The correlation between measurements using the PBMC and WB methods. a–c Blood samples were collected from 53 patients with lung cancer; each sample was divided into two and measured using PBMC and WB methods. Regression lines and correlation coefficients were calculated for %Teff (a), %Treg (b), and the K-index (c). The gray line represents the regression line, the light gray line represents the 95% confidence interval, and the dotted line represents the 95% prediction interval. PBMC, peripheral blood mononuclear cells; Teff, effector T cells; Tregs, regulatory T cells
We then investigated the repeatability of the %Teff, %Treg, and K-index measurements using the WB methods. The same measurements were repeated by equally dividing each blood sample into five tubes. As shown in Table 2, the percentage coefficient of variation values of the five measurements of %Teff, %Treg, and K-index was less than 10%, indicating that the WB method had a high repeatability.
We confirmed that the values (%Teff, %Treg, K-index) obtained by excluding dead cells from PBMCs using CyTOF [18] were correlated with those obtained by the WB method (Supplementary Fig. 3). This result indicated no or slight influence of dead cell contamination in the measurement of the WB method established in this study.
Adaptability of the WB method as a diagnostic test
The anticoagulants Heparin and EDTA-2K are commonly used during blood collection for blood cell analysis [19]. We investigated whether there were differences in the measured values of %Teff, %Treg, and K-index using the WB method depending on whether heparin or EDTA-2K was used. We found that regardless of whether heparin or EDTA-2K was used at the time of blood collection, the measured values of %Teff, %Treg, and K-index were the same for the same healthy volunteers or patients with lung cancer (Fig. 5a–c). These results indicate the possibility of sharing blood samples between K-index testing and other blood tests. This will contribute to a reduction in patient burden at the time of testing.
Effect of different anticoagulants during blood sampling in the WB method. a–c Blood samples were collected from 50 patients with lung cancer. Each sample was collected in heparin-containing and EDTA-2K-contained blood collection tubes. The correlation of the data obtained by both blood sampling methods is shown as %Teff (a), %Treg (b), and K-index (c). Regression lines and correlation coefficients were calculated for %Teff, %Treg, and the K-index. The gray line represents the regression line, the light gray line represents the 95% confidence interval, and the dotted line represents the 95% prediction interval. WB, whole blood; Teff, effector T cells; Treg, regulatory T cells
Depending on the circumstances, the collected blood samples were measured either immediately or at another laboratory. Therefore, we investigated whether blood samples could be stored for measurement using the WB method. Blood samples from patients with lung cancer were stored in heparin-containing blood collection tubes at room temperature (18–24 °C) for 1 d after blood sampling. The values of %Teff, %Treg, and the K-index of the same sample measured within 4 h after blood collection and after storage for 1 d (Fig. 6a–c) were the same. These results indicate that the blood samples can be stored at room temperature and sent to clinical laboratories to measure K-index.
Storage stability of blood samples in the WB method. a–c Blood samples collected into heparin-containing blood collection tubes from 20 patients with lung cancer patients were measured by the WB method a day after blood collection and compared with the values measured in the same manner within 4 h after blood collection. Regression lines and correlation coefficients were calculated for %Teff (a), %Treg (b), and K-index (c). Twenty-two samples collected from healthy individuals were measured using the WB method a day after blood collection and compared with the values measured in the same manner within 4 h after blood collection. The gray line represents the regression line, the light gray line represents the 95% confidence interval, and the dotted line represents the 95% prediction interval. WB, whole blood; Teff, effector T cells; Treg, regulatory T cells
Finally, we examined whether the WB method can be applied to different FCM instruments. The same blood samples from patients with lung cancer prepared using the WB method were measured simultaneously using a BD FACSCanto II and Sysmex XF-1600. The measured results were well correlated in both measurements using FACSCanto II and XF-1600 (Fig. 7a–c), indicating that the measurement of the K-index is a robust test and is not affected by differences in FCM instruments.
Effect of different FCM measuring devices on measured values in the WB method. a–c Blood samples were collected from 24 pretreated patients with lung cancer using the WB method and measured simultaneously using both XF-1600 and FACS Canto II. The correlation of both measurements was analyzed, and regression lines and correlation coefficients were calculated for %Teff (a), %Treg (b), and the K-index (c). The gray line represents the regression line, the light gray line represents the 95% confidence interval, and the dotted line represents the 95% prediction interval. WB, whole blood; FCM, flow cytometry; Teff, effector T cells; Treg, regulatory T cells
Discussion
Various PD-1 inhibitor combination therapies are being developed to enhance T cell restoration and increase the probability of long-term survival of patients with cancer [20,21,22,23]. However, excessive T cell restoration can lead to an increased incidence and severity of immune-related adverse events [21, 23,24,25]. To resolve this dichotomy, predicting whether patients will achieve sufficient long-term survival using a single PD-1 inhibitor is necessary. Monotherapy should be used when the probability of long-term survival with PD-1 blockade therapy is high, and combination therapy should be used when the probability is low [26]. Tumor PD-L1 expression assessed by IHC correlates with PD-1 inhibitor treatment efficacy and has been used as a reference for treatment selection in clinical practice [27]. However, the expression levels of PD-L1 detected by IHC lacks predictive accuracy because of its temporal and spatial heterogeneity [21, 23]. In this study, we demonstrated that among patients with NSCLC with a PD-L1 TPS ≥ 50%, despite varied pretreatment K-index, the PFS after pembrolizumab treatment was accurately predicted by the K-index. Therefore, the K-index is a promising diagnostic biomarker for predicting response to anti-PD-1 therapy.
Recent studies have revealed the main point of action of PD-1 inhibitors in CD8+ T cells [28, 29]. CD4+ T cells are essential for antitumor immunity, whereby they act as the driving force of the cancer immunity cycle by assisting the priming and clonal expansion of CD8+ T cells in the lymph nodes, promoting their migration into the peripheral blood circulation and infiltration into the tumor microenvironment []. Therefore, the K-index acts as a predictive biomarker that reflects the strength of CD4+ T cell immunity. Furthermore, it can be measured with a minimally invasive diagnostic method using peripheral blood and can also be measured over time. The K-index is a potential biomarker for appropriate patient selection in the development of new therapies using ICIs, such as adjuvant or combination therapy with ICI.
In our previous study [15], the experimental method for obtaining the K-index included many techniques requiring experimental skills that may not be suitable for widespread diagnostic testing. Therefore, in this study, we developed a method that can immediately and simply measure the K-index using WB samples. This method is based on isolating red blood cells from WB and simultaneously staining them with four types of fluorochrome-conjugated antibodies (anti-CD4, anti-CD25, anti-CD62L, and anti-Foxp3). The K-index measurements of the WB method correlated well with those of the original PBMC method (r = 0.908; Fig. 4c), and its repeatability was high (coefficient of variation < 10%; Table 2). The analytical performance and repeatability met the requirements of recent high-sensitivity FCM assay systems [31]. Therefore, the WB method can be used to predict the response to anti-PD-1 therapy instead of the PBMC method. However, since the K-index of the WB method was lower than that of the PBMC method (Fig. 4c), the cutoff value for clinical diagnosis needs to be adjusted accordingly. In this study, we conducted various experiments to develop a method that can be widely applied in clinical settings. We demonstrated that both heparin and EDTA-2K could be used as anticoagulants for blood sampling, and WB samples can be stored at room temperature (18–24 °C) for at least one day before measurement. Moreover, no difference was observed in the K-index measurements between the BD FACSCanto II and Sysmex XF-1600. Overall, here, we demonstrated the analytical performance of the WB method; however, we did not investigate its clinical performance. Therefore, clinical trials are needed to confirm the ability of the K-index (measured with the WB method) to predict the response to anti-PD-1 therapy.
We are currently working to evaluate the stability of the stored blood sample for more than 2 days and develop an automated sample preparation system for the WB method. Our future research aims to conduct multicenter studies to validate the clinical applicability of the K-index measured using the WB method and determine the cutoff values for clinical diagnosis.
Conclusion
This study demonstrated that the K-index could predict the efficacy of various anti-PD-1 therapies. The newly established WB method for obtaining the K-index can replace the cumbersome PBMC method used in the past. The findings of this study are expected to help demonstrate the importance of the K-index in predicting the response to anti-PD-1 therapy in various cancers, including NSCLC.
Availability of data and materials
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Abbreviations
- ICI:
-
immune checkpoint inhibitor
- IHC:
-
immunohistochemistry
- IVD:
-
in vitro diagnostics
- mOS:
-
median overall survival
- mPFS:
-
median progression-free survival
- NSCLC:
-
non-small cell lung cancer
- OS:
-
overall survival
- PBMC:
-
peripheral blood mononuclear cell
- PFS:
-
progression-free survival
- RBC:
-
red blood cell
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- Teff:
-
effector T cells
- FCM:
-
flow cytometry
- Treg:
-
regulatory T cells
- TPS:
-
tumor proportion score
References
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung Cancer. N Engl J Med. 2015;373:1627–39.
Brahmer J, Reckamp KL, Baas P, Crinò L, Eberhardt WE, Poddubskaya E, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung Cancer. N Engl J Med. 2015;373:123–35.
Ferris RL, Blumenschein G Jr, Fayette J, Guigay J, Colevas AD, Licitra L, et al. Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N Engl J Med. 2016;375:1856–67.
Gettinger S, Horn L, Jackman D, Spigel D, Antonia S, Hellmann M, et al. Five-year follow-up of Nivolumab in previously treated advanced non-small-cell lung Cancer: results from the CA209-003 study. J Clin Oncol. 2018;36:1675–84.
Kang YK, Boku N, Satoh T, Ryu MH, Chao Y, Kato K, et al. Nivolumab in patients with advanced gastric or gastro-oesophageal junction cancer refractory to, or intolerant of, at least two previous chemotherapy regimens (ONO-4538-12, ATTRACTION-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390:2461–71.
Motzer RJ, Escudier B, McDermott DF, George S, Hammers HJ, Srinivas S, et al. Nivolumab versus Everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373:1803–13.
Robert C, Long GV, Brady B, Dutriaux C, Maio M, Mortier L, et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 2015;372:320–30.
Wolchok JD, Kluger H, Callahan MK, Postow MA, Rizvi NA, Lesokhin AM, et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369:122–33.
Li H, Ma W, Yoneda KY, Moore EH, Zhang Y, Pu LL, et al. Severe nivolumab-induced pneumonitis preceding durable clinical remission in a patient with refractory, metastatic lung squamous cell cancer: a case report. J Hematol Oncol. 2017;10:64.
Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung Cancer. N Engl J Med. 2016;375:1823–33.
Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, von Pawel J, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389:255–65.
Topalian SL, Sznol M, McDermott DF, Kluger HM, Carvajal RD, Sharfman WH, et al. Survival, durable tumor remission, and long-term safety in patients with advanced melanoma receiving nivolumab. J Clin Oncol. 2014;32:1020–30.
Weber JS, Hodi FS, Wolchok JD, Topalian SL, Schadendorf D, Larkin J, et al. Safety profile of Nivolumab monotherapy: a pooled analysis of patients with advanced melanoma. J Clin Oncol. 2017;35:785–92.
Bravaccini S, Bronte G, Ulivi P. TMB in NSCLC: A Broken Dream? Int J Mol Sci. 2021;22:6536.
Kagamu H, Kitano S, Yamaguchi O, Yoshimura K, Horimoto K, Kitazawa M, et al. CD4+ T-cell immunity in the peripheral blood correlates with response to anti-PD-1 therapy. Cancer Immunol Res. 2020;8:334–44.
Mok TSK, Wu YL, Kudaba I, Kowalski DM, Cho BC, Turna HZ, et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393:1819–30.
Feehan C, Darlak K, Kahn J, Walcheck B, Spatola AF, Kishimoto TK. Shedding of the lymphocyte L-selectin adhesion molecule is inhibited by a hydroxamic acid-based protease inhibitor. Identification with an L-selectin-alkaline phosphatase reporter. J Biol Chem. 1996;271:7019–24.
Kagamu H, Yamasaki S, Kitano S, Yamaguchi O, Mouri A, Shiono A, et al. Single-cell analysis reveals a CD4+ T cell cluster that correlates with PD-1 blockade efficacy. Cancer Res. 2022. in press
Kaido M, Takagi Y, Kono M, Nakazawa F, Yamamoto S, Wada A, et al. Investigation of morphological changes for the discrimination of nucleated red blood cells and other leukocytes in Sysmex XN hematology analyzer scattergrams using transmission electron microscopy. Pract Lab Med. 2017;8:70–6.
Gadgeel S, Rodríguez-Abreu D, Speranza G, Esteban E, Felip E, Dómine M, et al. Updated analysis from KEYNOTE-189: Pembrolizumab or placebo plus Pemetrexed and platinum for previously untreated metastatic nonsquamous non-small-cell lung Cancer. J Clin Oncol. 2020;38:1505–17.
Hellmann MD, Paz-Ares L, Bernabe Caro R, Zurawski B, Kim SW, Carcereny Costa E, et al. Nivolumab plus Ipilimumab in advanced non-small-cell lung Cancer. N Engl J Med. 2019;381:2020–31.
Nasser NJ, Gorenberg M, Agbarya A. First line immunotherapy for non-small cell lung Cancer. Pharmaceuticals (Basel). 2020;13:373
Paz-Ares L, Ciuleanu TE, Cobo M, Schenker M, Zurawski B, Menezes J, et al. First-line nivolumab plus ipilimumab combined with two cycles of chemotherapy in patients with non-small-cell lung cancer (CheckMate 9LA): an international, randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22:198–211.
Wang DY, Salem JE, Cohen JV, Chandra S, Menzer C, Ye F, et al. Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and Meta-analysis. JAMA Oncol. 2018;4:1721–8.
Zhang B, Wu Q, Zhou YL, Guo X, Ge J, Fu J. Immune-related adverse events from combination immunotherapy in cancer patients: a comprehensive meta-analysis of randomized controlled trials. Int Immunopharmacol. 2018;63:292–8.
Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, et al. Five-year outcomes with Pembrolizumab versus chemotherapy for metastatic non-small-cell lung Cancer with PD-L1 tumor proportion score ≥ 50. J Clin Oncol. 2021;39:2339–49.
Gandini S, Massi D, Mandalà M. PD-L1 expression in cancer patients receiving anti PD-1/PD-L1 antibodies: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2016;100:88–98.
Wei SC, Levine JH, Cogdill AP, Zhao Y, Anang NAS, Andrews MC, et al. Distinct cellular mechanisms underlie anti-CTLA-4 and anti-PD-1 checkpoint blockade. Cell. 2017;170:1120–1133.e17.
Willsmore ZN, Coumbe BGT, Crescioli S, Reci S, Gupta A, Harris RJ, et al. Combined anti-PD-1 and anti-CTLA-4 checkpoint blockade: treatment of melanoma and immune mechanisms of action. Eur J Immunol. 2021;51:544–56.
Borst J, Ahrends T, Bąbała N, Melief CJM, Kastenmüller W. CD4+ T cell help in cancer immunology and immunotherapy. Nat Rev Immunol. 2018;18:635–47.
Selliah N, Eck S, Green C, Oldaker T, Stewart J, Vitaliti A, et al. Flow cytometry method validation protocols. Curr Protoc Cytom. 2019;87:e53.
Acknowledgments
We thank Ms. Koko Kodaira, Ms. Marliza Madung, Dr. Fumie Kato, Ms. Kyoko Hirai, and Mr. Tatsuya Yamagiwa for their technical assistance.
Funding
This research was supported by the Grants-in-Aid for Scientific Research (KAKENHI) program of the Japan Society for the Promotion of Science (Grant Number 17H04184) and the Agency for Medical Research and Development (AMED; grant number JP21ae0101074).
Author information
Authors and Affiliations
Contributions
Conception and design: OY and KA; Development of methodology: KA, YM, and HU; Acquisition of data: OY, KA, AS, AM, FN, YM, KH, YM, KK, and KK; Analysis and interpretation of data: KA, KY, NS, TM, NK, and HK; Writing, review, and/or revision of the manuscript: OY, KA, KY, HU, NS, and HK. The authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Internal Review Committee of Saitama Medical School International Medical Center and was performed in accordance with the Declaration of Helsinki. All patients provided written informed consent before participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Fig. 1.
Performance comparison between the antibody panels in the previous report [15] (X-axis) and this report (Y-axis). (a–c) Twenty commercially available PBMC (Cellular Technology Ltd., Shaker Heights, OH, USA) were stained with CD4-BV650 (Clone OKT4, BioLegend, San Diego, CA, USA), CD25-PE-CF594 (Clone M-A251, BD, Franklin Lakes, NJ, USA), CD62L-BV421 (Clone DREG56, BioLegend) and anti-FOXP3-PE (Clone 236A/E7, Thermo Fisher Scientific, Waltham, MA, USA) as the antibody panel in the previous report. The samples were analyzed using a BD FACSLyric™ (BD Biosciences). The correlation of the data obtained by both panels is shown as %Teff (a), %Treg (b), and the K-index (c). Regression lines and correlation coefficients were calculated for %Teff, %Treg, and the K-index. The gray line represents the regression line, the light gray line represents the 95% confidence interval, and the dotted line represents the 95% prediction interval. PBMC, peripheral blood mononuclear cells; Teff, effector T cells; Tregs, regulatory T cells.
Additional file 2: Supplementary Fig. 2.
Overall analysis data of response to initial pembrolizumab therapy in patients with NSCLC. Analysis of mPFS (a) and mOS (b). mOS, median overall survival; mPFS, median progression-free survival; NSCLC, non-small cell lung cancer; PD, progressive disease; PR, partial response; SD, stable disease.
Additional file 3: Supplementary Fig. 3.
Correlation between measurements obtained using the PBMC and WB methods. The measurements were performed using CyTOF in the PBMC method and FCM in the WB method. The gating strategy of CyTOF analysis was performed as described in a previous study [18]. In brief, dead cells were removed using 198Pt staining. The analysis of the lower layer of CD4+ cells was the same as the FCM analysis. Blood samples were collected from 53 patients with lung cancer. (a–c) Each sample was divided into two and measured using PBMC and WB methods. Regression lines and correlation coefficients were calculated for %Teff (a), %Treg (b), and the K-index (c). The gray line represents the regression line, the light gray line represents the 95% confidence interval, and the dotted line represents the 95% prediction interval. PBMC, peripheral blood mononuclear cells; Teff, effector T cells; Tregs, regulatory T cells.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yamaguchi, O., Atarashi, K., Yoshimura, K. et al. Establishing a whole blood CD4+ T cell immunity measurement to predict response to anti-PD-1. BMC Cancer 22, 1325 (2022). https://doi.org/10.1186/s12885-022-10445-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-10445-2