Abstract
Background
The aim of this study was to estimate occupational risk variation in the incidence of nasopharyngeal cancer (NPC) in a large population-based cohort of the Nordic Occupational Cancer (NOCCA) study.
Methods
This study is based on a cohort of almost 15 million persons from Denmark, Finland, Iceland, Norway and Sweden, with 2898 nasopharyngeal cancer cases diagnosed in 1961–2005. The data on occupations were gathered from population censuses and cancer data from the national cancer registries. Standardized incidence ratios (SIR) with 95% confidence intervals (CI) were estimated using the national NPC incidence rates as the reference.
Results
There were 1980 male and 918 female NPC patients. The highest SIRs of NPC were observed among male waiters (SIR 3.69, 95% CI 1.91–6.45) and cooks and stewards (SIR 2.24, 95% CI 1.16–3.91). Among women, launderers had the highest SIR of NPC (2.04, 95% CI 1.02–3.65). Significantly decreased SIRs were found among male farmers (SIR 0.79, 95% CI 0.68–0.92) and male textile workers (SIR 0.49, 95% CI 0.22–0.93).
Conclusions
This study suggests that NPC may be associated with several work-related exposure agents such as smoking, kitchen air pollution and solvents. In future, occupational exposure-risk relations should be studied to understand more about causality and to assess effective prevention strategies.
Similar content being viewed by others
Background
Close to 850,000 new head and neck squamous cell carcinoma (HNSCC) cases are diagnosed annually worldwide, and approximately 130,000 of these are nasopharyngeal carcinomas (NPC) [1]. The NPC incidence is much higher in South-Asia than in Europe and North America [1, 2]. The majority of NPC cases in endemic areas are non-keratinizing and predominantly associated with the Epstein-Barr virus (EBV) [3]. Another major risk factor for NPC is tobacco smoking [4,5,6].
Exposure to occupation-related agents such as formaldehyde and chlorophenol, wood and cotton dust, smokes, and combustion have been associated with the development of NPC [7,8,9,10,11,12]. Upper airways including the nasopharynx are directly affected by these often work-related exposures. For example, occupational exposures to formaldehyde and wood dust have been classified by the International Agency for Research on Cancer (IARC) as having sufficient evidence of causing NPC in humans [13]. Long-lasting wood dust exposure especially appears to increase the risk of NPC [14,15,16,17,18,19]. Cotton dust, which is common in the textile industry, is another exposure that has been linked with NPC, but evidence remains inconclusive [20, 21].
The aim of this study was to identify occupations linked to NPC in the five Nordic countries.
Methods
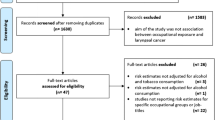
This study is based on NPC patients included in the Nordic Occupational Cancer (NOCCA) study cohort. The NOCCA cohort includes census participants covering a total of 14.9 million persons from Denmark, Finland, Iceland, Norway and Sweden followed up between 1961 and 2005 [22].
Subjects aged 30–64 years old and alive on January 1 of the year after the first available census were linked to their occupational data and cancer data with the help of the unique personal identity codes given to all residents of the Nordic countries [23]. The follow-up time of each individual started from the year following the first available census record of the person and ended at the date of emigration, death or at the end of the following years: Finland and Sweden 2005, Iceland 2004 and Norway and Denmark 2003 [24]. The present study used the occupational data that were originally coded according to Nordic Occupational Classification (NYK), International Standard of Classification of Occupations (ISCO) versions 58 and 68, or a special Danish classification were classified into 54 occupational categories. A detailed description of the NOCCA cohort and occupational data are presented in previous reports [23, 25]. For this study, all health care occupations were combined as the group of “health workers” because the number of cases in each category was low. Only occupational categories with ≥5 cases (Nordic total) are shown separately in the tables. The categories with less than 5 cases were added into the category “other economically active”.
Data on NPCs (International Classification of Diseases, 7th Revision, code 146) were obtained from the cancer registry of each country. During the follow-up period, all cancer registries received clinical notifications from hospitals and all except Denmark also from cancer laboratories in the public and private sectors [26].
The standardized incidence ratio (SIR) was used as the measure of relative risk of NPC. SIR is the ratio of the observed and expected numbers of cases. The expected number of cases in each country, gender, 5-year calendar period and 5-year age category was calculated by multiplying the number of person-years in the stratum by the respective national incidence rate of NPC. Exact 95% confidence intervals (CI) were determined by Poisson distribution, and the SIR was considered as statistically significant if its CI did not include 1.0. The study has permissions as required in each of the Nordic countries.
Results
Altogether, 2898 patients diagnosed with NPC were observed during the follow-up of the present study. There were 1980 male and 918 female NPC patients. The majority (n = 1524) of the patients were from Sweden, and only 18 patients were from Iceland.
The highest SIR of NPC was found among male waiters in the whole Nordic cohort (SIR 3.69, 95% CI 1.91–6.45) and separately in Norway (SIR 4.79, 95% CI 1.30–12.25) and Denmark (SIR 6.81, 95% CI 2.21–15.88) (Table 1). The SIR for female waiters was not significantly elevated (Table 2).
The SIR was significantly elevated among male cooks and stewards in the entire Nordic cohort (SIR 2.24, 95% CI 1.16–3.91) and in the Swedish cohort (SIR 2.68, 95% CI 1.08–5.53). The incidence of NPC was consistently elevated among male bricklayers in all countries. Finnish male administrators and sales agents had significantly elevated SIRs, but similar findings were not observed in other Nordic countries.
Among females, launderers had the highest and significantly elevated SIR in the entire cohort (SIR 2.04, 95% CI 1.02–3.65) and separately in the Norwegian cohort (SIR 5.38, 95% CI 1.47–13.79).
Significantly decreased incidence of NPC was found among Nordic male farmers (SIR 0.79, 95% CI 0.68–0.92) and male textile workers (SIR 0.49, 95% CI 0.22–0.93). The SIR for farmers was especially low in Finland and Denmark (SIR 0.58, 95% CI 0.36–0.88 and 0.65, 95% CI 0.42–0.95, respectively).
Male fishermen in Norway had a significantly elevated SIR (1.64, 95% CI 1.03–2.49, Table 1), and SIRs for both fishermen and seamen were consistently elevated in all countries except for Swedish fishermen, who had a low SIR.
Discussion
This study provides new evidence on occupational risk variation of NPC in the Nordic countries. Norwegian, Finnish and Swedish fishermen had elevated SIRs of NPC in the present study, which to our knowledge, is a new finding. In addition, the SIRs for seamen were consistently elevated. Salted fish is a confirmed risk factor for NPC and commonly used in Southern Asia [27], but we have no evidence whether fishermen in the three Nordic countries consume more salted fish than the reference population. Fishermen might have been exposed to off-gas from fermented fish, especially in former times when the storage tanks on fishing boards were emptied manually.
Cooks and stewards showed elevated SIRs in the present study. The elevated risk for lung cancer among cooks has been previously related to indoor air pollution, which may also be one link between cooks and NPC [28]. In addition, wood combustion has been found to be a potential risk factor for NPC and a potential exposure agent for cooks [29].
In some previous studies, frequent exposure to cotton dust has been associated with elevated risk of NPC [12, 21, 30]. We did not find an elevated SIR among female textile workers, and there was a statistically significant decreased SIR for male textile workers. Thus, this study does not support such evidence.
We found that female launderers had statistically significantly higher risk of NPC than the population on average. In drycleaning, tetrachloroethylene is the dominant solvent used throughout the world and in the Nordic countries [31].
The IARC classified formaldehyde and wood dust as occupational carcinogens in relation to NPC. In the present study, exposure to these agents is most likely among woodworkers, but we did not find elevated SIRs among them [32].
NPC incidence was significantly elevated among male waiters. Previously, Nordic waiters have been related to elevated incidence of lung cancer, oral cancer and pharyngeal cancer [33]. An increased risk of death from NPC was reported among waiters in China [34]. One explanation may be that waiters have been exposed to passive and active tobacco smoke, which has also been associated with NPC [4, 35]. Prior to smoking restrictions in bars and restaurants, waiters worked in a smoke-filled environment and had a higher proportion of active smokers than other workers [33]. Several studies have shown a modestly increased risk of NPC associated with tobacco smoking, and a meta-analysis indicated an approximately 60% increased risk for NPC among smokers [36, 37]. In Finland and Norway, smoke-free legislation in restaurants has shown effective results in the decrease of passive smoking exposure [35, 38] and improving lung function [39] among waiters. Therefore, it is expected that the excess incidence of NPC among restaurant staff will become smaller in the future.
Strengths of this study include the large cohorts with nationwide population-based data, long follow-up periods and high quality registry data [26]. A limitation of the present study was the missing stratification of NPCs by histological subtype, and the lack of information on factors not directly related to occupation. It has been demonstrated that the role of tobacco and alcohol use in the occupational risk variation in the risk for head neck cancer in the Nordic countries is large [40]. In addition, since the current data only reach to the end of the year 2005, they mainly reflect occupational exposures before the mid-1990s, considering the long latency in cancer process.
Conclusions
The present study suggests that certain work-related exposures such as passive smoking, kitchen air pollution and solvents may be associated with NPC. In future, exposure-risk relations should be studied to understand more about causality and to assess effective prevention strategies against NPC.
Availability of data and materials
The tabulated datasets generated and/or analysed during the current study are available in the NOCCA repository, https://astra.cancer.fi/NOCCA/.
Abbreviations
- EBV:
-
Epstein-Barr virus
- CI:
-
Confidence interval
- HNSCC:
-
Head and neck squamous cell carcinoma
- HPV:
-
Human papillomavirus
- IARC:
-
International Agency for Research on Cancer
- ISCO:
-
International Standard of Classification of Occupations
- NOCCA:
-
Nordic Occupational Cancer Study
- NPC:
-
Nasopharyngeal carcinoma
- NYK:
-
Nordic Occupational Classification
- SIR:
-
Standardized incidence ratio
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Tang LL, Chen WQ, Xue WQ, He YQ, Zheng RS, Zeng YX, et al. Global trends in incidence and mortality of nasopharyngeal carcinoma. Cancer Lett. 2016;374(1):22–30.
Young LS, Dawson CW. Epstein-Barr virus and nasopharyngeal carcinoma. Chin J Cancer. 2014;33(12):581–90.
Chang ET, Liu Z, Hildesheim A, Liu Q, Cai Y, Zhang Z, et al. Active and passive smoking and risk of nasopharyngeal carcinoma: a population-based case-control study in southern China. Am J Epidemiol. 2017;185(12):1272–80.
West S, Hildesheim A, Dosemeci M. Non-viral risk factors for nasopharyngeal carcinoma in the Philippines: results from a case-control study. Int J Cancer. 1993;55(5):722–7.
Fernandes Q, Merhi M, Raza A, Inchakalody VP, Abdelouahab N, Zar Gul AR, et al. Role of Epstein-Barr virus in the pathogenesis of head and neck cancers and its potential as an immunotherapeutic target. Front Oncol. 2018;8:257.
Beane Freeman LE, Blair A, Lubin JH, Stewart PA, Hayes RB, Hoover RN, et al. Mortality from solid tumors among workers in formaldehyde industries: an update of the NCI cohort. Am J Ind Med. 2013;56(9):1015–26.
Yu MC, Garabrant DH, Huang TB, Henderson BE. Occupational and other non-dietary risk factors for nasopharyngeal carcinoma in Guangzhou, China. Int J Cancer. 1990;45(6):1033–9.
Mirabelli MC, Hoppin JA, Tolbert PE, Herrick RF, Gnepp DR, Brann EA. Occupational exposure to chlorophenol and the risk of nasal and nasopharyngeal cancers among U.S. men aged 30 to 60. Am J Ind Med. 2000;37(5):532–41.
Vaughan TL, Stewart PA, Teschke K, Lynch CF, Swanson GM, Lyon JL, et al. Occupational exposure to formaldehyde and wood dust and nasopharyngeal carcinoma. Occup Environ Med. 2000;57(6):376–84.
Siew SS, Kauppinen T, Kyyrönen P, Heikkilä P, Pukkala E. Occupational exposure to wood dust and formaldehyde and risk of nasal, nasopharyngeal, and lung cancer among Finnish men. Cancer Manag Res. 2012;4:223–32.
Chen Y, Chang ET, Liu Q, Cai Y, Zhang Z, Chen G, et al. Occupational exposures and risk of nasopharyngeal carcinoma in a high-risk area: a population-based case-control study. Cancer. 2021;127(15):2724–35.
International agency for research on Cancer. Chemical agents and related occupations. In: IARC monographs on the evaluation of carcinogenic risks to humans, vol. 100F. Lyon: World Health Organization; 2012.
Chang ET, Ye W, Zeng YX, Adami HO. The evolving epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev. 2021;30(6):1035–47.
Yin J, Jin W, Mao Y, Wu Q, Qiu J. Wood dust exposure and risks of nasopharyngeal carcinoma: a meta-analysis. Eur J Public Health. 2020;30(4):817–22.
Malker HS, McLaughlin JK, Weiner JA, Silverman DT, Blot WJ, Ericsson JL, et al. Occupational risk factors for nasopharyngeal cancer in Sweden. Br J Ind Med. 1990;47(3):213–4.
Ekpanyaskul C, Sangrajrang S, Ekburanawat W, Brennan P, Mannetje A, Thetkathuek A, et al. Semi-quantitative exposure assessment of occupational exposure to wood dust and nasopharyngeal cancer risk. Asian Pac J Cancer Prev. 2015;16(10):4339–45.
Slack R, Young C, Rushton L, British Occupational Cancer Burden Study G. Occupational cancer in Britain. Nasopharynx and sinonasal cancers. Br J Cancer. 2012;107(Suppl 1):S49–55.
Beigzadeh Z, Pourhassan B, Kalantary S, Golbabaei F. Occupational exposure to wood dust and risk of nasopharyngeal cancer: a systematic review and meta-analysis. Environ Res. 2019;171:170–6.
Zheng W, McLaughlin JK, Gao YT, Gao RN, Blot WJ. Occupational risks for nasopharyngeal cancer in Shanghai. J Occup Med. 1992;34(10):1004–7.
Li W, Ray RM, Gao DL, Fitzgibbons ED, Seixas NS, Camp JE, et al. Occupational risk factors for nasopharyngeal cancer among female textile workers in Shanghai, China. Occup Environ Med. 2006;63(1):39–44.
Talibov M, Auvinen A, Weiderpass E, Hansen J, Martinsen JI, Kjaerheim K, et al. Occupational solvent exposure and adult chronic lymphocytic leukemia: no risk in a population-based case-control study in four Nordic countries. Int J Cancer. 2017;141(6):1140–7.
Riska A, Martinsen JI, Kjaerheim K, Lynge E, Sparen P, Tryggvadottir L, et al. Occupation and risk of primary fallopian tube carcinoma in Nordic countries. Int J Cancer. 2012;131(1):186–92.
Hadkhale K, Martinsen JI, Weiderpass E, Kjaerheim K, Lynge E, Sparen P, et al. Occupation and risk of bladder cancer in Nordic countries. J Occup Environ Med. 2016;58(8):e301–7.
Pukkala E, Martinsen JI, Lynge E, Gunnarsdottir HK, Sparén P, Tryggvadottir L, et al. Occupation and cancer - follow-up of 15 million people in five Nordic countries. Acta Oncol. 2009;48(5):646–790.
Pukkala E, Engholm G, Hojsgaard Schmidt LK, Storm H, Khan S, Lambe M, et al. Nordic Cancer registries - an overview of their procedures and data comparability. Acta Oncol. 2018;57(4):440–55.
Barrett D, Ploner A, Chang ET, Liu Z, Zhang C-X, Liu Q, et al. Past and recent salted fish and preserved food intakes are weakly associated with nasopharyngeal carcinoma risk in adults in southern China. J Nutr. 2019;149(9):1596–605.
Zhong L, Goldberg MS, Gao YT, Jin F. Lung cancer and indoor air pollution arising from Chinese-style cooking among nonsmoking women living in Shanghai, China. Epidemiol. 1999;10(5):488–94.
He Y-Q, Xue W-Q, Shen G-P, Tang L-L, Zeng Y-X, Jia W-H. Household inhalants exposure and nasopharyngeal carcinoma risk: a large-scale case-control study in Guangdong, China. BMC Cancer. 2015;15(1):1022.
Acquavella J, Olsen G, Cole P, Ireland B, Kaneene J, Schuman S, et al. Cancer among farmers: a meta-analysis. Ann Epidemiol. 1998;8(1):64–74.
Lynge E, Andersen A, Rylander L, Tinnerberg H, Lindbohm ML, Pukkala E, et al. Cancer in persons working in dry cleaning in the Nordic countries. Environ Health Perspect. 2006;114(2):213–9.
International Agency for Research on Cancer. Arsenic, metals, fibres and dusts. In: IARC monographs on the evaluation of carcinogenic risks to humans, vol. 100C. Lyon: World Health Organization; 2012.
Reijula J, Kjaerheim K, Lynge E, Martinsen JI, Reijula K, Sparén P, et al. Cancer incidence among waiters: 45 years of follow-up in five Nordic countries. Scand J Public Health. 2015;43(2):204–11.
Yu IT, Chiu YL, Wong TW, Tang JL. Deaths from nasopharyngeal cancer among waiters and waitresses in Chinese restaurants. Int Arch Occup Environ Health. 2004;77(7):499–504.
Reijula J, Johnsson T, Kaleva S, Tuomi T, Reijula K. Total prohibition of smoking but not partial restriction effectively reduced exposure to tobacco smoke among restaurant workers in Finland. Int J Occup Med Environ Health. 2013;26(5):682–92.
Xue W-Q, Qin H-D, Ruan H-L, Shugart YY, Jia W-H. Quantitative Association of Tobacco Smoking with the risk of nasopharyngeal carcinoma: a comprehensive meta-analysis of studies conducted between 1979 and 2011. Am J Epidemiol. 2013;178(3):325–38.
Long M, Fu Z, Li P, Nie Z. Cigarette smoking and the risk of nasopharyngeal carcinoma: a meta-analysis of epidemiological studies. BMJ Open. 2017;7(10):e016582.
Ellingsen DG, Fladseth G, Daae HL, Gjølstad M, Kjaerheim K, Skogstad M, et al. Airborne exposure and biological monitoring of bar and restaurant workers before and after the introduction of a smoking ban. J Environ Monit. 2006;8(3):362–8.
Skogstad M, Kjaerheim K, Fladseth G, Gjølstad M, Daae HL, Olsen R, et al. Cross shift changes in lung function among bar and restaurant workers before and after implementation of a smoking ban. Occun Environ Med. 2006;63(7):482–7.
Kjaerheim K, Haldorsen T, Lynge E, Martinsen JI, Pukkala E, Weiderpass E, et al. Variation in Nordic work-related cancer risks after adjustment for alcohol and tobacco. Int J Environ Res Public Health. 2018;15(12):2760.
Acknowledgements
We thank the Nordic Cancer Union for the financial support and Jan Ivar Martinsen (Cancer Registry of Norway) for data management and statistical analyses of the data.
Funding
Funding was provided by Finska Läkareskällskapet and open access funding was provided by Karolinska Institute. The data collection for the NOCCA study was supported by the Nordic Cancer Union.
Author information
Authors and Affiliations
Contributions
Timo Carpén, Evelina Gille, Lalle Hammastedt-Nordenvall and Antti Mäkitie; interpretation of results and writing of the manuscript; Elsebeth Lynge and Johnni Hansen: responsible for the data accuracy and SIR estimates of Denmark; Sanna Heikkinen current principal investigator in NOCCA study in Finland and leader of the NOCCA network; Jenny Selander: current principal investigator in NOCCA study in Sweden; Ingrid Sivesind Mehlum: current principal investigator in NOCCA study in Norway; Jóhanna Eyrún Torfadottir: current principal investigator in NOCCA study in Iceland; Eero Pukkala: design of the study, data analysis, interpretation of results, and writing the manuscript. All authors have commented the manuscript and read and approved the final version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The current study was based on data from existing registries and did not include any human intervention. The NOCCA study had ethics approvals and permissions as required in each of the participating countries at the time of data collection. The data were anonymized before using them in the analyses. Study participants were not contacted during the execution of the study. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Carpén, T., Gille, E., Hammarstedt-Nordenvall, L. et al. Occupational risk variation of nasopharyngeal cancer in the Nordic countries. BMC Cancer 22, 1130 (2022). https://doi.org/10.1186/s12885-022-10209-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-10209-y