Abstract
Background
Microsatellite instability (MSI) is a key marker for predicting the response of immune checkpoint inhibitors (ICIs) and for screening Lynch syndrome (LS).
Aim
This study aimed to see the characteristics of cancers with high level of MSI (MSI-H) in genetic medicine and precision medicine.
Methods
This study analyzed the incidence of MSI-H in 1000 cancers and compared according to several clinical and demographic factors.
Results
The incidence of MSI-H was highest in endometrial cancers (26.7%, 20/75), followed by small intestine (20%, 3/15) and colorectal cancers (CRCs)(13.7%, 64/466); the sum of these three cancers (15.6%) was significantly higher than that of other types (2.5%)(P < 0.0001). MSI-H was associated with LS-related cancers (P < 0.0001), younger age (P = 0.009), and family history, but not with smoking, drinking, or serum hepatitis virus markers. In CRC cases, MSI-H was significantly associated with a family history of LS-related cancer (P < 0.0001), Amsterdam II criteria [odds ratio (OR): 5.96], right side CRCs (OR: 4.89), and multiplicity (OR: 3.31). However, MSI-H was very rare in pancreatic (0.6%, 1/162) and biliary cancers (1.6%, 1/64) and was null in 25 familial pancreatic cancers. MSI-H was more recognized in cancers analyzed for genetic counseling (33.3%) than in those for ICI companion diagnostics (3.1%)(P < 0.0001). Even in CRCs, MSI-H was limited to 3.3% when analyzed for drug use.
Conclusions
MSI-H was predominantly recognized in LS-related cancer cases with specific family histories and younger age. MSI-H was limited to a small proportion in precision medicine especially for non-LS-related cancer cases.
Similar content being viewed by others
Background
Microsatellites are defined as 10 to 60 base pair regions which contain repeated multiple tandems consisting of 1 to 5 base pair motifs (≤ 10 bp) [1, 2] that are distributed widely throughout the genome. DNA repeats in the microsatellite loci are normally verified and maintained during cell division by the mismatch repair (MMR) function [3]. Impairment of a microsatellite system can render cells unable to regulate the length of microsatellites during cell division, a condition termed microsatellite instability (MSI). After multiple cycles of cell division, cells with an impaired MMR system will develop varying lengths in their microsatellite sequences.
MSI is a key marker to predict the effects of immune checkpoint inhibitors (ICIs) against several human cancers, as cancers with a high level of MSI (MSI-H) present increasing numbers of neoantigens that can be ICI targets [4, 5]. MSI is also a hypermutator phenotype that occurs in tumors with a deficient DNA mismatch repair function (dMMR) and therefore is a crucial screening factor for Lynch syndrome (LS), which has been diagnosed in 13–16% [6,7,8] of MSI-H cancers. As LS patients are at risk of developing multiple cancers, regular surveillance for their high-risk organs is performed to detect LS-related cancers in their early stages [9]. Hence, the detection of MSI in cancer has dual benefits in the genetic and oncological senses.
In this decade, MSI assays have become fully recognized among oncologists as a companion diagnostic or as a part of a multigene panel test [10,11,12] for judging indications of ICIs (PD-1 antagonist and PD-L1 antagonist). In December 2018, the Japanese national health insurance began covering MSI tests for cases with solid cancers refractory to the standard pharmacotherapy [13]. MSI can be analyzed using formalin-fixed paraffin-embedded cancer tissues [14] alone or in combination with non-neoplastic control DNA. The positivity of MSI or dMMR tends to be higher in LS-associated cancers, such as cancers in the colorectum, endometrium, small intestine, ureter, and renal pelvis [as defined in the Amsterdam II (AII) criteria] [8]. According to the revised Bethesda (rB) guidelines [7], which were established for indicating MSI testing, cancers of the stomach, pancreas, biliary tract, ovary, and brain and cutaneous neoplasms (keratoacanthoma and sebaceous gland adenoma) are also considered LS-associated cancers. In colorectal cancer (CRC) cases, MSI is also caused by the promoter methylation of MLH1 (often coupled with BRAF V600E mutation) [15, 16], characterized by the CpG island methylator phenotype [17] independent from LS.
This study analyzed the MSI status in 1000 Japanese human cancers with a comparison between genetic medicine and precision medicine (companion diagnostics). It also analyzed the characteristics of the MSI-H cancers with special reference to the patients’ personal and familial cancer histories.
Methods
Patients
A consecutive 1000 cancer patients [519 males and 481 females, 62.6 ± 12.0 years old (y.o.)], managed in the Shizuoka Cancer Center from January 2013 to September 2020, were entered in this study (Table 1). Of the 1000 cancers, 778 were analyzed for MSI to examine the indication of ICI via companion diagnostics and 222 were analyzed to detect LS in genetic counseling. These cancers included CRCs (466 cancers), pancreatic cancers (162), endometrial cancers (ECs)(75), biliary tract cancers (64), gastric cancers (36), uterine cervical cancers (34), laryngeal-pharyngeal and esophagus cancers (30), skin cancers (27), ovarian cancers (24), neuroendocrine carcinomas (NEC) (22), small intestine cancers (15), thymic cancers (10), breast cancers (7), hepatic cancers (6), brain tumors (2), and others (20) (Table 1). Age and incidence of smoking was not significantly different between the LS-related and non-LS-related cancers, however incidence of smoking was significantly higher in the non-LS-related cancer group (57.1%, 89/156) than LS-related cancer group (47.0%, 397/844) (P = 0.02) (Table 1).
At the initial hospital visit, patients and their families filled out questionnaires concerning disease history, family history, and lifestyles. The nurses reconfirmed the content of the questionnaires by conducting 20–30 min interviews with each patient. LS-associated cancers as defined in the AII criteria consisted of CRC, EC, renal pelvic and ureteral cancers, and small intestine cancer. Those defined in the rB guidelines included additional tumors: gastric, ovarian, pancreatic, and biliary tract cancers, brain tumors, and two cutaneous neoplasms (sebaceous adenoma and keratoacanthoma) [18]. None of the patients or their families had been diagnosed with LS before the MSI testing by the genetic counseling and companion diagnostics.
A pathological evaluation of the cancer, including the histological type and stage, was determined in the resected materials when the surgery was performed, but when using biopsy samples, the staging was judged on the clinical images, including computed tomography and endoscopy. Pathological data were corrected from the diagnostic reports by expert pathologists with their own expertise. In CRC cases, within the histological conditions described by the rB guidelines, only histological type (mucinous/signet-ring differentiation) was evaluated, as the patterns of lymphocytic reaction and cancer growth were sometimes difficult to determine in the biopsy specimens. If information of onset age or cancer type were unclear for the AII criteria and the rB guidelines, we treated them as not informative.
MSI analysis
MSI analysis for oncogenic purposes
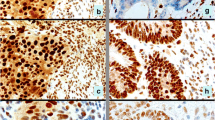
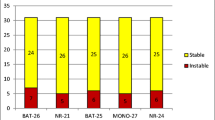
To view indications of ICI, Pembrolizumab (Keytruda®, Tokyo, MSD Japan), 778 cancers were analyzed for MSI by companion diagnostics using only tumor DNA extracted from the archives of pathological samples during December 2018 and September 2020. The pathological specimens during this period were fixed at a suitable time in 10% neutral buffered formalin for less than 48 h, then embedded in paraffin and preserved at room temperature following the Japanese guidelines on the handling and storage of tissue samples [19]. Only a small proportion of the samples were archived prior to this period. This assay was entrusted to the SRL laboratory company (Tokyo, Japan). Tumor DNA was extracted with macroscopic dissection from series of 5–10 slices of 10 μm thick sections. MSI analysis was performed by using the MSI Kit (FALCO biosystems, Kyoto, Japan), which is equipped with five mononucleotide microsatellite markers (Promega panel: BAT-25, BAT-26, MONO-27, NR-21, and NR-24), following the manufacturer’s protocol [13, 20]. MSI-H was defined when the tumor DNA demonstrated instability in two or more markers, whereas microsatellite stability (MSS) was defined when only one or a null marker showed instability.
MSI analysis for screening lynch syndrome
A total of 222 cancers were analyzed for MSI in the genetic medicine clinics to screen for LS suspected because of the patient’s cancer history and family history and the tumors’ histology and multiplicity, among other factors. Sixty-seven cancer samples (30.2%) were obtained before 2018, when the pathological sample handling guidelines were implemented. The MSI analysis was entrusted to the laboratory company FALCO biosystems and performed by following the abovementioned protocol, except for the additional use of non-neoplastic DNA as a control [20] and the partial use of Bethesda panel markers (BAT-25, BAT-26, D2S123, D5S346, and D17S250) [21] until September 2015 (11 of 222 cancers).
Statistical analysis
Statistical analyses were performed using JAMAevidence® and JMP ver.11.2.0 statistical software (SAS Institute Japan Ltd., Tokyo, Japan). A Fisher’s exact test was used to assess the categorical variables, and a Mann-Whitney U test was used to analyze the continuous variables. Multivariate analysis was performed by a logistic regression test. A value of P < 0.05 was considered statistically significant.
Results
MSI in various human cancers
As shown in Table 2, MSI-H was recognized in 98 of 1000 cancers (9.8%): 26.7% (20/75) of ECs, 20% (3/15) of small intestine cancers, 16.7% (1/6) of hepatic cancers, 13.7% (64/466) of CRCs, and 10% (1/10) of thymomas. In LS-associated cancers defined by the rB guidelines, MSI-H was very rare in pancreatic (0.6%, 1 of 162) and biliary tract cancers (1.6%, 1/64). The 25 cases of familial pancreatic cancer were completely MSS. In other cancer categories, one prostate cancer and one adrenocortical cancer were MSI-H. From the 1000 cancer MSI tests, only one case of CRC was returned with an inconclusive result; however, it was compensated with a preserved MMR protein analyzed by immunohistochemistry. Incidence of MSI-H was significantly higher in genetic counseling group than in companion diagnostics group in CRC (41.7% vs. 3.2%, P < 0.0001), endometrial cancer (45.2% vs.13.6%, P = 0.003), in ovarian cancer (66.7% vs. 0%, P = 0.011), in the subtotal of LS (AII)-related cancers (42.1% vs. 4.6%, P < 0.0001), and in the subtotal of non-LS-related cancers (40.0% vs. 2.6%, P = 0.011) (Table 2).
MSI and cancer histories
The incidence of MSI-H was highest in the AII criteria-defined LS-related cancer group (15.6%, 87/556), which was significantly higher than both other LS-related cancers defined by the rB guidelines (1.7%, 5/288)(OR: 10.50, 95% CI: 4.33–25.43, P < 0.0001) and non-LS-related cancer groups (OR: 4.64, 95% CI: 2.03–10.58, P < 0.0001) (Table 2). In these three groups, the number of the patients’ past cancers (excluding the cancer analyzed for MSI) was similar, either for any cancer type or for LS (rB)-related cancer types. However, the number of cancers developed in the FDRs was significantly higher in LS (rB)-related cancer patients (mean ± standard deviation: 1.1 ± 1.2) than in non-LS-related cancer patients (0.8 ± 1.0) (P = 0.003). This trend was commonly seen in the number of LS (rB)-related cancers in the FDRs (0.7 ± 1.0 in LS-related cancer patients vs. 0.5 ± 0.7 in non-LS-related cancer patients) (P = 0.004, Table 2) despite the similar ages of the patients among the three groups (Table 1).
Factors associated with MSI-H analyzed in 1000 cancers
Factors associated with MSI-H were determined in all 1000 cases using univariate and multivariate analyses (Table 3). MSI-H was significantly more recognized in younger patients (≤50 y.o.)[OR: 1.88, 95% confidence interval (95% CI): 1.17–3.01, P = 0.01]; cancer types were defined by the AII criteria (OR: 7.30, 95% CI: 3.88–13.72, P < 0.0001) and the rB guidelines (OR: 3.06, 95% CI: 1.24–6.95, P = 0.005). The incidence of MSI-H was nearly ten times as often in cancers in LS-suspected patients (33.3%, 74 of 222) than in those in which MSI was analyzed for oncological purposes (3.1%, 24 of 778) (P < 0.0001). Within the factors considered statistically significant by univariate analysis, LS-related cancer types categorized by AII criteria (OR: 9.56, 95% CI: 4.09–28.05, P < 0.0001) and cases who underwent MSI for the diagnosis of LS (OR: 15.01, 95% CI: 8.91–26.17, P < 0.0001) were signified by multivariate analysis (Table 3).
Factors associated with MSI-H in colorectal cancers
In total, MSI-H was recognized in 13.7% (64/466) of CRCs and was significantly more recognized in the CRCs of younger patients (≤50 y.o.) (OR: 2.11, 95% CI: 1.17–3.82, P = 0.02) meeting the AII criteria (OR: 5.96, 3.00–11.87, P < 0.0001) and rB guidelines (OR: 3.66, 95%CI: 1.93–6.94, P < 0.0001) than in the other patients (Table 4). Similarly, CRCs in patients with increasing numbers of relatives with a history of cancer showed high risks of MSI-H. The ORs of family histories of rB guideline-defined LS cancers showed higher values compared with those of family histories of any cancer (Table 4). CRCs located in the right side of the colon (OR: 4.88, 95% CI: 2.80–8.51, P < 0.0001), those diagnosed at an early stage (OR: 3.21, 95% CI: 1.55–6.65, P = 0.003), and synchronous and/or metachronous multiple CRCs (OR: 3.31, 95% CI: 1.70–6.47, P = 0.001) were also statistically significant factors of MSI-H. The incidence of MSI-H analyzed in genetic medicine (41.7%, 53/127) was more than ten times as often as that analyzed for oncological purposes (3.2%, 11 of 339) (P < 0.0001). Within the statistically significant factors analyzed by the univariate test, CRC cases in first-degree relatives (FDRs)(OR: 9.98, 95% CI: 1.47–205.1, P = 0.046), CRCs located in the right side of the colon (OR: 5.21, 95% CI: 2.61–10.81, P < 0.0001), and cases who underwent genetic counseling (OR: 24.98, 95% CI: 10.07–70.08, P < 0.0001) were determined as independent significant factors by multivariate analysis (Table 4).
MSI-H in endometrial cancer
Because the incidence of MSI-H was highest in ECs (26.7%, 18/74) (Table 2), we analyzed factors associated with MSI-H similar to those for CRCs. Incidence of MSI-H was significantly higher in genetic counseling group than in companion diagnostics group (45.2% vs. 13.6%, P = 0.003). Incidence of MSI-H showed a higher trend in younger patients (30% in ≤50 y.o. vs. 25.5% in > 50 y.o.) and cases meeting the AII criteria (42.9% in cases fulfilling AII criteria vs. 25% in the other cases); however, none of these statistics, including other family history analyses done in the CRC cases, reached significant values. Additionally, neither histological type or FIGO clinical stage showed an association with MSI-H; incidence of MSI-H was 27.2% (15/55) in endometrioid carcinoma and 25.0% (5/20) in other histological types of carcinoma (P = 1.000), and 28.6% (10/35) in FIGO I-II and 25.0% (10/40) in FIGO III-IV (P = 0.797).
Discussion
In the current study, we analyzed the MSI status of 1000 human cancers in a tertiary Japanese cancer center and examined the incidence of MSI-H in various cancers in association with several demographic and clinical factors. The results demonstrated a significantly higher incidence of MSI-H in the LS-related cancers categorized by the AII criteria but not by the rB guidelines, in younger patients (≤50 y.o.), and in patients who underwent genetic counseling rather than simple companion diagnostics. MSI status was not associated with other patient demographics, such as smoking, drinking, and hepatitis virus serum markers (Table 3). These data were informative as, so far, MSI data from a large number of cancer cases has not been fully reported in reference to family histories, particularly in Asian countries.
MSI status has recently been analyzed in a variety of cancers in Western countries by international genome projects [The Cancer Genome Atlas (TCGA) [22, 23]/International Cancer Genome Consortium (ICGC) [24]/Therapeutically Applicable Research to Generate Effective Treatments (TARGET) [22]] and as a part of precision medicine (e.g., Memorial Sloan Kettering-integrated mutation profiling of actionable cancer targets: MSK-IMPACT [8]). In these genome projects, the prevalence of MSI-H was highest in EC (28.3% [25]–31.4% [22]), followed by gastric (21.9% [25]), colon (19.7% [22]), rectal (5.7% [22]–9.2% [25]), adrenocortical (4.3% [22]–5.4% [25]), esophageal (3.3% [25]), and ovarian cancers (3.2% [25]). MSK-IMPACT [8], which focuses on the more advanced stages of cancers, demonstrated relatively lower incidence; however, the data combined MSI-low (MSI-L) with MSI-H: 29.8% in small intestine cancer, 22.7% in EC, 16.6% in CRC, 7.8% in esophageal cancer, and 5.0% in gastric cancer. These data trends resemble the current data in overall and in companion diagnostics, respectively, although the current data showed a trend with lower incidence (Table 2). Generally, MSI in LS-related cancers has been reported in lower frequencies in Asian countries; for example, 17.3–25.7% [26,27,28] in EC, 4.3–10.0% in CRC [26, 29,30,31], and 2.3–9.3% in gastric cancer [26, 29, 32], suggesting an ethnic deviation. This is also reflected in the lower incidences of LS in Asian countries (2.9% [33]–4.4% [28] in EC and 0.6% [34]–0.7% [35] in CRC).
Non-LS-related cancers, such as cervical and skin cancer and NEC, showed a significantly lower incidence of MSI-H (3.8%) compared with the LS (rB)-related cancer groups (10.9%)(P = 0.005) and the LS (AII)-related cancer group (15.6%)(P < 0.0001) (Table 2). This group showed a significantly lower incidence of personal and familial cancer histories than the LS-related cancer groups (Table 2), despite a significantly higher ratio of smoking (65%) and drinking (57%)(Table 1), suggesting that the majority of these cancers developed with chromosomal instability [36]. Furthermore, LS-related cancers categorized under the rB guidelines but not the AII criteria, such as gastric, pancreaticobiliary, and ovarian cancers and brain tumors showed significantly lower MSI-H incidence (1.7%) than the LS-related cancers defined in the AII criteria (15.6%)(P < 0.0001) (Table 2), which is also compatible with TCGA [22, 25]. This is despite the similar levels of patients’ personal histories and family histories of cancer between these two groups. For pancreaticobiliary cancers, the higher indication of ICI was expected because of their aggressive biological behavior and poor prognosis but much improved in cases with MSI-H and treated by ICI [37]. However, the current cases, including 25 familial pancreatic cancers and 2 familial biliary cancers, showed a very low MSI-H incidence (0.6–1.6%), similar to the low level of tumor mutation burden (0.5–2.2/Mb) demonstrated in our previous study [34]. In pancreatic and ovarian cancers, PARP inhibitors are effective when the patients harbor germline variants in the genes associated with homologous recombination pathways. In the K-ras wild-type pancreatic cancer cases, although in less than 10% of the cases, the mTOR inhibitors may have potential therapeutic importance since they often harbor RAS-MAPK pathway-activating alterations and elevated phosphorylation mTOR pathway proteins [38]. As the benefits from MSI companion diagnostics are limited in several cancer types, suitable molecular target agents should be selected by the specific genetic alterations detected in the cancer gene panel testing.
To date, the dMMR of CRCs has been analyzed in several studies. Although most of them were screened by MMR protein immunohistochemistry or by a partial combination with MSI, the concordance with MSI-H and loss of the MMR protein were reported to be very high in CRCs (> 99% [39] and κ = 0.81 [40]). When universal screening was conducted on CRCs, the incidence of dMMR varied in a small range by country [7.3% in Slovenia [41], 8.6% in Spain [42], 9.6–12.6% in the U.S. (similar in blacks, Hispanics and non-Hispanic whites) [40], 9.8% in France [43], 11.7% in Italy [44], 15.0% in Switzerland [45], 16.9% in Australia [46], and 4.3–10.0% in Asian countries [26, 29,30,31]]. dMMR is characteristically recognized in CRCs in younger patients [40, 44, 46], in multiple cancer cases [40], in the proximal colon [44], and with specific pathological features [47]; however, these findings were not always statistically significant, probably due to a low number of cases. The current 466 CRC cases, although not a universal series, showed a significantly higher incidence of MSI-H in cases meeting the AII criteria (OR: 5.91) and the rB guidelines (OR: 3.71), with increasing risk according to the number of family history of cancers, and in CRCs located in the right side of the colon (OR: 4.89), in early stage cancers (OR: 3.18), and in younger patients (≤50 y.o.)(OR: 1.97) (Table 4). With the reported knowledge of MSI-H CRCs in mind, we selected patients for genetic counseling, in whom we detected a significantly higher incidence of MSI-H (41.7%) compared with those who underwent a companion test (3.2%). We judge that this large difference is not dependent on the methodology of MSI testing between genetic medicine (using normal tissue DNA as a control) and companion diagnostics (tumor only) because tumor-only MSI analysis demonstrated a nearly perfect concordance with the standard method of measuring the quasi-monomorphic variation range of the PCR products of Promega microsatellite markers [48]. Younger age and family history in MSI-H cancer suggested the inherited predisposition of the CRC, or LS, existed in some proportion, hence the needs for the genetic counseling is emphasized.
In Japan, in December 2020, the national health insurance system was revised to support the analysis of MSI for surgically-resected advanced CRCs, in addition to unresected cases, to investigate the indication of ICI as adjuvant therapy. MSI testing was thus made available in ≥85% of surgically-resected and far-advanced CRCs [49]. Since 2018, the National Comprehensive Cancer Network (NCCN) guidelines recommend universal tumor screening using an MSI test or MMR immunohistochemistry in all newly diagnosed CRCs for detecting LS patients [50]. It is easily suggested that, with these nationwide policies, diagnoses of LS will increase in the near feature. With the current data in mind, other AII-defined cancers (EC and small intestine cancer) also need MSI testing. As of now, universal dMMR screening is not, at least not unanimously, thought to be cost-effective [51, 52]. Genetic medicine for cancer patients requires a sense of balance in mental, physical, temporal, and economic burdens on patients and needs to be conducted in more efficient ways to achieve systemic care of the patients and their families.
The current study had several limitations due to its retrospective design and being done in a single cancer center hospital. The study subjects were a mixture of patients who had undergone genetic medicine and companion diagnostics, and the ratio of such testing may differ by institution. Family histories were obtained from interviews with the patients and their families so that they may be lacking in detail, especially concerning onset age and exact cancer type, leading to the lower evaluation of cases meeting the AII criteria and the rB guidelines. The pathological evaluations of lymphocytic response around CRC [47] are excluded due to the biopsy specimens included in some proportion; therefore, fewer cases may have been evaluated as meeting the rB guidelines. Besides, a cancer of renal pelvis and ureter, one of LS-related cancers in the AII criteria, was not included in this study.
In conclusion, MSI-H was found to strongly deviate in LS-related cancers defined in the AII criteria with significant associations to personal and family cancer histories and younger age. LS screening needs to be performed in an efficient way in both genetic and precision medicine.
Availability of data and materials
The data analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MMR:
-
Mismatch repair
- MSI:
-
Microsatellite instability
- ICI:
-
Immune checkpoint inhibitor
- MSI-H:
-
High level of MSI
- dMMR:
-
Deficient DNA mismatch repair
- LS:
-
Lynch syndrome
- CRC:
-
Colorectal cancer
- y.o.:
-
Years old
- EC:
-
Endometrial cancer
- NEC:
-
Neuroendocrine carcinoma
- AII:
-
Amsterdam II
- rB:
-
Revised Bethesda
- MSS:
-
Microsatellite stability
- OR:
-
Odd’s ratio
- 95%CI:
-
95% confidence interval
- FDR:
-
First-degree relative
- SDR:
-
Second-degree relative
- TDR:
-
Third-degree relative
- TCGA:
-
The Cancer Genome Atlas
- ICGC:
-
International Cancer Genome Consortium
- TERGET:
-
Therapeutically Applicable Research to Generate Effective Treatments
- MSK-IMPACT:
-
Memorial Sloan Kettering-integrated mutation profiling of actionable cancer targets
- NCCN:
-
National Comprehensive Cancer Network
References
Schlotterer C. Genome evolution: are microsatellites really simple sequences? Curr Biol. 1998;8:R132–4.
Garrido-Ramos MA. Satellite DNA: An evolving topic. Genes (Basel). 2017;8:230.
Strand M, Prolla TA, Liskay RM, et al. Destabilization of tracts of simple repetitive DNA in yeast by mutations affecting DNA mismatch repair. Nature. 1993;365:274–6.
Petrelli F, Ghidini M, Ghidini A, et al. Outcomes following immune checkpoint inhibitor treatment of patients with microsatellite instability-high cancers: a systematic review and Meta-analysis. JAMA Oncol. 2020;6:1068–71.
Fountzilas E, Kurzrock R, Hiep Vo H, et al. Wedding of Molecular Alterations and Immune Checkpoint Blockade: Genomics as a Matchmaker. J Natl Cancer Inst. 2021;113:djab067 (in press).
Pinol V, Castells A, Andreu M, et al. Accuracy of revised Bethesda guidelines, microsatellite instability, and immunohistochemistry for the identification of patients with hereditary nonpolyposis colorectal cancer. JAMA. 2005;293:1986–94.
Umar A, Boland CR, Terdiman JP, et al. Revised Bethesda guidelines for hereditary nonpolyposis colorectal cancer (lynch syndrome) and microsatellite instability. J Natl Cancer Inst. 2004;96:261–8.
Latham A, Srinivasan P, Kemel Y, et al. Microsatellite instability is associated with the presence of lynch syndrome Pan-Cancer. J Clin Oncol. 2019;37:286–95.
Moller P, Seppala T, Bernstein I, et al. Cancer incidence and survival in lynch syndrome patients receiving colonoscopic and gynaecological surveillance: first report from the prospective lynch syndrome database. Gut. 2017;66:464–72.
Rizvi H, Sanchez-Vega F, La K, et al. Molecular determinants of response to anti-programmed cell death (PD)-1 and anti-programmed death-ligand 1 (PD-L1) blockade in patients with non-small-cell lung Cancer profiled with targeted next-generation sequencing. J Clin Oncol. 2018;36:633–41.
Carbone DP, Reck M, Paz-Ares L, et al. First-line Nivolumab in stage IV or recurrent non-small-cell lung Cancer. N Engl J Med. 2017;376:2415–26.
Gargiulo P, Della Pepa C, Berardi S, et al. Tumor genotype and immune microenvironment in POLE-ultramutated and MSI-hypermutated endometrial cancers: new candidates for checkpoint blockade immunotherapy? Cancer Treat Rev. 2016;48:61–8.
Akagi K, Oki E, Taniguchi H, et al. Real-world data on microsatellite instability status in various unresectable or metastatic solid tumors. Cancer Sci. 2021;112:1105–13.
Schrader KA, Cheng DT, Joseph V, et al. Germline variants in targeted tumor sequencing using matched Normal DNA. JAMA Oncol. 2016;2:104–11.
Deng G, Bell I, Crawley S, et al. BRAF mutation is frequently present in sporadic colorectal cancer with methylated hMLH1, but not in hereditary nonpolyposis colorectal cancer. Clin Cancer Res. 2004;10:191–5.
Nagasaka T, Sasamoto H, Notohara K, et al. Colorectal cancer with mutation in BRAF, KRAS, and wild-type with respect to both oncogenes showing different patterns of DNA methylation. J Clin Oncol. 2004;22:4584–94.
Toyota M, Ahuja N, Suzuki H, et al. Aberrant methylation in gastric cancer associated with the CpG island methylator phenotype. Cancer Res. 1999;59:5438–42.
Vasen HF, Moslein G, Alonso A, et al. Guidelines for the clinical management of lynch syndrome (hereditary non-polyposis cancer). J Med Genet. 2007;44:353–62.
Kanai Y, Nishihara H, Miyagi Y, et al. The Japanese Society of Pathology Guidelines on the handling of pathological tissue samples for genomic research: standard operating procedures based on empirical analyses. Pathol Int. 2018;68:63–90.
Kiyozumi Y, Matsubayashi H, Horiuchi Y, et al. Germline mismatch repair gene variants analyzed by universal sequencing in Japanese cancer patients. Cancer Med. 2019;8:5534–43.
Boland CR, Thibodeau SN, Hamilton SR, et al. A National Cancer Institute workshop on microsatellite instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 1998;58:5248–57.
Bonneville R, Krook MA, Kautto EA, et al. Landscape of Microsatellite Instability Across 39 Cancer Types. JCO Precis Oncol. 2017;1: PO.17.00073.
Hause RJ, Pritchard CC, Shendure J, et al. Classification and characterization of microsatellite instability across 18 cancer types. Nat Med. 2016;22:1342–50.
Fujimoto A, Fujita M, Hasegawa T, et al. Comprehensive analysis of indels in whole-genome microsatellite regions and microsatellite instability across 21 cancer types. Genome Res. 2020;30:334–46.
Cortes-Ciriano I, Lee S, Park WY, et al. A molecular portrait of microsatellite instability across multiple cancers. Nat Commun. 2017;8:15180.
Cui M, Li P, Mao Y, et al. Implication of microsatellite instability in Chinese cohort of human cancers. Cancer Manag Res. 2020;12:10287–95.
An HJ, Kim KI, Kim JY, et al. Microsatellite instability in endometrioid type endometrial adenocarcinoma is associated with poor prognostic indicators. Am J Surg Pathol. 2007;31:846–53.
Yoon SN, Ku JL, Shin YK, et al. Hereditary nonpolyposis colorectal cancer in endometrial cancer patients. Int J Cancer. 2008;122:1077–81.
Zang YS, Dai C, Xu X, et al. Comprehensive analysis of potential immunotherapy genomic biomarkers in 1000 Chinese patients with cancer. Cancer Med. 2019;8:4699–708.
Kumamoto K, Ishida H, Suzuki O, et al. Lower prevalence of lynch syndrome in colorectal cancer patients in a Japanese hospital-based population. Surg Today. 2016;46:713–20.
Arakawa K, Hata K, Kawai K, et al. Predictors for high microsatellite instability in patients with colorectal Cancer fulfilling the revised Bethesda guidelines. Anticancer Res. 2018;38:4871–6.
Huang SC, Ng KF, Yeh TS, et al. Subtraction of Epstein-Barr virus and microsatellite instability genotypes from the Lauren histotypes: combined molecular and histologic subtyping with clinicopathological and prognostic significance validated in a cohort of 1,248 cases. Int J Cancer. 2019;145:3218–30.
Takahashi K, Sato N, Sugawara T, et al. Clinical characteristics of lynch-like cases collaterally classified by lynch syndrome identification strategy using universal screening in endometrial cancer. Gynecol Oncol. 2017;147:388–95.
Kiyozumi Y, Matsubayashi H, Higashigawa S, et al. Role of tumor mutation burden analysis in detecting lynch syndrome in precision medicine: analysis of 2,501 Japanese Cancer patients. Cancer Epidemiol Biomark Prev. 2021;30:166–74.
Chika N, Eguchi H, Kumamoto K, et al. Prevalence of lynch syndrome and lynch-like syndrome among patients with colorectal cancer in a Japanese hospital-based population. Jpn J Clin Oncol. 2017;47:108–17.
Cancer genome atlas N. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–7.
Marabelle A, Le DT, Ascierto PA, et al. Efficacy of Pembrolizumab in patients with noncolorectal high microsatellite instability/mismatch repair-deficient Cancer: results from the phase II KEYNOTE-158 study. J Clin Oncol. 2020;38:1–10.
Cancer genome atlas research network. Electronic address aadhe, Cancer genome atlas research N. integrated genomic characterization of pancreatic ductal adenocarcinoma. Cancer Cell. 2017;32:185–203 e13.
Hissong E, Crowe EP, Yantiss RK, et al. Assessing colorectal cancer mismatch repair status in the modern era: a survey of current practices and re-evaluation of the role of microsatellite instability testing. Mod Pathol. 2018;31:1756–66.
Berera S, Koru-Sengul T, Miao F, et al. Colorectal tumors from different racial and ethnic minorities have similar rates of mismatch repair deficiency. Clin Gastroenterol Hepatol. 2016;14:1163–71.
Berginc G, Bracko M, Ravnik-Glavac M, et al. Screening for germline mutations of MLH1, MSH2, MSH6 and PMS2 genes in Slovenian colorectal cancer patients: implications for a population specific detection strategy of lynch syndrome. Familial Cancer. 2009;8:421–9.
Perez-Carbonell L, Ruiz-Ponte C, Guarinos C, et al. Comparison between universal molecular screening for lynch syndrome and revised Bethesda guidelines in a large population-based cohort of patients with colorectal cancer. Gut. 2012;61:865–72.
Canard G, Lefevre JH, Colas C, et al. Screening for lynch syndrome in colorectal cancer: are we doing enough? Ann Surg Oncol. 2012;19:809–16.
Urso E, Pucciarelli S, Agostini M, et al. Proximal colon cancer in patients aged 51-60 years of age should be tested for microsatellites instability. A comment on the revised Bethesda guidelines. Int J Color Dis. 2008;23:801–6.
Zumstein V, Vinzens F, Zettl A, et al. Systematic immunohistochemical screening for lynch syndrome in colorectal cancer: a single Centre experience of 486 patients. Swiss Med Wkly. 2016;146:w14315.
Brennan B, Hemmings CT, Clark I, et al. Universal molecular screening does not effectively detect lynch syndrome in clinical practice. Ther Adv Gastroenterol. 2017;10:361–71.
Jenkins MA, Hayashi S, O'Shea AM, et al. Pathology features in Bethesda guidelines predict colorectal cancer microsatellite instability: a population-based study. Gastroenterology. 2007;133:48–56.
Bando H, Okamoto W, Fukui T, et al. Utility of the quasi-monomorphic variation range in unresectable metastatic colorectal cancer patients. Cancer Sci. 2018;109:3411–5.
Nationwide Colorectal Cancer Registry (2000-2004). Edited by Japanese Society for Cancer of the Colon and Rectum & Japanese Society of Clinical Oncology: http://www.jsco-cpg.jp/guideline/13_siryou.html.
Gupta S, Provenzale D, Llor X, et al. NCCN guidelines insights: genetic/familial high-risk assessment: colorectal, version 2.2019. J Natl Compr Cancer Netw. 2019;17:1032–41.
Barzi A, Sadeghi S, Kattan MW, et al. Comparative effectiveness of screening strategies for lynch syndrome. J Natl Cancer Inst. 2015;107(4):djv005.
Erten MZ, Fernandez LP, Ng HK, et al. Universal versus targeted screening for lynch syndrome: comparing ascertainment and costs based on clinical experience. Dig Dis Sci. 2016;61:2887–95.
Acknowledgments
We sincerely thank to the FALCO biosystems for the MSI analysis.
Funding
None.
Author information
Authors and Affiliations
Contributions
HM performed acquisition and interpretation of data, drafting of manuscript, and genetic counseling. SH, YK, and YH peformed genetic counseling and statistical analysis. TO and KS made pathological diagnosis. HI, KI KH, YY, KI, TS, and HO performed endoscopic sampling and study suggestion. AT, TK, HS, HY TA, NM, HK did oncological managements. TS, HK, AS, NK, YH, YK, EB, MN, and SN performed surgery. MS provided molecular discussion. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional review board (IRB) of the Shizuoka Cancer Center ethically approved this study (IRB no. J2020–82), and all procedures were conducted in accordance with the Helsinki Declaration. All MSI tests were done with informed consent to the patients. As this study was a retrospective observation study of the clinical practice in Japan, informed consent was obtained using the opt-out approach according to the IRB policy.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Matsubayashi, H., Higashigawa, S., Kiyozumi, Y. et al. Microsatellite instability is biased in Amsterdam II-defined Lynch-related cancer cases with family history but is rare in other cancers: a summary of 1000 analyses. BMC Cancer 22, 73 (2022). https://doi.org/10.1186/s12885-022-09172-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09172-5