Abstract
Background
The ML18174 study, which showed benefits of bevacizumab (BEV) continuation beyond progression (BBP) for metastatic colorectal cancer (mCRC), excluded patients with first-line progression-free survival (PFS) shorter than 3 months. The present study was conducted to evaluate the efficacy of second-line chemotherapy after early disease progression during first-line chemotherapy containing bevacizumab.
Methods
The subjects of this study were mCRC patients who experienced disease progression < 100 days from commencement of first-line chemotherapy containing BEV initiated between Apr 2007 and Dec 2016. Second-line chemotherapy regimens were classified into two groups with and without BEV/other anti-angiogenic agents (BBP and non-BBP) and efficacy and safety were compared using univariate and multivariate analysis.
Results
Sixty-one patients were identified as subjects of this study. Baseline characteristics were numerically different between BBP (n = 37) and non-BBP (n = 25) groups, such as performance status (0–1/> 2/unknown: 89/8/3 and 56/40/4%), RAS status (wild/mutant/unknown: 32/54/16 and 76/16/8%). Response rate was 8.6% in BBP group and 9.1% in non-BBP group (p = 1.00). Median PFS was 3.9 months in BBP group and 2.8 months in non-BBP group (HR [95%CI]: 0.79 [0.46–1.34], p = 0.373, adjusted HR: 0.87 [0.41–1.82], p = 0.707). Median overall survival was 8.5 months in BBP group and 5.4 months in non-BBP group (HR 0.66 [0.38–1.12], p = 0.125, adjusted HR 0.53 [0.27–1.07], p = 0.078).
Conclusion
In mCRC patients who experienced early progression in first-line chemotherapy, second-line chemotherapy showed poor clinical outcomes regardless use of anti-angiogenic agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
For patients with unresectable metastatic colorectal cancer (mCRC), systemic chemotherapy is recognized as the standard treatment worldwide [1,2,3]. Cytotoxic doublet or triplet chemotherapy plus targeted agent, such as bevacizumab (BEV) or anti-epidermal growth factor receptor (EGFR) inhibitor, is recommended as the first-line chemotherapy [3]. After failure of chemotherapy with BEV as first-line treatment, two large observational studies suggested that BEV continuation beyond progression (BBP) might improve the prognosis [4, 5]. Since a randomized trial (ML18147) showed a survival benefit of BBP compared to chemotherapy alone in the second-line setting (Hazard ratio [HR], 0.81; 95% confidence interval [CI], 0.69–0.94; p = 0.0062) [6], it has been adopted as one of the standard treatment strategies in second-line chemotherapy for mCRC patients [3]. However, the ML18147 trial excluded mCRC patients whose progression-free survival (PFS) during first-line chemotherapy was less than 3 months, as well as those in whom progressive disease was observed later than 3 months after the last BEV administration, or those who were treated with first-line chemotherapy containing BEV for less than 3 months [6].
Antiangiogenic agents are generally considered less likely to induce drug-resistance than cytotoxic agents because antiangiogenic agents act mainly on endothelial cells rather than on tumor cells [7]. However, it is not known whether BBP would have clinical benefits for patients who experienced disease progression within 3 months during a first-line BEV-containing chemotherapy; this patient group may be intrinsically resistant to BEV.
Here, we conducted a multi-institutional retrospective study to evaluate the efficacy and safety of second-line chemotherapy with or without BEV/other anti-angiogenic agents after early disease progression within 3 months during first-line BEV-containing chemotherapy.
Methods
Patients
This multi-institutional retrospective study was conducted at 9 Japanese hospitals. The main selection criteria of the subjects were; histologically confirmed unresectable or recurrent mCRC, age > 18 years, PFS < 100 days (early disease progression) during first-line chemotherapy containing BEV in combination with doublet cytotoxic agents, fluoropyrimidine, and oxaliplatin or irinotecan, which was initiated from Apr 2007 to Dec 2016. Additionally, patients who were intolerant to the first-line chemotherapy containing BEV were excluded. This study was approved by all the participating institutional review boards. Because of the retrospective nature of this study, informed consent was not obtained from each patient.
Treatments
Patients were divided into the two groups according to the second-line chemotherapy regimens with or without BEV/other anti-angiogenic agents, and were subsequently described as subjects in the BBP and non-BBP groups, respectively. In the BBP group, patients received cytotoxic agents with BEV at 2.5 mg/kg per week (5.0 mg/kg every 2 weeks or 7.5 mg/kg every 3 weeks). In the non-BBP group, patients received single or doublet cytotoxic agents with or without anti- EGFR antibody, or anti-EGFR antibody alone.
Evaluations
Tumor responses were evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1. Toxicity was assessed using the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. PFS was defined as the time from the initiation of second-line chemotherapy to disease progression or death from any cause, and was censored at the last visit of patients surviving without documented disease progression. Overall survival (OS) was defined as time from the initiation of the second-line chemotherapy to death or censored at the last visit of surviving patients.
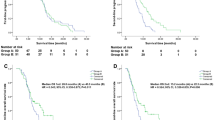
Survival curves for PFS and OS were estimated by the Kaplan-Meier method and confidence intervals (CI) were calculated based on the Greenwood formula. The confidence intervals of median survival time were calculated using the Brookmeyer-Crowley method. Hazard ratio (HR) and adjusted HR were obtained using Cox regression models with well-known prognostic factors (performance status [PS]), alkaline phosphatase (ALP), white blood cells (WBC), the number of metastatic organ sites [8], RAS status [9,10,11], sidedness [12,13,14] in multi-variate analysis. P-value < 0.05 as determined using the two-tailed test was considered to be significant. SAS version 9.4 was used for all statistical analysis.
Results
Patient characteristics
A total of 62 patients across 9 institutions were identified as the subjects of this study. According to the second-line chemotherapy regimens, 37 and 25 patents were classified into the BBP and non-BBP groups, respectively. The patients’ baseline characteristics are summarized in Table 1. In the BBP group, 33 patients (89.2%) were PS ≤1, 11 patients (32.4%) had KRAS/RAS wildtype, and 8 patients (21.6%) had peritoneal metastasis. In the non-BBP group, 14 patients (56.0%) were PS ≤1, and 19 patients (76.0%) had KRAS/RAS wild type, and 12 patients (48.0%) had peritoneum metastasis. There were no significant differences in age, sex, primary tumor location, disease status, number of metastatic organ sites or the first-line chemotherapy regimens between the two groups. Among the patients with measurable lesions, the best responses without confirmation in the first-line chemotherapy were stable disease in 6 patients (16.2%) and progressive disease in 29 (78.4%) of the BBP group and stable disease was seen in 6 (27.2%) patients and progressive disease was observed in 15 patients (68.2%) of the non-BBP group.
Second-line regimens
The regimens in the second-line chemotherapy are shown in Table 2. All patients in the BBP group received doublet chemotherapy plus BEV, while 16 (64%) and 9 (36%) patients in the non-BBP group were treated with anti-EGFR antibody-containing regimens or cytotoxic agents alone.
Efficacy
Two patients in the BBP group and three patients in the non-BBP group did not have measurable lesions. Among the patients with measurable lesions, the objective response and disease control rates were 8.6% (n = 3) and 51.4% in the BBP group and 9.1% (n = 2) and 36.4% in the non-BBP group (Table 2). With the median follow-up time was 6.2 months, median PFS was 3.9 months (95%CI: 2.3–5.5) in the BBP group, and 2.8 months (95%CI: 1.1–4.0) in the non-BBP group (HR [95%CI]: 0.79 [0.46–1.34], p = 0.373, adjusted HR [95%CI]: 0.87 [0.41–1.82], p = 0.707, Fig. 1, Table S1). Median OS was 8.5 months (95%CI: 4.9–9.7) in the BBP group, and 5.4 months (95%CI: 2.1–6.9) in the non-BBP group (HR [95%CI]: 0.66 [0.38–1.12], p = 0.125, adjusted HR [95%CI]: 0.53 [0.27–1.07], p = 0.078, Fig. 1, Table S1). PFS of three patients in the BBP group who had a partial response in the second line chemotherapy were as short as 3.0, 4.5, 9.3 months and OS were 6.4 9.5 20.5 months. In contrast, PFS of two responders in the non-BBP group were 8.0 and 9.9 months and OS were 13.9 months and 14.9 months. With regard to the patients who received combination chemotherapy with anti-EGFR antibody in the non-BBP group, the objective response and disease control rates were 22.2% (2/9 patients) and 44.4% (4/9 patients), while median PFS and OS were 3.3 months (95%CI: 0.7–7.3) and 4.9 months (95%CI: 1.2–13.9).
Treatment after second-line chemotherapy
All subsequent treatments after the second-line chemotherapy in both groups are shown in Table 3. In the BBP group, 21 patients (56.8%) had subsequent treatments after the second-line chemotherapy: irinotecan-based chemotherapy in 17 patients (45.9%) and TAS-102 in 15 patients (40.5%), while in the non-BBP group, only 8 patients (32.0%) received subsequent treatments: regorafenib in 2 patients (8.0%), anti-EGFR antibody monotherapy in 2 patients (8.0%). irinotecan-based chemotherapy in 2 patients (8.0%).
Safety
Adverse events during second-line chemotherapy are summarized in Table 4. The most common grade 3 or 4 adverse event was neutropenia in both the BBP and the non-BBP groups. In the BBP group, one patient (2.7%) had grade 3 febrile neutropenia. In the non-BBP group, 4 patients (16.0%) had grade 3–4 anemia and 2 patients (8.0%) had grade 3–4 anorexia. In the BBP group, hemorrhage, hypertension, proteinuria, embolism, and gastrointestinal perforation were rare.
Discussion
BBP has been recognized as a standard second-line treatment following the results of the ML18147 trial, in which median PFS and OS were 5.7 months and 11.2 months, respectively [6]. On the other hand, median PFS and OS when anti-EGFR antibody plus chemotherapy in the second-line treatment were 4.0–6.0 months and 10.7–16.2 months, respectively [15,16,17]. In this study, median PFS and OS were not significantly different between the BBP and non-BBP groups. Indeed, compared with the reported results of the randomized controlled trials of BBP and anti-EGFR antibody, the subjects in our study showed poor clinical outcomes regardless of the treatment strategy, BBP or non-BBP. In a randomized phase III trial for mCRC, the proportion of patients with early disease progression during first-line chemotherapy was only 3–4% [18]; this is similar to the incidence of early progression (4.1%) in patients allocated to the BEV-containing arm in the TRICOLORE trial [19]. Although the number of patients with early disease progression during BEV-containing first-line chemotherapy is small, we believe it is important to develop effective therapies for these patients.
There were substantial differences in patients’ backgrounds between the two groups in the present study. The proportion of patients with PS ≥2 was higher in the non-BBP group (40.0%) than in the BBP group (8.1%). All patients in the BBP group received doublet plus BEV, while only 8 patients (32.0%) in the non-BBP group received doublet plus a targeted agent. The proportion of patients with RAS wild type was higher in the non-BBP group (76.0%) than in the BBP group (32.4%), and 16 patients (64%) in the non-BBP group received chemotherapy containing anti-EGFR antibody, which is recommended by current guidelines [1,2,3]. These differences in patients’ conditions seem to have influenced the selection of chemotherapy regimens.
In this study, the adjusted HR for OS when BBP and non-BBP groups were compared was 0.66, while the adjusted HR for PFS was 0.87. However, in addition to the differences in patient’s background and chemotherapy regimens, there was a substantial difference in the proportion of patients receiving subsequent chemotherapy. Given these issues, it was challenging to compare efficacy between the two groups, especially for OS, even after adjusting for patient backgrounds with multivariate analysis. Limited to the patients who received standard treatment strategy both in the first- and second line chemotherapy, all 37 patients in the BBP group and 12 of 25 patients in the non-BBP group received combination chemotherapy of cytotoxic agents and molecular target agents. Among these 49 patients, there were some differences in PS and KRAS/RAS status: proportions of PS 0–1? 89.258.3%, and those of KRAS/RAS wild type 32.4 and 100% in BBP and non BBP groups. These poor condition of these 12 patients of the non-BBP group might result in short mPFS and mOS as 3.3 and 4.9 months. Thus, it is still difficult to compared between BBP and non-BBP even along with the standard treatment strategy. Therefore, it remains unclear whether BBP or non-BBP is the preferable treatment option for patients with early disease progression during first-line chemotherapy containing BEV.
As for the response to chemotherapy, the response rate (8.6%) in the BBP group of this study was very similar to that (5.4%) of the BBP group in the ML18147 trial; however, the disease control rate (51.4%) in our study was lower than that (68%) in ML18147 [6]. Conversely, the response rate in the non-BBP group in our study was slightly higher (9.1%) than in the BBP group, but the disease control rate lower at 36.4%. Based on the survival analysis, we think it is reasonable to speculate that many of the subjects in this study would have had tumors that were resistant to the agents used in second-line chemotherapy, regardless of whether they were in the BBP or non-BBP group. However, survival analysis results by best response in this study showed that better response in the second-line chemotherapy might lead to better clinical outcomes. It is considered that response/disease control in the second-line chemotherapy may be important to improve clinical outcomes of patients even with early disease progression in the first-line chemotherapy.
Biomarker analysis of the CALGB/SWOG 80405 trial showed that low baseline levels of serum VEGF-D were specifically predictive of longer PFS in patients who received FOLFOX plus BEV than in patients who received FOLFOX plus cetuximab as the first-line chemotherapy [20]. BEV suppresses tumor angiogenesis mainly by inhibiting the binding of VEGF-A to VEGFR-1/2. However, VEGF-D also binds to VEGFR-2 and promotes tumor angiogenesis, and therefore BEV efficacy may be poor in patients with high levels of serum VEGF-D. In addition to VEGF-D, biomarker studies suggest that VEGF-A [21] and PIGF [21, 22] might be associated with the efficacy of anti-angiogenic therapy. Therefore, we speculate that elevated activity of angiogenic pathway might be responsible for BEV resistance of some subjects in this study.
RAM and AFL are also anti-angiogenic agents that inhibit the VEGF pathway by mechanisms different from BEV [23, 24]. RAM is a fully human IgG-1 monoclonal antibody, and exerts its antitumor activity by binding to the VEGFR-2 extracellular domain [24, 25]. Subgroup analysis of the RAISE study showed that RAM was efficacious in patients with high levels of VEGF-D [26]. In addition, subgroup analysis of patients with first-line TTP < 6 months in the RAISE trial showed that median OS was 10.4 months versus 8.0 months (HR [95%CI]: 0.86 [0.64–1.13], p = 0.2759), and median PFS was 5.2 months versus 2.9 months (HR [95%CI]: 0.68[0.52–0.89], p = 0.0042) [27]. Actually in the present study, one patient who received FOLFIRI plus ramucirumab showed very favorable PFS and OS (Table S1). We suggest that future clinical researches should evaluate the benefits of switching to RAM for patients with high levels of VEGF-D who experience early progression during first-line chemotherapy containing BEV. AFL is a recombinant fusion protein that prevents VEGF-A, VEGF-B, and PIGF-1 from binding to their cognate receptors [23]. Subgroup analysis of patients with first-line TTP < 3 months in the VELOUR trial showed that median OS was 11.9 months in the AFL plus FOLFIRI group versus 9.8 months in placebo plus FOLFIRI (HR, 0.63), while median PFS was 7.0 months versus 3.9 months (HR, 0.55) [28]. These data, which are based on randomized trials, suggest that switching to other anti-angiogenic agents during second-line chemotherapy may be a treatment option for patients who had early disease progression during first-line BEV-containing chemotherapy. However, in the VELOUR trial, only 30.4% of patients received BEV as part of the first-line chemotherapy [28], whereas the number of patients who had TTP < 3 months during first-line chemotherapy and who received BEV containing chemotherapy was not clear. Further studies will be needed to test the validity of such an approach.
As for the non-BBP group in this study, it is very difficult to compare their response and disease control rates with those previously reported, because the non-BBP group contained various kinds of chemotherapy regimens. The majority of the patients who received combination chemotherapy with anti-EGFR antibody had a poor prognosis. Moreover, in a previous retrospective analysis, the efficacy of anti-EGFR antibody-containing treatments as second- or third-line chemotherapy was poorer in patients who previously received BEV than in patients without prior BEV [29]. It has been reported that patients who received a BEV-containing regimen had higher levels of VEGF-A than the patients without prior BEV [29]. Furthermore, experiments with CRC cell lines suggest that high levels of VEGF-A induce VEGFR-2- and STAT-3-dependent resistance to cetuximab [29]. Another preclinical study suggested that BEV-resistant CRC cells had higher levels of VEGF due to upregulation of the hypoxia induced factor (HIF)-VEGF signaling pathway [30]. We note that HIFs can also activate EGFR and the associated downstream signal transduction pathways [31]. These molecular mechanisms might underlie the poor efficacy of anti-EGFR antibody-containing regimens that we observed in this study. We suggest that the identification of biomarkers that aid selection of anti-EGFR antibody-containing chemotherapy for patients who experience early progression during first-line chemotherapy containing BEV should be prioritized.
This study has some limitations. First, it is a small retrospective study, leading to some bias in patients’ characteristics such as PS and selection of chemotherapy based on RAS mutational status. These imbalances might affect the survival outcomes in this study, which might not be adjusted even by multivariate analysis. Additionally, we retrospectively collected data during 10 years because of small population, and clinical practice such as mitigations, co-medications, monitoring and treatment of side effects and diagnostic methods changed during these 10 years. These factors might have some impact on the results of this study. Secondly, in some patients, we could not collect information of BRAF mutational status (unknown: n = 46); these genes are well-known prognostic factors in colorectal cancer [32,33,34]. Finally, we could not perform antiangiogenic biomarker analysis of molecules such as VEGF-D and A [20, 26] due to retrospective study design. As a consequence of these limitations, the question whether BEV continuation beyond progressions or not is more favorable cannot be answered by the results of this study. However, to the best of our knowledge, this is the first report that clarifies the efficacy and safety of BBP or non-BBP strategies as second-line chemotherapy for mCRC patients with early disease progression during first-line BEV-containing chemotherapy.
Conclusions
For mCRC patients with early disease progression in the first-line setting, the efficacy of second-line chemotherapy is modest, regardless of whether BBP or other strategies have been employed. The optimal treatment for these mCRC patients, BBP or other strategies could not be clarified. To improve clinical outcomes of these patients, new treatment strategies are warranted.
Availability of data and materials
The datasets generated during this study are not publicly available due to ethical restrictions, but these are available from the corresponding author on reasonable request.
Abbreviations
- AFL:
-
Aflibercept
- ALP:
-
Alkaline phosphatase
- BEV:
-
Bevacizumab
- BBP:
-
BEV continuation beyond progression
- CI:
-
Confidence interval
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- EGFR:
-
Epidermal growth factor receptor
- HIF:
-
Hypoxia induced factor
- HR:
-
Hazard ratio
- mCRC:
-
Metastatic colorectal cancer
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- PS:
-
Performance status
- RAM:
-
Ramucirumab
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- WBC:
-
White blood cells
References
Van Custem E, Cervantes A, Adam R, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27(8):1386–422. https://doi.org/10.1093/annonc/mdw235.
National Comprehensive Care Network. Clinical practice guidelines in oncology (NCCN guideline®). http://www.nccn.org/professionals/physician_gls/default.aspx (Accessed 13 June 2019).
Yoshino T, Arnold D, Taniguchi H, Pentheroudakis G, Yamazaki K, Xu RH, et al. Pan-Asian adapted ESMO consensus guidelines for the management of patients with metastatic colorectal cancer: a JSMO-ESMO initiative endorsed by CSCO, KACO, MOS, SSO and TOS. Ann Oncol. 2018;29(1):44–70. https://doi.org/10.1093/annonc/mdx738.
Grothey A, Sugrue MM, Purdie DM, Dong W, Sargent D, Hedrick E, et al. Bevacizumab beyond first progression is associated with prolonged overall survival in metastatic colorectal cancer: results from a large observational cohort study (BRiTE). J Clin Oncol. 2008;26(33):5326–34. https://doi.org/10.1200/JCO.2008.16.3212.
Grothey A, Flick ED, Cohn AL, Bekaii-Saab TS, Bendell JC, Kozloff M, et al. Bevacizumab exposure beyond first disease progression in patients with metastatic colorectal cancer: analyses of the ARIES observational cohort study. Pharmarcoepidemiol Drug Saf. 2014;23(7):726–34. https://doi.org/10.1002/pds.3633.
Bennoua J, Sastre J, Arnold D, et al. Continuation of bevacizumab after progression in metastatic colorectal cancer (ML18147): a randomised phase 3 trial. Lancet Oncol. 2013;14(1):29–37. https://doi.org/10.1016/S1470-2045(12)70477-1.
Kerbel RS. Inhibition of tumor angiogenesis as a strategy to circumvent acquired resistance to anti-cancer therapeutic agents. Bioessays. 1991;13(1):31–6. https://doi.org/10.1002/bies.950130106.
Köhne CH, Cunningham D, Di Costanzo F, et al. Clinical determinants of survival in patients with 5-fluorouracil-based treatment for metastatic colorectal cancer: results of a multivariate analysis of 3825 patients. Ann Oncol. 2002;13(2):308–17. https://doi.org/10.1093/annonc/mdf034.
De Roock W, Jonker DJ, Di Nicolantonio F, et al. Association of KRAS p.G13D mutation with outcome in patients with chemotherapy-refractory metastatic colorectal cancer treated with cetuximab. JAMA. 2010;304(16):1812–20. https://doi.org/10.1001/jama.2010.1535.
Tejpar S, Celik I, Schlichting M, Sartorius U, Bokemeyer C, van Cutsem E. Association of KRAS G13D tumor mutations with outcome in patients with metastatic colorectal cancer treated with first-line chemotherapy with or without cetuximab. J Clin Oncol. 2012;30(29):3570–7. https://doi.org/10.1200/JCO.2012.42.2592.
De Roock W, Claes B, Bernasconi D, et al. Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol. 2010;11(8):753–62. https://doi.org/10.1016/S1470-2045(10)70130-3.
Venook AP, Niedzwiecki D, Innocenti F, et al. Impact of primary (1°) tumor location on overall survival (OS) and progression-free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC): Analysis of CALGB/SWOG 80405 (Alliance). J Clin Oncol. 016;34(Suppl):3504.
Venook AP, Ou FS, Lenz HJ, et al. Primary tumor location as an independent prognostic marker from molecular features for overall survival in patients with metastatic colorectal cancer: analysis of CALGB/SWOG 80405 (Alliance). J Clin Oncol. 2017;35(Suppl):3503.
Arnold D, Lueza B, Douillard JY, Peeters M, Lenz HJ, Venook A, et al. Prognostic and predictive value of primary tumour side in patients with RAS wild-type metastatic colorectal cancer treated with chemotherapy and EGFR directed antibodies in six randomized trials. Ann Oncol. 2017;28(8):1713–29. https://doi.org/10.1093/annonc/mdx175.
Sobrero AF, Maurel J, Fehrenbacher L, Scheithauer W, Abubakr YA, Lutz MP, et al. EPIC: phase III trial of cetuximab plus irinotecan after fluoropyrimidine and oxaliplatin failure in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26(14):2311–9. https://doi.org/10.1200/JCO.2007.13.1193.
Peeters M, Price TJ, Cervantes A, Sobrero AF, Ducreux M, Hotko Y, et al. Randomized phase III study of panitumumab with fluorouracil, leucovorin, and irinotecan (FOLFIRI) compared with FOLFIRI alone as second-line treatment in patients with metastatic colorectal cancer. J Clin Oncol. 2010;28(31):4706–13. https://doi.org/10.1200/JCO.2009.27.6055.
Shitara K, Yonesaka K, Denda T, Yamazaki K, Moriwaki T, Tsuda M, et al. Randomized study of FOLFIRI plus either panitumumab or bevacizumab for wild-type KRAS colorectal cancer-WJOG 6210G. Cancer Sci. 2016;107(12):1843–50. https://doi.org/10.1111/cas.13098.
Yamazaki K, Nagase M, Tamagawa H, Ueda S, Tamura T, Murata K, et al. Randomized phase III study of bevacizumab plus FOLFIRI and bevacizumab plus mFOLFOX6 as first-line treatment for patients with metastatic colorectal cancer (WJOG4407G). Ann Oncol. 2016;27(8):1539–46. https://doi.org/10.1093/annonc/mdw206.
Yamada Y, Denda T, Gamoh M, Iwanaga I, Yuki S, Shimodaira H, et al. S-1 and irinotecan plus bevacizumab versus mFOLFOX6 or CapeOX plus bevacizumab as first-line treatment in patients with metastatic colorectal cancer (TRICOLORE): a randomized, open-label, phase III, noninferiority trial. Ann Oncol. 2018;29(3):624–31. https://doi.org/10.1093/annonc/mdx816.
Nixon A, Sibley A, Hatch AJ, et al. Blood-based biomarkers in patients (pts) with metastatic colorectal cancer (mCRC) treated with FOLFOX or FOLFIRI plus bevacizumab (Bev), cetuximab (Cetux), or bev plus Cetux: Results from CALGB 80405 (Alliance). J Clin Oncol. 2016;34(Suppl):3597.
Van Cutsem E, Paccard C, Chiron M, et al. Impact of Prior Bevacizumab Treatment on VEGF-A and PlGF Levels and Outcome Following Second-Line Aflibercept Treatment: Biomarker Post Hoc Analysis of the VELOUR Trial. Clin Cancer Res. 2020;26(3):717–25.
Lieu CH, Tran H, Jiang ZQ, Mao M, Overman MJ, Lin E, et al. The association of alternate VEGF ligands with resistance to anti-VEGF therapy in metastatic colorectal cancer. PLoS One. 2013;8(10):e77117. https://doi.org/10.1371/journal.pone.0077117.
Tang PA, Moore MJ. Aflibercept in the treatment of patients with metastatic colorectal cancer: latest findings and interpretations. Ther Adv Gastroenterol. 2013;6(6):459–73. https://doi.org/10.1177/1756283X13502637.
Bruns CJ, Liu W, Davis DW, Shaheen RM, McConkey DJ, Wilson MR, et al. Vascular endothelial growth factor is an in vivo survival factor for tumor endothelium in a murine model of colorectal carcinoma liver metastases. Cancer. 2000;89(3):488–99. https://doi.org/10.1002/1097-0142(20000801)89:3<488::AID-CNCR3>3.0.CO;2-X.
Tonra JR, Tomasek J, Yong CJ, et al. Synergistic antitumor effects of combined epidermal growth factor receptor and vascular endothelial growth factor receptor-2 targeted therapy. Clin Cancer Res. 2006;12(7):2197–207. https://doi.org/10.1158/1078-0432.CCR-05-1682.
Tabernero J, Hozak RR, Yoshino T, Cohn AL, Obermannova R, Bodoky G, et al. Analysis of angiogenesis biomarkers for ramucirumab efficacy in patients with metastatic colorectal cancer from RAISE, a global, randomized, double-blind, phase III study. Ann Oncol. 2018;29(3):602–9. https://doi.org/10.1093/annonc/mdx767.
Obermannova R, Van Custem E, Yoshino T, et al. Subgroup analysis in RAISE: a randomized, double-blind phase III study of irinotecan, folinic acid, and 5-fluorouracil (FOLFIRI) plus ramucirumab or placebo in patients with metastatic colorectal carcinoma progression. Ann Oncol. 2016;27(11):2082–90. https://doi.org/10.1093/annonc/mdw402.
Van Custem E, Joulain F, Hoff PM, et al. Aflibercept plus FOLFIRI vs. placebo plus FOLFIRI in second-line metastatic colorectal Cancer: a post hoc analysis of survival from the phase III VELOUR study subsequent to exclusion of patients who had recurrence during or within 6 months of completing adjuvant Oxaliplatin-based therapy. Target Oncol. 2016;11(3):383–400. https://doi.org/10.1007/s11523-015-0402-9.
Derangère V, Fumet JD, Boidot R, Bengrine L, Limagne E, Chevriaux A, et al. Does bevacizumab impact anti-EGFR therapy efficacy in metastatic colorectal cancer? Oncotarget. 2016;9(8):9309–21. https://doi.org/10.18632/oncotarget.7008.
Mésange P, Poindessous V, Sabbah M, Escargueil AE, de Gramont A, Larsen AK. Intrinsic bevacizumab resistance is associated with prolonged activation of autocrine VEGF signaling and hypoxia tolerance in colorectal cancer cells and can be overcome by nintedanib, a small molecule angiokinase inhibitor. Oncotarget. 2014;5(13):4709–21. https://doi.org/10.18632/oncotarget.1671.
Keith B, Johnson RS, Simon MC. HIF1α and HIF2α: sibling rivalry in hypoxic tumour growth and progression. Nat Rev Cancer. 2011;12(1):9–22. https://doi.org/10.1038/nrc3183.
Van Custem E, Kohne CH, Lang I, et al. Cetuximab plus irinotecan, fluorouracil, and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumor KRAS and BRAF mutation status. J Clin Oncol. 2012;29:2011–9.
Bokemeyer C, Bondarenko I, Hartmann JT, de Braud F, Schuch G, Zubel A, et al. Efficacy according to biomarker status of cetuximab plus FOLFOX-4 as first-line treatment for metastatic colorectal cancer: the OPUS study. Ann Oncol. 2011;22(7):1535–46. https://doi.org/10.1093/annonc/mdq632.
Peeters M, Oliner KS, Parker A, Siena S, van Cutsem E, Huang J, et al. Massively parallel tumor multigene sequencing to evaluate response to panitumumab in a randomized phase III study of metastatic colorectal cancer. Clin Cancer Res. 2013;19(7):1902–12. https://doi.org/10.1158/1078-0432.CCR-12-1913.
Acknowledgments
We thank WJOG for giving us the opportunity to connect the collaborating institutions. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
All authors were involved design of this study. SY contributed to coordinating this study and writing the first manuscript. KN contributed to analyzing the data of this study. TK, SM, MK, YT, NI, KK, YY, AM, KY, TM1, TE, TT, TN, HO, TM2 contributed to collecting the data at each hospital and reviewing this manuscript. NB contributed to supervising this study and revising this manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by all the participating institutional review boards (National Cancer Center:2017–494, Shizuoka Cancer Center: T30–21–30-1-5, Aichi Cancer Center:2018–1-036, National Hospital Organization Kyushu Cancer Center:2018–8, Tonan Hospital:341, St. Marianna University School of Medical Hospital:4005, Keiyukai Sapporo Hospital:H30–4, University of Tsukuba:H30–234, Japan Community Healthcare Organization Kyushu Hospital:568). It was determined to be a retrospective study of de-identified data, and thus was determined to be exempt from requiring written informed consent.
Consent for publication
This manuscript contains no additional individual person’s data.
Competing interests
NI and MK, KK, YY, TT, HO, TM2 have nothing to declare. SY has received honoraria from Ono Pharmaceuticals. KN has received honoraria from Pfizer R&D Japan G.K. TK has received honoraria from Chugai, Takeda Pharmaceutical, Taiho. SM has received research funding and honoraria from Taiho, honoraria from Takeda Pharmaceutical, Ono Pharmaceuticals. YT has received honoraria from Bayer, Merck Serono, Lilly, Chugai, Taiho, Ono Pharmaceuticals, Takeda Pharmaceutical, Medicon, Sawai Pharmaceutical. AM has received honoraria from Lilly, Chugai, Takeda Pharmaceutical. KY has received research funding and honoraria from Taiho, honoraria from Chugai, Daiichi Sankyo, Yakult Honsha, Takeda Pharmaceutical, Bayer, Merck Serono, Lilly, Sanofi, Ono Pharmaceuticals, MSD, Bristol-Myers Squibb. TM1 has received research funding from Ono Pharmaceuticals, MSD, Daiichi Sankyo, and honoraria from Takeda Pharmaceutical, Chugai, Merck Bio Pharma, Taiho, Bayer, Lilly, Yakult Honsha, Sanofi, Ono Pharmaceuticals. TE has received research funding from MSD, Novartis, Ono Pharmaceuticals, Daiichi Sankyo, Astellas, Astellas Amgen Biopharma, BeiGene, Pierre Fabre Medicament, Ignyta, Array BioPharma, Merck Serono, Dainippon Sumitomo, Taiho, honoraria from Chugai, Lilly. TN has received research funding from Chugai, Takeda Pharmaceutical, Sanofi, Daiichi Sankyo, Lilly, Nippon Kayaku, Ono Pharmaceuticals, MSD, Astellas, Sumitomo Dainippon Pharma, Eisai, Solasia Pharma, honoraria from Mochida Pharmaceutical, Celltrion Healthcare Japan, Taiho, Merck Serono, Chugai, Takeda Pharmaceutical, Sanofi, Daiichi Sankyo, Lilly, Nippon Kayaku, Ono Pharmaceutical, MSD, Sawai Pharmaceutical, Bayer, Bristol-Myers Squibb, Teijin Pharma, Pfizer, Novartis, Yakult Honsha, Nipro Co. NB has received research funding from Taiho, Ono Pharmaceuticals, honoraria from Taiho, Ono Pharmaceuticals and Bristol-Myers Squibb.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1S.
Progression-free survival and overall survival by second-line chemotherapy regimen.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yamamoto, S., Nagashima, K., Kawakami, T. et al. Second-line chemotherapy after early disease progression during first-line chemotherapy containing bevacizumab for patients with metastatic colorectal cancer. BMC Cancer 21, 1159 (2021). https://doi.org/10.1186/s12885-021-08890-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-021-08890-6