Abstract
Background
Clinical effectiveness and safety data of pazopanib in patients with advanced or mRCC in real-world setting from Asia Pacific, North Africa, and Middle East countries are lacking.
Methods
PARACHUTE is a phase IV, prospective, non-interventional, observational study. Primary endpoint was the proportion of patients remaining progression free at 12 months. Secondary endpoints were ORR, PFS, safety and tolerability, and relative dose intensity (RDI).
Results
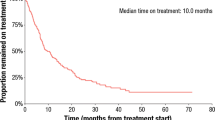
Overall, 190 patients with a median age of 61 years (range: 22.0–96.0) were included. Most patients were Asian (70%), clear-cell type RCC was the most common (81%), with a favourable (9%), intermediate (47%), poor (10%), and unknown (34%) MSKCC risk score. At the end of the observational period, 78 patients completed the observational period and 112 discontinued the study; 60% of patients had the starting dose at 800 mg. Median RDI was 82%, with 52% of patients receiving < 85%. Of the 145 evaluable patients, 56 (39%) remained progression free at 12 months, and the median PFS was 10 months (95% CI: 8.48–11.83). 19% of patients (21/109) were long-term responders (on pazopanib for ≥18 months). The best response per RECIST 1.1 was CR/PR in 24%, stable disease in 44%, and PD in 31%. Most frequent (> 10%) TEAEs related to pazopanib included diarrhoea (30%), palmar-plantar erythrodysesthesia syndrome (15%), and hypertension (14%).
Conclusions
Results of the PARACHUTE study support the use of pazopanib in patients with advanced or mRCC who are naive to VEGF-TKI therapy. The safety profile is consistent with that previously reported by pivotal and real-world evidence studies.
Similar content being viewed by others
Introduction
Pazopanib is an orally bioavailable adenosine triphosphate–competitive tyrosine kinase inhibitor (TKI) of vascular endothelial growth factor receptors (VEGFR) (1, 2, and 3), platelet-derived growth factor receptors (α and β), and c-Kit [1]. Pazopanib is approved by the Food and Drug Administration, European Medicines Agency, and other regulatory authorities as a monotherapy for patients with advanced renal cell carcinoma (RCC) and advanced soft tissue sarcomas [2, 3].
The efficacy of pazopanib has been demonstrated in two phase III randomised controlled trials [4, 5]. Pivotal phase III clinical trials are the best source of evidence for determining the efficacy of a treatment in a specific population; however, these studies cannot provide data for all possible clinical scenarios or disease characteristics. The real-world PRINCIPAL study demonstrated the effectiveness and safety of pazopanib in a routine clinical setting in patients with advanced or metastatic RCC [6]. Limited current knowledge on the use of pazopanib in routine clinical practice further highlights the need for real-world studies of pazopanib, especially for evaluating patients who have been under-represented in the registration trials.
PARACHUTE study aimed to describe the clinical effectiveness and safety of pazopanib in a real-world setting in patients with advanced or metastatic RCC who are naive to VEGFR-TKI therapy. This study was conducted across countries in Asia Pacific, North Africa, and Middle East regions, where data from registration trials were lacking or limited. The aim was to collect data from medical centres related to the management of patients treated with pazopanib for advanced or metastatic RCC.
Patients and methods
PARACHUTE, a phase IV, prospective, non-interventional, observational study, did not impose a therapeutic protocol, diagnosis/therapeutic interventions, or a strict visit calendar. Patients diagnosed with advanced or metastatic RCC of any histology who were treated according to local practices and who were treated for the first time with pazopanib were included. Patients were treated with pazopanib in accordance with the summary of product characteristics [7]. The study consisted of an observational period from baseline to month 12. Patients were allowed to participate in other interventional clinical studies. All patients provided informed consent, and the study was conducted in accordance with the International Conference on Harmonisation Good Clinical Practice guidelines, patient privacy requirements, and ethical principles outlined in the Declaration of Helsinki 2013.
The study was designed to enrol approximately 180 patients with advanced or metastatic RCC who were naive to VEGFR-TKI therapy in 15 countries across Asia Pacific, Middle East, and North Africa. The sample size was based on the conservative assumption of survival, i.e., by taking the lower limit of the confidence interval (CI) of the PRINCIPAL and VEG105192 studies, along with increasing the margin of error to 7.7% [4, 6]. Assuming 15% of the data was incomplete or censored before month 12 owing to reasons other than disease progression, the minimum sample size required based on a conservative assumption of a progression-free survival (PFS) of 38% with a 7.7% of margin of error was 180 patients [4]. The enrolment was competitive, with 35 centres participating in this study.
Patients aged ≥18 years with advanced or metastatic RCC who were about to start new treatment with pazopanib on study entry or had already started new treatment with pazopanib within 15 days before study entry based on the treating physician’s decision were eligible for the study. Prior cytokine therapy was allowed, but prior anti-VEGF therapy for RCC was not allowed.
Objectives and assessments
The primary objective of the study was to describe the clinical effectiveness of pazopanib in a real-world setting based on the proportion of patients remaining progression free at 12 months. Secondary objectives were to describe other clinical effectiveness factors for pazopanib: objective response rate (ORR) at 12 months, PFS, and response (ORR and progression-free response) based on the Memorial Sloan Kettering Cancer Center (MSKCC)/International Metastatic Renal Cell Carcinoma Database Consortium (IMDC) risk categories and age; gain information on treatment sequences; relative dose intensity (RDI) of pazopanib, collected in electronic case report forms; safety and tolerability of pazopanib; correlation of the RDI of pazopanib with its safety profile and treatment outcomes at 12 months. The exploratory objective of the study was to assess the proportion of patients who were long-term responders, i.e., those remaining progression-free for ≥18 months while receiving pazopanib treatment at the end of study (EOS).
The primary endpoint, i.e., the proportion of patients remaining progression-free at 12 months, was estimated along with the 95% CIs using the Kaplan-Meier method by means of the complementary log-log transformation [8, 9]. The Greenwood’s formula was used to calculate the standard error of the estimates from the Kaplan-Meier curve [8]. Secondary effectiveness variables were ORR, defined as the proportion of patients with a best response of complete response (CR) or partial response (PR) at 12 months for patients with measurable lesions evaluated using only the Response Evaluation Criteria in Solid Tumours (RECIST) version 1.1, and PFS, defined as the time from the date of the start of pazopanib therapy to the date of the event (defined as the first documented disease progression or death due to any cause) [10]. If a patient did not have an event, PFS was censored at the date of the last adequate tumour assessment. Long-term responders were defined as patients who were progression-free for ≥18 months while receiving pazopanib treatment. Secondary safety variables included safety and tolerability of pazopanib; RDI (defined as the ratio of the average daily dose of pazopanib to the recommended daily dose of pazopanib during the 12-month observational period); correlation of RDI with the safety profile; and treatment outcomes at 12 months.
Patients who received ≥1 dose of pazopanib (full analysis set [FAS]) were evaluable for efficacy, and all patients who received ≥1 dose of pazopanib and had ≥1 safety assessment on or after baseline (safety analysis set [SAS]) were evaluable for safety. The measurable disease population comprised patients with measurable disease at baseline and was used for the analysis of ORR.
Statistical analysis
The proportion of patients remaining progression-free at 12 months was estimated along with the 95% CIs using the Clopper-Pearson method. The best overall response for overall and measurable disease was estimated using the sample proportion (%) along with the 95% CIs with the Clopper-Pearson method. The Kaplan-Meier method was used to analyse PFS. Adverse events (AEs) and concomitant medication terms were coded using the Medical Dictionary for Regulatory Activities (MedDRA).
Results
A total of 200 patients from 15 countries were enrolled between June 2017 and December 2018. Ten patients were excluded owing to nonreliability of data, and 190 patients from 14 countries and 34 centres with a median (range) age of 61.0 (22.0–96.0) years were included in the final analysis. Most patients were Asian (70.0%), and clear cell carcinoma was the most common type of RCC (80.5%). Patient demographics are shown in Table 1.
A total of 189 patients were included in the FAS and 190 in the SAS. Overall, 78 (41.1%) patients completed the observational period and 67 (35.3%) completed the follow-up period. The most common (≥ 5%) reasons for discontinuation were progressive disease (30.0%), death (13.2%), and AEs (5.3%). Patient disposition by the end of the observational period is presented in Table 2.
Efficacy
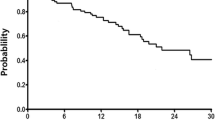
Of the 145 evaluable patients, 56 (39%; 95% CI: 30.7–47.2) remained progression-free at 12 months, and 37 (34%; 95% CI: 25.2–43.6) of the 109 evaluable patients remained progression-free at EOS. The overall median PFS was 9.7 months (95% CI: 8.5–11.8). The median time to progression was longer among patients aged < 65 years (11.2 months [95% CI: 9.5–15.9]) than among patients aged ≥65 years (6.8 months [95% CI: 4.2–9.9]). The median time to progression was longer for the intermediate categories (MSKCC: 8.9 months [95% CI: 7.1–11.5]; IMDC: 9.1 months [95% CI: 7.4–13.2]) than for the poor categories (MSKCC: 3.7 months [95% CI: 2.0–6.8]; IMDC: 4.2 months [95% CI: 2.6–9.7]). Median not reached in favourable group and median time to progression in unknown risk categories was comparable with the overall patients (MSKCC: 11.2 months [95% CI: 8.48–15.18]; IMDC: 9.9 months [95% CI: 8.48–12.22]) Fig. 1 shows PFS by baseline by MSKCC and IMDC criteria.
Among the 127 patients with available RECIST data, the most commonly reported best objective response by EOS was stable disease (56 patients [44.1%]), followed by progressive disease (PD; 40 patients [31.5%]), PR (27 patients [21.3%]), and CR (4 [3.1%] patients). The ORR (CR + PR) for the overall population was 24.4%. The disease control rate (DCR; CR + PR + stable disease) was 68.5%. For patients with measurable disease, the ORR was 25.7% and DCR was 67.3% (Table 3).
Patients in the < 65 years age group were more likely to achieve CR or PR as best response (27.5%) than patients in the ≥65 years age group (19.1%). Among patients with MSKCC and IMDC risk data available at baseline, the highest proportion of patients who achieved CR or PR as best response was the favourable group (7/12; 58.3% in the MSKCC risk group and 50.0% (4/8) in the IMDC risk group) (Table 4).
Treatment sequence profile
Overall, 14 (7.3%) patients had received prior treatment for RCC before switching to pazopanib. The most frequent prior treatment was interferon (12 of 15 patients [80.0%]); all other types of prior treatments were received by 1 patient (6.7%) each. Disease progression was the most common reason reported for switching to pazopanib (11 patients [73.3%]) (Table 5).
A total of 52 patients (27.4%) received treatment after discontinuing pazopanib. The most common (≥10.0%) treatments were nivolumab (21 patients [40.4%]), axitinib (13 patients [25.0%]), everolimus (13 patients [25.0%]), and sunitinib (9 patients [17.3%]). Disease progression was the most common reason reported for switching from pazopanib (45 patients [86.5%]) followed by AEs (7 patients [13.5%]) (Table 5).
Exposure to pazopanib
The starting dose of pazopanib was 800 mg (full dose) in 63.2% of patients, 600 mg in 22.1%, and 400 mg in 14.7%. Overall, 5.8% of the patients receiving 400 mg/day and 3.2% receiving 600 mg/day of pazopanib had a dose increase, while 10.5% of patients receiving 800 mg/day and 2.1% receiving 600 mg/day had a dose decrease. From the initial prescription of pazopanib, the overall mean (standard deviation [SD]) exposure to pazopanib was 10.1 (6.79) months.
The mean (SD) overall RDI was 79.4% (21.04), which was close to the median RDI of 81.9%. The minimum RDI was 32.5% and maximum was 100%. A total of 120 patients (63.2%) had a reduced RDI (< 100%), of whom 99 (52.1%) had an RDI of < 85%. A higher proportion of patients achieving CR or PR (32.7%) and a lower proportion of patients with PD (23.6%) were seen with a mean RDI of ≥85% vs a mean RDI of < 85% (ORR: 19.2%; PD: 37.0%). In patients who attained CR or PR, the overall mean (SD) RDI was 83.1% (19.4). The mean (SD) RDI in patients with an RDI of < 85% was 63.7% (12.8), and in patients with an RDI of ≥85%, the mean (SD) RDI was 98.2% (3.4). Patients with a mean RDI of ≥85% were less likely to experience an AE (76.9%) or a serious AE (SAE; 29.7%) than patients who had a mean RDI of < 85% (AE: 98.0%; SAE: 38.4%) (Table 6).
Long-term response
Of the 109 patients with evaluable data, 39 patients (35.8%) received pazopanib for ≥18 months and 21 remained progression-free at 18 months, with a proportion of 0.19 (19.3%; 95% CI: 12.3–27.9).
Safety
Overall, 167 patients (87.9%) experienced at least one treatment-emergent AE (TEAE) during the study period, of whom 138 (72.6%) experienced at least one TEAE related to pazopanib. The most common (≥ 15%) TEAEs were diarrhoea (31.1%) and hypertension (15.3%). A total of 65 patients (34.2%) experienced at least one SAE, of whom 13 (6.8%) experienced at least 1 SAE related to pazopanib. Of the 65 patients, 38 (20.0%) died owing to an SAE; three patients (1.6%) died owing to a treatment-related SAE. A total of 36 (18.9%) patients discontinued study treatment owing to a TEAE, of whom 11 (10.9%) discontinued owing to a TEAE related to pazopanib. A total of 77 (40.5%) patients required treatment interruptions or dose adjustments due to a TEAE, of whom 64 (33.7%) required treatment interruptions or dose adjustments due to a TEAE related to pazopanib. TEAEs related to pazopanib are summarised in Table 7.
Deaths
A total of 57 patients (30.0%) died during the study. The most common cause of death was disease progression (31 patients [16.3%]), followed by death from unknown causes (8 patients [4.2%]). Three deaths were suspected to be related to pazopanib, including deaths from cerebrovascular stroke, cytomegaloviral pneumonia, and sepsis (n = 1 each).
Discussion
The PARACHUTE study is the largest prospective, observational study of pazopanib aimed to assess the clinical effectiveness of pazopanib in real-world settings in patients with RCC who are naive to VEGFR-TKI therapy in countries in Asia Pacific, North Africa, and Middle East regions, where data from registration trials are lacking or limited. The proportion of patients remaining progression-free at 12 months, i.e., the primary efficacy outcome, was 38.6%, which was within the expected range of 38 to 52% based on the pazopanib pivotal trial [4], but was less than the 45% observed in PRINCIPAL, another prospective observational study of pazopanib [6].
Overall, the effectiveness and safety results from this study are largely consistent with those of the previously reported pazopanib studies [4,5,6]. A marginally low ORR was observed in this study (24.4% overall and 25.7% for patients with measurable disease) compared with the 30% ORR observed in the PRINCIPAL study [6]. Baseline patient characteristics age < 65 years and favourable risk based on either MSKCC or IMDC appear to be favourable factors to achieve a CR or a PR. The overall DCR observed in this study is the similar to the 68% DCR observed in the pivotal study of pazopanib [4].
The median PFS (9.7 months) in this study is comparable to the PFS noted in the pivotal study and real-world studies reported so far [6, 11, 12]. Baseline patient characteristics associated with PFS benefit included age < 65 years and favourable risk based by either MSKCC or IMDC criteria. Data for risk group classifications were unavailable for about one third of patients (33.7% with unknown MSKCC risk and 38.4% with risk) in this study and are comparable with the percentages reported in In PRINCIPAL study [6] with 27 and 20% and ADONIS study [13] with 46.8 and 48.7% of patients with unknown MSKCC and IMDC risk categories, respectively.
Median PFS for patients with unknown risk group is (months) is comparable with the median PFS of overall population. The proportion of patients remaining progression free for 18 months or longer while on pazopanib in this study was similar to that reported in a long-term response study of sunitinib (19.3% vs 18.9%, respectively) [14].
At the time of start of the PARACHUTE study, pazopanib was considered as one of the standard-of-care first-line therapies for RCC in most countries [7]. The recent development of immune checkpoint inhibitors, either alone or in combination with TKIs, has considerably changed the treatment paradigm of RCC [15,16,17]. As more treatment options become available, the optimal sequence for metastatic RCC remains unclear. Data on treatment patterns in routine clinical practice provide valuable information to healthcare professionals. In line with the European Society for Medical Oncology (ESMO) clinical practice guidelines for RCC [18], after discontinuation of pazopanib, the largest proportion of patients (40%) switched to nivolumab, an immune-oncology therapy approved for second-line therapy in RCC [19]. The other post-pazopanib treatments included axitinib (25%), everolimus (25%), and sunitinib (17.3%). Fewer than expected (only 9.6%) patients received cabozantinib after progression on pazopanib, with the lack of availability of the drug in many of these countries likely being the cause. Disease progression followed by AEs were the most common reasons for treatment switch.
A considerable proportion of patients (37%) started pazopanib at a reduced dose, with all patients being Asian. One potential explanation for this high percentage could be that most patients (70%) recruited in the study were Asian. Patients receiving a higher mean RDI showed better chances of achieving objective response, indicating a correlation between RDI and treatment outcomes. In contrast to the notion that higher RDI is associated with higher toxicity, patients in the high RDI group reported a better safety profile with fewer AEs and SAEs. Though the performance status was not recorded in this study, it is possible that the physically fit patients might have received higher doses and reported fewer AEs as compared to the lower dose intensity in less fit patients and resulting higher toxicity. The other less likely reason could be that patients on a full dose had a response that might have improved symptoms related to the disease.
With no new or unexpected AEs reported, the safety profile observed in this study is consistent with that seen in the pivotal and real-world evidence studies [15,16,17]. The most commonly reported AEs related to pazopanib were diarrhoea (30.5%), palmar-plantar erythrodysesthesia syndrome (14.7%), hypertension (14.2%), and nausea (10%). The percentage of patients who discontinued treatment owing to an AE in the current study was approximately 4% higher than that in the PRINCIPAL study. Disease progression was the most common reason for discontinuation as noticed in the pivotal and extension studies of pazopanib [4, 20]. The overall rate of dose changes or treatment interruptions was numerically higher than that observed in the PRINCIPAL study (53.7% vs 49.3%) [6]. Three deaths were suspected to be related to pazopanib, including deaths from cerebrovascular stroke, cytomegaloviral pneumonia, and sepsis.
Limitations of the study
This study was subject to some limitations, mainly the observational nature and non-interventional design of the study and lack of a control group or tests of hypothesis. However, the non-interventional nature of the study is best suited to obtain real-world data. The representative number of patients observed and the full safety reporting were assets of this study and minimised its limitations. Limitations such as information and selection bias and limitations of feasibility were expected to be similar to those of other multicentre, prospective non-interventional trials.
Conclusions
The PARACHUTE study represents the real-world evaluation of the effectiveness and safety of pazopanib in patients with advanced or metastatic RCC who are naive to VEGFR-TKI therapy in countries across Asia Pacific, North Africa, and Middle East regions. The results support the use of pazopanib in routine clinical practice and confirm the favourable safety profile of pazopanib consistent with the previously reported safety profile in pivotal and real-world evidence-based studies.
Availability of data and materials
“Novartis is committed to sharing with qualified external researchers, access to patient-level data and supporting clinical documents from eligible studies. These requests are reviewed and approved by an independent review panel on the basis of scientific merit. All data provided is anonymised to respect the privacy of patients who have participated in the trial in line with applicable laws and regulations.
This trial data availability is according to the criteria and process described on www.clinicalstudydatarequest.com.”
Change history
09 November 2021
A Correction to this paper has been published: https://doi.org/10.1186/s12885-021-08848-8
Abbreviations
- AE:
-
Adverse event
- CI:
-
Confidence interval
- CR:
-
Complete response
- DCR:
-
Disease control rate
- EOS:
-
End of study
- ESMO:
-
European Society for Medical Oncology
- FAS:
-
Full analysis set
- IMDC:
-
International Metastatic Renal Cell Carcinoma Database Consortium
- MedDRA:
-
Medical Dictionary for Regulatory Activities
- mRCC:
-
Metastatic renal cell carcinoma
- MSKCC:
-
Memorial Sloan Kettering Cancer Center
- ORR:
-
Objective response rate
- PD:
-
Progressive disease
- PFS:
-
Progression free survival
- PR:
-
Partial response
- RDI:
-
Relative dose intensity
- RECIST:
-
Response Evaluation Criteria in Solid Tumours
- SAE:
-
Serious adverse event
- SAS:
-
Safety analysis set
- SD:
-
Standard deviation
- TEAE:
-
Treatment emergent adverse event
- TKI:
-
Tyrosine kinase inhibitor
- VEGFR:
-
Vascular endothelial growth factor receptor
References
Kumar R, Knick VB, Rudolph SK, Johnson JH, Crosby RM, Crouthamel MC, et al. Pharmacokinetic-pharmacodynamic correlation from mouse to human with pazopanib, a multikinase angiogenesis inhibitor with potent antitumor and antiangiogenic activity. Mol Cancer Ther. 2007;6(7):2012–21. https://doi.org/10.1158/1535-7163.MCT-07-0193.
Votrient (pazopanib) European public assessment report (EPAR), Available from https://www.ema.europa.eu/en/medicines/human/EPAR/votrient#authorisation-details-section (Accessed 10-Nov-2020).
Votrient® (pazopanib) Prescribing information, Available from https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/022465s029lbl.pdf (Accessed 10-Nov-2020).
Sternberg CN, Davis ID, Mardiak J, Szczylik C, Lee E, Wagstaff J, et al. Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial. J Clin Oncol. 2010;28(6):1061–8. https://doi.org/10.1200/JCO.2009.23.9764.
Motzer RJ, Hutson TE, Cella D, Reeves J, Hawkins R, Guo J, et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med. 2013;369(8):722–31. https://doi.org/10.1056/NEJMoa1303989.
Schmidinger M, Bamias A, Procopio G, Hawkins R, Sanchez AR, Vazquez S, et al. Prospective observational study of Pazopanib in patients with advanced renal cell carcinoma (PRINCIPAL study). Oncologist. 2019;24(4):491–7. https://doi.org/10.1634/theoncologist.2018-0787.
Pak S, Suh YS, Lee DE, Kim SH, Joung JY, Park WS, et al. Association between postoperative detection of circulating tumor cells and recurrence in patients with prostate Cancer. J Urol. 2020;203(6):1128–34. https://doi.org/10.1097/JU.0000000000000704.
Collett D. Modelling survival data in medical research. 2nd ed. London: Chapman & Hall/CRC; 1994. https://doi.org/10.1007/978-1-4899-3115-3.
Lachin J. Biostatistical methods: the assessment of relative risks. Hoboken: John Wiley & Sons Ltd.; 2000. https://doi.org/10.1002/9780470317051.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Ruiz-Morales JM, Swierkowski M, Wells JC, Fraccon AP, Pasini F, Donskov F, et al. First-line sunitinib versus pazopanib in metastatic renal cell carcinoma: results from the international metastatic renal cell carcinoma database consortium. Eur J Cancer. 2016;65:102–8. https://doi.org/10.1016/j.ejca.2016.06.016.
Matrana MR, Bathala T, Campbell MT, Duran C, Shetty A, Teegavarapu P, et al. Outcomes of unselected patients with metastatic clear-cell renal cell carcinoma treated with first-line pazopanib therapy followed by vascular endothelial growth factor receptor tyrosine kinase inhibitors or mammalian target of rapamycin inhibitors: a single institution experience. BJU Int. 2016;118(2):264–71.
Schmidinger M, Porta C, Oudard S, Denechere G, Brault Y, Serfass L, et al. Real-world experience with Sunitinib treatment in patients with metastatic renal cell carcinoma: clinical outcome according to risk score. Clin Genitourin Cancer. 2020;18(5):e588–e97. https://doi.org/10.1016/j.clgc.2020.02.013.
Molina AM, Jia X, Feldman DR, Hsieh JJ, Ginsberg MS, Velasco S, et al. Long-term response to sunitinib therapy for metastatic renal cell carcinoma. Clin Genitourin Cancer. 2013;11(3):297–302. https://doi.org/10.1016/j.clgc.2013.04.001.
Motzer RJ, Penkov K, Haanen J, Rini B, Albiges L, Campbell MT, et al. Avelumab plus Axitinib versus Sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380(12):1103–15. https://doi.org/10.1056/NEJMoa1816047.
Rini BI, Plimack ER, Stus V, Gafanov R, Hawkins R, Nosov D, et al. Pembrolizumab plus Axitinib versus Sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380(12):1116–27. https://doi.org/10.1056/NEJMoa1816714.
Albiges L, Barthelemy P, Gross-Goupil M, Negrier S, Needle MN, Escudier B. TiNivo: safety and efficacy of tivozanib-nivolumab combination therapy in patients with metastatic renal cell carcinoma. Ann Oncol. 2021;32(1):97–102.
Escudier B, Porta C, Schmidinger M, Rioux-Leclercq N, Bex A, Khoo V, et al. Renal cell carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-updagger. Ann Oncol. 2019;30(5):706–20. https://doi.org/10.1093/annonc/mdz056.
Fizazi K, Shore N, Tammela TL, Ulys A, Vjaters E, Polyakov S, et al. Nonmetastatic, castration-resistant prostate Cancer and survival with Darolutamide. N Engl J Med. 2020;383(11):1040–9. https://doi.org/10.1056/NEJMoa2001342.
Sternberg CN, Davis ID, Deen KC, Sigal E, Hawkins RE. An open-label extension study to evaluate safety and efficacy of pazopanib in patients with advanced renal cell carcinoma. Oncology. 2014;87(6):342–50. https://doi.org/10.1159/000366227.
Acknowledgements
Medical writing and editorial support was provided by Anuradha Bandaru of Novartis Healthcare Pvt. Ltd. (Hyderabad, India).
Funding
The PARACHUTE study was sponsored by Novartis Pharmaceuticals Corporation; pazopanib is an asset of Novartis AG as of 1 March 2015.
Author information
Authors and Affiliations
Contributions
ME: Conceptualization, methodology, writing and review & editing of the manuscript; BB: Investigation and review of the manuscript; PD: Investigation and review of the manuscript; LC: Investigation and review of the manuscript; YFW: Investigation and review of the manuscript; TH: Investigation and review of the manuscript; CSL: Investigation and review of the manuscript; BK: Investigation and review of the manuscript; HJC: Investigation and review of the manuscript; CC: Data curation, formal analysis, validation, visualization, review of the manuscript; SI: Project administration data curation, formal analysis, validation; visualization, review of the manuscript; KS: Conceptualization, validation, visualization, review of the manuscript; RK: Conceptualization, methodology, writing and review & editing of the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was conducted ethically in accordance with the World Medical Association.
Declaration of Helsinki International Conference on Harmonisation Good Clinical Practice, patient privacy requirements, and ethical principles outlined in the Declaration of Helsinki.
2018. The protocol and ICF were reviewed and approved in Singapore by “Singhealth Centralised Institutional Review Board (CIRB)”, and also by properly constituted Institutional Review Boards/Independent Ethics Committees (IRB/IEC) of 34 other participating centres according to local regulations before the start of the study. Health authority approval was obtained per local regulations. Patients provided informed consent according to local requirements.
Consent for publication
Not Applicable.
Competing interests
ME reports honoraria from Novartis, Pfizer, Astellas, Janssen, BMS, MSD, Amgen, Nobel, Astra-Zeneca, Roche, and Gen Ilac outside the submitted work; TH is a member of advisory board, consultant and speaker for Hoffman la Roche, Novartis, Astra Zeneca, MSD, Amgen, Pfizer, Janssen Cilag, Merck Serono, and Mundi Pharma; BK reports clinical trials, satellite symposiums, congress and journal support from Roche, Pfizer, Novartis, Merck, Serono, MSD, Amgen, Bayer, Gen, BMS, and AstraZeneca; RK reports grants and personal fees from Eisai, Ipsen, BMS, MSD, Pfizer, Astellas, Johnson & Johnson, Amgen, Sanofi, and Mundipharma outside the submitted work; Sara Ingles is employed by Aerotek and contracted by Novartis AG; KS is an employee of Novartis and owner of stock options; CC is an employee of Novartis AG; BB, PD, LC, YFW, CSL, and HJC have declared that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The author given names and family names of Mustafa Erman, Bivas Biswas, Pongwut Danchaivijitr, Lingwu Chen and Chandrasekhar Chikatapu have been corrected.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Erman, M., Biswas, B., Danchaivijitr, P. et al. Prospective observational study on Pazopanib in patients treated for advanced or metastatic renal cell carcinoma in countries in Asia Pacific, North Africa, and Middle East regions: PARACHUTE study. BMC Cancer 21, 1021 (2021). https://doi.org/10.1186/s12885-021-08738-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-021-08738-z