Abstract
Background
Pulmonary sclerosing pneumocytoma (PSP) is a rare benign tumor. Although lymph node metastasis has been reported, it is still considered benign. No malignant transformation has been reported. This is the first case of malignant transformation of both cuboidal surface cells and stromal round cells.
Case presentation
A 64-year-old male had been complaining of intermittent hemoptysis several times per day for eight months. Chest computed tomography scan showed parenchymal infiltration with cystic lesion in the right lower lobe accompanied by enlarged right hilar lymph nodes. Lobectomy and systemic lymph node dissection was performed.
On grossly pathological examination, the lesion was 50 mm from the bronchial stump. It was a mixture of both cystic and solid components and 30 mm * 20 mm in size with unclear border. Microscopically, the cuboidal surface cells transformed to adenocarcinoma. The stromal round cells also had a malignant transformation. The Ki-67 proliferation index in malignant cuboidal surface cells and stromal round cells were 70 and 55%, respectively. Furthermore, E-cadherin was negative in primary tumor but positive in metastatic lymph node, which suggested that the mesenchymal to epithelial transition may play an important role in lymph node metastasis.
Conclusions
To our knowledge, we present the first case of malignant transformation of both cuboidal surface cells and stromal round cells in PSP. The process of mesenchymal to epithelial transition may play an important role in lymph node metastasis.
Similar content being viewed by others
Background
Pulmonary sclerosing pneumocytoma (PSP) is a rare benign tumor which has been described as sclerosing hemangioma [1]. It was previously considered as a vascular neoplasm, and now as a derivative from the primitive respiratory epithelium [2]. It is predominant in females, most commonly seen in middle aged females [3, 4]. Patients are always asymptomatic and computed tomography (CT) and X-ray of chest shows solitary, well circumscribed masses. The key pathological features of PSP involve two types of cells, cuboidal surface cells and stromal round cells, which are both neoplastic. Immunohistochemistry (IHC) studies show that thyroid transcription factor-1 (TTF-1) and epithelial membrane antigen (EMA) are both positive [2]. Pancytokeratin (CKpan) and Napsin A are both positive in cuboidal surface cells, while negative in stromal round cells [5]. Though lymph node metastasis has been reported, PSP is still considered benign [6, 7]. We report a unique case of PSP with malignant transformation in both cuboidal surface cells and stromal round cells, which has not been reported before.
Case presentation
A 64-year-old male had been complaining of intermittent hemoptysis several times per day for eight months. He had no fever, chest pain, shortness of breath, dizziness or amaurosis. He had no relevant medical history especially no history of cancer. He had no smoking history. The patient was admitted to The First Affiliated Hospital, School of Medicine, Zhejiang University due to symptoms getting worse. Chest computed tomography scan on July 1st, 2018 showed parenchymal infiltration with cystic lesion in the right lower lobe accompanied by enlarged right hilar lymph nodes (Fig. 1). Transbronchial lung biopsy under bronchofibroscopy was free of tumor cells. A primary surgical resection was recommended by surgeons. Lobectomy and systemic lymph node dissection was done on July 4th, 2018. The patient is now well after he recovered from surgery. So far there were no signs of tumor recurrence or metastasis.
Upon grossly pathological examination, the lesion was located in the right lower lobe, 50 mm from the bronchial stump. It was gray-tan to yellow on the section, with foci of hemorrhage. The lesion was a mixture of both cystic and solid components and was 30 mm *20 mm in size with unclear border. The solid component was in the middle of the lesion and was 17 mm*17 mm in size, surrounded by honeycomb cystic components.
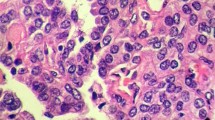
Microscopically, the structure of the solid component of the tumor was similar to a typical PSP. It was composed of areas of cuboidal surface cells and stromal round cells. The tumor showed a hemorrhage pattern (Fig. 2). Bronchial adenomatous hyperplasia and cystic dilatation were noticed in surrounding areas. TTF-1 and EMA were positive in both cuboidal surface cells and stromal round cells (Fig. 2) while CKpan and Napsin A were only positive in cuboidal surface cells.
(a, b) Tumor nodule showed a typical pulmonary sclerosing pneumocytoma of hemorrhage growth pattern comprising of large blood-filled spaces lined by surface cells (h&e). (c, d) Cuboidal surface cell were positive for pancytokeratin (CKpan), round cells were negative for CKpan. (e, f) Cuboidal surface cell were positive for Napsin A, round cells were negative. (g, h) Both cuboidal surface and stromal round cells were positive for thyroid transcription factor-1 (TTF-1). (i, j) Both cuboidal surface and stromal round cells were positive for epithelial membrane antigen (EMA)
In the case reported, while most of the surface cells being similar to a typical PSP in some areas of the tumor, a few transformed to adenocarcinoma. The nuclei were columnar and containing hyperchromatic nuclear chromatin. In addition, the surface cells replaced the alveolar lining and invaded the fibrous stroma and vascular walls with TTF-1, EMA, Napsin A and CKpan all positive. The Ki-67 proliferation index was 70% (Fig. 3). We also noticed atypical adenomatous hyperplasia (AAH) of cuboidal cells in the transition area (Fig. 3). Cuboidal surface cells proliferated along preexisting alveolar walls with mild to moderate cellular atypia. A typical hobnail appearance was also seen in the atypical cuboidal surface cells. Substantial gaps along the surface of basement membrane in the transition area were also evident of AAH.
A few stromal round cells had small, well-defined borders and central bland nuclei without nucleoli similar to that in a typical PSP. However, mild to moderate atypical stromal round cells proliferation was seen in the transition region (Fig. 4). Binuclearization and intranuclear eosinophilic inclusions were common in the transition area in our case. Furthermore, abundant cytoplasm, nuclear polymorphism, prominent nucleoli and irregular mitosis were observed in malignant stromal round cells, adjoining the transition areas (Fig. 4). Vascular invasion and pulmonary parenchyma involvements were also found in malignant lamellarlike stromal round cells. TTF-1, P63 and EMA were all positive. Only a small amount stromal round cells were positive for CKpan. However, stromal round cells were negative for beta-catenin and E-cadherin. The Ki-67 proliferation index in these areas was 55%, which was significantly increased compared to typical PSP areas (Fig. 4). Both stromal round cells and surface cells were negative for Progesterone receptor, CD20, CD3, S− 100, Melana, HMB45, Myogenin, MyoD1, CgA and Syn. Further molecular investigation using a polymerase chain reaction panel showed that no EGFR, ALK or ROS1 mutation was detected.
(a,b,c) Low power view and high power view demonstrated that stromal round cells in the left side transformed to the malignant tumor (black arrow), round cells in the transition area (yellow arrow) had dysplasia (h&e). (d, b, f) Low power view and high power view demonstrated that Ki-67 proliferation index was significantly increased in the malignant area (black arrow). (g) Thyroid transcription factor-1 (TTF-1) was positive in stromal round cells. (h) Pancytokeratin was negative in stromal round cells. (i) E-cadherin was negative in stromal round cells
In this case, we also found mediastinal lymph nodes involvement. The architecture of lymph nodes was replaced by abnormal proliferated stromal round cells with either vacuolated or eosinophilic cytoplasm (Fig. 5). IHC showed that these cells were positive for TTF-1, partial positive for CKpan and E-cadherin, but negative for beta-catenin. However, the E-cadherin was negative in malignant stromal round cells in the primary tumor (Fig. 4).
(a, b) Mediastinal lymph node metastasis of pulmonary sclerosing pneumocytoma (h&e). (c) Round cells were positive for thyroid transcription factor-1. (d) pancytokeratin (CKpan) were partial positive in round cells. (e) E-cadherin was partial positive in the metastatic lymph node. (f) Ki-67 proliferation index was significantly increased in the metastatic lymph node
Discussion and conclusion
PSP is considered as a rare benign tumor [1]. In searches of PubMed and Embase database, there are 24 cases of PSP with lymph node metastasis and recurrence (Table 1) [2, 6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25]. Five cases have mediastinal lymph node metastasis, four have distant metastasis, and only one have recurrence of PSP. However, no case about malignant transformation of PSP has been reported. One case reports overgrown stromal round cells and bone metastasis, accompanied by increased cellularity and necrotic areas, but a Ki-67 index of less than 5% [22]. Another case reports PSP with metastatic spread to stomach with Ki-67 indeice in primary tumor and metastatic gastric lesion of 17.6 and 19.4%, respectively [19]. The. However, no malignant pathomorphological change has been reported. In Iyoda’s research, cases with recurrence has a Ki-67 index of 0.4% [26]. These results show no significantly increased proliferation of cells even in patients with recurrence or metastasis. In our case, the Ki-67 proliferation index of the malignant cuboidal surface cells and the stromal round cells are 70 and 55%, respectively. The high proliferative activity and pathomorphological change in both cuboidal surface cells and stromal round cells suggest that PSP transformed to a malignant tumor. Liu reports a case of coexistence of PSP and primary adenocarcinoma in the same tumor [27], which is different from our case, where the AAH of cuboidal surface cells indicated malignant transformation from cuboidal surface cells to adenocarcinoma. Similarly, the malignant transformation of stromal round cells is also confirmed by the transition region.
In our case, the two well-established epithelial markers, E-cadherin and CKpan [28], are both positive in the metastatic lymph nodes with similar levels (black arrows in Fig. 5), although they should be negative in metastatic lymph nodes (composed of stromal round cells). The epithelial marker expression in metastatic lymph nodes suggests the mesenchymal-epithelial transition (MET) during lymph node metastasis. Previous studies show that MET process is able to promote distal metastasis in breast cancer [29], especially for establishing macrometastasis [30,31,32], which, combined with our results, suggests that the the MET process may play an important role in lymph node metastasis of PSP. Although based on previous studies, lymph node involvement doesn’t affect long-term survival rate [6, 23], patients with malignant PSP may still need close follow-up.
In summary, we report the first case of malignant transformation in both cuboidal surface cells and stromal round cells, which suggests the malignant potential of PSP. The fact that E-cadherin is negative in primary tumor but positive in metastatic lymph nodes suggests that the process of MET plays an important role in lymph node metastasis of PSP.
Availability of data and materials
The datasets used in this study are available from the corresponding author on reasonable requests.
Abbreviations
- AAH:
-
Typical adenomatous hyperplasia
- CKpan:
-
Pancytokeratin
- CT:
-
Computed tomography
- EMA:
-
Epithelial membrane antigen
- IHC:
-
Immunohistochemistry
- MET:
-
Mesenchymal-epithelial transition
- PSP:
-
Pulmonary sclerosing pneumocytoma
- TTF-1:
-
Thyroid transcription factor-1
References
Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015;10:1243–60.
Devouassoux-Shisheboran M, Hayashi T, Linnoila RI, et al. A clinicopathologic study of 100 cases of pulmonary sclerosing hemangioma with immunohistochemical studies: TTF-1 is expressed in both round and surface cells, suggesting an origin from primitive respiratory epithelium. Am J Surg Pathol. 2000;24:906–16.
Zhu J. Analysis of the clinical differentiation of pulmonary sclerosing pneumocytoma and lung cancer. J Thorac Dis. 2017;9:2974–81.
Yang CH, Lee LY. Pulmonary sclerosing pneumocytoma remains a diagnostic challenge using frozen sections: a clinicopathological analysis of 59 cases. Histopathology. 2018;72:500–8.
Zhou J, Covinsky MH. Sclerosing Pneumocytoma: a carcinoma mimicker. A case report and literature review. Ann Clin Lab Sci. 2017;47:103–5.
Adachi Y, Tsuta K, Hirano R, et al. Pulmonary sclerosing hemangioma with lymph node metastasis: a case report and literature review. Oncol Lett. 2014;7:997–1000.
Pokharel S, Dhillon SS, Ylagan L, et al. Sclerosing Pneumocytoma with lymph node metastasis. J Thorac Oncol. 2016;11:1802–4.
Tanaka I, Inoue M, Matsui Y, et al. A case of pneumocytoma (so-called sclerosing hemangioma) with lymph node metastasis. Jpn J Clin Oncol. 1986;16:77–86.
Chan AC, Chan JK. Pulmonary sclerosing hemangioma consistently expresses thyroid transcription factor-1 (TTF-1): a new clue to its histogenesis. Am J Surg Pathol. 2000;24:1531–6.
Yano M, Yamakawa Y, Kiriyama M, et al. Sclerosing hemangioma with metastases to multiple nodal stations. Ann Thorac Surg. 2002;73:981–3.
Kim KH, Sul HJ, Kang DY. Sclerosing hemangioma with lymph node metastasis. Yonsei Med J. 2003;44:150–4.
Kim GY, Kim J, Choi YS, et al. Sixteen cases of sclerosing hemangioma of the lung including unusual presentations. J Korean Med Sci. 2004;19:352–8.
Miyagawa-Hayashino A, Tazelaar HD, Langel DJ, Colby TV. Pulmonary sclerosing hemangioma with lymph node metastases: report of 4 cases. Arch Pathol Lab Med. 2003;127:321–5.
Chan NG, Melega DE, Inculet RI, Shepherd JG. Pulmonary sclerosing hemangioma with lymph node metastases. Can Respir J. 2003;10:391–2.
Katakura H, Sato M, Tanaka F, et al. Pulmonary sclerosing hemangioma with metastasis to the mediastinal lymph node. Ann Thorac Surg. 2005;80:2351–3.
Jiang ZN, Zhu T, Jin M, Wang LB. Sclerosing hemangioma with lymph node metastasis: report of a case. Zhonghua Bing Li Xue Za Zhi. 2007;36:282–3.
Vaideeswar P. Sclerosing hemangioma with lymph nodal metastases. Indian J Pathol Microbiol. 2009;52:392–4.
Suzuki H, Saitoh Y, Koh E, et al. Pulmonary sclerosing hemangioma with pleural dissemination: report of a case. Surg Today. 2011;41:258–61.
Bae YS, Ro JY, Shim HS, et al. Pulmonary sclerosing haemangioma with metastatic spread to stomach. Histopathology. 2012;60:1162–4.
Kita H, Shiraishi Y, Katsuragi N, et al. Pulmonary sclerosing hemangioma with lymph node metastasis. Kyobu Geka. 2013;66:1141–4.
Xu HM, Zhang G. A rare case of pulmonary sclerosing hemagioma with lymph node metastasis and review of the literature. Int J Clin Exp Pathol. 2015;8:8619–23.
Kim MK, Jang SJ, Kim YH, Kim SW. Bone metastasis in pulmonary sclerosing hemangioma. Korean J Intern Med. 2015;30:928–30.
Soo IX, Sittampalam K, Lim CH. Pulmonary sclerosing pneumocytoma with mediastinal lymph node metastasis. Asian Cardiovasc Thorac Ann. 2017;25:547–9.
Wang X, Zhang L, Wang Y, et al. Sclerosing pneumocytoma with metastasis to the mediastinal and regional lymph nodes. Indian J Pathol Microbiol. 2018;61:407–9.
Wei S, Tian J, Song X, Chen Y. Recurrence of pulmonary sclerosing hemangioma. Thorac Cardiovasc Surg. 2008;56:120–2.
Iyoda A, Hiroshima K, Shiba M, et al. Clinicopathological analysis of pulmonary Sclerosing Hemangioma. Ann Thorac Surg. 2004;78:1928–31.
Liu W, Tian XY, Li Y, et al. Coexistence of pulmonary sclerosing hemangioma and primary adenocarcinoma in the same nodule of lung. Diagn Pathol. 2011;6:41.
Perl AK, Wilgenbus P, Dahl U, et al. A causal role for E-cadherin in the transition from adenoma to carcinoma. Nature. 1998;392:190–3.
Mon AM, MacKinnon AC Jr, Traktman P. Overexpression of the VRK1 kinase, which is associated with breast cancer, induces a mesenchymal to epithelial transition in mammary epithelial cells. PLoS One. 2018;13:e0203397.
Umbreit C, Erben P, Faber A, et al. Lapatinib-induced mesenchymal-epithelial transition in squamous cell carcinoma cells correlates with unexpected alteration of beta-catenin expression. Oncol Lett. 2016;11:2715–24.
Guo F, Parker Kerrigan BC, Yang D, et al. Post-transcriptional regulatory network of epithelial-to-mesenchymal and mesenchymal-to-epithelial transitions. J Hematol Oncol. 2014;7:19.
Hamilton G, Rath B. Mesenchymal-epithelial transition and circulating tumor cells in small cell lung Cancer. Adv Exp Med Biol. 2017;994:229–45.
Acknowledgements
The authors express gratitude to all the technical and clinical staffs involved in patient management and laboratory diagnosis.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or nonprofit sectors.
Author information
Authors and Affiliations
Contributions
TX collected the data, reviewed the literature, drafted and edited the manuscript. TXD conceived the study, participated in experiment design and data acquisition and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received ethics approval from the Commission for Scientific Research in the First Affiliated Hospital, School of Medicine, Zhejiang University. The patient provided written informed consent.
Consent for publication
Written informed consent was obtained from the patient and his healthy sibling for the publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Teng, X., Teng, X. First report of pulmonary sclerosing pneomucytoma with malignant transformation in both cuboidal surface cells and stromal round cells: a case report. BMC Cancer 19, 1154 (2019). https://doi.org/10.1186/s12885-019-6356-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-019-6356-z