Abstract
Background
Although anaplastic lymphoma kinase (ALK) fusion genes are generally identified in lung adenocarcinoma patients, they are relatively rare in patients with squamous cell carcinoma (SqCC). Metastatic ALK-rearranged lung adenocarcinoma patients treated with ALK inhibitors demonstrate higher response rates, improved progression-free survival, and reduced toxicity relative to those treated with conventional chemotherapy regimens. However, the efficacy of treatment with ALK inhibitors in patients with ALK-rearranged lung SqCC remains unknown.
Case presentation
We discuss a 52-year-old Japanese-Brazilian woman without a history of smoking who was referred to our hospital for evaluation of severe left back pain and a left hilar mass observed on a chest radiograph. The patient was eventually diagnosed on the basis of computed tomography, pathological, and immunohistochemical findings as having Stage IV lung SqCC. First-line treatment with palliative radiotherapy and systemic chemotherapy with cisplatin plus vinorelbine was administered, but was not effective. ALK testing was subsequently performed, revealing positive ALK expression and gene rearrangement. Alectinib therapy was then initiated, which resulted in a gradual, but substantial reduction in tumor size.
Conclusions
To the best of our knowledge, this is the first case report to discuss the successful management of ALK-rearranged lung SqCC with alectinib. We propose that molecular testing for driver mutations should be considered in young patients with a light or no smoking history, even if the histological findings correspond with SqCC, and alectinib therapy represents a reasonable option in cases of ALK-rearranged lung SqCC.
Similar content being viewed by others
Background
Numerous oncogenic driver mutations have been identified in patients with non-small cell lung cancer. Research has reported that two genes in particular (human epidermal growth factor receptor [EGFR] and anaplastic lymphoma kinase [ALK]) are associated with improvements in therapeutic efficiency in non-small cell lung cancer patients receiving targeted therapies. ALK fusion genes are typically identified in approximately 5.0% of patients with lung adenocarcinoma, although they are rare in patients with squamous cell carcinoma (SqCC) [1, 2]. Treatment of metastatic ALK-rearranged non-small cell lung cancer with ALK inhibitors leads to higher response rates and improved progression-free survival relative to conventional chemotherapy regimens [3, 4]. However, the efficacy of such treatment for ALK-rearranged lung SqCC remains unknown, as ALK-rearranged lung SqCC is very rare and ALK testing is not routinely performed in this patient population. Herein, we describe a rare case of ALK-rearranged lung SqCC responding to alectinib.
Case presentation
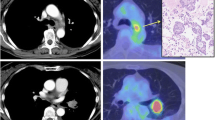
A 52-year-old Japanese-Brazilian woman without a history of smoking was referred to our hospital for evaluation of severe left back pain and a left hilar mass observed on a chest radiograph. Computed tomography of the chest revealed a solitary tumor in the left lower lobe with direct invasion to the seventh thoracic vertebra and rib. The patient also had mediastinal lymphadenopathy, left adrenal metastasis, and multiple bone metastases (Fig. 1a-b). Pathological examination of the transbronchial needle aspiration biopsy specimen revealed undifferentiated cancer with a mild tendency of cornification (hematoxylin and eosin staining, Fig. 2a). Upon immunohistochemical (IHC) analysis, the tumor cells exhibited strong positive staining for p40 and cytokeratin 5/6, but were negative for thyroid transcription factor-1 (Fig. 2b-d). Based on these findings, the patient was diagnosed with Stage IV lung SqCC and was treated with palliative radiotherapy and first-line systemic chemotherapy with cisplatin plus vinorelbine. After 2 cycles of chemotherapy, there was no evidence of a response. Second-line chemotherapy was thus indicated. Despite a diagnosis of SqCC, the patient underwent ALK testing, as she was a non-smoker diagnosed with lung cancer harboring the wild-type EGFR gene. IHC analysis indicated that the tumor cells were positive (2+ staining) for the ALK antibody (Histofine ALK iAEP Detection Kit; Nichirei Bioscience Inc., Tokyo, Japan). ALK break-apart fluorescence in situ hybridization (FISH) (Vysis ALK Break Apart FISH Probe Kit; Abbott Molecular, Inc., Des Plaines, IL, USA) confirmed the presence of an ALK gene rearrangement with a rearrangement-positive cell rate of 46.0% (Fig. 3). The patient was subsequently treated with alectinib, a selective ALK inhibitor. After 2 weeks of treatment, the symptoms gradually improved. After 3 months, a follow-up computed tomography scan revealed a remarkable response in the primary lesion and significant shrinkage of the left adrenal gland metastasis (Fig. 1c-d). At the latest follow-up, 11 months after commencing alectinib treatment, there was no evidence of progression or any remarkable toxicity.
Computed tomography findings before and after treatment with alectinib. A computed tomography scan before treatment revealed (a) a solitary tumor in the lower lobe of the left lung and (b) a left adrenal metastasis (arrow). A computed tomography scan 3 months after commencing treatment revealed (c) a dramatic reduction in tumor size and (d) almost no presence of metastases in the left adrenal gland (arrow)
Transbronchial lung biopsy specimen from a mediastinal lymph node. a Hematoxylin and eosin staining revealed undifferentiated cancer cells with a mild tendency of cornification (arrows). Immunohistochemical staining revealed that the tumor cells were negative for (b) thyroid transcription factor-1, but positive for (c) p40 and (d) cytokeratin 5/6
Discussion and conclusions
To the best of our knowledge, this is the first case report to discuss the successful management of ALK-rearranged lung SqCC with alectinib.
Our diagnosis of SqCC was confirmed by p40 immunostaining, which is useful and highly specific for the diagnosis of SqCC [5, 6]. Additionally, in our case, the results of the ALK detection test were concordant between IHC staining and FISH. Yamamoto et al. [7] reported a similar case, which was diagnosed with ALK-rearranged lung SqCC. The diagnosis was confirmed by IHC staining, which was positive for p40, but negative for thyroid transcription factor-1. The pathological specimen of their case [7] was also obtained from the primary lesion by bronchoscopic biopsy and no adenocarcinoma component was detected in the biopsy specimen. The case reported by Yamamoto et al. [7] was positive on FISH with a rearrangement-positive cell rate of just 20.0%, but negative on IHC staining. Ilie et al. [8] reported that cases with discordant ALK detection test results (i.e., FISH positive, but IHC staining negative) had lower rearrangement-positive cell rates of 15.0–20.0% and exhibited a tendency towards a lower response to crizotinib. However, since the case described by Yamamoto et al. [7] was treated with radiotherapy without chemotherapy, it remains unclear whether the patient exhibited a marked response to ALK targeted therapies. As shown in Table 1, only a few cases of ALK-rearranged lung SqCC responding to crizotinib have been reported to date [9,10,11,12]. Alectinib is a new drug that is expected to be safer and more effective than crizotinib as a first-line chemotherapy treatment for patients with ALK-rearranged lung adenocarcinoma [13]. Recently, Tamiya et al. [14] reported a case of ALK-rearranged lung SqCC that was treated with alectinib, although no response was observed. In our case, the patient with ALK-rearranged lung SqCC exhibited an antitumor response to alectinib. Further case reports are needed to confirm the efficacy of ALK targeted therapies for the treatment of ALK-rearranged lung SqCC patients.
There are some limitations to our case report. Our histological specimen was small and was obtained from a mediastinal lymph node. For this reason, there was the potential for an adenocarcinoma component to be contained in other regions or for there to be discrepancies between the primary lesion and metastatic lesions due to the heterogeneity and distribution of the tumor. In contrast, Hou et al. [15] reported a high concordance rate of ALK rearrangement between primary tumors and paired metastatic lymph nodes, which supports the findings of our case report.
In conclusion, molecular testing for driver mutations should be considered in young patients with a light or no smoking history, even if the histological findings correspond with SqCC. Alectinib represents a reasonable option in cases of ALK-rearranged lung SqCC.
Abbreviations
- ALK :
-
Anaplastic lymphoma kinase
- EGFR :
-
Epidermal growth factor receptor
- FISH:
-
Fluorescence in situ hybridization
- IHC:
-
Immunohistochemical
- SqCC:
-
Squamous cell carcinoma
References
Zhao W, Choi YL, Song JY, Zhu Y, Xu Q, Zhang F, et al. ALK, ROS1 and RET rearrangements in lung squamous cell carcinoma are very rare. Lung Cancer. 2016;94:22–7.
Kenmotsu H, Serizawa M, Koh Y, Isaka M, Takahashi T, Taira T, et al. Prospective genetic profiling of squamous cell lung cancer and adenosquamous carcinoma in Japanese patients by multitarget assays. BMC Cancer. 2014;14:786.
Seto T, Kiura K, Nishio M, Nakagawa K, Maemondo M, Inoue A, et al. CH5424802 (RO5424802) for patients with ALK-rearranged advanced non-small-cell lung cancer (AF-001JP study): a single-arm, open-label, phase 1-2 study. Lancet Oncol. 2013;14:590–8.
Solomon BJ, Mok T, Kim DW, Wu YL, Nakagawa K, Mekhail T, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371:2167–77.
Nobre AR, Albergaria A, Schmitt F. p40: a p63 isoform useful for lung cancer diagnosis - a review of the physiological and pathological role of p63. Acta Cytol. 2013;57:1–8.
Sakai Y, Nakai T, Ohbayashi C, Imagawa N, Yanagita E, Satake R, et al. Immunohistochemical profiling of ALK fusion gene-positive adenocarcinomas of the lung. Int J Surg Pathol. 2013;21:476–82.
Yamamoto Y, Kodama K, Maniwa T, Takeda M, Kishima H. Anaplastic lymphoma kinase-positive squamous cell carcinoma of the lung: a case report. Mol Clin Oncol. 2016;5:61–3.
Ilie MI, Bence C, Hofman V, Long-Mira E, Butori C, Bouhlel L, et al. Discrepancies between FISH and immunohistochemistry for assessment of the ALK status are associated with ALK ‘borderline’-positive rearrangements or a high copy number: a potential major issue for anti-ALK therapeutic strategies. Ann Oncol. 2015;26:238–44.
Wang Q, He Y, Yang X, Wang Y, Xiao H. Extraordinary response to crizotinib in a woman with squamous cell lung cancer after two courses of failed chemotherapy. BMC Pulm Med. 2014;14:83.
Mikes RE, Jordan F, Hutarew G, Studnicka M. First line crizotinib in anaplastic lymophoma kinase (ALK) rearranged squamous cell lung cancer. Lung Cancer. 2015;90:614–6.
Zhang Q, Wang J, Zhang S. ALK-rearranged squamous cell lung cancer: a case report. Int J Clin Exp Pathol. 2015;8:2195–8.
Vergne F, Quéré G, Andrieu-Key S, Descourt R, Quintin-Roué I, Talagas M, et al. ALK-rearranged squamous cell lung carcinoma responding to crizotinib: a missing link in the field of non-small cell lung cancer? Lung Cancer. 2016;91:67–9.
Nokihara H, Hida T, Kondo M, Kim YH, Azuma K, Seto T, et al. Alectinib (ALC) versus crizotinib (CRZ) in ALK-inhibitor naive ALK-positive non-small cell lung cancer (ALK+ NSCLC): Primary results from the J-ALEX study. J Clin Oncol. 2016;34(suppl; abstr 9008).
Tamiya A, Shimizu S, Atagi S. A case of squamous cell carcinoma harboring an EML4-ALK rearrangement that was unsuccessfully treated with the ALK inhibitor alectinib. J Thorac Oncol. 2015;10:e74.
Hou L, Ren S, Su B, Zhang L, Wu W, Zhang W, et al. High concordance of ALK rearrangement between primary tumor and paired metastatic lymph node in patients with lung adenocarcinoma. J Thorac Dis. 2016;8:1103–11.
Acknowledgements
Not applicable.
Funding
No specific funding was received for this study.
Availability of data and materials
The datasets generated and/or analyzed during this study are included in this published article.
Author information
Authors and Affiliations
Contributions
NM designed the case report and drafted the manuscript. KN designed the case report, participated in the diagnosis and management of the patient, and revised the manuscript for important intellectual content. T. Naito and TT participated in the diagnosis and management of the patient and revised the manuscript for important intellectual content. T. Nakajima participated in the diagnosis of the patient by conducting the histological and pathological investigations. ME participated in the diagnosis of the patient by conducting the radiographic investigations and obtaining the bronchoscopy specimens. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This case report was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
K.N. has received honoraria from Ono Pharmaceutical Co., Ltd. (Tokyo, Japan) and Taiho Pharmaceutical Co., Ltd. (Tokyo, Japan). T. Naito and M.E. have received honoraria from Ono Pharmaceutical Co., Ltd. (Tokyo, Japan). N.M. and T. Nakajima declare that they have no competing interests. T.T. has received grants and honoraria from Ono Pharmaceutical Co., Ltd. (Tokyo, Japan) and AstraZeneca K.K. (Osaka, Japan).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mamesaya, N., Nakashima, K., Naito, T. et al. ALK-rearranged lung squamous cell carcinoma responding to alectinib: a case report and review of the literature. BMC Cancer 17, 471 (2017). https://doi.org/10.1186/s12885-017-3468-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-017-3468-1