Abstract
Background
Recent preclinical and phase I studies have reported that rebamipide decreased the severity of chemoradiotherapy-induced oral mucositis in patients with oral cancer. This placebo-controlled randomized phase II study assessed the clinical benefit of rebamipide in reducing the incidence of severe chemoradiotherapy-induced oral mucositis in patients with head and neck cancer (HNC).
Methods
Patients aged 20–75 years with HNC who were scheduled to receive chemoradiotherapy were enrolled. Patients were randomized to receive rebamipide 2% liquid, rebamipide 4% liquid, or placebo. The primary endpoint was the incidence of grade ≥ 3 oral mucositis determined by clinical examination and assessed by central review according to the Common Terminology Criteria of Adverse Events version 3.0. Secondary endpoints were the time to onset of grade ≥ 3 oral mucositis and the incidence of functional impairment (grade ≥ 3) based on the evaluation by the Oral Mucositis Evaluation Committee.
Results
From April 2014 to August 2015, 97 patients with HNC were enrolled, of whom 94 received treatment. The incidence of grade ≥ 3 oral mucositis was 29% and 25% in the rebamipide 2% and 4% groups, respectively, compared with 39% in the placebo group. The proportion of patients who did not develop grade ≥ 3 oral mucositis by day 50 of treatment was 57.9% in the placebo group, whereas the proportion was 68.0% in the rebamipide 2% group and 71.3% in the rebamipide 4% group. The incidences of adverse events potentially related to the study drug were 16%, 26%, and 13% in the placebo, rebamipide 2%, and rebamipide 4% groups, respectively. There was no significant difference in treatment compliance among the groups.
Conclusions
The present phase II study suggests that mouth washing with rebamipide may be effective and safe for patients with HNC receiving chemoradiotherapy, and 4% liquid is the optimal dose of rebamipide.
Trial registration
ClinicalTrials.gov under the identifier NCT02085460 (the date of trial registration: March 11, 2014).
Similar content being viewed by others
Background
Oral mucositis is an adverse event (AE) frequently induced by radiotherapy and chemotherapy during cancer treatment. Common symptoms are pain, dysphagia, dysgeusia, and infection, which can considerably affect the patient’s quality of life. Additionally, oral mucositis is a risk factor for sepsis in patients with low neutrophil count secondary to cancer treatment toxicity. During cancer treatment, aggravation of oral mucositis leads to dose reduction, suspension, or discontinuation of treatment, thereby affecting the patient prognosis [1, 2].
Approximately 600,000 patients worldwide are currently undergoing cancer treatment with radiotherapy and/or chemotherapy, and are at risk of developing oral mucositis [3]. Reportedly, oral mucositis develops in more than 90% of patients receiving chemoradiotherapy (CRT) for head and neck cancer (HNC) [4]. Thus, there is a particularly strong demand for the development of prophylactic and therapeutic agents for oral mucositis.
Oral mucositis results from direct cell injury caused by chemotherapy or radiotherapy. Tissue injury is amplified by reactive oxygen species, proinflammatory cytokines and pathways, and metabolic byproducts of colonizing microorganisms [1]. Some agents targeting these underlying mechanisms have been evaluated for oral mucositis treatment. Palifermin, a keratinocyte growth factor-1, has been approved by the Food and Drug Administration for stem cell transplantation; however, it has not been approved for HNC, although it was shown to decrease oral mucositis effectively [5, 6]. Rebamipide, originally developed by Otsuka Pharmaceutical Co., Ltd. (Tokyo, Japan) for gastritis, gastric ulcer, and xerophthalmia enhances endogenous prostaglandin production in the gastric mucosa and inhibits free radical production [7,8,9]. Additionally, it has been shown to inhibit neutrophil activation and inflammatory cytokine production by mononuclear cells, gastric mucosa, and vascular endothelial cells, and to inhibit other inflammatory reactions [10,11,12].
In pilot studies performed to assess the efficacy of rebamipide liquid for CRT-induced oral mucositis in patients with oral cancer, rebamipide decreased the severity of mucositis [13, 14]. Additionally, rebamipide liquid administered at doses of 1%, 2%, and 4%, resulted in a dose-dependent reduction of total injury extension and tongue ulcerations in a rat model of irradiation-induced oral mucositis [15].
In accordance with these preclinical and phase I studies, rebamipide 2% and 4% liquids were chosen as potential prophylactic and therapeutic agents for CRT-induced oral mucositis in patients with HNC. The aim of this phase II exploratory study was to compare the incidence of oral mucositis in patients receiving rebamipide 2% and 4% liquids, or placebo.
Methods
Study design
This was a multicenter, randomized, double-blind, placebo-controlled, parallel-group, dose-ranging phase II study. This study is registered at ClinicalTrials.gov under the identifier NCT02085460 (the date of trial registration: March 11, 2014). The institutional review boards of the 20 participating institutions (Additional file 1) approved the study protocol. All study procedures were conducted in accordance with the 1964 Declaration of Helsinki and its later amendments, and in compliance with the Good Clinical Practice Guidelines specified by the Ministry of Health, Labour and Welfare of Japan.
Dynamic allocation was used to randomize patients, with stratification based on the purpose of CRT for HNC (definitive or post-operative) and primary site (oral cavity, nasopharynx, oropharynx, hypopharynx, or larynx). Subject enrollment and random study drug allocation were performed using the Interactive Web Response System. The subjects and investigators were kept masked to the treatment allocation until the end of the study. A sample size of 90 subjects was planned based on the feasibility of patient enrollment. Patients were randomly assigned to one of three groups, with 30 patients each: placebo, rebamipide 2% liquid, and rebamipide 4% liquid.
Patients
All study participants provided written informed consent at enrollment, 10 to 28 days prior to the initiation of CRT. Screening was performed based on the inclusion and exclusion criteria (Additional file 1). Briefly, patients between the ages of 20 and 75 years with histopathological diagnosis of primary tumor in the nasopharynx, oropharynx, hypopharynx, larynx, or oral cavity, regardless of the stage, scheduled to undergo definitive or postoperative CRT with ≥50 Gy irradiation to the buccal mucosa, floor of the mouth, tongue, or soft palate, with an Eastern Cooperative Oncology Group (ECOG) performance status (PS) score of 0 or 1, life expectancy of at least 3 months, without a history of chemotherapy, radiotherapy, or CRT for HNC, who could perform mouth washing and swallow fluids, and could attend follow-up visits, were included in this study.
Study treatment
The study drugs consisted of placebo (same formulation as rebamipide liquids) and rebamipide 2% and 4% liquids, which were given 6 times daily, preferably once after every meal, twice between meals, and once before bedtime. Patients were instructed to wash their mouth with 5 mL of the study drug for at least 30 s and then swallow it. The use of all other drugs for oral mucositis treatment, including oral ointment of corticosteroid, was prohibited. The only local treatments permitted in this study were oral aerosol spray for xerostomia, local antibiotics for the treatment of infection (e.g., amphotericin b or miconazole), and analgesic agents (e.g., xylocaine, opioid analgesics, and acetaminophen).
The treatment started 3 days prior to the initiation of CRT and continued for another 77 days. Cisplatin at 80–100 mg/m2 was administered thrice at 3-week intervals. Radiotherapy at ≤2.2 Gy/fraction was administered once daily, with 5 fractions per week, up to a total dose of ≥60 Gy. Withdrawal from the study was accepted before Day 77 if oral mucositis resolved completely, if oral mucositis did not develop 1 week after CRT completion, or if a patient requested to withdraw from the study.
Post-treatment examinations, including the assessment of adverse events and observation of oral mucositis, were performed 1 week after completion of CRT or 1 week after the patient decided to withdraw from the study. Subjects who underwent post-treatment examination were defined as subjects who completed the study.
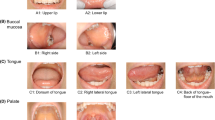
Oral assessment
Investigators who had undergone specific training assessed the severity of oral mucositis twice every week. To evaluate the severity of oral mucositis objectively, the clinical findings of the oral mucosa as well as functional disorders and symptomatic aspects were recorded in the Oral Mucositis Assessment Sheet (Additional file 1) by each investigator. Photographic documentation of the oral mucosa was also submitted by each investigator, 3 days before or 57 days after initiation of CRT, or at the time of withdrawal. The Oral Mucositis Assessment Sheet allows the relevant findings at each site in the oral cavity (10 sites in total) to be recorded separately. The Oral Mucositis Assessment Sheets and photographic documentation were then reviewed by the Oral Mucositis Evaluation Committee to grade the severity of oral mucositis according to the Common Terminology Criteria for Adverse Events (CTCAE) 3.0. Grade 3 for clinical examination was defined as “confluent ulcerations or pseudomembranes (bleeding with minor trauma),” and grade 3 for function/symptoms was defined as “symptomatic and unable to adequately ingest food or hydrate orally.”
Endpoints
The primary endpoint was the incidence of grade ≥ 3 oral mucositis assessed via clinical examination according to the CTCAE version 3.0. Secondary endpoints were time to onset of grade ≥ 3 oral mucositis and the incidence of functional impairment (grade ≥ 3) based on the Oral Mucositis Evaluation Committee evaluation. Exploratory endpoints were total cisplatin dose and compliance with radiotherapy during the study. Pharmacokinetics was assessed in terms of safety in the patients who ingested the drug. The AEs were assessed and classified based on the MedDRA system organ class and preferred term.
Statistical analysis
The full analysis set (FAS) comprised patients who received the study drug or placebo at least once and whose efficacy data were collected immediately after beginning the treatment. The safety set (SS) comprised those who received the study drug or placebo at least once and whose safety data were collected at least once after beginning the treatment. The per protocol set (PPS) consisted of patients who were compliant with the protocol. Patients who did not satisfy the inclusion/exclusion criteria, did not receive adequate radiotherapy, or did not comply with the prescription of combination therapy, or show drug compliance were excluded from the PPS.
The incidence of oral mucositis in each group was compared using the chi-square test. A step-down strategy was used for the between-group comparison, adjusting for multiplicity. Comparisons were made first between the rebamipide 4% and the placebo groups, and then between the rebamipide 2% and placebo groups. The Cochran-Armitage test was used as a trend test. All statistical analyses were performed using SAS 9.2 (SAS Institute Japan, Tokyo, Japan).
Results
Patient characteristics
Of 97 subjects randomized between April 2014 and August 2015, approximately 50% of the subjects had a primary tumor in the oropharynx, and approximately 20% of the subjects had a history of surgery for head and neck cancer. However, as a whole, the baseline characteristics of patients were well balanced between the treatment groups (Table 1).
Patient disposition
A total of 94 patients received the study drug and were included in the FAS and the SS. Sixty-two (66%) patients completed the study. The most frequent reason for study withdrawal in all three groups was patient request (22%, 33%, and 16% in the placebo, rebamipide 2% and 4% groups, respectively) (Fig. 1).
Incidence of oral mucositis
In the FAS, the incidence of grade ≥ 3 oral mucositis determined by clinical examination and assessed by the Oral Mucositis Evaluation Committee was 29% and 25% in the rebamipide 2% and 4% groups, respectively, compared with 39% in the placebo group (Fig. 2a). In a trend test, a decrease in the incidence of grade ≥ 3 oral mucositis was observed with an increasing concentration of rebamipide liquid; however, this decrease was not statistically significant (p = 0.2399). In the PPS, the incidence of grade ≥ 3 oral mucositis was 45% (n = 20), 36% (n = 22), and 27% (n = 30) in the placebo, rebamipide 2%, and rebamipide 4% groups, respectively, with no significant difference (p = 0.1779) (Fig. 2b). The incidence of functional impairment (Grade 3 or higher) was 29%, 36%, and 22% in the placebo, rebamipide 2% and 4% groups, respectively (Fig. 2c).
Time to onset of grade ≥ 3 oral mucositis
The rebamipide 2% and 4% groups showed a trend of delaying the time to onset of grade ≥ 3 oral mucositis as compared with the placebo group, although the difference between the groups was not statistically significant (Fig. 3). For instance, the proportion of patients who did not develop grade ≥ 3 oral mucositis by day 50 of treatment was 57.9% in the placebo group, whereas the proportion was 68.0% in the rebamipide 2% group and 71.3% in the rebamipide 4% group.
Treatment compliance
Oral retention and swallowing compliance for the study drugs were better in the rebamipide groups than in the placebo group. The proportion of patients whose oral retention and swallowing compliance was ≥80% was highest in the rebamipide 4% group, being 78.1%. In contrast, the proportion in the rebamipide 2% group was the same as that in the placebo group (58.1%). No significant differences in the total doses of cisplatin and the total radiation dose were observed among the groups (Table 2), suggesting that compliance with CRT was not influenced by the study drug.
Pharmacokinetics
Peak plasma concentration (mean ± standard deviation) of rebamipide on day 64 was 241 ± 160 ng/mL in the rebamipide 2% group (n = 11) and 568 ± 235 ng/mL in the rebamipide 4% group (n = 15) (Additional file 2: Fig. S1). No remarkable inter-patient variation was observed. The plasma concentration of rebamipide did not reach a sufficient level to induce the biochemical effects of rebamipide.
Safety
The incidence of AEs potentially related to the study drug was 16% (5/31), 26% (8/31), and 13% (4/32) in the placebo, rebamipide 2%, and rebamipide 4% groups, respectively. Nausea and vomiting were the most frequently reported AEs (Table 3). All patients experienced at least one AE and there was no significant difference in the incidence among the groups (data not shown).
Discussion
Basic oral care is considered common sense in the management of radiation-induced mucositis. However, a systematic oral care program alone is insufficient to decrease the incidence of severe oral mucositis in patients with HNC undergoing CRT [16]. Therefore, there is a strong demand for the development of prophylactic and therapeutic agents against oral mucositis. This phase II study evaluated the suppressive effect and safety of rebamipide liquid for CRT-induced oral mucositis in patients with HNC and assessed the optimal dose of rebamipide liquid.
As reported by the investigators and evaluated by the Oral Mucositis Evaluation Committee, we observed a decreased incidence of grade ≥ 3 oral mucositis in patients treated with rebamipide 2% and 4% liquids compared with those treated with placebo; however, these differences were not statistically significant. Furthermore, there was a trend towards a prolongation in the time to onset of grade ≥ 3 oral mucositis and a decrease in functional impairment in patients treated with rebamipide 4% liquid compared with those treated with placebo. These results may suggest a clinical benefit of rebamipide in reducing the incidence of severe oral mucositis induced by CRT. Recently, a small randomized, double-blind, placebo-controlled trial was conducted in patients with oral cancer treated with CRT at a total radiation dose of 40 Gy and concomitant weekly chemotherapy with docetaxel 10 mg/m2. The results revealed that the incidence of grade ≥ 3 mucositis (World Health Organization grade 3 or 4) in patients receiving rebamipide 0.1% was 33% (p = 0.036), compared with 83% in patients receiving placebo [9]. Even though the mean total radiation dose in our study was higher than that in their study, our patients had a lower incidence of grade ≥ 3 mucositis with rebamipide 4% liquid.
Previous reports showed that a rebamipide concentration ≥ 10 μM was required to exhibit its inhibitory effect on the production of radical and inflammatory cytokines [8, 9, 11, 12]. In this study, the plasma concentration in the rebamipide 4% group was 568 ± 235 ng/mL (1.53 μM). This suggests that the concentration reached after swallowing rebamipide, and its subsequent intestinal absorption, was insufficient to achieve a biologically active plasma concentration. We hypothesize that the local concentration of rebamipide achieved through mouth washing plays a major role in the clinical effect of rebamipide on oral mucositis. Furthermore, in patients who underwent definitive CRT, the response rate was 62.5%, 62.5%, and 69.2% in the placebo, rebamipide 2% and 4% groups, respectively. No new lesions were observed in all patients who underwent postoperative CRT at the point of the first scan. These results may suggest that rebamipide has no remarkable effect on local disease control despite its free radical scavenging effect on reactive oxygen species.
Although all patients reported at least one AE, there were no significant differences in the incidence of AEs among the groups. Therefore, no concerns were raised regarding the safety profiles of either rebamipide 2% or rebamipide 4% liquid. The safety profile of rebamipide suggests that ingestion of rebamipide 2% and 4% liquid formulations is safe.
The efficacy and safety profiles suggest that the optimal dose of rebamipide for the next phase of the study is rebamipide 4% liquid. Unfortunately, no statistically significant differences were observed between the rebamipide liquids and placebo with regard to the suppressive effect on CRT-induced oral mucositis. Several factors may explain this negative result. The first is the poor compliance in the rebamipide 2% and 4% groups, and the placebo group. The most common reason for discontinuation of treatment was related with the taste and smell of the formulation. For instance, in a recent patient survey of Japanese patients with liver cirrhosis, poor adherence to treatment with branched-chain amino acid granules was significantly associated with disinterest and distaste owing to the flavor and volume of the medication [17]. Their finding and ours suggest that patients are highly susceptible to the smell and taste of medications that require frequent intake. Therefore, the taste of the medication needs to be improved in the future. The second factor is the small sample size. A small sample size and poor compliance with the study drug may lead to statistically underpowered results. Further, in the present study, subjects who discontinued treatment were not followed-up after the treatment discontinuation. Therefore, there is a possibility that compliance with CRT and the incidence of grade ≥ 3 oral mucositis were not assessed accurately in the subjects who discontinued the treatment. Because of these factors and the lack of statistical significance, the benefit of rebamipide might be underestimated.
There were almost no differences in functional and symptomatic aspects between the placebo and rebamipide groups. The functional and symptomatic aspects are not only affected by mucositis, but also by a combination of multiple factors, including dysgeusia, salivary gland secretion, and swallowing dysfunction associated with irradiation of the pharyngeal constrictor muscles. Therefore, control of mucositis only by rebamipide may not be sufficient to prevent functional impairment.
Conclusions
Our study indicates that mouth washing with rebamipide liquid may be potentially effective and safe for patients with HNC receiving CRT. The efficacy and safety profiles suggest that 4% liquid is the optimal dose of rebamipide. Based on the present results and those of previous pilot studies [13, 14], we consider that it is highly relevant to conduct the next phase of study with a larger sample size.
Abbreviations
- AE:
-
Adverse event
- CRT:
-
Chemoradiotherapy
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- ECOG:
-
Eastern Cooperative Oncology Group
- FAS:
-
Full analysis set
- HNC:
-
Head and neck cancer
- PPS:
-
Per protocol set
- PS:
-
Performance status
References
Lalla RV, Bowen J, Barasch A, Elting L, Epstein J, Keefe D, et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer. 2014;120:1453–61.
Al-Ansari S, Zecha JA, Barasch A, de Lange J, Rozema FR, Raber-Durlacher JE. Oral mucositis induced by anticancer therapies. Curr Oral Health Rep. 2015;2:202–11.
Datamonitor Healthcare Market Briefs Product Code: BFHC0606: Oral Mucositis Challenging the Priorities of Cancer Therapy.
Naidu MU, Ramana GV, Rani PU, Mohan IK, Suman A, Roy P. Chemotherapy-induced and/or radiation therapy-induced oral mucositis--complicating the treatment of cancer. Neoplasia. 2004;6:423–31.
Le QT, Kim HE, Schneider CJ, Muraközy G, Skladowski K, Reinisch S, et al. Palifermin reduces severe mucositis in definitive chemoradiotherapy of locally advanced head and neck cancer: a randomized, placebo-controlled study. J Clin Oncol. 2011;29:2808–14.
Henke M, Alfonsi M, Foa P, Giralt J, Bardet E, Cerezo L, et al. Palifermin decreases severe oral mucositis of patients undergoing postoperative radiochemotherapy for head and neck cancer: a randomized, placebo-controlled trial. J Clin Oncol. 2011;29:2815–20.
Uchida M, Tabusa F, Komatsu M, Morita S, Kanbe T, Nakagawa K. Studies on 2(1H)-quinolinone derivatives as gastric antiulcer active agents. 2-(4-Chlorobenzoylamino)-3-[2(1H)-quinolinon-4-yl]propionic acid and related compounds. Chem Pharm Bull. 1985;33:3775–86.
Ogino K, Hobara T, Ishiyama H, Yamasaki K, Kobayashi H, Izumi Y, et al. Antiulcer mechanism of action of rebamipide, a novel antiulcer compound, on diethyldithiocarbamate-induced antral gastric ulcers in rats. Eur J Pharmacol. 1992;212:9–13.
Naito Y, Yoshikawa T, Tanigawa T, Sakurai K, Yamasaki K, Uchida M, et al. Hydroxyl radical scavenging by rebamipide and related compounds: electron paramagnetic resonance study. Free Radic Biol Med. 1995;18:117–23.
Arakawa T, Kobayashi K, Yoshikawa T, Tarnawski A. Rebamipide: overview of its mechanisms of action and efficacy in mucosal protection and ulcer healing. Dig Dis Sci. 1998;43(9 Suppl):5S–13S.
Kim CD, Kim HH, Hong KW. Inhibitory effect of rebamipide on the neutrophil adherence stimulated by conditioned media from helicobacter pylori-infected gastric epithelial cells. J Pharmacol Exp Ther. 1999;288:133–8.
Masamune A, Yoshida M, Sakai Y, Shimosegawa T. Rebamipide inhibits ceramide-induced interleukin-8 production in Kato III human gastric cancer cells. J Pharmacol Exp Ther. 2001;298:485–92.
Yasuda T, Chiba H, Satomi T, Matsuo A, Kaneko T, Chikazu D, et al. Preventive effect of rebamipide gargle on chemoradiotherapy-induced oral mucositis in patients with oral cancer: a pilot study. J Oral Maxillofac Res. 2011;2:1–8.
Yasuda T, Chiba H, Satomi T, Matsuo A, Kaneko T, Miyamatsu H. A pilot study of rebamipide-gargle for chemoradiotherapy-induced mucositis in oral cancer patients. Gan To Kagaku Ryoho. 2008;35:1157–61.
Nakashima T, Sako N, Matsuda T, Uematsu N, Sakurai K, Ishida T. Novel submicronized rebamipide liquid with moderate viscosity: significant effects on oral mucositis in animal models. Biol Pharm Bull. 2014;37:671–8.
Yokota T, Tachibana H, Konishi T, Yurikusa T, Hamauchi S, Sakai K, et al. Multicenter phase II study of an oral care program for patients with head and neck cancer receiving chemoradiotherapy. Support Care Cancer. 2016;24:3029–36.
Eguchi Y, Furukawa N, Furukawa T, Egashira Y, Hotokezaka H, Oeda S, et al. "weariness" and "unpleasantness" reduce adherence to branched-chain amino acid granules among Japanese patients with liver cirrhosis: results of a single-center cross-sectional survey. Hepatol Res. 2016 May 18; doi:10.1111/hepr.12745.
Acknowledgments
Medical writing and editorial support was provided by Dr. Keyra Martinez Dunn (Edanz Group Japan K.K.) and by ELMCOM™. The authors would also like to acknowledge the participation of Dr. Takao Ueno from the Department of General Internal Medicine, Dentistry, Oncologic Emergency, National Cancer Center Hospital, Tokyo, Japan; Dr. Sadamoto Zenda from the Division of Radiation Oncology and Particle Therapy, National Cancer Center Hospital East, Chiba, Japan; Dr. Tetsuhito Konishi from the Department of Dentistry, National Cancer Center Hospital East, Chiba, Japan; Dr. Takashi Yurikusa from the Dental and Oral Surgery, Shizuoka Cancer Center, Shizuoka, Japan; and Dr. Takeshi Kodaira from the Department of Radiation Oncology, Aichi Cancer Center Hospital and Research Institute, Nagoya, Japan. These five doctors were responsible for centrally reviewing data from each participating site.
Funding
This work was supported by Otsuka Pharmaceutical Co., Ltd., Japan. Medical writing and editorial support was funded by Otsuka Pharmaceutical Co., Ltd..
Availability of data and materials
The data are not published in publicly accessible repositories. Additional data and materials may be requested from the corresponding author.
Authors’ contribution
TY, TO, ST, KO, TF, KT, SI, IO, TU, NM, KM, HK, SU, KS, YF, YH, TB, HN, SH, MF and MT contributed to data acquisition and critically revised the manuscript. YN and YM contributed to data analysis and interpretation of the data, and revised the manuscript. TY contributed to interpretation of the data and writing of the first draft of the manuscript. MF, MT, YN. and YM. designed the study in collaboration with Department of Clinical Department, Otsuka Pharmaceutical. All authors read and approved the final manuscript.
Competing interests
T.Y, T.O, S.T, K.O, T.F, K.T, S.I, I.O, T.U, N.M, K.M, H.K, S.U, K.S, Y.F, Y.H, T.B, H.N, S.H, M.F, and M.T have received research grant from Otsuka Pharmaceutical Co., Ltd.; I.O, M.T, S.T and Y.H have received honoraria from Otsuka Pharmaceutical Co., Ltd.. Y.N and Y.M are employees of Otsuka Pharmaceutical Co., Ltd.
Consent for publication
Not applicable.
Ethics and approval and consent to participate
The institutional review boards of the 20 participating institutions (Additional file 1) approved the study protocol. All study procedures were conducted in accordance with the 1964 Declaration of Helsinki and its later amendments and in compliance with Good Clinical Practice Guidelines. All study participants provided written informed consent at enrollment, 10 to 28 days prior to the initiation of CRT.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional files
Additional file 1:
Supplementary Information: centers participating in the study; inclusion and exclusion criteria; oral mucositis assessment sheet. (DOCX 25 kb)
Additional file 2: Fig. S1.
Mean peak plasma concentrations of rebamipide. (DOCX 37 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yokota, T., Ogawa, T., Takahashi, S. et al. Efficacy and safety of rebamipide liquid for chemoradiotherapy-induced oral mucositis in patients with head and neck cancer: a multicenter, randomized, double-blind, placebo-controlled, parallel-group phase II study. BMC Cancer 17, 314 (2017). https://doi.org/10.1186/s12885-017-3295-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-017-3295-4