Abstract
Background
Neoadjuvant androgen deprivation therapy (ADT) has been suggested to confer several clinical benefits in patients with prostate cancer (PCa) undergoing transperineal prostate brachytherapy (TPPB). Unlike gonadotropin-releasing hormone (GnRH) receptor agonists, a GnRH antagonist such as degarelix can achieve castrate levels of testosterone without testosterone flare. However, normalization of serum testosterone levels following completion of neoadjuvant ADT in either form of treatment has never been compared in clinical trials.
Methods/Design
This is a single-center, open-label, randomized controlled study that will compare the efficacy and safety of degarelix with those of existing GnRH agonists combined with 125I-TPPB. A total of 56 patients with low/intermediate-risk clinically localized PCa will be enrolled and randomized to one of two treatment groups: the GnRH agonist group and the degarelix group. Patients in the GnRH agonist group will receive leuprorelin acetate or goserelin acetate, and those in the degarelix group will receive the initial dose of 240 mg as 2 subcutaneous injections of 120 mg each, and then 80 mg of maintenance doses every 4 weeks for 12 weeks. Those randomly assigned to the 12-week intervention period will subsequently undergo 48-weeks of follow-up after 125I-TPPB. The primary endpoint is defined as normalization of serum testosterone levels (>50 ng/dL) following completion of neoadjuvant ADT. All patients will be assessed every 4 weeks for the first 24 weeks, then every 12 weeks for the next 36 weeks after administrations of these drugs. Secondary endpoints are the proportion of normalized serum luteinizing hormone (LH) and follicle-stimulating hormone (FSH), the percent reduction in prostate specific antigen (PSA) compared with pretreatment levels, the percent reduction in total prostate volume (TPV) during neoadjuvant ADT, the percent increase in TPV after 125I-TPPB, the percent reduction in hemoglobin, serum alkaline phosphatase (ALP), changes in free testosterone and bone mineral content measurement, the proportion of patients who have serum testosterone levels over 50 ng/dL at 12 weeks following completion of neoadjuvant ADT, and the improvement of quality of life (QOL).
Discussion
The present study will provide additional insight regarding the benefit and potency of degarelix and will examine its potential as a new option for administration in neoadjuvant ADT.
Trial registration
Identification number: UMIN000015519.
Registration date: October 24, 2014.
Similar content being viewed by others
Background
Androgen deprivation therapy (ADT) that effectively reduces serum testosterone levels has been a core tool for treating metastatic and advanced prostate cancer (PCa) [1]. It is also an integral part of definitive treatment in combination with radiotherapy in the management of localized and locally advanced diseases [2, 3]. In Japan, 125I-transperineal prostate brachytherapy (TPPB) has been approved as one of the definitive options to treat localized PCa since 2003 [4]. Efficacy of neoadjuvant and adjuvant ADT using gonadotropin-releasing hormone (GnRH) agonists and anti-androgen with 125I-TPPB are currently tested in a phase III, multicenter, randomized, controlled trial (Seed and Hormone for Intermediate-risk Prostate Cancer (SHIP) 0804 study) [5].
Some studies have shown that patients treated with neoadjuvant ADT have fewer positive surgical margins but without improving biochemical control after radical prostatectomy [6, 7]. A significant reduction in total prostate volume (TPV) after 3 to 8-month neoadjuvant ADT has been reported [8–12]. Although GnRH agonists have been used for many years as ADT, they may be associated with a counterintuitive initial testosterone surge that can delay castration and which may stimulate PCa cells, resulting in potentially detrimental exacerbation of clinical symptoms particularly in advanced diseases [13]. An alternative approach to ADT has emerged in the form of a GnRH antagonist that involves the direct and rapid blockade of GnRH receptors, producing rapid suppression of testosterone and prostate specific antigen (PSA) levels. The effect occurs more rapidly than with GnRH agonists, without testosterone flare. Studies that evaluate the optimal agents and duration of ADT that produce outcomes with fewer adverse events are thus important.
Treatment with ADT is not avoid of adverse events, such as fatigue, diminished sexual function hot flushes and most importantly cardiovascular disease(CVD) which mainly due to a suppression of testosterone [14–16]. Many studies have shown testosterone recoveries after discontinuance of ADT. The extent and time to normalization of serum testosterone are relevant to the pre-treatment patients’ characteristics such as ages, treatment duration, pretreatment testosterone level, species, Gleason score and the level of dihydroxytestosterone [17–21]. However, most of those studies are retrospectively designed and inconclusive owing to the unavailability of pretreatment testosterone. Regarding adverse events, the results from previous studies are controversial and confusing. Shore ND et al. stated the potential advantages of GnRH antagonists in adverse events and oncological outcome [22], while Kimura T et al. questioned the real advantage of that drug [23]. In this study, we hypothesized 3 months GnRH antagonist to be more advantageous than GnRH agonists owing to more rapid recovery of serum testosterone after discontinuation. This may result in reduced incidence of ADT-related adverse events.
We describe our study protocol for low/intermediate-risk PCa, which is a single-center, open-label, randomized controlled study of a 12-week intervention period as neoadjuvant ADT followed by 48-weeks follow-up after 125I-TPPB. Japanese regulations specify the maximum permitted number of seeds for use, and the maximum intensity of radiation [5, 24]. To comply with these requirements, it is our common practice to administer neoadjuvant ADT even for low- to intermediate-risk PCa in patients with relatively large prostate glands (≥40 ml). In this study, we will evaluate temporal changes in serum testosterone levels and TPV before and after the discontinuation of short-term degarelix and GnRH agonist administration. The final goal of this study is to establish an appropriate strategy in neoadjuvant ADT for PCa without testosterone surge or microsurges by using short-term degarelix administration combined with 125I-TPPB.
Methods/Design
Aim of the study
To perform a comparative study between GnRH antagonist, degarelix and GnRH agonists on the recovery of serum testosterone levels for low/intermediate risk PCa after neoadjuvant ADT combined with 125I-TPPB. GnRH antagonist is hypothesized to have significantly more rapid testosterone recovery after discontinuation.
Study design
The present study is designed as a single-center, open-label, randomized controlled study to be performed in patients with low/intermediate-risk PCa. The outline of the study protocol is shown in Fig. 1. All patients are randomized to one of two treatment groups in which patients receive 12 weeks neoadjuvant therapy with either GnRH agonists or antagonist followed by 48 weeks of follow-up after 125I-TPPB.
Intervention
All eligible patients will be assigned randomly to one of two groups, the GnRH antagonist group and the GnRH agonist group. The initial dose of degarelix is 240 mg given as 2 subcutaneous injections of 120 mg each at 40 mg/ml in the abdomen. After the initial dose, the maintenance dose of 80 mg is given as one subcutaneous injection in the abdomen at 20 mg/ml, every 4 weeks. Leuprorelin acetate is administered subcutaneously once every 4 weeks at a dose of 3.75 mg, and goserelin acetate is administered subcutaneously in the abdomen once every 4 weeks at a dose of 3.6 mg.
Informed consent-ethics approval
This study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2000. All treatments for PCa are undertaken following written informed consent. Study approval was granted by the Jikei University Ethics Committee Institutional Review Board (approval No. 25–366 ((7501)), date June 2, 2014).
Technique of 125I-TPPB
125I-TPPB for all patients is administered using an ultrasound-guided technique with either the Mick applicator or intraoperatively built custom linked seed technique [5, 24, 25]. The implant is planned to deliver a dose of at least 144 Gy to the clinical target volume, which includes the prostatic gland and treatment margin [26]. Although individual technical aspects are institution-dependent, efforts are made to assure optimal quality control of the radiation dose based on our over 1,000 cases of experience [27]. Computed tomography images, taken at 2–5 mm intervals, are obtained 1 month after 125I-TPPB to determine the extent of edema. Dose-volume histograms for the prostate, urethra, and rectum are computed to obtain post-planning distribution data. V100 and D90 should be over 95 % and 144 Gy respectively for the clinically targeted volume [26, 28].
Definition of endpoints
Primary endpoints
The primary endpoint is defined as normalization of serum testosterone (>50 ng/dL) after discontinuation of GnRH agonists and antagonists.
Secondary endpoints
Secondary endpoints are: 1) the proportion of normalized serum luteinizing hormone (LH) and follicle-stimulating hormone (FSH), 2) the percent reduction in PSA compared with pretreatment levels, 3) the percent reduction in TPV during neoadjuvant ADT, 4) the percent increase in TPV after 125I-TPPB, 5) the percent reduction in hemoglobin and serum alkaline phosphatase, 6) changes in free testosterone and bone mineral content measurement, 7) the proportion of patients who have serum testosterone levels over 50 ng/dL at 12 weeks after completion of neoadjuvant ADT, 8) the improvement of QOL using the international prostate symptom score (IPSS) for lower urinary tract symptoms, 9) the improvement of QOL using the Expanded Prostate Cancer index Composite (EPIC), and 10) the improvement of QOL using the international index of erectile function (IIEF5). The assessment schedule is shown as Table 1.
Eligibility criteria-inclusion criteria
Patients must:
-
a.
Be at least 20 years of age, with a definitive histological diagnosis of PCa by needle biopsy.
-
b.
Be adaptable to 125I-TPPB.
-
c.
Have low/intermediate-risk localized PCa as follows: low-risk PCa: cT1a-T2a, Gleason score 2–6 and PSA < 10 ng/ml; intermediate-risk PCa: cT2b-T2c or Gleason score 7 or PSA 10–20 ng/ml (excluding Gleason score ≥ 8, PSA ≥ 20 ng/ml).
-
d.
Have TPV 35–60 ml.
-
e.
Agree in writing to participate in this clinical study after receiving adequate explanation.
Eligibility criteria-exclusion criteria
Patients are ineligible if they:
-
a.
Have previously received hormonal therapies including GnRH agonists, GnRH antagonists, antiandrogen agents, estrogen agents or orchiectomy for PCa.
-
b.
Are using 5α reductase inhibitors.
-
c.
Have severe asthma (e.g. use inhaled corticosteroid that is necessary for daily life), anaphylactic reaction, severe urticaria and complication or medical history of angioedema.
-
d.
Are sensitive to mannitol.
-
e.
Have multiple malignancies.
-
f.
Have alanine aminotransferase (ALT) ≥ 100 IU/L or total bilirubin ≥ 1.3 mg/dL.
-
g.
Are for any other reason considered by the investigator to be inappropriate for participation in the present study.
Tracking and monitoring adverse events
Patients will be monitored for unwanted symptoms and adverse events throughout the study period. Adverse events reported spontaneously by the patient or observed by physicians are similarly assessed and recorded. They all must be reported to the principal investigator and will be followed until they have abated or until a stable situation has been reached.
Data collection
This study design was chosen to ensure accurate, standardized, and high-quality data collection. All patients giving written informed consent to the study are asked to complete a short family history and epidemiology questionnaire. Electronic Data Capture (EDC) systems licensed by Pharma Consulting Group are used to collect clinical data in electronic format, with clinical data being obtained from patient medical records. A follow-up data form is completed by the investigator at week 4, 8, 12, 24, 36 and 48 after 125I-TPPB. These forms capture information regarding patient characteristics, serum testosterone, free testosterone, LH, FSH, serum ALP, hemoglobin, PSA, IPSS, IIEF5, EPIC, TPV, bone mineral content and adverse events.
Statistical consideration
Sample size
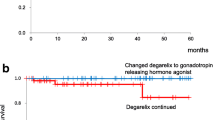
This study is designed to examine the superiority of GnRH antagonist over agonists in terms of testosterone recovery after its discontinuation. In the previous studies that investigated the time to normalization of testosterone levels after discontinuation of GnRH agonist administration, 50 % of patients with clinically localized PCa showed more than castration level testosterone (>50 ng/dL) within 4–5 months after 3-month GnRH agonist treatment [29, 30]. By contrast, the time to normalization of testosterone levels for degarelix treatment was 1.6 [31] or 2 months [32]. The hazard ratio calculated from both of median survival for time to normalization of testosterone levels was approximately 3.1. Assuming the hazard ratio of 3.1, it was found that a sample size of 26 patients per group would be necessary using the log-rank test with a significance level of 5 and power of 80 %. Assuming that 5 % dropout rate, the target sample was set at 28 patients per group (56 patients in total).
Statistical methods
Statistical analyses will be performed on an intention-to-treat basis. Serum testosterone levels after neoadjuvant ADT will be tested and normalization of serum testosterone levels above castration level (50 ng/dL) will be defined as event. Survival curves will be estimated using the Kaplan-Meier method. The log-rank test will be used to test the differences between the two groups. The hazard ratio will be estimated using the Cox proportional hazard model. The longitudinal change of QOL scores (IPSS, IIEF5 and EPIC) following 125I-TPPB will also be compared between groups. Patients will be evaluated for toxicity, graded according to the National Cancer Institute Common Toxicity Criteria version 4.0 (https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_40). All tests will be two-sided, and a p-value of 0.05 will be considered statistically significant.
Methods of recruitment and randomization
Recruiting began in 2015. Eligible patients are randomly assigned to one of two treatment groups through the EDC system. Randomization is done centrally using dynamic allocation [33] to obtain good between-group balance for factors including age category (<68/ ≥ 68) and the TPV (<45 mL/ ≥ 45 mL) before administrations of degarelix and GnRH agonists. The probability to be assigned to the group of lowest imbalance is set to 0.8.
Patient enrollment and anticipated completion of enrollment
Our current expectation is that the final patient will be enrolled by March, 2017; the study will be clinically completed by April, 2018 and results will be available during the third quarter of 2018.
Discussion
Some previous studies that have investigated the impact of ADT on intermediate- to high-risk PCa treated with 125I-TPPB suggested clinical advantages for the addition of ADT to 125I-TPPB [34, 35]. Lee et al. [34] reported that hormonal therapy consisting of LH-releasing hormone agonist combined with an antiandrogen for 3 months before brachytherapy and continued for 2–3 months afterward significantly improved 5-year actuarial freedom from biochemical failure, 79 % vs 54 % without hormonal therapy. Contrary to these reports, there are several reports showing that neoadjuvant ADT did not improve outcome for any risk group [36], and a large retrospective matched-pair analysis failed to show benefit of neoadjuvant ADT combined with either 125I-TPPB or 103Pd-TPPB [37]. Thus, there is still controversy regarding the impact of ADT on intermediate to high-risk PCa treated with 125I-TPPB and the most effective and safe treatment strategy remains to be established. It should be critical for designing the study protocol to take into consideration of the agents, the duration and the optimal timing of ADT combined with 125I-TPPB. Additionally, potential adverse events such as fatigue, diminished sexual function, and hot flushes, caused by this treatment should be taken into consideration. Although the optimal duration of concomitant ADT for intermediate-risk PCa when combined with 125I-TPPB remains unknown until the results from SHIP0804 study [5] are available, it may be possible to minimize the duration of ADT and its related toxicities for patients who achieve a rapid fall in testosterone and PSA after starting neoadjuvant ADT. Shortening this intervention period will be expected to reduce costs and side effects, and to improve QOL [38].
The agents that are mainly used as adjuvant ADT include estrogens, anti-androgen monotherapy, and combined androgen blockade using an anti-androgen plus a GnRH receptor agonist [1]. However, despite their efficacy, GnRH agonists have several drawbacks associated with their mechanism of action, including an initial testosterone surge. Compared to GnRH agonist, degarelix, a recently approved GnRH receptor antagonist, can achieve castration levels of testosterone much faster, without the risks associated with testosterone flare. Mason et al. recently conducted a comparative study for the use of degarelix and GnRH agonist in neoadjuvant ADT in combination with radiotherapy, and reported that a short-period such as 12-weeks of degarelix treatment achieved comparable efficacy with that of goserelin plus bicalutamide as neoadjuvant ADT before radiotherapy [39].
Note that our study protocol also focuses on the evaluation of temporal change of testosterone levels and TPV downsizing after withdrawal of degarelix, comparing it with that of existing GnRH agonists, in neoadjuvant ADT combined with 125I-TPPB. Although testosterone suppression is the primary outcome and it has been used as a surrogate endpoint during the approval of several hormonal treatments, only a few studies evaluated serum testosterone levels after the discontinuations of GnRH agonists [29, 30] and degarelix administrations [31]. Given that the TPV downsized with GnRH agonists, it might be expected that serum testosterone would be restored to normal levels immediately. However, suppression of testosterone levels remained and continued to lower even more than a half year after the discontinuation of GnRH agonist administrations [19, 40]. By contrast, the normalization of testosterone level to more than castration level after discontinuation of degarelix treatment was 1.6 [31] or 2 months [32]. Therefore, it is interesting to conduct a comparative study on the efficacy and safety for degarelix and GnRH agonists after the simultaneous discontinuation of these treatments, however, no such study has reported so far.
In conclusion, the present study is conducted to prospectively evaluate the efficacy and safety of degarelix, comparing it with the existing GnRH agonist, in neoadjuvant ADT for patients with low/intermediate-risk PCa. We expect that degarelix will prove to be an effective and well-tolerated agent, providing a useful addition to the hormonal armamentarium for PCa, and offering patients with hormone-sensitive disease a valuable alternative treatment option in neoadjuvant ADT.
Abbreviations
- ADT:
-
Androgen deprivation therapy
- EBRT:
-
External beam radiotherapy
- EDC:
-
Electronic data capture
- EPIC:
-
Expanded prostate cancer index composite
- FSH:
-
Follicle-stimulating hormone
- GnRH:
-
Gonadotropin-releasing hormone
- IIEF5:
-
International index of erectile function
- IPSS:
-
International prostate symptom score
- LH:
-
Luteinizing hormone
- PCa:
-
Prostate cancer
- PSA:
-
Prostate specific antigen
- QOL:
-
Quality of life
- TPPB:
-
Transperineal prostate brachytherapy
- TPV:
-
Total prostate volume
References
Mottet N, Bastian PJ, Bellmunt J, van den Bergh R.C.N, Bolla M, van Casteren NJ, P: European Association of Urology. Guidelines on prostate cancer. [https://uroweb.org/wp-content/uploads/1607-Prostate-Cancer_LRV3.pdf]
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guideline). Prostate cancer Version 3. [http://www.cus.cz/wp-content/uploads/2012/10/NCCN-C61-2014.pdf]
Payne H, Mason M. Androgen deprivation therapy as adjuvant/neoadjuvant to radiotherapy for high-risk localised and locally advanced prostate cancer: recent developments. Br J Cancer. 2011;105:1628–34.
Saito S, Nagata H, Kosugi M, Toya K, Yorozu A. Brachytherapy with permanent seed implantation. Int J Clin Oncol. 2007;12:395–407.
Miki K, Kiba T, Sasaki H, Kido M, Aoki M, Takahashi H, Miyakoda K, Dokiya T, Yamanaka H, Fukushima M, Egawa S. Transperineal prostate brachytherapy, using I-125 seed with or without adjuvant androgen deprivation, in patients with intermediate-risk prostate cancer: study protocol for a phase III, multicenter, randomized, controlled trial. BMC Cancer. 2010;10:572.
Soloway MS, Pareek K, Sharifi R, Wajsman Z, McLeod D, Wood Jr DP, Puras-Baez A, Lupron Depot Neoadjuvant Prostate Cancer Study Group. Neoadjuvant androgen ablation before radical prostatectomy in cT2bNxMo prostate cancer: 5-year results. J Urol. 2002;167:112–6.
Schulman CC, Debruyne FM, Forster G, Selvaggi FP, Zlotta AR, Witjes WP. 4-Year follow-up results of a European prospective randomized study on neoadjuvant hormonal therapy prior to radical prostatectomy in T2-3N0M0 prostate cancer. European Study Group on Neoadjuvant Treatment of Prostate Cancer. Eur Urol. 2000;38:706–13.
Whittington R, Broderick GA, Arger P, Malkowicz SB, Epperson RD, Arjomandy B, Kassaee A. The effect of androgen deprivation on the early changes in prostate volume following transperineal ultrasound guided interstitial therapy for localized carcinoma of the prostate. Int J Radiat Oncol Biol Phys. 1999;44:1107–10.
Kucway R, Vicini F, Huang R, Stromberg J, Gonzalez J, Martinez A. Prostate volume reduction with androgen deprivation therapy before interstitial brachytherapy. J Urol. 2002;167:2443–7.
Sanghani MV, Schultz D, Tempany CM, Titelbaum D, Renshaw AA, Loffredo M, Cote K, McMahon B, D’Amico AV. Quantifying the change in endorectal magnetic resonance imaging-defined tumor volume during neoadjuvant androgen suppression therapy in patients with prostate cancer. Urology. 2003;62:487–91.
Gleave ME, Goldenberg SL, Chin JL, Warner J, Saad F, Klotz LH, Jewett M, Kassabian V, Chetner M, Dupont C, Van Rensselaer S, Canadian Uro-Oncology Group. Randomized comparative study of 3 versus 8-month neoadjuvant hormonal therapy before radical prostatectomy: biochemical and pathological effects. J Urol. 2001;166:500–6. discussion 506–507.
Henderson A, Langley SE, Laing RW. Is bicalutamide equivalent to goserelin for prostate volume reduction before radiation therapy? A prospective, observational study. Clin Oncol (R Coll Radiol). 2003;15:318–21.
Thompson IM. Flare associated with LHRH-agonist therapy. Rev Urol. 2001;3 Suppl 3:S10–14.
Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, Lin X, Greenfield TK, Litwin MS, Saigal CS, Mahadevan A, Klein E, Kibel A, Pisters LL, Kuban D, Kaplan I, Wood D, Ciezki J, Shah N, Wei JT. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008;358:1250–61.
Chi KN, Nguyen PL, Higano CS. Androgen deprivation for prostate cancer: when and how, the good and the bad. Am Soc Clin Oncol Educ Book. 2013. doi:10.1200/EdBook_AM.2013.33.e176.
Albertsen PC, Klotz L, Tombal B, Grady J, Olesen TK, Nilsson J. Cardiovascular morbidity associated with gonadotropin releasing hormone agonists and an antagonist. Eur Urol. 2014;65:565–73.
Gulley JL, Figg WD, Steinberg SM, Carter J, Sartor O, Higano CS, Petrylak DP, Chatta G, Hussain MH, Dahut WL. A prospective analysis of the time to normalization of serum androgens following 6 months of androgen deprivation therapy in patients on a randomized phase III clinical trial using limited hormonal therapy. J Urol. 2005;173(5):1567–71.
Murthy V, Norman AR, Shahidi M, Parker CC, Horwich A, Huddart RA, Bange A, Dearnaley DP. Recovery of serum testosterone after neoadjuvant androgen deprivation therapy and radical radiotherapy in localized prostate cancer. BJU Int. 2006;97(3):476–9.
Nejat RJ, Rashid HH, Bagiella E, Katz AE, Benson MC. A prospective analysis of time to normalization of serum testosterone after withdrawal of androgen deprivation therapy. J Urol. 2000;164(6):1891–4.
Pickles T, Agranovich A, Berthelet E, Duncan GG, Keyes M, Kwan W, McKenzie MR, Morris WJ. British Columbia cancer agency, prostate cohort outcomes initiative. Testosterone recovery following prolonged adjuvant androgen ablation for prostate carcinoma. Cancer. 2002;94(2):362–7.
Tsumura H, Satoh T, Ishiyama H, Hirano S, Tabata K, Kurosaka S, Matsumoto K, Fujita T, Kitano M, Baba S, Hayakawa K, Iwamura M. Recovery of serum testosterone following neoadjuvant and adjuvant androgen deprivation therapy in men treated with prostate brachytherapy. World J Radiol. 2015;7(12):494–500.
Shore ND, Abrahamsson PA, Anderson J, Crawford ED, Lange P. New considerations for ADT in advanced prostate cancer and the emerging role of GnRH antagonists. Prostate Cancer Prostatic Dis. 2013;16(1):7–15.
Kimura T, Sasaki H, Akazawa K, Egawa S. Gonadotropin-releasing hormone antagonist: A real advantage? Urol Oncol. 2015;33(7):322–8.
Saito S, Kiba T, Aoki M, Ito K, Koga H, Yamashita T, Kitagawa S, Daimon T, Dokiya T, Yamanaka H. Japanese prostate cancer outcome study of permanent I-125 seed implantation (J-POPS study): Interim results of a prostate cohort study assessing efficacy, saftety and QOL. J Clin Oncol. 2008;26:(May 20 supple; abstr 16137).
Zauls AJ, Ashenafi MS, Onicescu G, Clarke HS, Marshall DT. Comparison of intraoperatively built custom linked seeds versus loose seed gun applicator technique using real-time intraoperative planning for permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2011;81(4):1010–6.
Nath R, Anderson LL, Luxton G, Weaver KA, Williamson JF, Meigooni AS. Dosimetry of interstitial brachytherapy sources: recommendations of the AAPM Radiation Therapy Committee Task Group No. 43. American Association of Physicists in Medicine. Med Phys. 1995;22:209–34.
Kido M, Kuruma H, Sasaki H, Miki K, Aoki M, Kimura T, Takahashi H, Kanehira C, Egawa S. Pulmonary metastases after low-dose-rate brachytherapy for localized prostate cancer. Korean J Urol. 2014;55:309–14.
Raben A, Chen H, Grebler A, Geltzeiler J, Geltzeiler M, Keselman I, Litvin S, Sim S, Hanlon A, Yang J. Prostate seed implantation using 3D-computer assisted intraoperative planning vs. a standard look-up nomogram: Improved target conformality with reduction in urethral and rectal wall dose. Int J Radiat Oncol Biol Phys. 2004;60:1631–8.
Oefelein MG. Time to normalization of serum testosterone after 3-month luteinizing hormone-releasing hormone agonist administered in the neoadjuvant setting: implications for dosing schedule and neoadjuvant study consideration. J Urol. 1998;160:1685–8.
Oefelein MG. Serum testosterone-based luteinizing hormone-releasing hormone agonist redosing schedule for chronic androgen ablation: a phase I assessment. Urology. 1999;54:694–9.
Clinical trial registration record with persistent identifier, NCT00117949 (2011): An Open-Label, Multi-Center, Ascending, Single Dose Study Investigating the Pharmacokinetics, Pharmacodynamics and Safety of FE200486. [http://www.clinicaltrials.gov/ct2/show/results/NCT00117949?term=degarelix+AND+CS06&rank=2§=X01256#all]. Accessed 24 June 2014.
Nobushita T, Ishizaki F, Takizawa I, Hoshii T, Hara N, Nishiyama T, Takahashi K, Akaza H. In Proceedings of the 100th Annual Meeting of the Japanese Urological Association: PP-0534 [Abstract]. Yokohama: The Japanese Urologucal Association; 2001.
Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics. 1975;31:103–15.
Lee LN, Stock RG, Stone NN. Role of hormonal therapy in the management of intermediate to high risk prostate cancer treated with permanent radioactive seed implantation. Int J Radiat Oncol Biol Phys. 2002;52:444–52.
Stone NN, Stock RG. Neoadjuvant hormonal therapy improves the outcomes of patients undergoing radioactive seed implantation for localized prostate cancer. Mol Urol. 1999;3:239–44.
Joseph J, Al-Qausieh B, Ash D, Bottomley D, Carey B. Prostate-specific antigen relapse-free survival in patients with localized prostate cancer treated by brachytherapy. BJU Int. 2004;94:1235–8.
Potters L, Torre T, Ashley R, Leibel S. Examining the role of neoadjuvant androgen deprivation in patient undergoing prostate brachytherapy. J Clin Oncol. 2000;18:1187–92.
Evers J, Kupper N, Kessing D, Davits R, Engelen A, Poortmans P, Mols F. No long-term effects of hormonal therapy preceding brachytherapy on urinary function and health-related quality of life among prostate cancer patients. Urology. 2010;76:1150–6.
Mason M, Maldonado Pijoan X, Steidle C, Guerif S, Wiegel T, van der Meulen E, Bergqvist PB, Khoo V. Neoadjuvant androgen deprivation therapy for prostate volume reduction, lower urinary tract symptom relief and quality of life improvement in men with intermediate- to high-risk prostate cancer: a randomised non-inferiority trial of degarelix versus goserelin plus bicalutamide. Clin Oncol. 2013;25:190–6.
Shahidi M, Norman AR, Gadd J, Huddart RA, Horwich A, Dearnaley DP. Recovery of serum testosterone, LH and FSH levels following neoadjuvant hormone cytoreduction and radical radiotherapy in localized prostate cancer. Clin Oncol. 2001;13:291–5.
Acknowledgements
We thank DOT international Co., LTD who provided data management service through Viedoc™ licensed by Pharma Consulting Group and medical writing service both funded by the Department of Urology, Jikei University School of Medicine.
Funding
This study is supported by a part of grant of Astellas Pharma Inc (Tokyo, Japan) and SHIP0804 (NCT00664456).
Availability of data and materials
The trial is ongoing and no data is available.
Authors’ contributions
KM and SE planned, coordinated and conducted the study. Medical care was provided by KM, HS, MK, MA and SE. KM provided randomization. HT contributed pathological diagnosis. KM and SE took part in conducting the study. The scientific program was planned by KM and SE, and carried out by KM. All authors read and approved the final manuscript. All other participants in this study contribute to the enrollment, treatment and follow up of patients.
Authors’ information
KM, HS, MK, SE are urologists, HT is a pathologist and MA is a radiation oncologist.
Competing interests
All of the authors, except one (S. E.), report they have no conflict of interest to disclose. One (S.E.) has received honoraria and travel expenses for speaking at an event organized by Astellas Pharma Inc (Tokyo, Japan), AstraZeneca K. K (Osaka, Japan), Takeda Pharmaceutical Co., Ltd. (Osaka, Japan), and Nihon Medi-Phycs Co., Ltd. (Tokyo, Japan).
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was performed according to the Helsinki Declaration of 1975, as revised in 2000. This protocol has been reviewed and approved by the Jikei University Ethics Committee Institutional Review Board (approval No. 25–366 ((7501)), date June 2, 2014). Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Miki, K., Sasaki, H., Kido, M. et al. A comparative study on the efficacies of gonadotropin-releasing hormone (GnRH) agonist and GnRH antagonist in neoadjuvant androgen deprivation therapy combined with transperineal prostate brachytherapy for localized prostate cancer. BMC Cancer 16, 708 (2016). https://doi.org/10.1186/s12885-016-2737-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-016-2737-8