Abstract
Background
It remains a matter of debate whether colorectal cancer resection in an emergency setting negatively impacts on survival. Our objective was therefore to assess the impact of urgent versus elective operation on overall and disease-free survival in patients undergoing resection for colorectal cancer by using propensity score adjusted analysis.
Methods
In a single-center study patients operated for colorectal cancer between 1989 and 2013 were identified from a prospectively maintained database. Median follow-up was 44 months. Patients with neoadjuvant treatment were excluded. The impact of urgent operation on overall and disease-free survival was assessed using both Cox regression and propensity score analyses.
Results
Of 747 patients with colorectal cancer, 84 (11 %) had urgent and 663 elective cancer resection. The propensity score revealed strongly biased patient characteristics (0.22 ± 0.16 vs. 0.10 ± 0.09; P < 0.001). In unadjusted analysis urgent operation was associated with a 35 % increased risk of overall mortality (hazard ratio(HR) of death = 1.35, 95 % confidence interval(CI):1.02–1.78, P = 0.045). In risk-adjusted Cox regression analysis urgent operation was not associated with poor overall (HR = 1.08, 95 %CI:0.79–1.48; P = 0.629) or disease-free survival (HR = 1.02, 95 %CI:0.76–1.38; P = 0.877). Similarly in propensity score analysis urgent operation did not influence overall (HR = 0.98, 95 % CI:0.74–1.29), P = 0.872) and disease-free survival (HR = 0.89, 95 %CI:0.68 to 1.16, P = 0.387).
Conclusions
This study provides evidence that worse oncologic outcomes after urgent operation for colorectal cancer are caused by clinical circumstances and not due to the urgent operation itself. Urgent operation is not a risk factor for colorectal cancer resection.
Similar content being viewed by others
Background
Colorectal cancer remains one of the most prevalent malignancies worldwide and a leading cause of cancer related death. Surgical resection including systematic lymphadenenctomy is the treatment of choice. Unfortunately, only half of these curatively operated patients will survive beyond five years. Up to 30 % of colorectal cancer patients are first diagnosed during emergency department presentation due to symptomatic disease [1–3]. Previous studies demonstrated that mortality rates are as much as four times higher for the immediate postoperative period in patients undergoing urgent operation. Results concerning long time survival are more conflicting [1–10]. However, many studies report on rather small sample sizes, state only immediate postoperative mortality rates or do not compare their results with a comparative group of electively operated patients [4, 9, 11–14]. Retrospective study design as well as a small percentage of patients presenting as an emergency make potential bias very likely. Randomisation could eliminate such bias but is not applicable for these symptomatic patients. Propensity score matching accounts for such bias in nonrandomized studies by eliminating different distribution of observed variables between two groups.
The objective of this study was to assess the impact of urgent surgery on oncologic outcomes in a large homogenic cohort of colorectal cancer patients. Both Cox proportional hazard regression analyses as well as propensity-scoring methods were used.
Methods
Data for the present retrospective study were extracted from the prospectively maintained cancer registry database at our institution, a tertiary care center in Switzerland. Overall, 830 patients undergoing colorectal cancer resection between 1989 and 2013 were identified. Eighty patients with neoadjuvant therapy were excluded as were three patients who were lost to follow-up. 747 patients remained for further analyses. Two groups were compared, 84 patients with urgent operation and 663 patients who did undergo elective cancer resection. The study was approved by the local ethical committee (Ethikkommission Nordwest- und Zentralschweiz). Follow-up data were collected from the treating general practitioner of the respective patients. Approval of data collection was obtained prior to surgery in years 1989–2005. For patients operated between 2006 and 2013 consent was obtained via letters of enquiry that were sent to these patients.
Data collection and definitions
Data on patients’ demographics, mode of presentation, operative details, postoperative mortality and histological results were collected from the patients case notes. All operations were performed or supervised by experienced colorectal surgeons. Definition of urgent surgery was used according to the NCEPOD classification of intervention (e.g., immediate (within minutes), urgent (<hours), expedited (<days) and elective (planned)) [15]. For the purpose of this study, patients undergoing immediate or urgent operations were grouped as urgent surgery. However, no patients underwent immediate surgery within minutes after emergency department presentation.
According to the postoperative staging adjuvant chemotherapy was administered routinely in patients with node positive disease. Follow-up and recurrence data could be almost entirely collected from our clinical records, or the bureau of vital statistics and the treating physician, respectively.
Statistical analyses
Statistical analyses were performed using the R statistical software (www.r-project.org). A two-sided p-value < 0.05 was considered statistically significant. Continuous data are expressed as means ± standard deviation. For comparing proportions, Chi-Square statistics and for comparing continuous variable, t-tests and Mann–Whitney U-tests were used as appropriate. Missing data were imputed using the random survival forest method [16].
First, the bias concerning elective versus urgent operation was assessed regarding age, gender, tumor localisation, tumor stage, and adjuvant therapy. The same set of covariates, including elective versus urgent operation were then assessed as putative prognostic factors for overall and disease-free survival in unadjusted and risk-adjusted Cox regressions, including a backward variable selection procedure from the full Cox regression model based on the Akaike’s information criterion. Moreover, a propensity score analysis as a superior and more refined statistical method of adjusting for potential baseline confounding variables was performed [17–20]. We used the “Matching” R package to perform a bipartite weighting propensity score analysis [21, 22]. The baseline risk profiles of the matched patients were compared to assure that no major differences in baseline patients characteristics persisted. The prognostic value of elective versus urgent operation for overall and disease-free survival was finally assessed in a stratified Cox regression analysis applying the subclasses and the weights obtained by the propensity score analysis.
Results
Patient characteristics and bias in urgent versus elective operation
747 patients with a median follow-up time of 44 months (range 0–247 months, mean 63.5 months) were eligible for the present analysis. 84 patients underwent urgent operation and 663 patients had elective cancer resection as defined above. The 30 day postoperative mortality rate was 5.2 % (35 of 663 patients) following curative resection and 8.3 % (7 of 84 patients) after urgent colorectal cancer resection. In more than 90 % of patients complete resection of the tumor could be achieved and about half of the patients presented with node positive disease (49.4 %, n = 369). Table 1 summarizes the characteristics of patients with urgent and elective cancer resection. In univariate analysis tumor localisation, perforation, resection status and number of extracted lymph nodes significantly differed between patients with urgent and elective operation (Table 1). After multivariable adjustment, number of extracted lymph nodes was associated with urgent surgery and perforation was an independent statistically significant predictor for urgent operation (Table 1). Other differences in the patient characteristics failed to reach the significance level.
Urgent operation as a prognostic factor for overall survival
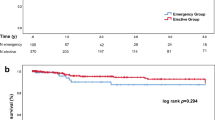
An unadjusted Cox proportional hazards regression analysis revealed urgent operation as a statistically significant prognostic factor with an approximately 35 % increased risk of overall mortality (HR of death = 1.35, 95 % CI: 1.02 to 1.78, P = 0.045) and an approximately 33 % increased risk of disease recurrence (HR of event = 1.33, 95 % CI: 1.02 to 1.74, P = 0.043) (Table 2). The five-year overall survival for patients with urgent operation was 35.9 % (95 % CI: 26.1 to 49.4 %) compared to 50.8 % (95 % CI: 47.0 to 54.9 %) in patients with elective operation (Fig. 1, left panel). The five-year disease-free survival for patients with urgent operation was 30.6 % (95 % CI: 21.6 to 43.3 %) compared to 45.0 % (95 % CI: 41.2 to 49.1 %) in patients undergoing elective operation (Fig. 1, right panel). When adjusting for potential confounding factors in risk-adjusted Cox regression analyses, urgent operation did not influence overall survival (HR of death = 1.08, 95 % CI: 0.79 to 1.48; P = 0.629) or disease-free survival (HR of event = 1.02, 95 % CI: 0.76 to 1.38; P = 0.877). Elective versus urgent operation was excluded from the full Cox regression models based on the change in the Akaike’s information criterion as these two variables did not show relevant predictive value for OS and DFS(Table 2).
Propensity score analysis
The propensity score for patients who underwent urgent operation was 0.22 ± 0.16 compared to 0.10 ± 0.09 in patients who underwent elective operation (P < 0.001), thus indicating a strong bias regarding the patient characteristics in the two groups. When performing the propensity score matching procedure, 42 patients with elective operation and one patient with urgent operation had to be excluded because their characteristics could not be matched with patients from the other group. Hence, the propensity score-matched analysis was based on 704 patients. After the matching procedure, the propensity score was virtually the same in the two patient groups (0.21 ± 0.15 vs. 0.21 ± 0.15, P = 0.969). Fig. 2 displays the change in the distribution of the propensity score due to the matching procedure. After adjusting the data according to the propensity score analysis, urgent versus elective operation did not influence overall survival (HR = 0.98, 95 % CI: 0.74 to 1.29), P = 0.872) and disease-free survival (HR = 0.89, 95 % CI: 0.68 to 1.16, P = 0.387) (Fig. 3).
Distribution of propensity scores before and after propensity score analysis. The left upper and lower panels show the distribution of the propensity scores for patients with urgent and elective operation before the matching procedure. The right upper and lower panels demonstrate the distribution of the propensity scores after bipartite propensity score matching
Discussion
The present study is the first study using both Cox regression analyses as well as propensity scoring methods to assess the impact of urgent versus elective operation on overall and disease-free survival in patients undergoing resection for colorectal cancer. This study provides evidence that patient characteristics are strongly biased regarding urgent operation. Optimal adjustment for this bias demonstrates no significant differences in overall and disease-free survival neither after multivariable Cox regression nor after propensity score-adjusted analyses.
In our study, 11 % of patients underwent urgent operation for colorectal cancer. This is comparable to other published investigations [3, 8, 23], although some studies report emergency presentation rates of up to 30 % [1, 2, 6, 10]. However, these studies did not clearly state whether patients were operated within hours or have been operated days after hospital admission. One of the strengths of our study is the clear definition of urgent surgery. This may account for the rather low percentage of patients in this group.
Urgent operation was not associated with poor survival in our study. Although unadjusted risk analysis did show reduced survival following urgent operation, this difference was no longer of statistical relevance after risk-adjustment. The increased risk observed in unadjusted analysis is clearly due to differences in baseline characteristics and not due to the urgent operation itself. Our results are supported by findings from recent studies which showed no statistical differences in long term survival [5, 7, 9, 10]. These reports differ from some larger studies that reported poorer survival for colorectal cancer patients presenting as an emergency [1–3, 6]. But it is not clear from these studies to what extent adjuvant therapy was administered and if so, differences were observed between the investigated groups. Furthermore the information if patients with neoadjuvant therapy were included in the respective studies is not provided. In our study, all patients receiving neoadjuvant treatment were excluded and administration of adjuvant chemotherapy was not different between the two groups. Adjuvant chemotherapy was confirmed as an independent favorable prognostic factor for overall survival as well as the number of harvested lymph nodes. Age, tumor location, resection status, tumor stage, and affected lymph nodes as well as tumor grade were confirmed to be independent prognostic factors for overall and disease free survival (Table 2). Besides these well known prognostic factors, patients receiving urgent surgery significantly more often presented with tumor perforation (Table 1). This is explained by the fact that peritonitis on the basis of perforated colorectal cancer is a common cause of emergency department presentation [24]. However, tumor perforation failed to be a prognostic factor for survival in our analysis. This is most likely based on the fact that not only free intraperitoneal rupture of the tumor was included in this group but also tumors showing localized perforation or those with penetration of the serosal surface in histological analysis.
Surprisingly, lymph node yield was higher in patients undergoing urgent operation in the present study (Table 1). Unfortunately, most of the published studies do not state the amount of resected lymph nodes [1, 2, 4, 8–12]. This is somewhat surprising, giving the fact that the number of harvested lymph nodes is crucial for staging of colorectal cancer patients because lymph node involvement represents the strongest prognostic factor and serves as the most important selection criterion for adjuvant chemotherapy [25]. Additionally, the number of surgically removed and pathologically assessed lymph nodes influences the staging accuracy and impacts overall survival [26, 27]. As a consensus standard, a minimum of 12 examined lymph nodes per patient is therefore recommended for accurate staging. In the present investigation 88.1 % of urgent surgery and 76.5 % of elective surgery patients had ≥ 12 lymph nodes resected (p = 0.016). This demonstrates that proper oncologic resection is achievable in urgent operations. Furthermore, the comparable quality of oncologic resection in both groups may be an explanation for the unobserved differences in overall and disease-free survival. It is well known from the literature that both, surgeon as well as hospital specific specialisation and caseload are important predictors for outcome after colorectal cancer resection what seems to apply also for these results [28, 29].
Our study has several limitations. First, this is a retrospective cohort study and not a randomized controlled trial. However, it is not possible to perform a randomized trial for this research question. A cohort study adopting Cox regression analyses as well as propensity-scoring methods probably represents the most appropriate and highest-evidence level study design. Second, while we did comprehensive risk-adjustment for observed confounders, potential bias due to unknown or unobserved confounders, such as American Society of Anaesthesiologist (ASA) grade, comorbidities and adherence to cancer related follow-up care, cannot be completely excluded. And last, all operations in this study were performed or supervised by experienced surgeons of a tertiary care center, what may also have influenced survival rates.
Conclusion
In summary, urgent colorectal cancer resection does not influence overall and disease-free survival after risk-adjusting in multivariable Cox proportional as well as propensity score analyses. The observed association between urgent operation and oncologic outcome is caused by differences in patient and tumor characteristics. Urgent operation itself is not a risk factor and colorectal cancer resection should therefore not be postponed for oncologic outcome reasons.
Abbreviations
- ASA:
-
American Society of Anaesthesiologist
- HR:
-
hazard ratio
References
McArdle CS, Hole DJ. Emergency presentation of colorectal cancer is associated with poor 5-year survival. Br J Surg. 2004;91(5):605–9.
Bass G, Fleming C, Conneely J, Martin Z, Mealy K. Emergency first presentation of colorectal cancer predicts significantly poorer outcomes: a review of 356 consecutive Irish patients. Dis Colon Rectum. 2009;52(4):678–84.
Oliphant R, Mansouri D, Nicholson GA, Mcmillan DC, Horgan PG, Morrison DS. Emergency presentation of node-negative colorectal cancer treated with curative surgery is associated with poorer short and longer-term survival. Int J Colorectal Dis. 2014;29:591–8.
Chiarugi M, Galatioto C, Panicucci S, Scassa F, Zocco G, Seccia M. Oncologic colon cancer resection in emergency: are we doing enough? Surg Oncol. 2007;16 Suppl 1:S73–7.
Biondo S, Martí-Ragué J, Kreisler E, Parés D, Martín A, Navarro M, et al. A prospective study of outcomes of emergency and elective surgeries for complicated colonic cancer. Am J Surg. 2005;189(4):377–83.
Anderson JH, Hole D, McArdle CS. Elective versus emergency surgery for patients with colorectal cancer. Br J Surg. 1992;79(7):706–9.
Smothers L, Hynan L, Fleming J, Turnage R, Simmang C, Anthony T. Emergency surgery for colon carcinoma. Dis Colon Rectum. 2003;46(1):24–30.
Cuffy M, Abir F, Audisio RA, Longo WE. Colorectal cancer presenting as surgical emergencies. Surg Oncol. 2004;13:149–57.
Coco C, Verbo A, Manno A, Mattana C, Covino M, Pedretti G, et al. Impact of emergency surgery in the outcome of rectal and left colon carcinoma. World J Surg. 2005;29(11):1458–64.
Chen Y-L, Chang W-C, Hsu H-H, Hsu C-W, Lin Y-Y, Tsai S-H. An evolutionary role of the ED: outcomes of patients with colorectal cancers presenting to the ED were not compromised. Am J Emerg Med. 2013;31(4):646–50.
Lee YM, Law WL, Chu KW, Poon RT. Emergency surgery for obstructing colorectal cancers: a comparison between right-sided and left-sided lesions. J Am Coll Surg. 2001;192(6):719–25.
Faiz O, Warusavitarne J, Bottle A, Tekkis PP, Clark SK, Darzi AW, et al. Nonelective excisional colorectal surgery in English National Health Service Trusts: a study of outcomes from Hospital Episode Statistics Data between 1996 and 2007. J Am Coll Surg. 2010;210(4):390–401.
Sjo OH, Larsen S, Lunde OC. Nesbakken a. Short term outcome after emergency and elective surgery for colon cancer. Colorectal Dis. 2009;11(7):733–9.
Odermatt M, Miskovic D, Siddiqi N, Khan J, Parvaiz A. Short- and long-term outcomes after laparoscopic versus open emergency resection for colon cancer: an observational propensity score-matched study. World J Surg. 2013;37(10):2458–67.
National Confidential Enquiry into Patient Outcome and Death. [accessed 2014 Oct 10]. Available from: http://www.ncepod.org.uk
Ishwaran BH, Kogalur UB, Blackstone EH, Lauer MS. Random survival forests. Ann App Statist. 2008;2(3):841–60.
Joffe MM, Rosenbaum PR. Invited commentary: propensity scores. Am J Epidemiol. 1999;150(4):327–33.
Rosenbaum PR. Model-based direct adjustment. J Am Stat Assoc. 1987;82(398):387–94.
Rosenbaum PR. Optimal matching for observational studies. J Am Stat Assoc. 1989;84(408):1024–32.
Rubin D. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127(8 Pt 2):757–63.
Hansen B. Optimal full matching and related designs via network flows. J Comput Graph Stat. 2006;15(3):609–27.
Sekhon JS. Multivariate and propensity score matching software with automated balance optimization: the matching package for R. J Stat Softw. 2011;42(7):1–52.
Merkel S, Meyer C, Papadopoulos T, Meyer T, Hohenberger W. Urgent surgery in colon carcinoma. Zentralbl Chir. 2007;132(1):16–25.
Biondo S, Parés D, Martí Ragué J, De Oca J, Toral D, Borobia FG, et al. Emergency operations for nondiverticular perforation of the left colon. Am J Surg. 2002;183(3):256–60.
Benson AB, Schrag D, Somerfield MR, Cohen AM, Figueredo AT, Flynn PJ, et al. American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol. 2004;22(16):3408–19.
Bilchik A, Nissan A, Wainberg Z, Shen P, McCarter M, Protic M, et al. Surgical quality and nodal ultrastaging is associated with long-term disease-free survival in early colorectal cancer: an analysis of 2 international multicenter prospective trials. Ann Surg. 2010;252(3):467–74. discussion 474–6.
Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, et al. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol. 2003;21(15):2912–9.
Archampong D, Borowski D, Iversen LH. Workload and surgeon’s specialty for outcome after colorectal cancer surgery (Review). Cochrane Database Syst Rev. 2012;3:CD005391.
Schrag D, Panageas KS, Riedel E, Hsieh L, Bach PB, Guillem JG, et al. Surgeon volume compared to hospital volume as a predictor of outcome following primary colon cancer resection. J Surg Oncol. 2003;83(2):68–78. discussion 78–9. 8.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
BW was responsible for the conception of the study, acquisition of data, analysis and interpretation of data, drafting the article and final approval. RW participated in the design of the study and performed the statistical analysis, drafted the article and was also responsible for final approval. MR was involved in data acqusition, was responsible for analysis and interpretation of the data and drafting the manuscript. RD contributed to the conception and design of the study, analysis and interpretation of the results, revised the manuscript and was responsible for final approval. UvH contributed to the conception and design of the study, analysis and interpretation of the results, revised the manuscript and was responsible for final approval. DO contributed to the conception and design of the study, was responsible for analysis and interpretation of the results, revised the manuscript critically and was responsible for final approval. CK was responsible for the conception and design of the study, analysis and interpretation of the results, revised the manuscript and was responsible for final approval. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Weixler, B., Warschkow, R., Ramser, M. et al. Urgent surgery after emergency presentation for colorectal cancer has no impact on overall and disease-free survival: a propensity score analysis. BMC Cancer 16, 208 (2016). https://doi.org/10.1186/s12885-016-2239-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-016-2239-8