Abstract
Background
Limited clinical data on real-world practice patterns are available for patients with metastatic/relapsed soft tissue sarcomas (STS). The primary objective of this study was to evaluate treatment patterns in patients with metastatic/relapsed STS following failure of prior chemotherapy by examining data collected from 2000 to 2011 from a major tertiary academic cancer center in the United States.
Methods
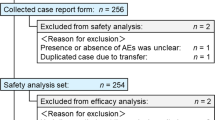
Medical records, including community-based referral records, from a tertiary cancer center for adult patients with metastatic/relapsed STS with confirmed disease progression who commenced second-line treatment between January 1, 2000 and February 4, 2011, and with at least 3 months of follow-up data following second-line treatment initiation, were retrospectively reviewed. Overall survival, time to progression, and clinician-reported tumor response were collected.
Results
A total of 99 patients (leiomyosarcoma, n = 48; synovial cell sarcoma, n = 7; liposarcoma, n = 5; or other histological subtypes, n = 39) received an average of four lines of treatment (maximum of 10). No consistent or dominant regimens were used in each treatment line beyond the second line. Median second-line treatment duration was 4.1 months (95% confidence interval, 3.0–5.0). Overall, 72 of 99 patients (73%) discontinued second-line treatment due to progressive disease. Median progression-free survival from initiation of second-line treatment varied across regimens from 2.0 to 6.6 months (overall median, 5.4 months).
Conclusions
Wide variations in treatment were evident, with no single standard of care for patients with metastatic/relapsed STS. Most patients discontinued second-line treatment due to progressive disease, often receiving additional systemic therapy with other drugs. These data suggest a high unmet need for more efficacious treatment options and improved data collection to guide practice among patients with relapsed/refractory STS.
Similar content being viewed by others
Background
Soft tissue sarcomas (STS) are rare cancers of mesenchymal cell origin that include more than 50 histological subtypes, as well as many more molecularly distinct entities [1,2]. STS can resemble the differentiation of various connective tissues, including muscle fat, nerves, vessels, stromal tissues, or bone. Gastrointestinal stromal tumor (GIST) is the most common subtype of all sarcomas [3]. Other STS categories include leiomyosarcomas, liposarcomas, and pleomorphic undifferentiated sarcoma (formerly malignant fibrous histiocytoma) [3,4]. The American Cancer Society estimated that 11 280 new cases of STS were diagnosed and 3900 patients died in 2012 in the United States [4]. Survival estimates for primary localized STS depend on many factors, including anatomic location and tumor grade [1]. Despite treatment, approximately 50% of patients with STS will ultimately develop recurrences or metastatic disease [5,6].
For patients with primary resectable STS, surgery is the mainstay of treatment [7,8]. However, for patients with metastatic STS, systemic therapy with conventional cytotoxic chemotherapy remains the main treatment modality. The National Comprehensive Cancer Network [7] and the European Society for Medical Oncology [8] recommend anthracyclines (alone or combined with other agents) in most cases as first-line treatment for metastatic STS, although first-line treatment recommendations may vary by histological subtype and previous treatment. Until recently, doxorubicin was the only agent formally approved by regulatory authorities for most types of metastatic/relapsed STS [9]. Pazopanib, a multitargeted tyrosine kinase inhibitor, is now also approved for use in patients following disease progression despite prior chemotherapy based on clinical studies documenting the benefit of disease control in this population [10,11]. Several other systemic agents, including ifosfamide, gemcitabine, dacarbazine, and trabectedin, are commonly used to treat metastatic/relapsed STS, but evidence supporting these therapies is largely limited to phase II trials [12-15].
Considering the wide range of STS histological subtypes, it is difficult to draw conclusions for specific entities based on generally uncontrolled trials of heterogeneous unselected patients with STS with a variety of different treatments. In addition, information in the published literature about treatment patterns and outcomes in STS is sparse. Studies in the United States [16] and internationally [6] showed a wide variety of systemic therapy administered in patients following failure of first-line chemotherapy.
Currently, there is no globally accepted standard based on high-quality evidence for patients with advanced STS following failure of prior chemotherapy to control advanced disease. The primary objective of this study was to evaluate treatment patterns in patients with metastatic/relapsed STS following failure of prior chemotherapy by examining data collected from 2000 to 2011 from a large tertiary academic cancer center in the United States. For the purpose of this study, STS will refer to sarcomas other than GIST. As a secondary objective, this study sought to gain a high-level assessment of the clinical effectiveness of various treatments given to patients with metastatic/relapsed STS.
Methods
This study was a retrospective analysis of patient medical records from the Dana-Farber Cancer Institute affiliated with Harvard Medical School in Boston, Massachusetts, USA, and was approved by the Dana-Farber Cancer Institute ethics committee.
All patients provided informed consent to approve the use of their medical records based on an institutional review board-approved protocol. Individual patient records were retrospectively reviewed in a sequential manner from this prospectively collected Sarcoma Center consented registry, based upon a diagnosis of metastatic/relapsed STS in patients aged 18 years or older who had received at least two lines of systemic therapies with initiation of second-line systemic therapy between January 1, 2000 and February 4, 2011. In addition, documentation of confirmed disease progression on or after first-line therapy and at least 3 months of data following commencement of a second-line therapy were also required.
Initially, data collection focused on patients with leiomyosarcoma; however, enrollment was subsequently expanded to include a broad range of STS histological subtypes. Patients were excluded if they had been diagnosed with GIST, bone sarcoma, or dermatofibrosarcoma protuberans, or had received treatment with pazopanib (including experimental use). Patient data were abstracted into an electronic case report form that was independently reviewed and queried. Unless otherwise specified, analyses presented here include all eligible patients and histological subtypes.
For the analysis, the variables collected from the medical records included patient demographics, histological subtype, treatment type and duration for all lines of systemic therapy, adverse events leading to treatment modifications (e.g. discontinuation), overall survival, clinician-reported tumor response rate, and progression-free survival (PFS; calculated as time to clinician-reported tumor progression or date of death, whichever came first). Clinician-reported responses were based on imaging results, if available, and/or clinical assessment notes by the treating physician. The treating oncologist’s written evaluation in the medical record was used to define a tumor response, rather than strictly limited to the use of formal oncology criteria such as Response Evaluation Criteria in Solid Tumors (RECIST) to define “objective responses.”
For the purpose of data analysis, patients were categorized according to the following types of second-line systemic therapy received: gemcitabine-based (including gemcitabine plus docetaxel), anthracycline-based (including anthracycline combined with other agents like ifosfamide), alkylating agents (including ifosfamide monotherapy), taxane-based, investigational agents (trabectedin, angiogenesis inhibitors), or other.
Continuous variables were summarized as means with standard deviation or median and range, as appropriate. Categorical variables were summarized by absolute frequencies and percentages. Time-to-event statistics were computed using Kaplan-Meier survival analyses.
Results
Of the 99 patients with metastatic/relapsed STS included in this analysis, the mean age was 51.9 years and 62% were women (Table 1). Approximately one-half of the patients (48%) had leiomyosarcoma, and about 67% of the patients in this referral center population had participated in a clinical trial at some point in their care.
The primary reason for treatment discontinuation of second-line therapy was progressive disease, which accounted for 73% of patients (Table 1). Only 10% were considered to have “completed” their course of therapy prior to developing progressive disease or discontinuing due to adverse events. Six percent of patients discontinued second-line therapy due to an adverse event.
One selection criterion for this study was that all patients were required to have had first- and second-line systemic therapies. This study population then received subsequent systemic therapy as follows: 78.8% had third-line, 49.5% had fourth-line, and 35.5% received fifth-line therapies. The maximum number of lines of systemic therapies received was 10. Figure 1A summarizes these treatments.
Systemic therapy treatment patterns. Treatment patterns according to (A) therapy line, and (B) second-line and third-line systemic therapy received according to histological subtype. *Patients were required to have at least one second-line systemic therapy for soft tissue sarcomas to be eligible for this study. Therefore, the first-line therapy distribution was based on those patients receiving at least one additional line of therapy (i.e. second-line or second-line plus additional lines of therapy).
For patients receiving first-line treatment, 44% received anthracycline-based therapy, and a significant fraction (28%) received gemcitabine-based regimens as first-line therapy (Figure 1A). For patients with leiomyosarcoma, no clear difference was seen in the initial treatment regimens received by patients with uterine leiomyosarcoma versus non-uterine leiomyosarcoma (Table 2).
For patients receiving second-line systemic therapy, gemcitabine-based therapies were commonly used (28%), with a similar percentage of patients receiving anthracycline-based therapies (24%) (Figure 1A). Second- and third-line treatment patterns according to histological subtype did not suggest any clear trends (Figure 1B).
Median PFS from initiation of second-line treatment varied somewhat across regimens, ranging from 2.0 to 6.6 months (overall median [95% confidence interval (CI)], 5.4 months [3.3–7.0]). Median PFS (95% CI) was 6.4 months (3.0–16.5) for gemcitabine-based therapy (n = 28), 5.8 months (2.3–8.0) for anthracycline-based therapy (n = 24), 3.7 months (1.4–13.6) for trabectedin (n = 13), 2.0 months (0.7–5.1) for alkylating agents (n = 12), 6.5 months (1.0–8.4) for angiogenesis inhibitors (n = 7), 4.7 months (2.0–7.0) for taxane-based agents (n = 3), and 6.6 months (2.4–18.1) for other agents (n = 7).
Median duration for second-line treatment across all regimens was 4.1 months (95% CI, 3.0–5.0). A clinician-documented response was observed in less than 20% of patients during any individual line of systemic therapy (Table 3). Just over one-third of patients (n = 38/99 [38%]) had a clinician-documented response to any line of chemotherapy. The mean duration of any line of therapy beyond first-line treatment was in the range of 2 to 6 months (Table 3), documenting the frequent incidence of treatment discontinuation or switching, possibly due to lack of efficacy, toxicity, patient intolerance, or other adverse factors.
The median overall survival from initial STS diagnosis was 4.8 years (95% CI, 3.6–5.6) in this highly selected referral center population of patients with metastatic/relapsed STS (Figure 2). The median overall survival from first diagnosis of metastatic STS was 3.3 years (95% CI, 2.4–4.5).
Discussion
The goals of this retrospective study were to assess treatment patterns for metastatic/relapsed STS and to identify whether any consistent “standard of care” for metastatic/relapsed STS could be identified in clinical practice from this population of patients generally treated in the community prior to referral to a tertiary care academic medical center in the United States. The only general trend identified was in the choice of initial treatment regimen. Most patients received anthracycline-based and gemcitabine-based therapy for first-line and second-line treatment, respectively. Notably, a high percentage of patients received gemcitabine-based therapy as first-line treatment of STS, and these patients generally received anthracycline-based therapy upon failure of the first-line regimen. However, no clear patterns for third-line therapy and beyond were noted. In addition, there was no clear link between histological subtypes and any particular treatment patterns.
A retrospective study describing international treatment patterns, the Sarcoma Treatment and Burden of Illness in North America and Europe (SABINE) study, similarly found that anthracycline-based regimens were most commonly used as first-line therapy in metastatic/relapsed STS [6]. The most common STS subtype in the SABINE study was leiomyosarcoma (46.5%). Doxorubicin monotherapy (34%) or an anthracycline (doxorubicin or epirubicin) combined with ifosfamide (30%) were identified as the most common first-line treatments in the SABINE study, which contrasts to more diverse first-line options in this study with 44% of patients receiving anthracycline-based therapy. The most common second-line treatment in the SABINE study was gemcitabine plus docetaxel (18.0%). This is similar to the 28% of patients who received gemcitabine-based therapy in the present study—who predominantly received gemcitabine plus docetaxel. The common use of gemcitabine in both studies could be related to the high proportion of patients with leiomyosarcoma in this study sample. The SABINE study found that trabectedin, which is approved for use in Europe but is only available as an investigational agent in the United States at specific centers, was commonly used after failure of first- and second-line therapy, which is consistent with results here. Similar to the observations noted in our study, the proportion of favorable responses to chemotherapy in the SABINE study declined with additional lines of treatment.
The majority of patients in the current study discontinued second-line treatment due to progressive disease and received additional lines of treatment. Less than 20% of these patients had a favorable response to treatment during any line of therapy (Table 3).
The median overall survival from diagnosis of metastatic disease was 3.3 years (39 months) in our study, which was considerably longer than the 10 to 18 months frequently reported in the literature for metastatic/relapsed STS [10,17,18]. However, the SABINE study reported a similar median overall survival from diagnosis of metastatic disease of 33.3 months [6]. It was not possible to assess the contribution of referral bias of more fit patients to tertiary care sarcoma centers versus the value of highly coordinated expert care delivered by sarcoma-dedicated teams, but these components could have contributed to longer survival. It is also likely that patients who go on to receive at least two rounds of chemotherapy have a better prognosis than those patients who might be too frail to receive chemotherapy. The high proportion of patients participating in clinical trials (67%) is also consistent with the hypothesis that this referral center patient population is likely to have fewer adverse clinical factors that could negatively influence survival.
Although data suggest that survival has somewhat improved in patients with sarcoma over the past two decades, the overall outcomes of metastatic STS remain poor. Italiano and colleagues [18] reported that overall survival of patients with metastatic/relapsed STS in the French Sarcoma Group database improved from 14 months (1987–1991) to 18 months (2002–2006). Multimodal treatment approaches may account for some improvement in survival over time [19,20]. Despite these improvements, a pressing need remains for more effective treatment options of these life-threatening diseases.
Effectiveness results from this study may not be fully representative of the broader metastatic/relapsed STS population given the selected patient population treated in a single tertiary sarcoma center. This retrospective analysis also used a practice-based approach to defining criteria for response rates and disease progression compared with the rigorously standardized criteria used in a clinical trial setting (e.g. RECIST), which may also confound direct comparisons between the effectiveness data from such a practice-based review and prospectively defined clinical research trials. In addition, the small number of patients included from a single tertiary care center led to wide CIs, particularly in the subtypes, and may limit the generalizability of these findings, although the data reviewed included community-based practice assessments of treatment regimens prior to referral to the academic center.
STS represents a diverse and varied collection of histological subtypes with distinct biological characteristics, natural histories, and responses to treatment. Because of the heterogeneity of patients receiving later lines of therapy, conclusions about these very limited subsets of the STS population should be made with care. Considering histological subtypes, the STS subtypes represented in our study do not reflect the natural distribution, and only leiomyosarcomas, which comprised 48% of our sample, were adequately represented. Of note, 39% of the population was derived from “other” subgroups, thus making assessment difficult and clouding the ability to identify uniform standards.
Conclusions
This retrospective analysis from a large academic cancer center shows wide variation in treatment patterns, including switching between anthracycline- and gemcitabine-based therapy in early lines and significant heterogeneity in decisions regarding later lines of treatment. The majority of patients discontinued second-line treatment due to progressive disease and often received additional lines of treatment, with frequent switching of treatment. A significant unmet medical need exists for effective treatments among patients with metastatic/relapsed STS.
Abbreviations
- GIST:
-
Gastrointestinal stromal tumor
- PFS:
-
Progression-free survival
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- SABINE:
-
Sarcoma Treatment and Burden of Illness in North America and Europe
- STS:
-
Soft tissue sarcoma
References
Jones NB, Iwenofu H, Scharschmidt T, Kraybill W. Prognostic factors and staging for soft tissue sarcomas: an update. Surg Oncol Clin N Am. 2012;21:187–200.
Benjamin R, Pisters Peter WT, Helman LJ, Bramwell Vivien HC, Rubin BP, O′Sullivan B. Sarcomas of Soft Tissue. In: Abeloff MD, Armitage JO, Niederhuber JE, Kastan MB, McKeena WG, editors. Clinical Oncology, vol. 4. 4th ed. Philadelphia, PA: Churchill Livingstone Elsevier; 2008. p. 2009–56.
Ducimetière F, Lurkin A, Ranchère-Vince D, Decouvelaere AV, Pèoc'h M, Istier L, et al. Incidence of sarcoma histotypes and molecular subtypes in a prospective epidemiological study with central pathology review and molecular testing. PLoS One. 2011;6:e20294.
American Cancer Society. Sarcoma - Adult Soft Tissue Cancer. Atlanta, GA: American Cancer Society, 2014. [http://www.cancer.org/acs/groups/cid/documents/webcontent/003138-pdf.pdf]
Coindre JM, Terrier P, Guillou L, Le Doussal V, Collin F, Ranchère D, et al. Predictive value of grade for metastasis development in the main histologic types of adult soft tissue sarcomas: a study of 1240 patients from the French Federation of Cancer Centers Sarcoma Group. Cancer. 2001;91:1914–26.
Leahy M, Garcia del Muro X, Reichardt P, Judson I, Staddon A, Verweij J, et al. Chemotherapy treatment patterns and clinical outcomes in patients with metastatic soft tissue sarcoma. The SArcoma treatment and Burden of Illness in North America and Europe (SABINE) study. Ann Oncol. 2012;23:2763–70.
National Comprehensive Cancer Network. Soft Tissue Sarcoma. NCCN Clinical Practice Guidelines in Oncology, 2012. [https://www.nccn.org/store/login/login.aspx?ReturnURL=http://www.nccn.org/professionals/physician_gls/pdf/sarcoma.pdf]
European Society for Medical Oncology/European Sarcoma Network Working Group. Soft tissue and visceral sarcomas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23 Suppl 7:vii92–9.
National Cancer Institute. Drugs Approved for Soft Tissue Sarcoma. National Cancer Institute, 2012. [http://www.cancer.gov/cancertopics/druginfo/softtissuesarcoma]
van der Graaf WT, Blay JY, Chawla SP, Kim DW, Bui-Nguyen B, Casali PG, et al. Pazopanib for metastatic soft-tissue sarcoma (PALETTE): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2012;379:1879–86.
US Food and Drug Administration. Votrient (Pazopanib) Tablets: For Treatment of Patients with Soft Tissue Sarcoma. FDA Oncologic Drugs Advisory Committee Briefing Document (NDA 22-465). March 2012. [http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/OncologicDrugsAdvisoryCommittee/UCM296303.pdf]
Demetri GD, Chawla SP, von Mehren M, Ritch P, Baker LH, Blay JY, et al. Efficacy and safety of trabectedin in patients with advanced or metastatic liposarcoma or leiomyosarcoma after failure of prior anthracyclines and ifosfamide: results of a randomized phase II study of two different schedules. J Clin Oncol. 2009;27:4188–96.
Maki RG, Wathen JK, Patel SR, Priebat DA, Okuno SH, Samuels B, et al. Randomized phase II study of gemcitabine and docetaxel compared with gemcitabine alone in patients with metastatic soft tissue sarcomas: results of sarcoma alliance for research through collaboration study 002 [corrected]. J Clin Oncol. 2007;25:2755–63.
van Oosterom AT, Mouridsen HT, Nielsen OS, Dombernowsky P, Krzemieniecki K, Judson I, et al. Results of randomised studies of the EORTC Soft Tissue and Bone Sarcoma Group (STBSG) with two different ifosfamide regimens in first- and second-line chemotherapy in advanced soft tissue sarcoma patients. Eur J Cancer. 2002;38:2397–406.
Garcia del Muro X, Lopez Pousa A, Martin J, Buesa JM, Martinez Trufero J, Casado A, et al. A phase II trial of temozolomide as a 6-week, continuous, oral schedule in patients with advanced soft tissue sarcoma: a study by the Spanish group for research on sarcomas. Cancer. 2005;104:1706–12.
Butrynski JE, Duh M, Fournier A, Moyneur E, Dial E, Neary MP, et al. Soft tissue sarcoma (STS): challenges in identification, treatment patterns, and costs of disease management in the US [abstract]. J Clin Oncol. 2008;26:10573. Abstract.
Howlader N, Noone A, Krapcho M, Neyman N, Aminou R, Altekruse SF, et al. SEER Stat Fact Sheets: Soft Tissue including Heart. In: SEER Cancer Statistics Review, 1975–2009. Bethesda, MD: National Cancer Institute; 2012; based on November 2011 SEER data submission, posted to the SEER web site; 2012. [http://seer.cancer.gov/statfacts/html/soft.html]
Italiano A, Mathoulin-Pelissier S, Cesne AL, Terrier P, Bonvalot S, Collin F, et al. Trends in survival for patients with metastatic soft-tissue sarcoma. Cancer. 2011;117:1049–54.
Bedi M, King DM, Charlson J, Whitfield R, Hackbarth DA, Zambrano EV, Wang D. Multimodality management of metastatic patients with soft tissue sarcomas may prolong survival. Am J Clin Oncol. 2014;37:272–7.
Penel N, Van Glabbeke M, Marreaud S, Ouali M, Blay JY, Hohenberger P. Testing new regimens in patients with advanced soft tissue sarcoma: analysis of publications from the last 10 years. Ann Oncol. 2011;22:1266–72.
Acknowledgments
All listed authors meet the criteria for authorship set forth by the International Committee for Medical Journal Editors. The authors wish to acknowledge Nancy Price, PhD, of AOI Communications, L.P., for medical writing and editorial assistance. The authors are also grateful to Francis Vekeman, MS, and Rajeev Ayyagari, PhD, at Analysis Group, Inc. for their assistance in data quality assurance and analysis. This work was supported in part by GlaxoSmithKline, Philadelphia, Pennsylvania, through a research grant to Analysis Group, Inc. and the Dana-Farber Cancer Institute. The Ludwig Center at Harvard also provided partial support for this work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
SCM and JD are employees of and hold stock in GlaxoSmithKline (GSK). MSD, CK, and FS are employees of Analysis Group, Inc., which provided consultancy to and received research funding from GSK for this and other studies. MPN was an employee of and held stock in GSK at the time of the study. GDD has served as a scientific consultant to GSK, and Dana-Farber Cancer Institute (GDD's primary employer) has received research funding from GSK. GDD has also provided unpaid expert regulatory testimony on behalf of GSK and Bayer. GDD has also been a consultant or advisor to ARIAD Pharmaceuticals, Bayer, Janssen, ZIOPHARM Oncology, Blueprint Medicines, Foundation Medicine, Kolltan Pharmaceuticals, Novartis, Pfizer, and Sanofi Oncology, and his institution has received research funding from Bayer, Novartis, Pfizer, Janssen, and Sanofi Oncology. GDD holds equity ownership in Kolltan Pharmaceuticals and Blueprint Medicines. All remaining authors have declared no conflicts of interests.
Authors’ contributions
MJW, MSD, CK, MPN, and GDD contributed to the study concept and design; MJW, LIA, and GDD participated in the acquisition of the data; MSD, CK, and FS performed the statistical analysis and MJW, LIA, MSD, CK, SCM, JD, and GDD analyzed and interpreted the data. All authors participated in the development, critical review, and editing of the manuscript. All authors have read and approved the final manuscript. As noted above, employees of the funding sources participated from the concept of the study through final approval for submission.
Michael J Wagner and Leo Ismaila Amodu contributed equally to this work.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wagner, M.J., Amodu, L.I., Duh, M.S. et al. A retrospective chart review of drug treatment patterns and clinical outcomes among patients with metastatic or recurrent soft tissue sarcoma refractory to one or more prior chemotherapy treatments. BMC Cancer 15, 175 (2015). https://doi.org/10.1186/s12885-015-1182-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-015-1182-4