Abstract
Background
The birth experience plays a pivotal role in the mother´s mental well-being and has a crucial effect on the mother-child bond. Unanticipated medical interventions, including fundal pressure, episiotomy, assisted vaginal delivery (AVD), or unplanned cesarean section (CS) during labor, may adversely affect the birth experience. The objective of this study is to identify factors contributing to the diminished evaluation of the birth experience after assessing the prevalence of unplanned obstetrical interventions in Germany.
Methods
For this cross-sectional analysis, 4000 mothers whose children were born 8 or 12 months before were asked about their birth experience via a paper-based questionnaire. Overall 1102 mothers participated in the study, representing a response rate of 27.6%. The revised Childbirth Experience Questionnaire (CEQ2) was used to measure the childbirth experience. In addition to descriptive and bivariate analyses using the Wilcoxon rank-sum test and Kruskal-Wallis-test, we calculated multivariate linear regression models for each dimension of the CEQ2.
Results
In general, the participants evaluated their childbirth experience favorably, assigning an average rating of 3.09 on a scale ranging from 1 to 4. Women who experienced fundal pressure, an AVD, or an unplanned CS rated their birth experience significantly worse compared to women who gave birth without interventions. Unplanned CSs received the lowest ratings for “personal capability” and “perceived safety,” and an AVD resulted in lower scores for “professional support” and “participation.” However, the interventions we studied did not account for much of the variation in how the childbirth experience plays out for different individuals.
Conclusion
Obstetric interventions have a significant effect on different dimensions of the birth experience. If a high level of birth satisfaction is to be achieved, it is important to know which dimension of satisfaction is affected by the intervention so that explicit measures, like fostering communication, participation or safety can be taken to promote improvement.
German Clinical Trial Register
DRKS00029214, retrospectively registered (Registration Date 22.06.2023).
Similar content being viewed by others
Introduction
The birth experience is a crucial factor that significantly impacts the development of postpartum stress disorders [1, 2], the mother-child bond [3, 4], the decision to have further children [5], and the choice of future birthing methods [6]. According to the FIGO statement on respectful maternity care, obstetric care should be supportive, individualized, and evidence-based [7]. The birth experience is significantly influenced by the self-efficacy experienced during birth, the possibility to actively participate in the decisions of the birth process and being well-informed and empowered [8,9,10]. This is also reflected in the fact that global birth satisfaction is made up of individual dimensions that can be measured and influenced individually [11].
Research has demonstrated that, obstetric interventions can influence the mother’s satisfaction with the birth experience, with fewer interventions generally leading to higher satisfaction levels [6, 12]. Obstetric interventions are often employed to improve maternal and/or fetal birth outcomes. To expedite delivery in cases of fetal distress, practitioners may utilize techniques such as fundal pressure [13], episiotomy [14], assisted vaginal delivery (AVD) using forceps or vacuum extraction (VE) [15], or unplanned cesarean section (CS) [16].
Fundal pressure, also known as the Kristeller maneuver, is applied by obstetricians/midwives to enhance the downward progression of the fetus through the birth canal by applying suprapubic pressure on the maternal abdomen [13]. A study from the US in 2005 found fundal pressure rates of 5% [17], and in Austria, fundal pressure was practiced in 23% of births [18]. While no data exist on the prevalence for Germany, the German guideline states that fundal pressure should be avoided if possible and, if done, only after strict indication [19]. From the mother’s perspective, pain during fundal pressure or a sense of powerlessness due to a lack of information or opportunities for participation has been reported [20, 21].
Although there is only weak evidence, an episiotomy can be performed to accelerate delivery in cases of suspected fetal hypoxia or to prevent obstetric anal sphincter injury in vaginal operative deliveries [22]. In Western countries, the episiotomy rate is below 30% on average and shows a downward trend, unlike in developing countries, which often still have episiotomy rates of over 70% [23]. Birthing mothers are often not informed about an episiotomy [24], and this could negatively influence the birth experience [25, 26].
Other medical procedures to expedite the birth of a potentially compromised fetus include AVD, and unplanned CS, whereby AVD seems preferred over unplanned CS from the mother´s perspective [27, 28]. The rate of AVD in Germany is around 7% [19], which is twice as high as in the US [27]. Studies indicate a negative association between AVD and birth satisfaction [29, 30]. Unplanned CS is another intervention that influences the birth experience not only by changing the mode of birth but also by possibly triggering a feeling of powerlessness and helplessness in the birthing person [31].
All the interventions referred to occur unplanned at a time when the health of the mother or fetus appears to be at risk or the birth process is protracted. At the same time performing a medical intervention shifts the physiological birth process to a medical procedure [32]. This vulnerable phase presents a particular challenge to caregivers in terms of providing respectful maternal care, as it is essential not only to ensure the safety of the mother and the fetus, but also to involve the mothers individually in medical decision-making and respect their personal needs [33].
Even though the influence of obstetric interventions on global satisfaction has already been investigated, there has not yet been a specific examination of the effects of obstetric interventions on the individual dimensions of satisfaction [34].
One approach to encompassing these aspects from the mothers’ perspective is through the utilization of the revised version of the Child Birth Experience Questionnaire (CEQ2), a validated survey instrument that explores four different dimensions of maternal satisfaction with the childbirth experience [35]. Knowledge of the impact of obstetric interventions on the individual dimensions of birth satisfaction, like perceived safety or participation is important for taking targeted countermeasures to ensure satisfaction with the birth experience.
The aim of this analysis is therefore to gain a better understanding of the association between unplanned medical interventions and the individual dimensions of maternal childbirth experiences (CEQ2).
Methods
The cross-sectional data are derived from a questionnaire survey of mothers 8 and 12 months after birth. This survey was conducted in cooperation with two statutory health insurance companies as part of the MAM-Care study (FKZ 01GY2110).
From all insured persons meeting the inclusion criteria, the health insurers drew a random sample of 4000 mothers who were invited to participate in the study. The inclusion criterion was the documented birth of a live-born child (ICD codes Z37.0 “Singleton, live-born,” Z37.2 “Twins, both live-born,” or Z37.5 “Other multiples, all live-born”) in a German hospital in May or September 2022. Consent to the anonymous survey was given implicitly by returning the questionnaire. No personal data were collected and no information from the health insurance company was linked.
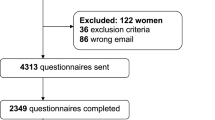
Overall 1102 mothers participated in the study, corresponding to a response rate of 27.6% (Fig. 1). Data from mothers who did not meet the inclusion criteria (birth in May or September 2022) were removed from the dataset. In addition, mothers with a planned CS and with contradictory information on the mode of birth were excluded from this analysis. In addition, 97 cases were removed due to missing values in the analysis variables. The data from two respondents who indicated their year of birth instead of their age were recoded.
Dependent variable
We used the revised version of the Childbirth Experience Questionnaire (CEQ2), a validated survey instrument that explores various dimensions of maternal satisfaction with the childbirth experience [11, 35]. The instrument comprises four domains: “Own Capacity,” “Professional Support,” “Perceived Safety,” and “Participation.” It has undergone international validation and has been employed in various studies [35,36,37]. The “Own Capacity” domain serves to document the woman’s coping mechanisms during the birthing process, her perceived level of control, and the alignment between her expectations and the actual experience [35]. This aspect is addressed in CEQ2 through the participation dimension, which assesses the woman’s level of feeling informed, her involvement in decisions, and the consideration of her opinion [35]. Another decisive factor in the decision-making process is how supported a woman feels by medical staff. This is addressed by the “professional support” dimension and contains respectful maternity care, empathy and privacy [35]. The aspect of “perceived safety” focuses on the woman’s emotions and her sense of security throughout the childbirth process. We applied the CEQ2 to assess the birth experience from the birthing persons` perspective [35]. To enable the international comparability of our results, we used the validated German translation [38] with the item structure of the original scale [35]. Furthermore, to ensure that mothers who have had a cesarean section also feel addressed, we have adapted the wording in consultation with the authors of the German translation and replaced “during labor and delivery” with “during the birth process” (CEQ2.0-R). The response options for the items in all four domains ranged from 1 (totally disagree) to 4 (totally agree) on a four-point Likert scale. Items worded in reverse have been recoded accordingly. All four dimensions of the scale are considered individually in the descriptive presentation and in the analyses (Tables 2 and 3). The individual dimensions comprise the mean values of the associated items. To calculate the total score, the values of the individual dimensions sub scores were summed up and then divided by four.
Independent variables
The medical interventions considered are fundal pressure, episiotomy, AVD (forceps and VE) and unplanned CS. There were yes and no response options to the questions “Was pressure applied externally to the abdomen by medical personnel during birth?” “Was an episiotomy performed during birth?“ and “How did you give birth: vaginal with forceps / vaginal with VE?“. The birth mode unplanned CS was assumed if CS was selected as the birth mode, and it was unplanned (i.e., occurred after the onset of labor or after induction).
In addition to the hypothesis-testing study variables, the following confounders were included in the analyses: maternal age, primipara vs. multipara, educational level (at least a university degree vs. Abitur [equivalent to at least 12 or 13 years of schooling [(High School)] vs. no Abitur), birth weight higher 3500 g and the child´s birth month (May vs. September 2022) to consider possible COVID-19 associated influences.
Statistical analysis
To explore the association of medical interventions with the reported birth experience, we assessed the impact of interventions on the individual dimensions of the CEQ2 using both the bivariate Wilcoxon rank-sum test and the Kruskal-Wallis test. Subsequently, linear regression models with robust estimators were built for each dimension of the CEQ2, since the normal distribution assumption was not fulfilled (Shapiro-Wilk test) and heteroskedasticity could not be excluded (test of Szroeter was negative, Breusch-Pagan and Cook-Weisberg test was positive). The analyses were conducted using the software Stata 16.1 and R 4.2.0 with the ggplot2, Gtsummary and jtools packages [39,40,41,42].
Results
The average age of the birthing person was 33.19 (SD 4.01). Table 1 shows the characteristics of the study population. The most frequently experienced intervention in the sample was fundal pressure (19%); a total of 12% of the respondents gave birth via an unplanned cesarean section, while 8% gave birth via instrumental birth. An episiotomy was performed on 14% of the respondents.
When interventions are examined based on individual dimensions (Fig. 3), it becomes apparent that women tend to rate their coping options lower for AVD and unplanned CS compared to those who experienced fundal pressure or an episiotomy (only women who have undergone an episiotomy without any other intervention are considered here). In all individual dimensions, the highest score was attained for vaginal birth without intervention. Regarding interventions, no consistent pattern was observed, with unplanned CS obtaining the lowest scores for “own capacity” and “perceived safety.” In contrast, for “professional support” and “participation,” AVD yielded lower scores than unplanned CS.
Table 2 shows the CEQ2 in its four dimensions. Overall, the person giving birth rated their birth experience as positive (mean 3.09 on a scale from 1 to 4), and only 5% of the respondents gave a CEQ2 score of 1.9 or below. A review of the individual dimensions reveals a high level of satisfaction with the professional support during birth and the opportunity to participate. The lowest rating was given to their coping skills (own capacity).
Regarding the overall assessment, the greatest satisfaction, and therefore, the highest were given for vaginal births without medical intervention (Fig. 2). The birth experience was rated worst for AVD and unplanned CS.
For the multivariate analyses, an initial model was computed for each dimension (Table 3, Additional file 1). In all the models, the association of the intervention compared to vaginal birth without intervention on the individual dimensions of the birth experience is calculated, while considering confounders such as maternal age, education, parity, birth weight and birth period. Across all the models, there is a significant negative association with AVD and fundal pressure. A similar pattern is observed for unplanned CS, with significant associations in all dimensions except “participation”.
Discussion
Our analyses aimed to compare obstetric interventions used in the second stage of labor and their effect on different dimensions of the birth experience.
On average, the respondents´ CEQ2 score was 3.09 on a scale from 1 to 4, with 5% of respondents having a CEQ2 score of 1.9 or less, and therefore, experiencing the birth of their child as very negative overall. Moreover, women who had none of the observed medical interventions rated both the entire birth and its sub-dimensions significantly better than women who had experienced one of the analyzed interventions.
Fundal pressure is known to have a negative association with the birth experience, and there has been ongoing controversy surrounding this issue. Although this intervention is internationally classified as potentially dangerous and ineffective and, according to the German guidelines, should not be exercised, if possible [19], it was performed in about one-fifth of births in our sample. Although the women who had experienced fundal pressure gave higher scores in all dimensions than women with AVD or CS, they rated all dimensions except professional support significantly worse than women who had no interventions. The reason for this may lie in the experienced self-efficacy, which tends to be perceived as less effective and lower in women who experienced fundal pressure [43]. Our results show that further efforts should be made to support womens´ self-efficacy (own capacity) during the birthing process. Based on the current evidence and the very critical voices that speak out against the use of fundal pressure [44], it can be questioned to what extent fundal pressure should still be applied at all, or at least efforts should be made to reduce the frequency of fundal pressure.
The impact of episiotomies on the individual dimensions of the CEQ2 is not evident in the multivariate analysis. From this perspective, it can be inferred that adequate support by the staff is already in place, or episiotomy may not be fundamentally relevant for the birth experience, as Bossano et al. pointed out [45]. However, it is important to note that the potential long-term effects of episiotomies are not considered in this analysis.
AVD and unplanned cesarean section have the strongest negative association with the CEQ2 score. This result is consistent with findings from other research using the CEQ2 [36, 46] and other research in this field [47, 48]. An examination of the individual dimensions reveals that women who had AVD rate their capacity and participation, in particular, as significantly worse than women who did not receive this intervention. Descriptive and bivariate analyses conducted by other researchers in similar studies have yielded comparable results [35, 36]. Therefore, the empowerment of women giving birth is particularly essential for a positive birth experience despite instrumental delivery [49]. However, cooperation and empowerment, in particular, interact with the medical staff providing care [49]. Compared to all other interventions, women who had an AVD rated both professional support and the assessment of having sufficient opportunities to participate during childbirth the lowest. This result is not consistent with the findings of a previous study that examined women with induced labor using the original CEQ, where caesarean section was rated as less favorable than AVD in all dimensions [37]. Although Germany´s AVD rate of 8% is lower than England´s [50], for example, data from the US (2.5%) show that a further reduction in the AVD rate is possible [51] whereby this may lead to an increase in the CS-rate.
Women who had an unplanned CS rated their overall birth experience slightly worse than women who had a AVD – even though there are only minimal differences between the two. This evaluation of the unplanned CS confirms findings from another study that report higher satisfaction ratings for instrumental birth when compared to emergency CS [47]. Based on the individual dimensions, the explanation for mothers’ bad experiences with CS lies particularly in perceived low self-efficacy (own capacity) and concerns about the safety of the baby and oneself (perceived safety). However, the moderating effect of the support experienced by the staff on satisfaction with the birth experience must always be considered [52]. Therefore, support from the staff can mitigate the negative effect of the cesarean birth mode. Our data show that women who had an unplanned CS (median 3.2) rated professional support better than women who had a AVD (median 3.0). Regarding participation, differences were observed between women who had experienced a AVD and those who had experienced a CS. From this result, it can be deduced that even in the case of CS, it was possible from the mothers’ point of view to participate and be part of decision-making processes. However, the differences regarding participation in vaginal birth are not significant in the multivariate model.
The results, particularly for AVD and CS, indicate that professional support, communication, empowerment and opportunities for participation are crucial for the woman giving birth. This particularly applies to the phase of childbirth, characterized by exhaustion and possibly concern for the health of the mother and/or fetus. This highlights the significance of raising awareness among obstetric personnel about the occurrence of traumatic procedures and equipping them with techniques to prevent adverse experiences and trauma. Overall, it is worth discussing why individual interventions per se play only a minor role in explaining the total birth experience. Our analysis demonstrates that negative experiences in one aspect of the CEQ2 can be compensated for by positive experiences in other areas. It is more meaningful to examine individual dimensions rather than the overall score. In practical terms, this implies that an intervention, does not necessarily result in a negative birth experience when the patient feels safe and is professionally supported by the staff. Furthermore, it is important to provide mothers with the opportunity to experience their own self-efficacy during interventions and to participate in the birth. This highlights that establishing contact, fostering involvement, providing support, and making efforts to alleviate anxiety can contribute to a positive birth experience despite interventions.
Limitations
Overall, with 1102 questionnaires returned a moderate response rate of 27.6% was achieved. The survey documents were sent to the participants by post, ensuring that all information was provided in written form to the respondents. This means that the distribution of the questionnaires did not depend on the clinical staff and all participants receive the same information, thus avoiding a selection bias trough in the maternity clinic. At the same time, however, this also means that no information about the maternity clinic is available and there is no additional possibility to motivate women to participate.
The two cooperating health insurance funds cover around 17.5% of people with statutory health insurance in Germany. The health insurance companies are one nationwide and one regional health insurance company, which only covers North Rhine and Hamburg. Compared to the population as a whole, only a few mothers with a low education level and a migration background were reached. It is possible that these vulnerable groups have more negative birth experiences than those with a higher education level and/or are native Germans.
A further limitation of the study is that the interventions included in the multivariate models only account for a small proportion of the variance. This is a hint that other influencing factors such as personality traits or hospital characteristics are important factors to consider.
Conclusion
Our analyses indicate that individual obstetric interventions have a limited impact on the variability in the birth experience. However, women who underwent unplanned CS or AVD expressed significantly higher dissatisfaction with the childbirth experience compared to those who gave birth vaginally without any intervention. Further research is warranted to explore the substantial unexplained variance, particularly in the realm of the effects of empowerment and support during childbirth. Our study underscores the significance of professional support and efforts to alleviate fears during childbirth. Developing strategies with the obstetrical team may be beneficial to minimize the prevalence of adverse birth experiences during necessary birth control interventions.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AVD:
-
Assisted Vaginal Delivery
- CS:
-
Cesarean Section
- CEQ:
-
Childbirth Experience Questionnaire
- CEQ2:
-
Childbirth Experience Questionnaire 2
- VE:
-
Vacuum Extraction
References
Czarnocka J, Slade P. Prevalence and predictors of post-traumatic stress symptoms following childbirth. Br J Clin Psychol. 2000;39:35–51. https://doi.org/10.1348/014466500163095.
Weigl T, Beck-Hiestermann FML, Stenzel NM, Benson S, Schedlowski M, Garthus-Niegel S. Assessment of Childbirth-related PTSD: Psychometric properties of the German version of the City Birth Trauma Scale. Front Psychiatry. 2021;12:731537. https://doi.org/10.3389/fpsyt.2021.731537.
Seefeld L, Weise V, Kopp M, Knappe S, Garthus-Niegel S. Birth experience mediates the Association between Fear of Childbirth and Mother-Child-Bonding up to 14 months Postpartum: findings from the prospective cohort study DREAM. Front Psychiatry. 2021;12:776922. https://doi.org/10.3389/fpsyt.2021.776922.
Eitenmüller P, Köhler S, Hirsch O, Christiansen H. The impact of Prepartum Depression and Birth Experience on Postpartum Mother-Infant Bonding: a longitudinal path analysis. Front Psychiatry. 2022;13:815822. https://doi.org/10.3389/fpsyt.2022.815822.
Gottvall K, Waldenström U. Does a traumatic birth experience have an impact on future reproduction? BJOG. 2002;109:254–60. https://doi.org/10.1111/j.1471-0528.2002.01200.x.
Shorten A, Shorten B. The importance of mode of birth after previous cesarean: success, satisfaction, and postnatal health. J Midwifery Womens Health. 2012;57:126–32. https://doi.org/10.1111/j.1542-2011.2011.00106.x.
International Federation of Gynecology and Obstetrics. FIGO Statement: Ethical Framework for Respectful Maternity Care During Pregnancy and Childbirth. 2021. https://www.figo.org/resources/figo-statements/ethical-framework-respectful-maternity-care-during-pregnancy-and-childbirth. Accessed 20 Nov 2023.
Larsen KE, O’Hara MW, Brewer KK, Wenzel A. A prospective study of self-efficacy expectancies and labour pain. J Reproductive Infant Psychol. 2001;19,3:203–14. https://doi.org/10.1080/02646830125493.
Berentson-Shaw J, Scott KM, Jose PE. Do self‐efficacy beliefs predict the primiparous labour and birth experience? A longitudinal study. J Reproductive Infant Psychol. 2009;27:357–73. https://doi.org/10.1080/02646830903190888.
Coates D, Thirukumar P, Henry A. Women’s experiences and satisfaction with having a cesarean birth: an integrative review. Birth. 2020;47,2:169–82. https://doi.org/10.1111/birt.12478.
Dencker A, Taft C, Bergqvist L, Lilja H, Berg M. Childbirth experience questionnaire (CEQ): development and evaluation of a multidimensional instrument. BMC Pregnancy Childbirth. 2010;10:81. https://doi.org/10.1186/1471-2393-10-81.
Salmon P, Drew N. Multidimensional Assessment of Women´s experience of Childbirth: relationship to Obstetric Procedure, Antenatal Preparation and Obstetric History. J Psychosom Res. 1992;36:317–27.
Hofmeyr GJ, Vogel JP, Cuthbert A, Singata M. Fundal pressure during the second stage of labour. Cochrane Database Syst Rev. 2017;3:CD006067. https://doi.org/10.1002/14651858.CD006067.pub3.
Young C, Bhattacharya S, Woolner A, Ingram A, Smith N, Raja E-A, Black M. Maternal and perinatal outcomes of prolonged second stage of labour: a historical cohort study of over 51,000 women. BMC Pregnancy Childbirth. 2023;23:467. https://doi.org/10.1186/s12884-023-05733-z.
Verma GL, Spalding JJ, Wilkinson MD, Hofmeyr GJ, Vannevel V, O’Mahony F. Instruments for assisted vaginal birth. Cochrane Database Syst Rev. 2021;9:CD005455. https://doi.org/10.1002/14651858.CD005455.pub3.
Hofmeyr GJ, Singata-Madliki M. The second stage of labor. Best Pract Res Clin Obstet Gynaecol. 2020;67:53–64. https://doi.org/10.1016/j.bpobgyn.2020.03.012.
Declercq ER, Sakala C, Corry MP, Applebaum S. October. Listening to Mothers II: Report of the Second National U.S. Survey of Women´s Childbearing Experiences. New York; 2006.
Schulz-Lobmeyr I, Zeisler H, Pateisky N, Husslein P, Joura EA. Fundal pressure during the second stage of labor: a prospective pilot study. Geburtshilfe Frauenheilkd. 1999:558–61.
Abou-Dakn M, Schäfers R, Peterwerth N, Asmushen K, Bässler-Weber S, Boes U et al. December. Vaginal Birth at Term - Part 2. Guideline of the DGGG, OEGGG and SGGG (S3-Level, AWMF Registry No. 015/083, 2020). Geburtshilfe Frauenheilkd. 2022;82:1194–248. https://doi.org/10.1055/a-1904-6769.
Rubashkin N, Torres C, Escuriet R, Dolores Ruiz-Berdún M. Just a little help: a qualitative inquiry into the persistent use of uterine fundal pressure in the second stage of labor in Spain. Birth. 2019;46,3:517–22. https://doi.org/10.1111/birt.12424.
Çalik KY, Karabulutlu Ö, Yavuz C. First do no harm - interventions during labor and maternal satisfaction: a descriptive cross-sectional study. BMC Pregnancy Childbirth. 2018;18:415. https://doi.org/10.1186/s12884-018-2054-0.
Laine K, Yli BM, Cole V, Schwarz C, Kwee A, Ayres-de-Campos D, et al. European guidelines on perinatal care- peripartum care episiotomy. J Matern Fetal Neonatal Med. 2022;35,25:8797–802. https://doi.org/10.1080/14767058.2021.2005022.
Clesse C, Lighezzolo-Alnot J, de Lavergne S, Hamlin S, Scheffler M. Statistical trends of episiotomy around the world: comparative systematic review of changing practices. Health Care Women Int. 2018;39,6:644–62. https://doi.org/10.1080/07399332.2018.1445253.
Meijer M, Brandão T, Cañadas S, Falcon K. Components of obstetric violence in health facilities in Quito, Ecuador: a descriptive study on information, accompaniment, and position during childbirth. Int J Gynaecol Obstet. 2020;148:355–60. https://doi.org/10.1002/ijgo.13075.
Soriano-Vidal FJ, Oliver-Roig A, Richart-Martínez M, Cabrero-García J. Predictors of childbirth experience: prospective observational study in eastern Spain. Midwifery. 2023;124:103748. https://doi.org/10.1016/j.midw.2023.103748.
Waldenström U, Borg IM, Olsson B, Sköld M, Wall S. The childbirth experience: a study of 295 new mothers. Birth. 1996;23:144–53. https://doi.org/10.1111/j.1523-536x.1996.tb00475.x.
Bahl R, Hotton E, Crofts J, Draycott T. Assisted vaginal birth in 21st century: current practice and new innovations. Am J Obstet Gynecol. 2023;230:3. https://doi.org/10.1016/j.ajog.2022.12.305.
Crossland N, Kingdon C, Balaam M-C, Betrán AP, Downe S. Women’s, partners’ and healthcare providers’ views and experiences of assisted vaginal birth: a systematic mixed methods review. Reprod Health. 2020;17:83. https://doi.org/10.1186/s12978-020-00915-w.
Thaels E, Meermans H, Beeckman K. What influences women’s experiences of childbirth in Flanders? - a quantitative cross-sectional analysis of the Babies Born Better survey. Midwifery. 2023;126:103810. https://doi.org/10.1016/j.midw.2023.103810.
Vogels-Broeke M, Cellissen E, Daemers D, Budé L, de Vries R, Nieuwenhuijze M. Women’s decision-making autonomy in Dutch maternity care. Birth. 2023;50:384–95. https://doi.org/10.1111/birt.12674.
Guittier M-J, Cedraschi C, Jamei N, Boulvain M, Guillemin F. Impact of mode of delivery on birth experience in first time mothers: a qualitative study. BMC Pregnancy Childbirth. 2014;14:254. https://doi.org/10.1186/1471-2393-14-254.
Jansen L, Gibson M, Bowles BC, Leach J. First do no harm: interventions during childbirth. J Perinat Educ. 2013;22,2:83–92. https://doi.org/10.1891/1058-1243.22.2.83.
Murphy DJ, Strachan BK, Bahl R, on behalf of the Royal College of Obstetricans Gynaecologists. Assist Vaginal Birth BJOG. 2020;127:e70–112. https://doi.org/10.1111/1471-0528.16092.
Viirman F, Hesselman S, Poromaa IS, Svanberg AS, Wikman A. Overall childbirth experience: what does it mean? A comparison between an overall childbirth experience rating and the Childbirth Experience Questionnaire 2. BMC Pregnancy Childbirth. 2023;23:176. https://doi.org/10.1186/s12884-023-05498-5.
Dencker A, Bergqvist L, Berg M, Greenbrook JTV, Nilsson C, Lundgren I. Measuring women’s experiences of decision-making and aspects of midwifery support: a confirmatory factor analysis of the revised Childbirth Experience Questionnaire. BMC Pregnancy Childbirth. 2020;20:199. https://doi.org/10.1186/s12884-020-02869-0.
Walker KF, Dencker A, Thornton JG. Childbirth experience questionnaire 2: validating its use in the United Kingdom. Eur J Obstet Gynecol Reprod Biol X. 2020;5:100097. https://doi.org/10.1016/j.eurox.2019.100097.
Place K, Rahkonen L, Verho-Reischl N, Adler K, Heinonen S, Kruit H. Childbirth experience in induced labor: a prospective study using a validated childbirth experience questionnaire (CEQ) with a focus on the first birth. PLoS ONE. 2022;17:e0274949. https://doi.org/10.1371/journal.pone.0274949.
Pedersen A, Sieprath K, Köhler M. Validierung der deutschen Übersetzung des Childbirth Experience Questionnaire (CEQ2). Diagnostica. 2021;67,2:87–97. https://doi.org/10.1026/0012-1924/a000267.
R Core Team. R: A language and environment for statistical computing. 2022.
Wickham H. ggplot2: elegant graphics for data analysis. New York: Springer; 2016.
Sjoberg DD, Whiting K, Curry M, Lavery JA, Larmarange J. Reproducible Summary tables with the Gtsummary Package. 2021;13:570–80. https://doi.org/10.32614/RJ-2021-053.
Long JA. jtools: Analysis and Presentation of Social Scientific Data. 2022.
Gudeta TG, Terefe AB, Muhamed AN, Mengistu GT, Sori SA. Perceived Childbirth Self-Efficacy and its Associated factors among pregnant women in South-Central Ethiopia. Int J Womens Health. 2023;15:1431–42. https://doi.org/10.2147/IJWH.S423784.
WHO. WHO recommendations: intrapartum care for a positive childbirth experience. Geneva: World Health Organization; 2018. License: CC BY-NC-SA 3.0 IGO.
Bossano CM, Townsend KM, Walton AC, Blomquist JL, Handa VL. The maternal childbirth experience more than a decade after delivery. Am J Obstet Gynecol. 2017;217:342e1. 342.e8.
Sigurðardóttir VL, Mangindin EL, Stoll K, Swift EM. Childbirth experience questionnaire 2 - Icelandic translation and validation. Sex Reprod Healthc. 2023;37:100882. https://doi.org/10.1016/j.srhc.2023.100882.
Falk M, Nelson M, Blomberg M. The impact of obstetric interventions and complications on women’s satisfaction with childbirth a population based cohort study including 16,000 women. BMC Pregnancy Childbirth. 2019;19:494. https://doi.org/10.1186/s12884-019-2633-8.
Hildingsson I, Karlström A, Nystedt A. Parents’ experiences of an instrumental vaginal birth findings from a regional survey in Sweden. Sex Reprod Healthc 4. 2013;4:3–8. https://doi.org/10.1016/j.srhc.2012.12.002.
Sjödin M, Rådestad I, Zwedberg S. A qualitative study showing women’s participation and empowerment in instrumental vaginal births. Women Birth. 2018;31(3):e185–9. https://doi.org/10.1016/j.wombi.2017.09.006.
NHS. NHS Maternity Statistics. England, 2022-23. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-maternity-statistics/2022-23. Accessed 6 Jun 2024.
Osterman M, Hamilton BE, Martin JA, Driscoll AK, Valenzuela CP. Births: final data for 2020. Natl Vital Stat Rep. 2022;70.
An S, Sun S. Effect of delivery mode on Chinese women’s maternal satisfaction: a moderated mediation model of support from medical staff and women’s self-assessment of health. J Psychosom Obstet Gynaecol. 2023;44(1):2238892. https://doi.org/10.1080/0167482X.2023.2238892.
Acknowledgements
We want to thank the mothers who contributed to our study and shared their intimate experiences with us. We also thank the two health insurance companies (AOK Rhineland/Hamburg and Techniker Krankenkasse) who strongly supported our survey.
Funding
Open Access funding enabled and organized by Projekt DEAL. This project was funded by the Federal Ministry of Education and Research (BMBF, fundingno.: 01GY2110). The funding body played no role in the design of the study nor of the collection, analysis, interpretation or writing of the manuscript. All stages of the study were entirely performed by the authors. See Author contributions for further details.
Author information
Authors and Affiliations
Contributions
Conceptualization: NS, AV; Methodology: NS, AV; Software: AV, JK; Validation: AV, JK; Formal Analysis: NS, AV, JK; Investigation: NS, AV, MO, LB, CO; Resources: NS; Data Curation: NS, AV; Writing – Original Draft Preparation: NS, AV; Writing – Review & Editing: NS, AV, CH, JK, MO, LB, CO; Visualization: JK, NS, AV; Supervision: CH, NS; Project Administration: AV, MO; Funding Acquisition: NS. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by and carried out in accordance with the institutional review board of the ethics committee of the Medical Faculty, University of Cologne (Vote No. 22-1260). Informed Consent was obtained from all the participants involved in the study. Study participants have been informed by written study information and implied consent to participate was assumed by the willingness to return the completed questionnaire to the IMVR. No directly identifying information was collected in the survey.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Volkert, A., Bach, L., Hagenbeck, C. et al. Obstetric interventions’ effects on the birthing experience. BMC Pregnancy Childbirth 24, 508 (2024). https://doi.org/10.1186/s12884-024-06626-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06626-5