Abstract
Background
There are few support interventions for women with fear of childbirth tailored towards type of fears and parity. To inform the future development of an acceptable and relevant intervention for women with severe fear of childbirth, primary objectives were to examine: (1) pregnant women’s experiences of and preferences for support and (2) barriers and facilitators to help-seeking. Secondary objectives were to examine if there are any differences based on pregnant women’s parity.
Methods
Pregnant women with a severe fear of childbirth in Sweden completed an online cross-sectional survey between February and September 2022. Severe fear of childbirth was measured using the fear of childbirth scale. Quantitative data were analysed using descriptive and inferential statistics and free answers were analysed using manifest content analysis. A contiguous approach to integration was adopted with qualitative and quantitative findings reported separately.
Results
In total, 609 participants, 364 nulliparous and 245 parous women, had severe fear of childbirth. The main category “A twisting road to walk towards receiving support for fear of childbirth” was explored and described by the generic categories: Longing for support, Struggling to ask for support, and Facilitating aspects of seeking support. Over half (63.5%), of pregnant women without planned or ongoing treatment, wanted support for fear of childbirth. Most (60.2%) pregnant women with ongoing or completed fear of childbirth treatment regarded the treatment as less helpful or not at all helpful. If fear of childbirth treatment was not planned, 35.8% of women would have liked to have received treatment. Barriers to help seeking included stigma surrounding fear of childbirth, previous negative experiences with healthcare contacts, fear of not being believed, fear of not being listened to, and discomfort of having to face their fears. Facilitators to help seeking included receiving respectful professional support that was easily available, flexible, and close to home.
Conclusions
Most pregnant women with severe fear of childbirth felt unsupported during pregnancy. Findings emphasise the need to develop individual and easily accessible psychological support for women with severe fear of childbirth, delivered by trained professionals with an empathetic and respectful attitude.
Similar content being viewed by others
Background
Fear of childbirth exists on a continuum, ranging from mild to severe and disabling [1,2,3]. When fear of childbirth during pregnancy is left untreated, there is an increased risk for pregnancy-related anxiety, which is further associated with impaired neuro-emotional development in newborns [4, 5]. High levels of anxiety during pregnancy may also interfere with a woman’s ability to cope with everyday life and preparations to become a mother [6]. Severe fear of childbirth can lead to avoidance of pregnancy, and is more prominent among foreign born woman living in Sweden [7]. Fear of childbirth is a common reasons for requesting a caesarean section (CS) [1,2,3], and associated with an increased use of epidurals during labour [8, 9], having a negative birth experience [10,11,12,13], and postpartum psychological ill-health [12, 14], that can negatively impact the mother-child relationship [15].
Most pregnant women prefer their partner to be present during childbirth [16] with their involvement contributing to positive outcomes for the mother [17], with women feeling empowered by having a supportive partner [18]. In Sweden, 98% of prospective fathers participate during the birth [19]. However, lack of partner support [18, 20], partner violence, and women’s dissatisfaction with the partnership [8] are associated an increased risk of fear of childbirth.
Despite these adverse impacts, fear of childbirth is an underrecognised and underprioritised healthcare issue due to factors such as lack of consensus of the definition of fear of childbirth [6], lack of structured treatments [21], and lack of routine screening during pregnancy [11, 22]. Psychological interventions including psychoeducation [PE] [23], cognitive behavioural therapy [CBT], enhanced midwifery care [24], psychodynamic therapy [PDT], and eye movement desensitization and reprocessing therapy [EMDR] [25,26,27], have been found to reduce fear of childbirth in pregnant women. However, the evidence base has been criticised due to poor methodological quality [24], and primarily focusing only on depression as an outcome [28]. Further, research suggests a need to develop fear of birth interventions that are better tailored to women’s individual needs [18]. Additionally, the majority of studies have not focused on pregnant women experiencing severe fear of childbirth [26, 29]; thus, there is a need for more research examining the experiences of and preferences for support in this population.
Fear of childbirth in relation to parity
Both nulliparous and parous pregnant women may experience fear of childbirth [30]. Research suggests fear of childbirth in nulliparous women may stem from general fears starting in adolescence or early adulthood or prior history of anxiety disorders [31], whereas parous women with a previous traumatic birth experience are more likely to experience fear of childbirth during their next pregnancy [32]. Nulliparous women and parous women with a severe fear of childbirth may have different experiences and need different types of psychological support [12].
The Swedish context for supportive counselling
In Sweden, approximately 110 000 women give birth annually [33], where 20% of expectant mothers suffer from severe fear of childbirth [34]. In 2020, approximately 10% of all pregnant women in Sweden received supportive counselling related to fear of childbirth [12]. Supportive counselling is delivered by a midwife, sometimes in cooperation with an obstetrician, psychologist, counsellor, psychiatrist, or behavioural therapist [35]. Supportive counselling has been found to help women feel safe and increase confidence in giving birth, and is related to a positive birth experience [9, 36]. Standard referral procedures for supportive counselling vary between Swedish antenatal care units. Midwives may ask women a general question about fear or use a screening instrument to identify fear of childbirth. Whilst some antenatal care units follow local referral guidelines, others require women to self-refer to a counselling unit [9]. Despite all antenatal clinics in Sweden offering supportive counselling for women with fear of childbirth [3], the structure and content of the counselling and its organisation differs greatly between clinics [3, 9].
Research aim and objectives
The overall aim was to explore pregnant women with severe fear of childbirth and their preferences for support to inform the future development of a psychological intervention for severe fear of childbirth. primary objectives were to examine: (1) pregnant women’s experiences of and preferences for support and (2) barriers and facilitators to help-seeking. Secondary objectives were to examine if there are any differences in experiences of and preferences for support and barriers and facilitators based on pregnant women’s parity.
Methods
Design
A cross-sectional concurrent mixed-methods design [37], using an anonymous, online survey hosted by REDCap (Research Electronic Data Capture) [38], following the Checklist for Reporting Results of Internet E-Surveys [39]. Ethical approval was obtained from the regional ethical board in Sweden (Nr: 2021–03759.)
Participants
Eligible participants were (1) 18 years of age or older; (2) self-identified as a pregnant woman, either nulliparous (i.e. a woman who has not given birth to a child) or parous (i.e. a woman who has given birth to any number of children); (3) living in Sweden; (4) able to read and understand Swedish or English enough to complete an online survey; and (5) had fear of childbirth (≥ 60 on the Fear of Birth Scale.
Recruitment
A convenience sample was recruited from February 2022 to September 2022 via a number of recruitment strategies:
Hospital recruitment
Six hospitals across five counties in Sweden (Malmö, Karlstad, Stockholm, Uppsala, and Umeå) supported recruitment. Potential participants were informed about the study by a midwife either at the end of an appointment in the counselling clinic or at the routine ultrasound. Potential participants were handed a study information brochure with a survey weblink and QR (Quick Response) code for the survey (Appendix I).
Social medical advertisements
Advertisements were posted on social media (i.e., Facebook and Instagram), on websites, and in newsletters of non-profit organisations for pregnant women, groups for men and parents, and paid Facebook advertisements via an advertising company in collaboration with Uppsala University. Paid Facebook advertisements were used for approximately four weeks (July-August 2022). Study advertisement examples can be found in Appendix II. A survey web link and/or QR code was provided at the bottom of the advertisement.
Procedure
Informed consent
Potential participants were informed about the study purpose via study information presented on REDCap. Study information stated participation was voluntary and would not affect their clinical care, and answers could be anonymous. Participants were advised that by clicking “yes” they consented to participate.
Survey
The survey comprised of three sections (1) Sociodemographic and obstetric characteristics including the Fear of Birth Scale (15 items) [15] (2) preferences for and experiences of support (9 items) [18] and (3) barriers and facilitators to help-seeking (9 items) [40] (Appendix III). Participants were able to review and/or change answers by using a back button. Survey functionality was tested by the research team. IP addresses were not stored in order to maintain participant anonymity.
Fear of birth scale
The Fear of Birth Scale is a self-report scale consisting of two 100 mm Visual Analogue Scales that are summed and then averaged. Participants answer the question “How do you feel right now about the approaching birth?” and by placing a mark the two scales (scale one ranges from calm to worried, and scale two ranges from no fear to strong fear). The cut-off point ≥ 60 as severe fear of childbirth and < 60 as no, mild or moderate fear of childbirth was used in accordance with previous research [14, 15, 34, 41, 42].
Open questions
Three open questions with free-text responses were included [37]: (1) “If no treatment is planned, would you like to receive treatment/support for your fear of childbirth?” and “If yes, please state why?”; (2) “What obstacles have you experienced in seeking help for your fear of childbirth?” and (3) “What would make it easier to seek help for fear of childbirth?”
Pilot testing
Research team members pilot-tested the online survey. After small logic errors and item-wording changes were made, the survey was pilot tested with three pregnant women prior to data collection to ensure the survey was understandable and acceptable. Feedback was provided via email or phone, and only minor wording changes were suggested and to clarify some items.
Data analysis
Quantitative
We created several dichotomous variables to facilitate cross-tabulation. Age was recoded into two groups (1) < 35 years and (2) ≥ 35 (defining advanced maternal age, and reported to be associated with various pregnancy complications) [43, 44]. Relationship status was recoded into two groups (1) Cohabiting with a partner (married or living with someone) and (2) Not cohabiting (single or with a partner but not living together). Education was recoded into two groups (1) primary or high school (9–13 years) and (2) at least some or more college/university. Country of birth was recoded as (1) Sweden or (2) Other. Partner support was recoded into two groups (1) more partner support (those who responded “to a very large extent” or “to a fairly large extent”) and (2) less partner support (those who responded “to a small extent” or “not at all”). To be considered parous, participants needed to state “yes” that they had given birth to a child previously. Gestational week was recoded into three levels (1) < 25 weeks, (2) 25–36 weeks, and (3) > 36 weeks.
Data analysis was performed in IBM SPSS Statistics for Windows 28.0 (IBM Corporation). Descriptive statistics were used to compute frequencies, percentages, mean, and Standard Deviation [SD]. Chi-square test and Fisher´s Exact Test were used to assess differences in demographics and other covariates based on participants with severe fear of childbirth. We then compared differences between nulliparous and parous pregnant women. Thresholds for significance were set at p < .05.
Qualitative data
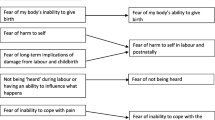
A manifest content analysis approach [45] was adopted to analyse responses to open survey questions informed by other mixed methods surveys [46]. Data analysis was managed using Word. Data about experiences of and preferences for support, barriers and facilitators to help-seeking were analysed separately. Three steps were followed to analyse the text (1) preparation, (2) organizing and (3) reporting. Two authors (CNR and MJ) read the free-text responses to gain an overall understanding of the free-text responses. Next, CNR and MJ identified condensed meaning units (e.g., text sharing a common meaning) and performed line-by-line coding separately. CNR reviewed initial meaning units and coding, with variations discussed by CNR and MJ. Subsequently, CNR and MJ sorted codes into three generic categories, including eight sub-categories that described the main category (Fig. 1). Identified categories were discussed by CNR and MJ to ensure mutual exclusivity and a credible foundation in data. Descriptions of main category, generic categories and sub-categories were prepared by CNR and MJ, with other co-authors performing peer examination of written descriptions. Trustworthiness was also established via independent coding by CNR and MJ and record keeping. To strengthen results, quotations from free text responses are presented, with quotations presented only with the women´s parity and age, to preserve confidentiality.
Data integration
A contiguous approach to data integration was adopted with qualitative and quantitative findings reported separately [47]. First, we analysed the quantitative data to describe the sample and examine experiences of and preferences for as well as barriers and facilitators to help-seeking. Second, we analysed the free-text responses to develop a deeper and more nuanced understanding of preferences for and experiences of support and barriers and facilitators to help-seeking.
Results
Participant characteristics
A total of 609 pregnant women were included: 60% (n = 364) were nulliparous and 40% (n = 245) were parous women. Participants had a mean age of 32.7 years (SD 4.305) and were, on average, in pregnancy week 26 (SD 9.734). Most participants were Swedish-born, lived with their partner, and had a university level of education (Table 1). Nulliparous women were more likely to be younger (p < .001), live in a city (p = .020), have experienced previous mental health difficulties (p = .024), and receive partner support (p < .001) compared to parous women. Parous women were more likely to be on parental leave (p = .008), and to have had previous experience of miscarriage (p < .001) compared to nulliparous women (Table 1).
Qualitative findings
Qualitative analysis resulted in the main category “A twisting road to walk towards receiving support for fear of childbirth” described by three generic categories: (1) Longing for support, (2) Struggling to ask for support, and (3) Facilitating aspects of seeking support (Fig. 1).
Experiences of and preferences for support
Quantitative findings
In total, 337 (63%) of pregnant women reported wanting to receive support in relation to fear of childbirth. A little over one-third (219/609, 36%) of pregnant women either planned to receive, currently received, or had completed fear of childbirth treatment. An additional one-third (36%) of pregnant women would like to receive treatment, but had not yet planned or started any treatment options (Table 2). Of those with ongoing or completed treatment, 60% (59/101) regarded the treatment as less helpful or not at all helpful. Treatment offered for fear of childbirth was described as mainly supportive counselling through clinical professionals (Table 2). Parous women were more likely to have had a planned treatment (p = .002), as well as want individual support (p = .019) compared to nulliparous women (Table 2).
Qualitative findings
Sixty-seven women responded to the open question regarding their experiences of support and preferences for support. Analysis resulted in the generic category “Longing for support” and includes the sub-categories: Support in preparing for childbirth, Individual-based help in well-functioning antenatal care, and Guarantees for safety during childbirth (Fig. 1).
Support in preparing for childbirth concerns expressed preferences for receiving support to help prepare for childbirth. Nulliparous and parous women wanted to be informed about pain relief methods, how to reduce risk of infections in the uterus, and criteria for early hospital discharge after birth. Women expressed receiving information about the antenatal care organization and their routines could facilitate feelings of safety and instill a sense of security. To better prepare for childbirth, women wanted help to design a written birth plan in early pregnancy including wishes concerning mode of birth, length of hospital stay after the birth, and that the plan is respected, rather than questioned and negotiated by professionals. A parous woman aged 34 expressed her need for support:
I would like to have a plan for how my birth will go and that the plan is also carried out to 100% to make me safer and reduce my fear of childbirth.
Women wanted support from labour ward professionals and a doula, and to learn how to cope with their fears, seeing it as their right to seek and receive support.
Women perceived psychological support as something that could help them feel safer, reduce their fear of childbirth, and help to deal with anxiety experienced. A nulliparous woman aged 32 expressed a preference to “Talk about it [the birth] with someone who takes me seriously. Probably need to process the last birth as well.”
However, not all women who had received psychological treatment for fear of childbirth found the treatment helpful, with one parous woman, aged 30, describing her treatment experience as:
Exposing me, bringing up my wounds, standing there alone with no support … a very naked vulnerable feeling. That the support [offered] is too insignificant in comparison to my own fear.
Individual-based help in well-functioning antenatal care concerns women asking for well-organised antenatal care with adequate resources to allow pregnant women to attend a labour ward of their choosing, to process previous negative birth experiences, to receive continuous antenatal care during childbirth, and sufficient midwifery support during active labour. As one parous woman, aged 31, explained:
I would like to talk about my previous birth, why it turned out the way it did, and talk through how the next birth can be different and what options I have and how I can prepare differently.
Women expressed alternative antenatal care models, with being able to choose between several different types of care, to have a paid home birth with a midwife, and continuity of care, expressed as ways to feel supported. Receiving continuous support by a known midwife throughout antenatal, intrapartum, and postnatal care, and being assigned one specific midwife and physician during a hospital birth were also suggested.
Guarantees for safety during childbirth concerns women wanting to receive improved guarantees of safety and health and well-being of themselves and their baby during childbirth via increased ultrasound checks, receiving appropriate care, and that sufficient resources are available during childbirth. One parous woman, aged 39, expressed wanting to:
Get guarantees that I will receive support and pain relief during labor and that the staff will minimize the risks for me, but above all, my baby, during labor.
The receipt of pain relief during childbirth according to preference was also expressed as important, as were professionals working to minimize health risks for the woman and the baby as well as offering postnatal care follow-ups, especially after vaginal tears and caesarean section.
Barriers to help seeking for childbirth fear
Quantitative findings
The most prevalent barriers for help-seeking were: fear of not being listened to by others, fear of not being believed by others, previous negative experience of health care contacts, and discomfort of having to face my own fears. Stigma surrounding fear of childbirth was a barrier for 14% of all pregnant women but higher for nulliparous women (p = .105). Parous women were more likely to regard previous negative experience of healthcare contacts as a barrier, compared to nulliparous women (p = .012) (Table 3).
Qualitative findings
Ninety-two women responded to the open question regarding barriers to help-seeking.
Analysis resulted in the generic category “Struggling to ask for support” and includes the sub-categories: Keeping the fear inside oneself, Not being offered support for fear of childbirth and Unprofessional care that does not help (Fig. 1).
Keeping the fear inside oneself concerns women expressing feeling troublesome and awkward about their encounters with antenatal care, experiencing difficulties explaining their fears to others and admitting their fear to themselves. Women struggled to explain what they were afraid of, leading to concerns that professionals would not believe them. Some women did not take their own fear seriously, believing others to have more to be afraid of to be in more need of more help. These women expressed not wanting to bother and burden professionals and hoped the fear would disappear by itself. Some women found it difficult to understand whether the fear was “normal” or whether they needed professional help. Women expressed feeling “ridiculous”, “dumb”, “silly”, and “shameful” and regarded their fear as just “stupid thoughts” and therefore there was no need to seek support. Women felt too tired, lacked energy, or were unmotivated to start dealing with their fear. A nulliparous woman, aged 35, explained:
I don’t want more meetings as I don’t think there is much that can help, and I get so tired and exhausted from crying.
Women also expressed keeping the fear inside oneself due to more practical concerns, for example, everyday life being time-consuming and needing to travel long distances to access help.
Not being offered support for fear of childbirth concerned women reporting not receiving support for their fear due to challenges contacting healthcare, difficulties understanding what support was available, and not knowing where to access help. Women described either no support being available or lack of availability of their preferred intervention. Women also expressed not being believed or taken seriously by professionals or their fear being dismissed as “normal” anxiety. One nulliparous aged 32 woman noted:
The midwife at the antenatal clinic had instructions that you had to have a strong enough fear of childbirth to be referred to the Aurora clinic, I had to nag repeatedly which felt really hard”.
Not receiving early support in pregnancy was experienced as particularly painful, and had a negative impact on mental health. One nulliparous aged 28 woman stated:
I’m considering terminating the pregnancy because I don’t want to go through labour and my midwife said treatment for the fear only starts after the routine ultrasound.
Unprofessional care that does not help concerns women not being offered professional or helpful care. Women expressed barriers such as lack of healthcare resources, limited appointments, long waiting times, and tired, stressed, irritated, and understaffed professionals. This led to women feeling not listened to and considering it pointless to continue to seek help. Some women considered antenatal care to be poorly organized, resulting in unhelpful care that was not worth seeking. For some women receiving support for their fear, support was perceived as unprofessional with professionals described as being “uncomfortable” in counselling support, “ignorant”, “incompetent”, “sluggish”, and “unmotivated” with a lack of understanding of their problems. One parous woman aged 33 stated:
A midwife at the antenatal clinic who asked a ‘routine question’ about childbirth fear was surprised by the answer and my reaction. I felt like I needed to handle that [the fear] myself”.
Some women perceived that the support offered would make no difference to either the women’s emotions of “panic” and “loss of control” or a negative birth outcome, with the fear considered hard to overcome. One nulliparous woman, aged 27, described it as: “I couldn’t work the rest of the day after the counselling support and got a disturbed night’s sleep … the whole thing got even more traumatic”. Another nulliparous woman, aged 33, said: “I felt resignation when I received the support offered, I got the notion that there is nothing they can help me with”.
Some women felt stigmatised by professionals, and perceived their fear to have been turned into a clinical diagnosis, creating a disadvantage in “power”, alongside misconceptions and preconceived notions on perinatal mental health and previous mental illness before childbirth. One nulliparous woman, aged 31, reported:
My history with anorexia and anxiety often comes into focus. [I have this] feeling that everything comes down to making a diagnosis and it scares me. There have been errors in communication with the psychologist and I have received a diagnosis I do not feel comfortable with.
Facilitators to help-seeking for childbirth fear
Quantitative findings
Facilitators to help-seeking were receiving easily available help, professional support close to home, and being able to choose between different appointment times. There were no significant differences between nulliparous and parous women. It was regarded as important by women to have the opportunity to influence the care they received. For example, being able to choose between digitally-based meetings with lectures, and webinars was regarded as important. Digital solutions were considered to make it easier to seek help due to saving time on transportation and facilitating anonymity. Some women preferred to be offered physical meetings and to be allowed to visit the labour ward during pregnancy. Nulliparous women were more likely to prefer support by internet links (p = .007) and mobile applications (p = .009) compared to parous women (Table 4).
Qualitative findings
Ninety-four women responded to the open question regarding facilitators to seeking support. Analysis of responses resulted in the generic category “Facilitating aspects of seeking support” and includes the sub-categories: Being actively offered easily accessible support in early pregnancy, and Respectful evidence-based support (Fig. 1).
Being actively offered easily accessible support in early pregnancy concerns women describing being asked actively and directly by the midwife several times during pregnancy as a way of facilitating help-seeking. One nulliparous woman aged 34 wrote:
The fact that the midwife asks about support for fear of childbirth is something I’m interested in. I’m afraid of feeling or appearing silly, immature and not ready to be a parent if I express fear of childbirth.
Women considered being offered and encouraged to receive support before (e.g., for women with a previous traumatic birth experience) or in early pregnancy as ways to facilitate help-seeking. Women also wanted to be able to receive support for fear of childbirth without having to be referred for consultation. One parous woman aged 34 noted:
If I had received the slightest help before I got pregnant, it would have felt easier to receive help during the pregnancy. I would have also had greater confidence that the maternity care genuinely wanted to help me based on my circumstances.
Respectful evidence-based support concerns women expressing being offered respectful evidence-based support as a way to facilitate seeking help for their fear. Women wanted competent antenatal care professionals with knowledge and training in mental health, childbirth complications, and available support and treatment options. One nulliparous woman aged 30 described:
Finally, I spoke to a psychologist who was also trained and had worked as a midwife for many years. I felt that she could guide me and to deal with my feelings. The support meant a lot to me and it gave me security.
Women also expressed respectful care, for example, empathy, warmth, and understanding for women who are not within the “norm” as facilitating accessing support. Women wanted to be listened to, taken seriously, and not rejected, belittled, put down, ignored, trivialized, or questioned by professionals. One parous woman, aged 36, asked for: “Professionals that have enough time to provide support, and offer suitable therapists who instill confidence”.
It was expressed by women that having the right to decide over one’s own body and to choose the mode of birth was important also. Women did not want to receive coercive treatment and motivational talks for their fear with the aim of forcing women to give birth vaginally. One nulliparous woman aged 31 wrote: “[It] must be easier to get a caesarian section in case of severe fear of childbirth. [It is] unreasonable to put patients through months of extreme anxiety”.
Discussion
Around two-thirds (63%) of women with fear of childbirth had not planned nor had received any supportive psychological treatment for fear of childbirth. Of those who had received support, 60% reported that the support received was less helpful or not helpful at all. Pregnant women preferred to receive individual-based support provided by antenatal healthcare professionals with sufficient mental health knowledge. Barriers to seeking support included a fear of not being listened to, or believed in by others, the discomfort of having to face their own fears, previous negative healthcare contacts, and the general stigma surrounding fear of childbirth. Facilitators to seeking support included respectful evidence-based support that was easily available, flexible, and close to home.
Support for fear of childbirth
Swedish standard antenatal care states that women with fear of childbirth should be offered support via counselling with a midwife [21]. Our findings suggest not all pregnant women with severe fear of childbirth who had wanted psychological treatment actually received it. Some antenatal clinics may not support all pregnant women with a severe fear of childbirth, given the quality of clinical care and resources differs throughout Sweden [21].
Our findings indicate that parous women were more likely to receive a planned treatment for fear of childbirth than nulliparous women. This difference may partly be because parous women, especially those who had a complicated birth or negative birth experience, such as a caesarean section [48], are routinely invited to review their records with a physician or a midwife and offered a plan of care for the next birth [3]. A recent meta-analysis suggests nulliparous and parous women have similar levels of fear, but have fear for different reasons [12]; therefore, they may have different support needs. Qualitative findings suggested nulliparous women wanted support to prepare for childbirth via information and counselling with an individual birthing plan to help make them feel safe. This finding is in line with other research with nulliparous women, suggesting support may need to focus on handling the unknown and upcoming birth, receiving information on different childbirth scenarios, and injury prevention [12].
Importantly, 60% of the women who received support for fear of childbirth considered it less helpful or not helpful at all. Whilst Swedish research suggested women were satisfied with counselling, effects on fear, anxiety, and requests for a caesarean section have not been shown to differ from those not receiving supportive counselling [36]. Non-pharmacological interventions have been found to reduce fear of childbirth; however, effects were not clinically meaningful [18].
Importantly, 45% of pregnant women with severe fear of childbirth in the present study did not know if they wanted to receive psychological treatment. Previous research suggests pregnant women may believe they can manage their fear by not talking to others about it [18, 42, 49], and subsequently, refrain from participating in antenatal parental classes [49]. Parous women may adopt additional avoidant coping strategies such as blocking memories of previous traumatic childbirth experiences [49], and avoid discussing their upcoming birth with healthcare professionals [18].
Barriers to help-seeking for childbirth fear
Barriers to help-seeking included fear of not being listened to, or believed in by others. Other research suggests women with fear of childbirth experience a lack of understanding from healthcare professionals [49], with their birthing wishes disregarded in favour for standardised procedures [50]. Pregnant women with fear of childbirth have described the importance of being treated by a competent midwife during counselling e.g., who is calm, skilled, whom acknowledges and listens to the women´s thoughts and feelings, thus enhancing a sense of trust and security [36]. However, our findings suggest previous negative healthcare contacts were a barrier to help-seeking. During pregnancy, women in Sweden have regular contact with an antenatal care midwife providing opportunities for the woman-midwife team to work with any previous negative healthcare experiences, and create new positive experiences [3]. Research has found parous women to be more likely to regard previous negative healthcare experiences as a barrier in seeking help for fear of childbirth, compared to nulliparous women [50].
Another barrier identified was stigma. Stigma has been found to be a barrier to the implementation of perinatal mental health policy and practice [24]. Feelings of isolation, guilt, and shame, due to perceived stigma have been reported by women with fear of childbirth in other research, with women feeling unable to talk about their fears with their partners or midwives since pregnancy is generally seen as a time of happiness [51]. Gendered norms and ideals about how a pregnant woman, or a woman in labour, should feel, think, and act, impact both the way healthcare professionals treat women and the way women express and behave themselves [52] and act as barriers to help-seeking.
Facilitators in help-seeking for childbirth fear
Facilitators to help-seeking include the provision respectful evidence-based support that is easily available, flexible, and close to home. Examples of flexible solutions include digital self-help interventions [28, 53, 54] and healthcare professionals being able to provide support via telephone or video conversations, allowing care at a distance and facilitating access for women who have little time for physical visits e.g., full-time jobs and childcare responsibilities [28]. Interventions to overcome stigma for women with fear of childbirth may be important to develop, with such interventions found to be effective for reducing stigma in relation to perinatal depression [55] and may be helpful to enhance help-seeking in the population.
Results also suggest a need for midwives to be knowledgeable in psychological treatment for fear of childbirth, with women needing compassionate, respectful, and supportive care by healthcare professionals, regardless of fear and birthing preferences [49]. Facilitators to the effective implementation of perinatal mental health policy and practice include the provision of flexible women-centered services, delivered by knowledgeable healthcare professionals working for continuity of care [24]. The quality of the healthcare-provider relationship, healthcare professionals normalising perinatal mental health problems, knowing that help is available, and understanding different treatment options have been found to be facilitators to mental health screening among pregnant women [40].
Overall, results suggest a need for more research to develop and evaluate evidence-based psychological interventions for women with severe fear of childbirth that are tailored to women´s needs and preferences. Evidence suggests midwife-led continuity of care models with women supported throughout the childbirth period are beneficial for women with fear of childbirth [56, 57]. Policy makers need to consider Swedish systems of care and allow evidence-based care that optimises a woman´s chance of forming a trusting relationship with healthcare providers. However, the implementation of perinatal mental health policy and practice is complex and varied [24] and lack of training and knowledge of healthcare professionals, complex referral pathways, and lack of trusting relationships between the woman and healthcare providers have been found to be barriers to effective implementation [24].
Strengths and the limitations
This study provides a comprehensive overview of the experiences of and preferences for support, barriers and facilitators to help-seeking, and it also examines differences based on pregnant women’s parity. Another strength is the relatively large sample size and that all counties in Sweden are represented. Despite these strengths, the study has several limitations. Recruitment relied on convenience sampling, and based on sample characteristics, our sample only represents Swedish-speaking women. Thus, findings may not be generalizable to non-Swedish-speaking women in Sweden. Due to the online survey format women needed to have some level of digital literacy to complete the survey which may have impacted the transferability of findings. Qualitative data consisted of free-text responses that varied in length and depth. However, the data still provided important insights into the experiences of women with severe fear of childbirth, their needs, and perceived barriers and facilitators to help-seeking.
Conclusions
This is among the first studies in Sweden to provide a comprehensive overview of the experiences of and preferences for support of pregnant women with severe fear of childbirth and barriers and facilitators to help-seeking, and to examine differences based on pregnant women’s parity. Results indicate not all women with severe fear of childbirth receive support, and many who do receive support regard it as unhelpful. Developing a more comprehensive understanding of experiences and preferences for support, alongside barriers and facilitating for help-seeking, including taking into consideration differences based on women´s parity, are important first steps to inform the development of more acceptable,, relevant, and effective support for women with severe fear of childbirth. Findings highlight the importance of developing accessible, flexible, and individualised support, delivered by trained professionals with an empathetic and respectful attitude, enabling pregnant women to sustain their autonomy during pregnancy and childbirth.
Data availability
The datasets used and/or analysed during the current study are available on request from Carita Nordin-Remberger, Department of Women´s and Children´s Health, Uppsala University. Dag Hammarskjölds väg 20, 752 37 Uppsala, Sweden.
Abbreviations
- CBT:
-
Cognitive behavioural therapy
- CS:
-
Caesarean Section
- EMDR:
-
Eye Movement Desensitization and Reprocessing
- MRC:
-
Medical Research Council
- PE:
-
Psychoeducation
- PDT:
-
Psychodynamic therapy
- PT:
-
Psychotherapy
- SD:
-
Standard Deviation
References
Rondung E, Thomtén J, Sundin Ö. Psychological perspectives on fear of childbirth. J Anxiety Disord. 2016;44:80–91.
Rouhe H, Salmela-Aro K, Gissler M, Halmesmäki E, Saisto T. Mental health problems common in women with fear of childbirth. Br J Obstet Gyneacology. 2011;118:1104–11.
SFOG. Swedish Society of Obstetrics & Gynecology [Svensk förening för Obstetrik och Gynekologi]. Childbirth fear [In Swedish: Förlossningsrädsla]. Report No: 77. Stockholm: 2017.
Erickson NL, Gartstein MA, Dotson JAW. Review of Prenatal Maternal Mental Health and the development of infant temperament. J Obstet Gynecol Neonatal Nurs. 2017 Jul-Aug;46(4):588–600.
Van den Bergh BRH, Mulder EJH, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and the child: links and possible mechanisms. A review. Neurosci Biobehav Rev. 2005;29(2):237–58.
O´ Connell MA, Leahy-Warren P, Khashan AS, Kenny LC, O´Neill SM. Worldwide prevalence of tochophobia in pregnant women: systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2017;96:907–20.
Ternström E, Hildingsson I, Haines H, Rubertsson C. Higher prevalence of childbirth related fear in foreign born pregnant women–findings from a community sample in Sweden. Midwifery. 2015;31(4):445–50.
Saisto T, Salmela-Aro K, Nurmi JE, Halmesmäki E. Psychosocial characteristics of women and their partners fearing vaginal childbirth. Br J Obstet Gynaecol. 2001;108(5):492–8.
Larsson B, Karlström A, Rubertsson C, Ternström E, Ekdahl J, Segebladh B. Hildingsson I. Birth preference in women undergoing treatment for childbirth fear: a randomised controlled trial. Women Birth. 2017;30(6):460–7.
Salomonsson B, Wijma K, Alehagen S. Swedish midwives perceptions of fear of childbirth. Midwifery. 2010;26(3):327–37.
Elvander C, Cnattinggius S, Kjerulff KH. Birth experience in women with low, intermediate or high levels of fear: findings from the first baby study. Birth Berkeley Calif. 2013;40:289–96.
Dencker A, Nilsson C, Begley C, Jangsten E, Mollberg M, Patela H. Causes and outcomes in studies of fear of childbirth: a systematic review. Women Birth. 2019;32(9):99–111.
Henriksen L, Grimsrud E, Schei B, Lukasse M. Factors related to a negative birth experience – A mixed methods study. Midwifery. 2017;51:33–9.
Grundström H, Malmquist A, Ivarsson A, Torbjörnsson E, Walz M, Nieminen K. Fear of childbirth postpartum and its correlation with post-traumatic stress symtoms and quality of life among women with birth complications – a cross sectional study. Arch Women Ment Health. 2022;25(2):485–91.
Haines HM, Pallant JF, Fenwick J, Gamble J, Creedy DK, Toohill J, Hildingsson I. Identifying women who are afraid of giving birth: a comparison of the fear of birth scale with the WDEQ-A in a large Australian cohort. Sex Reproductive Healthc. 2015;6(4):204–10.
Jomeen J. Fathers in the birth room: choice or coercion? Help or hindrance? J Reproductive Infant Psychol. 2017;35(4):321–3.
Bäckström C, Thorstensson S, Mårtensson LB, Grimming R, Nyblin Y, Golsäter M. To be able to support her, I must feel calm and safe’: pregnant women’s partners perceptions of professional support during pregnancy. BMC Pregnancy Childbirth. 2017;17:1–11.
O’Connell MA, Khashan AS, Leahy-Warren P, Stewart F, O’Neill SM. Interventions for fear of childbirth including tocophobia. Cochrane Database of Systematic Reviews. 2021, Issue 7. Art. No.: CD013321. https://doi.org/10.1002/14651858.CD013321.pub2.
Eggermont K, Beeckman D, Van Hecke A, Delbaere I, Verhaeghe S. Needs of fathers during labour and childbirth: a cross-sectional study. Women Birth. 2017;30(4):e188–97. https://doi.org/10.1016/j.wombi.2016.12.001.
Hildingsson I, Johansson M. A cluster analysis of reasons behind fear of birth among women in Sweden. J Psychosom Obstet Gynecol. 2024;45(1):2319291.
Larsson B, Karlström A, Rubertsson C, Hildingsson I. The effects of counselling on fear of childbirth. Acta Obstet Gynecol Scand. 2015;94(6):629–36.
Nieminen K, Malmquist A, Wijma B. Nulliparous pregnant women’s narratives of imminent childbirth before and after internet-based cognitive behavioural therapy for severe fear of childbirth: a qualitative study. BJOG. 2015;122:1259–65.
Striebich S, Mattern E, Ayerle GM. Support for pregnant women identified with fear of childbirth (FOC)/tokophobia – a systematic review of approaches and interventions. Midwifery. 2018;61:97–115.
Webb R, Bond R, Romero-Gonzalez B, Mycroft R, Ayers S. Interventions to treat fear of childbirth in pregnancy: a systematic review and meta-analysis. Psychol Med. 2021;51(12):1964–77.
Moghaddam Hosseini V, Nazarzadeh M, Jahanfar S. Interventions for reducing fear of childbirth: a systematic review and meta-analysis of clinical trials. Women Birth. 2017;31(4):254–62.
Stoll K, Swift EM, Fairbrother N, Nethery E, Janssen P. A systematic review of nonpharmacological prenatal interventions for pregnancy-specific anxiety and fear of childbirth. Birth. 2018;45(1):7–18.
Shefaly S, Downe S, Chua J, Byrne SO, Fobelets M, Lalor JG. Effectiveness of psychological interventions to improve the mental well-being of parents who have experienced traumatic childbirth: a systematic review and meta-analysis. Trauma Violence Abuse. 2023;24(3):1238–53.
Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. 2020;19(3):313–27.
Loughnan SA, Wallace M, Joubert AE, Haskelberg H, Andrews G, Newby JM. A systematic review of psychological treatments for clinical anxiety during the perinatal period. Arch Women Ment Health. 2018;21:481–90.
Fenwick J, Toohill J, Creedy DK, Smith J, Gamble J. Sources, responses and moderators of childbirth fear in Australian women: a qualitative investigation. Midwifery. 2015;31(1):239–46.
Handelzalts JE, Becker G, Ahren M-P, Lurie S, Raz N, Tamir Z, Sadan O. Personality, fear of childbirth and birth outcomes in nulliparous women. Arch Gynecol Obstet. 2015;291(5):1055–62.
Räisänen S, Lehto S, Nielsen H, Gissler M, Kramer M, Heinonen S. Fear of childbirth in nulliparous and multiparous women: a population-based analysis of all singleton births in Finland in 1997–2010. BJOG. 2014;121:965–70.
Stephansson O, Petersson K, Björk C, Conner P, Wikström AK. The Swedish pregnancy Register—for quality of care improvement and research. Acta Obstet Gynecol Scand. 2018;97(4):466–76.
Hildingsson I, Haines H, Karlström A, Nystedt A. Presence and process of fear of birth during pregnancy – findings from a longitudinal cohort study. Women Birth: J Australian Coll Midwives. 2017;30(5):242–7.
Larsson B, Karlström A, Rubertsson C, Hildingsson I. Counseling for childbirth fear- a national survey. Sex Reprod Healthc. 2016;8:82–7.
Larsson B, Hildingsson I, Ternström E, Rubertsson C, Karlström A. Women’s experience of midwife-led counselling and its influence on childbirth fear: a qualitative study. Women Birth. 2019;32(1):88–94.
Creswell John W. Mapping the field of mixed methods research. J Mixed Methods Res. 2009;3(2):95–108.
Maré IA, Kramer B, Hazelhurst S, Nhlapho MD, Zent R, Harris PA, Klipin M. Electronic Data capture System (REDCap) for Health Care Research and Training in a resource constrained Environment: Technology Adoption Case Study. JMIR Med Inf. 2022;10(8):e33402.
Eysenbach G. Improving the quality of web surveys: the Checklist for reporting results of internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34.
Kingston D, Austin MP, Heaman M, McDonald S, Lasiuk G, Sword W, Giallo R, Hegadoren K, Vermeyden L, van Zanten SV, Kingston J, Jarema K, Biringer A. Barriers and facilitators of mental health screening in pregnancy. J Affect Disord. 2015;186:350–7.
Richens Y, Smith DM, Lavender DT. Fear of birth in clinical practice: a structured review of current measurement tools. Sex Reproductive Healthc. 2018;16:98–112.
Rondung E, Ternström E, Hildingsson I, Haines HM, Sundin Ö, Ekdahl J, Rubertsson C. Comparing internet-based cognitive behavioural therapy with standard care for women with fear of birth: Randomized controlled trial. J Med Internet Res. 2018;5(3):10420.
Lean SC, Derricott H, Jones RL, Heazell AEP. Advanced maternal age and adverse pregnancy outcomes: a systematic review and meta-analysis. PLoS ONE. 2017;12(10):0186287.
Sauer MV. Reproduction at an advanced maternal age and maternal health. Fertil Steril. 2015;103(5):1136–43.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15.
Hagström J, Woodford J, von Essen A, Lähteenmäki P, von Essen L. Opt-out rates and reasons for non-participation in a single-arm feasibility trial (ENGAGE) of a guided internet-administered CBT-based intervention for parents of children treated for cancer: a nested cross-sectional survey. BMJ Open. 2022;12(4):e056758.
Fetters, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res. 2013;48(6pt2):2134–56.
Jenabi E, Khazaei S, Bashirian S, Aghababaei S, Matinnia N. Reasons for elective cesarean section on maternal request: a systematic review. J Maternal-Fetal Neonatal Med. 2020;33(22):3867–72.
Wigert H, Nilsson C, Dencker A, Begley C, Jangsten E, Sparud-Lundin C, Mollberg M, Patel H. Women’s experiences of fear of childbirth: a metasynthesis of qualitative studies. Int J Qual Stud Health Well-Being. 2020;15:1704484.
Lukasse M, Schroll AM, Karro H, Schei B, Steingrimsdottir T, Van Parys AS, Ryding EL, Tabor A. Prevalence of experienced abuse in healthcare and associated obsteric characteristics in six European countries. Acta Obstet Gynecol Scand. 2015;94(5):508–17.
Lyberg A, Severinsson E. Fear of childbirth: mothers’ experiences of team-midwifery care – a follow-up study. J Nurs Adm Manag. 2010;18:383–90.
Westergren A. Deficient bodies and divine interventions. Women, midwives, and the medicalisation of childbirth – A gender perspective. 2021.
Fritzson Nordin A, Børøsund E, Johansson M, Varsi C, Ängeby K. A mobile application for early labour support -feasibility pilot study. Women Birth: J Australian Coll Midwives. 2023. https://doi.org/10.1016/j.wombi.2023.03.008.
Iwaya NA, Fritsch L, Børøsund E, Johansson M, Varsi C, Ängeby K. Early Labour App: developing a practice-based mobile health application for digital early labour support. Int J Med Inf (Shannon Ireland). 2023;177:105139–105139. https://doi.org/10.1016/j.ijmedinf.2023.105139.
Ford E, Roomi H, Hugh H, Van Marwijk H. Understanding barriers to women seeking and receiving help for perinatal mental health problems in UK general practice: development of a questionnaire. Prim Health Care Res Dev. 2019;20:1–8.
Hildingsson I, Karlström A, Haines H, Johansson M. Swedish women’s interest in models of midwifery care–time to consider the system? A prospective longitudinal survey. Sex Reproductive Healthc. 2016;7:27–32.
Hodnett ED, Gates S, Hofmeyr GJ, Sakala C. (2013). Continuous support for women during childbirth. Cochrane database of systematic reviews, (7).
Acknowledgements
We would like to thank the midwives at the clinics involved and organisations and individuals who helped us to promote the survey advertisements, and the women who invested their time in completing the survey.
Funding
Open access funding provided by Uppsala University. This study was carried out as part of doctoral studies at the Uppsala University, which is supported by WOMHER research school.
Open access funding provided by Uppsala University.
Author information
Authors and Affiliations
Contributions
CNR was responsible for conceptualization, methodology, formal analysis, investigation, data curation, writing - original draft, and visualization. MBW was responsible for conceptualization, methodology, data curation, writing - review and editing. JW was responsible for conceptualization, methodology, writing - review and editing. KSL was responsible for methodology, writing - review and editing. MJ was responsible for conceptualization, methodology, formal analysis, investigation, data curation, writing - original draft, review and editing, visualization, supervision and project administration. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Swedish National Ethical Review Authority board approved the research procedures and questionnaire for the Medical Research Ethics Committee in Lund, on September 6th, 2021 [Approval number: 2021–03759]. In addition, informed consent for participants 18 years of age or older, self-identified as a pregnant woman, living in Sweden, and able to read and understand Swedish was obtained prior to the data collection. All methods were carried out in accordance with applicable guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nordin-Remberger, C., Wells, M.B., Woodford, J. et al. Preferences of support and barriers and facilitators to help-seeking in pregnant women with severe fear of childbirth in Sweden: a mixed-method study. BMC Pregnancy Childbirth 24, 388 (2024). https://doi.org/10.1186/s12884-024-06580-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06580-2