Abstract
Objective
We sought to investigate the impact of individualized exercise guidance during pregnancy on the incidence of macrosomia and the mediating effect of gestational weight gain (GWG).
Design
A prospective randomized clinical trial.
Setting
A Hospital in Xingtai District, Hebei Province.
Population
Older than 20 years of age, mid-pregnancy, and singleton pregnant women without contraindications to exercise during pregnancy.
Methods
A randomized clinical trial was conducted from December 2021 to September 2022 to compare the effects of standard prenatal care with individualized exercise guidance on the incidence of macrosomia.
Main outcome measure
Incidence of macrosomia.
Results
In all, 312 singleton women were randomized into an intervention group (N = 162) or a control group (N = 150). Participants who received individualized exercise guidance had a significantly lower incidence of macrosomia (3.73% vs. 13.61%, P = 0.002) and infants large for gestational age (9.94% vs. 19.73%, P = 0.015). However, no differences were observed in the rate of preterm birth (1.86% vs. 3.40%, P = 0.397) or the average gestational age at birth (39.14 ± 1.51 vs. 38.69 ± 1.85, P = 0.258). Mediation analysis revealed that GWG mediated the effect of exercise on reducing the incidence of macrosomia.
Conclusion
Individualized exercise guidance may be a preventive tool for macrosomia, and GWG mediates the effect of exercise on reducing the incidence of macrosomia. However, evidence does not show that exercise increases the rate of preterm birth or affects the average gestational age at birth.
Trial registration
The trial is registered at www.clinicaltrails.gov [registration number: NCT05760768; registration date: 08/03/2023 (retrospectively registered)].
Similar content being viewed by others
Recommendations
-
1. Pregnant women without contraindications should exercise according to their own conditions with management and supervision aided by information technology devices.
-
2. We should pay greater attention to the management of controllable and preventable factors, such as gestational weight gain, in patients under prenatal care.
Introduction
Macrosomia refers to a neonatal birth weight greater than 4000 g [1]. The prevalence of macrosomia varies among different countries and regions, as developed countries have a prevalence rate of approximately 5% ~ 20%, while developing countries have a prevalence rate of approximately 0.5% ~ 14.9% [2]. In China, various studies have reported different rates of macrosomia, and a cross-sectional study including 14 provinces in China reported a rate of 7.83% in 2005 [3], while a multicentre study reported a rate of 7.3% in 2011 [4]. A nationally representative cross-sectional survey in mainland China illustrated that the overall prevalence of macrosomia in Chinese children younger than 6 years in 2013 was 7.35% [5]. The rate of macrosomia is consistently high and is associated with several maternal complications, such as caesarean delivery, postpartum haemorrhage, chorioamnionitis, soft birth canal laceration and even uterine and bladder rupture [6, 7]. In neonates, macrosomia increases the risk of shoulder dystocia, clavicle fractures, brachial plexus injury, respiratory distress, meconium aspiration syndrome, hypoglycaemia, polycythaemia and even mortality [1, 6,7,8]. In addition, macrosomia also affects the long-term health of offspring, as it increases the risk of overweight or obesity, hypertension, diabetes and cardiovascular disease [9]. Consequently, reducing the incidence of macrosomia is a public health issue that should be addressed.
Gestational weight gain (GWG) has been shown to be associated with macrosomia and large for gestational age (LGA) infants [10, 11]. Individual participant data from a meta-analysis revealed that excessive gestational weight gain (EGWG) was related to a greater risk of macrosomia (RR = 1.52, 95% CI: 1.33 ~ 1.73) than adequate GWG [12]. Furthermore, EGWG is regarded as an independent risk factor for macrosomia. An observational study revealed that for pregnant women with gestational diabetes mellitus (GDM), restriction of continued EGWG after commencing GDM management could reduce the risk of LGA infants [13]. Therefore, it is essential to control weight gain during pregnancy.
Exercise may be a useful method to control weight gain during pregnancy. A randomized controlled study revealed that pregnant women who did not exercise were 2.5 times more likely to give birth to newborns with macrosomia [14]. A systematic review and meta-analysis showed that exercise during pregnancy could decrease the incidence of macrosomia without affecting the likelihood of having an infant with preterm birth or low birth weight [15]. Additionally, exercise during pregnancy also plays an essential role in preventing other adverse pregnancy outcomes. Several systematic reviews and meta-analyses have shown that exercise during pregnancy can reduce the risk of EGWG, GDM, and hypertensive disorders, among others, during pregnancy [16, 17].
However, the mechanisms that underlie the effects of exercise on macrosomia are not fully understood. Therefore, we hypothesize that exercise during pregnancy reduces the incidence of macrosomia by decreasing GWG. In our study, we established an individualized exercise guidance programme for pregnant women and combined online and offline channels for monitoring. We aimed to explore the preventive effect of exercise on macrosomia and whether GWG has a mediating effect.
Materials and methods
The RCT (NCT05760768) was a single-centre and parallel-group study conducted from December 2021 through September 2022 in Xingtai, Hebei Province. The research protocol was reviewed and approved by the Medical Ethics Committee of Xindu District Central Hospital in Xingtai City (reference number: 18). All participants provided written informed consent, and the ethics committee approved the consent procedure.
Participants and randomization
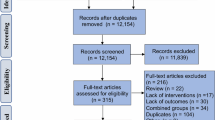
Overall, 326 pregnant women who visited Xingtai Xindu District Central Hospital for the first time between December 2021 and January 2022 were assessed for eligibility (Fig. 1). Singleton women aged older than 20 years who were in mid-pregnancy, who planned to undergo regular prenatal follow-ups and who gave birth at Xingtai Xindu District Central Hospital were included in this study. Pregnant women with contraindications to exercise during pregnancy, such as persistent vaginal bleeding or abdominal pain, cervical insufficiency, placenta previa, and severe heart failure, were excluded. Those who were unwilling to provide informed consent were also excluded.
In all, 312 pregnant women were randomly allocated to either an individualized exercise guidance (intervention) group or a standard prenatal care (control) group. The randomized participant assignment to the two groups alternatively followed the time of recruitment. The two researchers enrolled participants, generated the allocation sequence and assigned participants to interventions. Due to the nature of the intervention, all participants and research staff were aware of the allocations. The entire study was facilitated by obstetric specialists and qualified teachers who provided individualized exercise guidance. These teachers had received professional training in prenatal and postnatal exercise guidance.
Participant demographics
Demographic and other information (pregravid weight and height), parity, medical and family history, and current pregnancy information were obtained at the time of enrolment. Information on prepregnancy exercise of the participants was collected through questionnaires. The ratio of weight to height squared was calculated to obtain the prepregnancy body mass index (BMI). According to weight monitoring and evaluation of pregnant Chinese women [18], prepregnancy BMI was classified into four categories: underweight (BMI < 18.5 kg/m2), normal weight (18.5 kg/m2 ≤ BMI < 24.0 kg/m2), overweight (24.0 kg/m2 ≤ BMI < 28.0 kg/m2) and obese (BMI ≥ 28.0 kg/m2).
Standard prenatal care (control) group
Pregnant women randomly allocated to the control group received standard prenatal care, which was consistent with that of the intervention group. Participants in the control group also received general advice about the effects of physical activity and were not restricted from exercising on their own during pregnancy. No special dietary recommendations were given. A self-designed questionnaire was used to collect information on the exercise habits of the two groups, including exercise type, duration and frequency.
Individualized exercise guidance (intervention) group
Based on standard prenatal care, pregnant women randomly assigned to the intervention group received individualized exercise guidance immediately after randomization. The researchers informed the participants in the intervention group in detail about their contraindications to exercise and the timing of termination of exercise, which ensured patient safety during the intervention. According to age, prepregnancy BMI, previous physical activity habits, physical conditions and personal preferences, the researchers issued individualized exercise guidance, which was based on the American College of Obstetricians and Gynecologists (ACGO) committee recommendation [19] (Fig. 2). One of the exercise types was aerobic exercise, which includes jogging, fertility dance, swimming and yoga. The other was strength training, which was supplemented by tools such as elastic bands and dumbbells. The duration of exercise gradually increased from at least 15 min per session to at least 30 min per session. The exercise intensity was predominantly moderate. If a participant did not have a history of regular exercise before pregnancy, then a low-intensity exercise program that gradually increased to a moderate-intensity exercise program was recommended. The Borg Rating of Perceived Exertion (RPE) and the "talk test" were jointly used as indicators of exercise intensity. The Borg scale is the most commonly used method for assessing personal RPE and ranges from 6 to 20, representing exercise, which is considered “very, very light” to “very, very hard” [20]. For pregnant women, exercise intensity is generally controlled between Borg 13 and 14 [19, 21]. The "talk test" is another method: as long as a woman can have a conservation while exercising, she is likely not overexerting herself [22]. The frequency of exercise gradually increased from 3 times per week to 5 times per week. Each exercise included a warm-up session at the beginning and a stretching and relaxation session at the end. During the study, individualized exercise guidance was continuously adjusted by the researchers according to the participants’ tolerance and discomfort.
To guarantee quality, the researchers monitored and managed participants through both online and offline channels. Pregnant women in the intervention group had to ensure that they received individualized exercise guidance in a group setting as part of pregnancy education at the hospital at least three times per week and could exercise on their own at home for the remaining time. The researchers established a WeChat group to regularly send video, audio and text content to the participants in the intervention group and to collect information about the duration and type of exercise as well as discomfort felt during exercise through an electronic questionnaire. A personal data file was created for each participant and included information on exercise status and physical condition during pregnancy. The researchers summarized and provided feedback to all participants each week. Questions about pregnancy were collected once a week and were answered at the end of the week. Participants were encouraged to share their exercise or pregnancy experience and feelings in the WeChat group, which aimed to enhance peer support and peer education.
Outcomes
Primary outcome
Macrosomia refers to neonatal weight greater than 4000 g [1]. The primary outcome was the number of macrosomia cases (percentage/incidence).
Secondary outcomes
The secondary outcomes included the rates of low birth weight (LBW) (birth weight < 2500 g), large for gestational age (LGA) (birth weight > 90th percentile for gestational age) and small for gestational age (SGA) (birth weight < 10th percentile for gestational age).
Gestational weight gain (GWG) was calculated according to the weight before delivery minus the pregravid weight and was stratified by prepregnancy BMI categories based on weight monitoring and evaluation of pregnant Chinese women [18]. Adequate gestational weight gain was as follows: 11 ~ 16 kg for underweight, 8 ~ 14 kg for normal weight, 7 ~ 11 kg for overweight, and 5 ~ 9 kg for obese. Lower weights than the above criteria are considered inadequate gestational weight gain, while higher weights are considered excessive gestational weight gain. The diagnoses of GDM, gestational hypertension and preterm birth obtained from the medical records were also included.
Postpartum weight retention (PPWR) was measured as the weight at 42 days after delivery minus pregravid weight. PPWR ≥ 5 kg was considered substantial and < 5 kg was considered insubstantial [23]. Diastasis recti abdominis (DRA) is defined as a palpated separation of ≥ 2 fingerbreadths either 4.5 cm above or 4.5 cm below the umbilicus. DRA was also measured at 42 days after delivery and was classified into three categories depending on the largest measured inter-rectus distance among the three locations [24]: 1) mild: 2–3 fingerbreadths; 2) moderate: 3–4 fingerbreadths; and 3) severe: 4 or more fingerbreadths.
Statistical analysis
Power calculations for the primary outcome (the incidence of macrosomia) revealed a prevalence of 0.95% in the exercise group and 6.88% in the standard of care group according to a previous study [25]. Under these assumptions with a 2-sample comparison, a 10% level of significance and a power of 0.80, assuming a maximum loss to follow-up of 10%, approximately 150 pregnant women were needed for each group at baseline.
Continuous variables are presented as the means ± SDs, and categorical variables are presented as numbers and percentages. Differences in the means between two groups were evaluated using independent sample t tests and analysis of variance. Pearson’s X2 test was used for categorical variables. Missing data have been deleted. The mediation effect analysis was based on the following strategy proposed by Baron [26]: 1) the independent variable (IV) significantly affects the mediation factor; 2) in the absence of the mediation factor, the IV significantly affects the dependent variable (DV); 3) the mediation factor has a significant effect on the DV; and 4) the effect of the IV on the DV weakens upon the addition of a mediation factor in the model. A mediation model suitable for combining categorical and continuous variables was developed by Iacobucci [27]. The formulas are as follows:
If the mediation factor and dependent variable are continuous variables, the original formula of the Sobel test is applicable:
If the mediation factor or dependent variables are categorical variables, then the original formula of the Sobel test is rederived into a new formula:
Here, a is the simple linear or logistic regression coefficient for the IV against the mediation factor, while b is the regression coefficient for the mediation factor against the DV in the binary linear or regression model. Additionally, Sa and Sb represent the standard deviations of a and b, respectively. Zm values exceeding |1.96|,|2.57|, and|3.90| (for the two-tailed test) are significant at a = 0.05, 0.01 and 0.001, respectively [28]. We conducted the statistical analyses using SPSS software (version 24.0; IBM Crop, Armonk, NY). The level of significance was set to < 0.05.
Results
We concluded the study in September 2022 after all participants completed the follow-up. A total of 312 pregnant women met the inclusion criteria. After randomization, 1 pregnant woman in the intervention group was lost to follow-up because of newly developed contraindications, while 3 pregnant women in the control group were lost to follow-up because of newly developed contraindications (n = 1) and personal reasons (n = 2). In all, 308 pregnant women were analysed: 161 in the intervention group and 147 in the control group. Among them, data on PPWR and DRA were missing for 49 pregnant women. Pregnant women in the intervention group received regular individualized exercise guidance from enrolment until delivery.
Maternal characteristics
Personal data, as shown in Table 1, were collected from all participants at the beginning of the study. The two groups were well matched at baseline, with no significant differences between them. After the study, significant differences were observed in the type, duration and frequency of exercise between the two groups (Supplementary Table 1). Only 42.86% (63/147) of the pregnant women in the control group engaged in exercise, which was predominantly walking, during pregnancy (Supplementary Fig. 1).
Macrosomia and other pregnancy outcomes
In the individualized exercise guidance group vs. the standard prenatal care group (Table 2), exercise significantly reduced the incidence of macrosomia (P = 0.002) and LGA (P = 0.015). No significant differences were found between the two groups in LBW or SGA, and no change was observed in gestational age at birth. Exercise reduced GWG (P < 0.001) and promoted adequate gestational weight gain (P < 0.001) in mothers in the intervention group compared with those in the control group. However, the two groups exhibited no significant differences in the incidences of GDM, gestational hypertension or preterm birth. Pregnant women randomized to the intervention group had a significantly lower PPWR (p < 0.001) than those in the control group. In addition, moderate and severe DRA were significantly less common in the intervention group than in the control group (p = 0.037).
Outcomes based on different prepregnancy BMIs
To investigate whether the effect of exercise on macrosomia was independent of prepregnancy BMI, we analysed the data by dividing the participants into two groups based on prepregnancy BMI (Table 3). A statistically significant difference was observed in the incidence of macrosomia between the intervention group and the control group in the underweight and normal weight pregnant women but not in the overweight and obese pregnant women. For mothers, exercise was effective in reducing GWG and PPWR and preventing substantial PPWR, irrespective of prepregnancy BMI.
Mediation analysis
Significant differences were found in GWG between the two groups, and the difference was also significant among the different prepregnancy BMI groups. Hence, we used GWG as a mediating factor to analyse its mediating effect between exercise during pregnancy and other outcomes (Fig. 3). Figure 3 A and B show that GWG mediated the effect of exercise during pregnancy and reduced the incidence of macrosomia (Zm = 2.80, P < 0.01) and LGA (Zm = 2.71, P < 0.01). Figure 3 C shows that GWG mediated the effect of exercise during pregnancy and decreased the PPWR (Zm = 6.36, P < 0.001). Figure 3 D illustrates that GWG did not mediate the effect of exercise during pregnancy on the prevention of moderate or severe DRA (Zm = 1.61, P > 0.05).
Mediating effect of GWG on exercise and A macrosomia, B LGA, C PPWR, and D DRA. c is the simple linear or logistic regression coefficient for the independent variable against the dependent variable in the absence of a mediating factor. c’ is the binary linear or logistic regression coefficient for the independent variable against the dependent variable in the presence of a mediating factor. a Simple linear or logistic regression coefficient for the independent variable against the mediating factor. b is the regression coefficient for the mediation factor against the dependent variable in the binary linear or regression model. Sa and Sb represent the standard deviations of a and b, respectively. Independent variable: exercise; mediation factor: GWG; dependent variables: macrosomia, LGA, PPWR and DRA. P < 0.05, **P < 0.01
Discussion
We conducted a prospective RCT to evaluate the efficacy of individualized exercise guidance for preventing macrosomia. Compared with previous studies, our study combined offline guidance and online remote management to improve the compliance of pregnant women. The main finding of our study was that GWG may play a mediating role in the preventive effect of exercise during pregnancy on macrosomia.
The overall rate of macrosomia in our study was 8.44%, with 13.61% in the standard prenatal care group and 3.73% in the individualized exercise guidance group. Our exercise intervention reduced the incidence of macrosomia, which was consistent with the conclusions of previous studies. A systemic review and meta-analysis also revealed that exercise during pregnancy was a protective factor against macrosomia [15]. Among overweight and obese pregnant women, although the occurrence of macrosomia was lower in the intervention group than in the control group, the difference was not statistically significant, which is consistent with the findings of Chen Wang et al. [29]. In our study, the small number of overweight and obese pregnant women may be the reason that no significant difference was found. However, regardless of the prepregnancy BMI, exercise during pregnancy reduced the incidence of macrosomia by approximately 10%, which agrees with the overall findings. Therefore, regardless of prepregnancy BMI, it is suggested that all pregnant women exercise appropriately during pregnancy according to their own conditions to decrease the occurrence of adverse pregnancy outcomes.
Our study also revealed that individualized exercise guidance could effectively reduce GWG regardless of prepregnancy BMI. A systematic review and meta-analysis revealed that pregnant women who performed physical activity during pregnancy gained 1.04 kg more than those who did not exercise [16], which was also confirmed in our study. In addition, our exercise intervention also prevented EGWG, which is regarded as a risk factor for childhood obesity [30] and adverse pregnancy outcomes, including GDM, hypertensive disorders of pregnancy, preterm birth, and caesarean delivery [31]. The incidence of EGWG in the standard prenatal care group was more than twice as high as that in the individualized exercise guidance group. However, after adjusting for prepregnancy BMI, the above findings did not hold true for overweight or obese pregnant women. Overweight and obesity are considered risk factors for excessive gestational weight gain [32], possibly because the preventive effect of exercise during pregnancy does not offset the harmful effects of overweight and obesity.
More importantly, we found that exercise during pregnancy reduces the occurrence of macrosomia by decreasing GWG; that is, GWG mediates the effect of exercise on macrosomia. Previous studies have predominantly focused on the protective effect of exercise on macrosomia, while our study also investigated the mediating role of GWG in this relationship. This result not only suggests that in prenatal care, attention should be given to the management of controllable and modifiable factors such as GWG to reduce prenatal complications and adverse pregnancy outcomes but also provides further insights into the mechanisms through which exercise influences foetal growth.
A variety of factors, such as genetic background, environmental factors, and maternal health status, predispose a newborn to macrosomia [1, 7, 33]. Multiple studies have confirmed that excessive gestational weight gain is a risk factor for macrosomia, regardless of race, region, and other factors [32, 34,35,36]. A cross-sectional, observational study revealed that even without GDM, the rate of GWG was a potentially modifiable contributor to insufficient β-cell function [37]. Another study revealed that more weight gain than what is recommended during pregnancy is associated with a greater decrease in insulin sensitivity between 15 and 35 weeks of gestation [38], which can lead to maternal and foetal hyperglycaemia. Consequently, the foetal release of insulin, insulin-like growth factors, and growth hormone can also increase, which, in turn, could lead to increased foetal fat deposition and larger foetal size [33].
Our study also revealed that exercise during pregnancy reduced the incidence of LGA infants and that GWG mediated this effect. Similarly, a systematic review and meta-analysis revealed that the likelihood of delivering LGA infants decreased by 17% among normal weight women who exercised during pregnancy [39]. Excessive gestational weight gain was found to be a risk factor for LGA infants, independent of the impact of prepregnancy BMI on LGA [32, 36, 40]. Thus, exercise during pregnancy reduces the occurrence of LGA by reducing GWG.
We also found that exercise during pregnancy may effectively reduce PPWR by decreasing GWG. Substantial postpartum weight retention increases the risk of subsequent hypertension and diabetes, as well as the risk of developing GDM and gestational hypertension in subsequent pregnancies [41]. Excessive gestational weight gain is one of several factors that influences PPWR [17]. However, we did not find that GWG mediated the effect on the prevention of moderate or severe DRA. We speculate that this may be due to exercise strengthening the abdominal wall muscles, thereby reducing the occurrence of moderate or severe DRA.
Furthermore, our study did not find that exercise during pregnancy increased adverse side effects. The preterm birth rate in the standard prenatal care group was 3.40%, while that in the individualized exercise guidance group was lower than that at only 1.86%. No statistically significant differences were observed in mean gestational age at birth between the two groups. A review revealed that exercise did not increase the risk of preterm birth [42]. A systematic review and meta-analysis also suggested that exercise did not affect preterm birth [16].
Our study showed that exercise during pregnancy is a protective factor against macrosomia, large for gestational age infants, and excessive gestational weight gain. Pregnancy is not an exclusion criterion for exercise. The ACOG [19] recommends that pregnant women without contraindications to exercise engage in moderate-intensity exercise for 20–30 min per day or at least 4 times per week. The SOCG and CSEP [43] also recommend that pregnant women without contraindications to exercise accumulate at least 150 min of moderate-intensity physical activity per week, combining aerobic and resistance exercise. However, each pregnant woman has different personal circumstances, and individualized exercise plans that are dynamically adjusted according to her physical changes during pregnancy need to be developed. It is also difficult to implement a pregnancy exercise plan entirely in the hospital. Therefore, it is recommended that all pregnant women without contraindications perform physical activity during pregnancy according to their own conditions with management and supervision aided by information technology devices. We also found that only a few pregnant women in the control group voluntarily exercised during pregnancy, which suggested that we should strengthen the education and management of exercise during pregnancy in perinatal care.
Strengths and weaknesses
First, the major strength of our study is that it was an RCT with high adherence (> 90%) in the two groups, which ensures the reliability and authenticity of the study results. This high adherence may be related to the development of individualized exercise guidance for participants based on their personal situations. Second, our study combined offline exercise guidance and online remote supervision. Pregnant women randomized to the intervention group received individualized exercise guidance at least 3 times per week in the hospital and exercised on their own at home for the remainder of their pregnancy. Moreover, the researchers established a WeChat group to understand the exercise situation of each participant and to strengthen their knowledge, education and peer education. Third, our study not only reaffirmed that exercise during pregnancy reduces the incidence of macrosomia but also revealed that GWG mediates this effect. Our study also highlights that interventions that focus on reducing modifiable risk factors, such as GWG, should be incorporated into prenatal care.
Our study also has some limitations. First, our study did not consider the impact of dietary patterns of energy intake during pregnancy on outcomes. Although both groups received standard prenatal care, including dietary advice during pregnancy, personal compliance may vary. In future research, both exercise and diet together should be considered. Furthermore, our study did not consider the intensity of daily physical activity, such as work and housework.
Further research is needed to investigate whether overall lifestyle interventions during pregnancy, including exercise, diet and other factors, can more effectively improve pregnancy outcomes. At the same time, it is essential to perform follow-up to explore the incidence of overweight/obesity and other cardiovascular diseases in the offspring of pregnant women who exercise during pregnancy.
Availability of data and materials
The data and materials that support the findings of this study are available from the corresponding author upon reasonable request.
References
Macrosomia: ACOG Practice Bulletin, Number 216. Obstet Gynecol. 2020;135(1):e18–35. https://doi.org/10.1097/AOG.0000000000003606.
Koyanagi A, Zhang J, Dagvadorj A, Hirayama F, Shibuya K, Souza JP, Gülmezoglu AM. Macrosomia in 23 developing countries: an analysis of a multicountry, facility-based, cross-sectional survey. Lancet. 2013;381(9865):476–83.
Lu Y, Zhang J, Lu X, Xi W, Li Z. Secular trends of macrosomia in southeast China, 1994–2005. BMC Public Health. 2011;11:818.
Li G, Kong L, Li Z, Zhang L, Fan L, Zou L, Chen Y, Ruan Y, Wang X, Zhang W. Prevalence of macrosomia and its risk factors in china: a multicentre survey based on birth data involving 101,723 singleton term infants. Paediatr Perinat Epidemiol. 2014;28(4):345–50.
Shen L, Wang J, Duan Y, Yang Z. Prevalence of low birth weight and macrosomia estimates based on heaping adjustment method in China. Sci Rep. 2021;11(1):15016.
Beta J, Khan N, Khalil A, Fiolna M, Ramadan G, Akolekar R. Maternal and neonatal complications of fetal macrosomia: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2019;54(3):308–18.
Araujo Júnior E, Peixoto AB, Zamarian AC, Elito Júnior J, Tonni G. Macrosomia. Best Pract Res Clin Obstet Gynaecol. 2017;38:83–96.
Rowe R, Soe A, Knight M, Kurinczuk JJ. Neonatal admission and mortality in babies born in UK alongside midwifery units: a national population-based case-control study using the UK Midwifery Study System (UKMidSS). Arch Dis Child Fetal Neonatal Ed. 2021;106(2):194–203.
Palatianou ME, Simos YV, Andronikou SK, Kiortsis DN. Long-term metabolic effects of high birth weight: a critical review of the literature. Horm Metab Res. 2014;46(13):911–20.
Richards M, Strickland MJ, Flanders WD, Klein M, Darrow LA. Gestational Weight Gain and Birth Outcome: A Comparison of Methods of Accounting for Gestational Age. Am J Epidemiol. 2022;191(10):1687–99.
Du J, Zhang X, Chai S, Zhao X, Sun J, Yuan N, Yu X, Zhang Q. Nomogram-based risk prediction of macrosomia: a case-control study. BMC Pregnancy Childbirth. 2022;22(1):392.
Perumal N, Wang D, Darling AM, Liu E, Wang M, Ahmed T, Christian P, Dewey KG, Kac G, Kennedy SH, et al. Suboptimal gestational weight gain and neonatal outcomes in low and middle income countries: individual participant data meta-analysis. BMJ. 2023;382: e072249.
Barnes RA, Wong T, Ross GP, Griffiths MM, Smart CE, Collins CE, MacDonald-Wicks L, Flack JR. Excessive Weight Gain Before and During Gestational Diabetes Mellitus Management: What Is the Impact? Diabetes Care. 2020;43(1):74–81.
Barakat R, Pelaez M, Cordero Y, Perales M, Lopez C, Coteron J, Mottola MF. Exercise during pregnancy protects against hypertension and macrosomia: randomized clinical trial. Am J Obstet Gynecol. 2016;214(5):649.e641-648.
Davenport MH, Meah VL, Ruchat SM, Davies GA, Skow RJ, Barrowman N, Adamo KB, Poitras VJ, Gray CE, Jaramillo Garcia A, et al. Impact of prenatal exercise on neonatal and childhood outcomes: a systematic review and meta-analysis. Br J Sports Med. 2018;52(21):1386–96.
Teede HJ, Bailey C, Moran LJ, Bahri Khomami M, Enticott J, Ranasinha S, Rogozinska E, Skouteris H, Boyle JA, Thangaratinam S, et al. Association of Antenatal Diet and Physical Activity-Based Interventions With Gestational Weight Gain and Pregnancy Outcomes: A Systematic Review and Meta-analysis. JAMA Intern Med. 2022;182(2):106–14.
Ruchat SM, Mottola MF, Skow RJ, Nagpal TS, Meah VL, James M, Riske L, Sobierajski F, Kathol AJ, Marchand AA, et al. Effectiveness of exercise interventions in the prevention of excessive gestational weight gain and postpartum weight retention: a systematic review and meta-analysis. Br J Sports Med. 2018;52(21):1347–56.
Society CN: Weight monitoring and evaluation during pregnancy period of Chinese women. 2021.
Physical Activity and Exercise During Pregnancy and the Postpartum Period: ACOG Committee Opinion, Number 804. Obstet Gynecol. 2020;135(4):e178–88. https://doi.org/10.1097/AOG.0000000000003772.
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–81.
Perales M, Artal R, Lucia A. Exercise During Pregnancy. JAMA. 2017;317(11):1113–4.
Persinger R, Foster C, Gibson M, Fater DC, Porcari JP. Consistency of the talk test for exercise prescription. Med Sci Sports Exerc. 2004;36(9):1632–6.
Vinter CA, Jensen DM, Ovesen P, Beck-Nielsen H, Tanvig M, Lamont RF, Jørgensen JS. Postpartum weight retention and breastfeeding among obese women from the randomized controlled Lifestyle in Pregnancy (LiP) trial. Acta Obstet Gynecol Scand. 2014;93(8):794–801.
Sperstad JB, Tennfjord MK, Hilde G, Ellström-Engh M, Bø K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016;50(17):1092–6.
Barakat R, Pelaez M, Lopez C, Lucia A, Ruiz JR. Exercise during pregnancy and gestational diabetes-related adverse effects: a randomised controlled trial. Br J Sports Med. 2013;47(10):630–6.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82.
Mackinnon DP, Cox MC. Commentary on “Mediation Analysis and Categorical Variables: The Final Frontier” by Dawn Iacobucci. J Consum Psychol. 2012;22(4):600–2.
Chen YH, Chou YH, Yang TY, Jong GP. The Effects of Frequent Coffee Drinking on Female-Dominated Healthcare Workers Experiencing Musculoskeletal Pain and a Lack of Sleep. J Pers Med. 2022;13(1):25. https://doi.org/10.3390/jpm13010025.
Wang C, Wei Y, Zhang X, Zhang Y, Xu Q, Sun Y, Su S, Zhang L, Liu C, Feng Y, et al. A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women. Am J Obstet Gynecol. 2017;216(4):340–51.
Voerman E, Santos S, Patro Golab B, Amiano P, Ballester F, Barros H, Bergström A, Charles MA, Chatzi L, Chevrier C, et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: An individual participant data meta-analysis. PLoS Med. 2019;16(2): e1002744.
Champion ML, Harper LM. Gestational Weight Gain: Update on Outcomes and Interventions. Curr Diab Rep. 2020;20(3):11.
Kominiarek MA, Peaceman AM. Gestational weight gain. Am J Obstet Gynecol. 2017;217(6):642–51.
Catalano PM, Hauguel-De Mouzon S. Is it time to revisit the Pedersen hypothesis in the face of the obesity epidemic? Am J Obstet Gynecol. 2011;204(6):479–87.
Bowers K, Laughon SK, Kiely M, Brite J, Chen Z, Zhang C. Gestational diabetes, pre-pregnancy obesity and pregnancy weight gain in relation to excess fetal growth: variations by race/ethnicity. Diabetologia. 2013;56(6):1263–71.
Alberico S, Montico M, Barresi V, Monasta L, Businelli C, Soini V, Erenbourg A, Ronfani L, Maso G. The role of gestational diabetes, pre-pregnancy body mass index and gestational weight gain on the risk of newborn macrosomia: results from a prospective multicentre study. BMC Pregnancy Childbirth. 2014;14:23.
Ferraro ZM, Barrowman N, Prud’homme D, Walker M, Wen SW, Rodger M, Adamo KB. Excessive gestational weight gain predicts large for gestational age neonates independent of maternal body mass index. J Matern Fetal Neonatal Med. 2012;25(5):538–42.
Lindsay KL, Gyllenhammer LE, Entringer S, Wadhwa PD. Rate of Gestational Weight Gain and Glucose-Insulin Metabolism Among Hispanic Pregnant Women With Overweight and Obesity. J Clin Endocrinol Metab. 2022;107(2):e734–44.
Cade WT, Mittendorfer B, Patterson BW, Haire-Joshu D, Cahill AG, Stein RI, Schechtman KB, Tinius RA, Brown K, Klein S. Effect of excessive gestational weight gain on insulin sensitivity and insulin kinetics in women with overweight/obesity. Obesity (Silver Spring). 2022;30(10):2014–22.
Chen Y, Ma G, Hu Y, Yang Q, Deavila JM, Zhu MJ, Du M. Effects of Maternal Exercise During Pregnancy on Perinatal Growth and Childhood Obesity Outcomes: A Meta-analysis and Meta-regression. Sports Med. 2021;51(11):2329–47.
Santos S, Voerman E, Amiano P, Barros H, Beilin LJ, Bergström A, Charles MA, Chatzi L, Chevrier C, Chrousos GP, et al. Impact of maternal body mass index and gestational weight gain on pregnancy complications: an individual participant data meta-analysis of European. North American and Australian cohorts Bjog. 2019;126(8):984–95.
McKinley MC, Allen-Walker V, McGirr C, Rooney C, Woodside JV. Weight loss after pregnancy: challenges and opportunities. Nutr Res Rev. 2018;31(2):225–38.
Herzberger V, Bäz E, Kunze M, Markfeld-Erol F, Juhasz-Böss I. Exercise During Pregnancy. Dtsch Arztebl Int. 2022;119(46):793–7.
Mottola MF, Davenport MH, Ruchat SM, Davies GA, Poitras VJ, Gray CE, Jaramillo Garcia A, Barrowman N, Adamo KB, Duggan M, et al. 2019 Canadian guideline for physical activity throughout pregnancy. Br J Sports Med. 2018;52(21):1339–46.
Acknowledgements
The authors thank all the trial participants. Special thanks are given to the teachers of the Maternity School at Xindu District Central Hospital who were responsible for the specific implementation of the entire study. Finally, we would like to express our gratitude to the experts from Peking Union Medical College Hospital for their careful guidance and supervision during the implementation of this study.
Funding
The study was supported by the National Key Research and Development Program of China (Grant number. 2022YFC2703304), the Medical and Health Technology Innovation Project of the Chinese Academy of Medical Sciences (Grant number. 2020-I2M-2–009, 2021-I2M-1–023) and the Clinical and Translational Medicine Research Fund of the Central Public Welfare Research Institutes of the Chinese Academy of Medical Sciences (Grant number. 2019XK320007). The funders had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
Xuanjin Yang, Yin Sun and Liangkun Ma were involved in writing the study protocol design, data analysis and writing the final article. Guiwang Wang was involved in implementation of the study and data collection. Nana Liu and Yaxing Wang were involved in writing the study protocol. Suhan Zhang and Hang Lin were involved in implementation of the study. Can Zhu and Li Liu were involved in data collection.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The research protocol was reviewed and approved by the Medical Ethics Committee of Xindu District Central Hospital in Xingtai City (reference number: 18) on 25 November 2021. All methods were performed in accordance with relevant guidelines and regulations. All experimental protocols were approved by a named institutional and licensing committee. Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing of interests
The authors report no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, X., Wang, G., Liu, N. et al. Mediating effect of gestational weight gain on the preventive effect of exercise during pregnancy on macrosomia: a randomized clinical trial. BMC Pregnancy Childbirth 24, 384 (2024). https://doi.org/10.1186/s12884-024-06527-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06527-7