Abstract
Background
Pregnant and postpartum women’s experiences of the COVID-19 pandemic, as well as the emotional and psychosocial impact of COVID-19 on perinatal health, has been well-documented across high-income countries. Increased anxiety and fear, isolation, as well as a disrupted pregnancy and postnatal period are widely described in many studies. The aim of this study was to explore, describe and synthesise studies that addressed the experiences of pregnant and postpartum women in high-income countries during the first two years of the pandemic.
Methods
A qualitative evidence synthesis of studies relating to women’s experiences in high-income countries during the pandemic were included. Two reviewers extracted the data using a thematic synthesis approach and NVivo 20 software. The GRADE-CERQual (Confidence in the Evidence from Reviews of Qualitative research) was used to assess confidence in review findings.
Results
Sixty-eight studies were eligible and subjected to a sampling framework to ensure data richness. In total, 36 sampled studies contributed to the development of themes, sub-themes and review findings. There were six over-arching themes: (1) dealing with public health restrictions; (2) navigating changing health policies; (3) adapting to alternative ways of receiving social support; (4) dealing with impacts on their own mental health; (5) managing the new and changing information; and (6) being resilient and optimistic. Seventeen review findings were developed under these themes with high to moderate confidence according to the GRADE-CERQual assessment.
Conclusions
The findings from this synthesis offer different strategies for practice and policy makers to better support women, babies and their families in future emergency responses. These strategies include optimising care delivery, enhancing communication, and supporting social and mental wellbeing.
Similar content being viewed by others
Background
As of February 2024 SARS-CoV-2 has infected over 774 million people, and 7 million deaths have been attributed to coronavirus 19 (COVID-19) infection [1]. Maternal and newborn health services are essential for pregnant and postpartum women, and the COVID-19 pandemic significantly altered provision and access to routine care. Reduced services, limited face-to-face care, transition to virtual and remote care, and limited access to maternity care providers were commonly cited as barriers to accessing quality care by pregnant and postpartum women [2,3,4,5,6]. Additionally, reduced lengths of stay within hospitals and restrictions on support people imposed by health facilities have impacted women receiving care and placed an additional burden on nursing and midwifery staff [7,8,9]. This had significant impacts on pregnant and postpartum women’s emotional and psychosocial wellbeing.
Pregnant women and their babies were at an increased risk of adverse effects if she contracted SARS-CoV-2 [10, 11]. The direct impacts of the COVID-19 pandemic were largely focused on the clinical manifestations of SARS-CoV-2 such as symptoms, risk factors, management and treatment, as well as adverse maternal and newborn outcomes [12,13,14,15]. However, at a wider level, the impacts of policy changes, health system reforms and changes to maternity care services indirectly affected the provision of care for all women giving birth over this time period. Women’s experiences of the transition from pregnancy to motherhood were also impacted. For example, in many countries, pregnant women were encouraged to homestay at home, receive care through telehealth rather than face-to-face and reduce face-to-face education [16, 17]. Isolation from family, friends and peers has negatively impacted women’s mental health, with increased levels of anxiety, depression and stress globally [18,19,20,21].
Since the beginning of the pandemic, there has been a plethora of qualitative studies on women’s experiences [19, 22,23,24,25,26] – the significant volume of papers highlights the need for a clear synthesis. Reviews of qualitative evidence have reported pregnant women’s experiences of social support [27], as well as highlighting the challenges they faced as they embraced motherhood during the pandemic [28]. Collating the evidence in a systematic and transparent manner will allow policymakers to consider the indirect implications of public health restrictions on the physical, emotional, and psychosocial health and wellbeing of pregnant and postpartum women.
Qualitative evidence synthesis (QES) is an approach that can systematically collate qualitative data in a transparent manner to inform policy and practice [29]. Findings from a QES can enable a richer interpretation of a particular phenomenon and enable a greater understanding of individual experiences, views and beliefs [30]. This QES aimed to explore, describe and synthesise the experiences of pregnant and postpartum women living in high-income countries during the first two years of the COVID-19 pandemic. This research method allows a deeper understanding of their views and experiences during this time. It also facilitates identification of areas of improvement for maternity care services, to ensure high-quality care is available at all times.
Methods
A QES was undertaken to identify, evaluate and summarise findings from qualitative studies providing a cohesive and transparent documentation of the contextual variations, stakeholder preferences and experiences to ultimately influence policy and practice [31, 32]. This type of synthesis integrates diverse perspectives, which is needed to capture the complexity of the indirect impacts of the COVID-19 pandemic on pregnant and postpartum women’s experiences. This QES was structured to include findings from qualitative studies, as well as qualitative findings from mixed-methods studies. Emphasis was placed on including different types of qualitative evidence that can potentially enrich a synthesis, such as narrative data from qualitative components of mixed-methods studies or free-text from questionnaires [29].
We followed the relevant Cochrane guidelines [29] and used the “Enhancing transparency in reporting the synthesis of qualitative research” (ENTREQ) statement to guide our approach and reporting (Supplementary 1, S1) [33]. In addition, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for reporting the different phases of identifying studies was used as recommended by the ENTREQ statement (S2) [34]. The protocol and systematic review were not registered.
Eligibility criteria
We defined “indirect impacts of the pandemic on women”, to mean the impact of regulations, recommendations and public health measures enforced by governments as a response to the COVID-19 pandemic had on pregnant and postpartum women and their newborns. We adopted the World Health Organization’s definition of the postpartum period beginning immediately after birth of the baby and extending to six weeks (42 days) after birth [35].
Participants within these studies were those who were pregnant or within the postpartum period, of childbearing age (15-49 years), and received any type of maternity care during the COVID-19 pandemic. Studies of women with pre-existing comorbidities were also eligible, as well as those focused on migrants, refugee populations or ethnic minority groups. To facilitate exploration of findings from women of diverse backgrounds we have used the term ‘culturally and linguistically diverse (CALD) populations’. We focussed on women living in high-income countries (HICs). Studies were included if they were conducted in countries listed in the Organisation for Economic Co-operation and Development (OECD) [36] and Human Development Index (HDI) list of “Very high human development” list [37]. This allowed for similar contexts and countries to be compared.
Eligible study designs were those that addressed the indirect impact of COVID-19 using qualitative methodologies, including phenomenology, ethnography, grounded theory studies and case studies. We also included any study that obtained data through qualitative methods for data collection such as, interviews, focus groups, online forums and document analysis.
The decision to limit the eligibility based on year of publication, to only include studies published in the first two years of the COVID-19 pandemic (1st Jan 2020 – 1st Jan 2022) was to emphasise the impact of the stricter restrictions and lockdowns during this time period. Globally, public health measures to reduce spread and transmission included, mandatory quarantine, limiting movement, lockdowns, closure of schools and workplaces and shielding of vulnerable populations. These measures were significantly harsher during the first two years and subsequently relaxed as vaccine roll-outs occurred and infection rates began to decline [38, 39]. The Oxford Coronavirus Government Response Tracker reported a stringency index which reiterates the trend of harsher restrictions implemented by governments throughout 2020-2022 time period and reflects the gradual decline after this date [40].
Search strategy
Six electronic databases (EBSCO Medline, Embase, APA PsycInfo, CINAHL and Maternity and Infant Care (MIDIRS)) were searched to identify all qualitative research articles published between 1st January 2020 – 1st January 2022. Search strategy included terms such as, “pregnan*”, “postpartum”, “mother”, “views”, “experiences”, “opinion*”, “indirect”, “COVID-19”, “coronavirus”. The search strategy was reviewed by a university librarian (S3). Search hits from each of the databases were imported into Endnote 20 which was then used as our reference library. References were imported into Covidence for screening [41].
Study selection and sampling framework
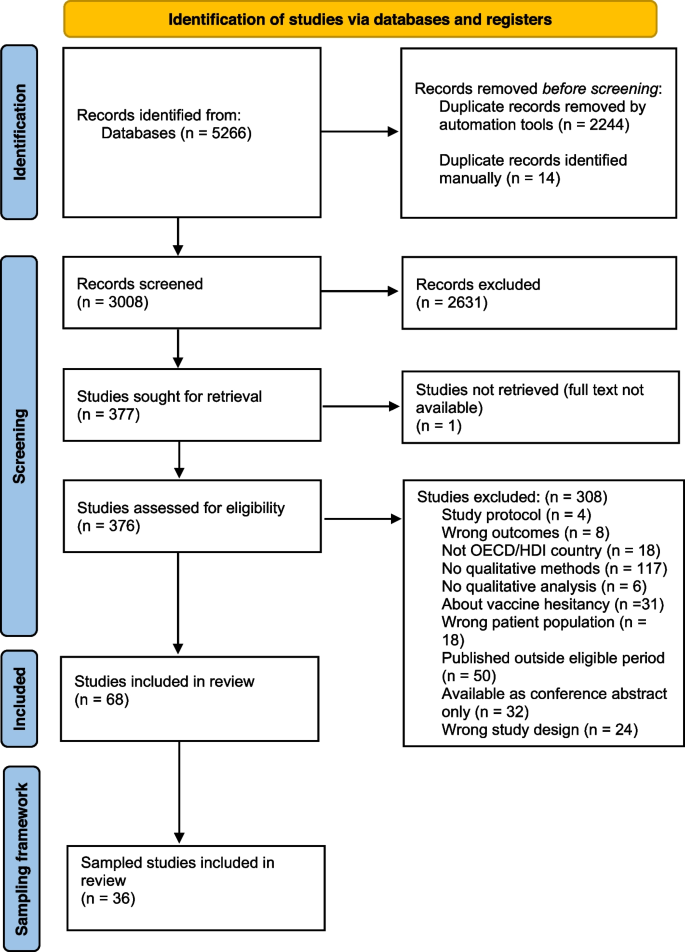
Two review authors (AT, AB) independently screened titles, abstracts and full texts for inclusion, with any conflicts resolved by discussion or consulting a third author. Reasons for exclusion are described within PRISMA flowchart (Fig. 1). Sixty-eight studies were included following full-text review. The Cochrane guidelines for QES highlight that for reviews with large amounts of primary studies (50 or more) can result in a high volume of data, which can threaten quality of the synthesis. In such situations, a sampling framework can enhance the quality and diversity of the papers and ensure the number of studies and amount of data are manageable [42,43,44]. A QES worked example by Ames et al., 2019 was used as a guide to develop the sampling framework for data richness [45]. Two independent reviewers scored included studies from 1 to 5 based on the criteria outlined in Table 1, to ensure that the sampling framework was reliable and replicable. Any conflicts were resolved by discussion, or a third review author was consulted. Studies with a score ≥4 were included for data extraction and are referred to as ‘sampled’ studies (S4).
Reporting of adapted PRISMA flowchart of included and sampled studies in accordance with PRISMA and ENTREQ guidelines [33]
Quality assessment
The Critically Appraisal Skills Program (CASP) tool for qualitative research was used by two independent review authors (AT, AB) to assess methodological limitations of sampled studies (S5) [46]. Any disagreements were resolved through discussion, or when required, a third review author was consulted. Sampled studies were graded as no or very minor, minor, moderate or severe concerns with methodological limitations.
Data extraction and synthesis
A “Characteristics of sampled studies” table was created in Excel and details are reported in Table 2. Two independent reviewers familiarised themselves with the sampled studies and extracted key themes using Braun and Clarke’s reflexive approach to inductive and deductive thematic analysis [47]. Data were managed using NVivo 20 [48]. This was an iterative process as many of the themes and sub-themes overlapped and were relevant in many aspects throughout the perinatal period (Table 3). The findings were developed iteratively, and periodically shared with the broader team to evolve our interpretation. Any quotes taken from studies were selected as they reiterated findings, and provided additional depth and meaning to review findings.
Extracted data were populated into two tables for analysis. The first table collated quotes and author interpretations of findings (S6), whilst the second table summarised these into review findings (Table 4).
Assessment of confidence in the review findings (GRADE-CERQual)
The GRADE-CERQual tool assesses the confidence in review findings from qualitative evidence syntheses [83]. Lewin et al., 2018 state that that “the approach has been developed to support the use of findings from qualitative evidence syntheses in decision-making, including guideline development and policy formulation” [83]. The GRADE-CERQual Interactive Summary of Qualitative Findings (iSoQ) online platform was used to manage and assess confidence in review findings [84].
Confidence in review findings was determined based on four criteria: methodological limitations, coherence, adequacy and relevance [83]. For each criterion, review authors determined if there were no or very minor, minor, moderate or serious concerns. An overall GRADE-CERQual assessment of confidence was placed on the findings, levels included: high, moderate, low and very low confidence. Review findings are considered at the highest confidence level and downgraded as there are greater concerns for each individual criterion (Table 4). This process was conducted by two authors, with any disagreements resolved through discussion and consulting other authors.
Managing our own reflexivity
Throughout the conceptualisation, data collection and analytical process, the authors considered their own individual views and beliefs about maternity care during the COVID-19 pandemic. As clinicians and researchers working on maternity care (including during the pandemic), we recognised that the COVID-19 period impacted indirectly on women and babies, including their experiences of care, their own anxieties and worries. We are public health professionals with diverse backgrounds including nursing and midwifery, maternal and newborn health, epidemiology and qualitative health research. We met regularly, both to explore the findings and the processes but also to ensure that we separated our individual experiences and beliefs on the interpretation of the analysis and the findings. Employing a systematic and transparent approach to the analytical process, such as including reflection notes after analysing each sampled paper, facilitated collaborative discussions, ensure objectivity and reduced the impact of personal biases.
Results
A total of 36 studies contributed to the synthesis of qualitative evidence to understand pregnant and postpartum women’s experiences during the first two years of the pandemic. There were six over-arching themes: (1) dealing with public health restrictions; (2) navigating changing health policies; (3) adapting to alternative ways of receiving social support; (4) dealing with impacts on their own mental health; (5) managing the new and changing information; and (6) being resilient and optimistic. Seventeen sub-themes were developed within these 6 themes and illustrative quotes are presented in Table 3 to demonstrate theme development. Themes were categorised to differentiate major disruptors to the pregnancy and postpartum period and sub-themes aimed to categorise the indirect impacts that occurred within the major themes.
Characteristics of contributing studies
After applying the sampling framework (data richness score ≥4), 36 sampled studies were included for data extraction and analysis. Thirteen out of 36 studies had a score of 5 [49, 52, 57, 58, 61,62,63, 66, 68, 69, 71, 77, 82], with the remainder scoring 4 [9, 16, 50, 51, 53,54,55,56, 59, 60, 64, 65, 67, 70, 72,73,74,75,76, 78,79,80,81,82] (S5). Most studies (N=27/36, 75%) used specific qualitative methodologies, six were mixed-methods studies, two were cross-sectional studies, and one was a case series report.
Studies were conducted across nine countries, almost one-third (N=10/36, 28%) of studies published from the UK, Canada (N=7) and the USA (N=7) (Table 2). Country-specific responses to the pandemic largely included border closures, mandatory lockdowns and restrictions on movement; it is interesting to note that Sweden did not mandate this but instead enforced social distancing practices [68]. Additionally, some studies reported on a specific sub-population of pregnant and postpartum women, for example women from ethnic minority groups, those with pre-existing comorbidities, and those who were COVID-19 positive. Some studies also included results from women with babies who were greater than 6 months of age, and any findings directly from these participants were omitted from analysis where possible.
The number of participants in studies that conducted interviews ranged from 3 to 84, and studies using qualitative data from open-ended questions or survey data included responses from 16 to 4,611 participants. Where demographic data were available, approximately 1,192 women were primiparous (having their first baby) and approximately 8,017 women were surveyed or interviewed postpartum. Sampled studies were generally of high quality and assessment of methodological limitations indicated that 29 studies were assigned “no or very minor concerns”, six studies were assigned “minor concerns”, and one study was assigned “moderate concerns”. When available, quotes obtained from studies have included additional demographic data. Factors included pregnant or postpartum status at time of data collection, parity and geographical location.
Theme 1: Dealing with public health restrictions
The rapid introduction of public health restrictions has had adverse effects on mental health, social isolation, and the pregnancy experience. Women had to navigate these restrictions and adapt accordingly, realising quickly that their pregnancy and postpartum experience was going to be very different from their expectations.
Sub-theme 1.1. Limited support networks from health care system and providers (High confidence)
Support networks were limited. Women felt that they were “on their own”, “unimportant or irrelevant” or treated as “second class citizens” after birth, because of a lack of physical supports from healthcare providers [51, 60,61,62, 70, 72, 74]. Limited or no access to physical and social support networks was commonly cited as a reason for deteriorating mental health.
Sub-theme 1.2. Balancing exposure risk and need for healthy behaviours (High confidence)
Women balanced COVID-19 exposure risks by shielding, either because of health providers recommendations [16, 69] or because they felt it was needed to protect their baby [50, 68, 71, 77, 81]. Women delayed or postponed antenatal appointments [50, 57, 69, 72, 82], opted for induction of labour [74], or waited until labour was quite advanced before attending hospital [60, 61, 77]. These decisions were due to pandemic-induced fear, and the perceived risk of infection in a high-risk environment such as the hospital [16, 56, 80].
Sub-theme 1.3: Missing out on social opportunities (High confidence)
Women felt sad, unseen and heartbroken that they were not able to have social opportunities, especially sharing their newborns with family and friends [9, 54, 56, 61, 66, 70, 71, 75, 76]. On postnatal wards, women with older children were disappointed that their nuclear families could not visit and bond with their newborn in the early postpartum period [56, 59, 80, 82]. While this was disappointing for many, one woman described still feeling well-supported, “we were supposed to have a baby shower, the weekend after everything shut down … definitely got a lot of gifts in the mail and people who drop things off …. [we] feel like even though he’s being born in this super crazy time and he doesn’t necessarily get to meet people in person, that they are excited about him and want to support us” (USA) [52]. Primiparous women felt that they missed the opportunity to share many “firsts” with extended families - one woman said, “this is my family’s first grandchild so it just breaks my heart they will miss her whole babyhood” (postpartum, Canada) [64].
Sub-theme 1.4: Breastfeeding challenges and triumphs (High confidence)
Women that struggled with the lack of support around breastfeeding said, "when it came time for breastfeeding, I had no idea what to do or any challenges that could come. There were so, so, so many questions and I felt so confused during everything” (postpartum, primiparous, UK) [60]. Lactation consultations through virtual remote care was considered inadequate by most women [51, 66, 71, 73, 75], especially when practical hands-on education and assistance was needed [51, 53, 72, 77]. These challenges led some women to cease breastfeeding early [51, 62, 73].
Conversely, public health restrictions enforcing women to stay at home allowed some women to practice responsive breastfeeding, without concern for social obligations or visitors [51, 62, 64, 71, 75, 79]. Some women valued this flexibility - “there’s no right or wrong way. You know, at the end of the day the ultimate goal is that my baby needs to be fed.… you know, feed him breast milk, breast milk, or formula. He’s fed. He’s happy. Sweet. That’s done. Job done! The important thing is actually [to] be kind to yourself, you know?” (postpartum, primiparous, UK) [62].
Challenges and triumphs were felt by both multiparous and primiparous women [51]. The difference between experienced and first-time mothers was stark in some studies, highlighted by multiparous women who felt ‘knowledgeable’ and ‘had the experience’, and sharing empathetic messages towards primiparous women with limited breastfeeding support [62, 78].However, the lack of face-to-face breastfeeding support meant that first-time mothers and experienced mothers also faced hardships. As one mother recounts her sadness: “I had virtual appointments [with lactation consultants], which I found totally useless… I was devastated that it wasn’t working with [the new baby] because it was something I was really looking forward to” (postpartum, multiparous, Canada) [73].
Theme 2: Navigating changing health policies
The ever-changing nature of the pandemic created periods of uncertainty. Women and their families were expected to accept and adapt to changing health policies which directly impacted their antenatal, labour and birth and postnatal experiences.
Sub-theme 2.1: A birthing experience filled with uncertainty and unknowns (High confidence)
Many women reported that, given the constantly changing policies, they were unsure what to expect for their labour and birth [9, 49, 60, 75, 77]. Limitations included not being able to have a water birth, use a bath or the shower, access nitrous oxide gas during labour [49, 74, 82] and others could not have their desired support people present [60, 77]. In some cases, women opted for medicalised interventions to retain a sense of control - choosing a caesarean birth to ensure their partner was present at birth [60, 74]. Women struggled with the prospect of early discharge, lacking confidence and fearing reduced support at home, with some feeling pushed out of the hospital [49, 53, 60, 74]. Some women chose to leave hospital early due to the lack of support or poor experiences while in hospital [60]. Conversely, some women welcomed early discharge, wanting to be away from the hospital and to be reunited with family members [62, 80]. Women who tested positive to COVID-19 early in the pandemic described additional challenges, such as a lack of certainty on how care was going to be managed [77]. They felt this restricted their autonomy over their labour and birth choices.
Sub-theme 2.2: Reduced support and partner presence healthcare settings (High confidence)
Due to the public health restrictions in hospitals, women often missed having their partner and family supports [16, 49, 57, 66, 71]. For example, “one of my coping mechanisms is having my partner there to hear the same things I am hearing because I kind of shut down sometimes when I get too upset. It’s always good to have that second person listening… and walking out with strength of unity” (pregnant, primiparous, Australia) [49]. The inability for some women to have their partners present negatively impacted women’s birthing experience [53, 70, 79, 80], confidence on the postnatal ward and many expressed the sense of being “robbed of this experience” (pregnant, UK) [75].
Sub-theme 2.3: Transitioning to telehealth, virtual and remote care (Moderate confidence)
Public health restrictions limited face-to-face health care appointments with a maternity care provider [54]. Negative telehealth experiences were expressed predominantly by first-time mothers [71], with many saying, “over the phone just doesn’t do it… you don’t get to look into somebody’s eyes and to trust them and for them to say, you’re okay” (postpartum, Ireland), adding to their anxieties. This was felt similarly by CALD women as there was a disconnect with health care providers using virtual methods and this was exacerbated for women who were not able to access interpreters [80]. Positive encounters with telehealth were associated with the increased accessibility to health services and generally preferred by multiparous women [54, 65, 68]. Whilst many were glad that telehealth services were available, this woman highlighted the inequities, “I think I would question the accessibility of that. Not everyone has a smartphone and expecting people to be able to receive a video call is not necessarily the most inclusive thing” (postpartum, primiparous, UK) [77] indicating that some women may have fallen through the gaps of maternity care.
Sub-theme 2.4: Barriers to accessing health services (High confidence)
The closure of so-called non-essential services, such as, physiotherapists, chiropractors, pools and gyms indirectly impacted women [66, 74]. This often increased women’s anxiety, stress, feelings of helplessness and frustration [16, 54, 60, 74] and incidence of postnatal depression [82]. This also limited opportunities to receive reassurance from healthcare providers, reducing women’s confidence [49, 71, 72, 77]. Typically, women accessed networks for information and support, such as, family and friends with midwifery clinical expertise, or referred to recent pregnancy experience [52, 68, 75, 79]. Women had to advocate strongly for physical assessments for themselves and their newborns [74].
Additionally, women from CALD populations were challenged in accessing culturally appropriate care with changes to interpretation services, “it creates like a…a gap in communication where if something you express is not clearly understood so maybe they could be left with some misinterpretation” (UK) [63]. Another example of the inequities faced by CALD women was expressed by this woman who did not receive interpretation services during appointments, “sometimes they explained things to me by using signs and I understand a little English but it’s hard to understand medical terms and they didn’t use an interpreter for this” (postpartum, multiparous, Canada) [80].
Theme 3: Adapting to alternative ways of receiving social support
Support networks, such as, family and friends, peer support groups (e.g. mother’s groups), and formal support from maternity care providers provide the foundation for a healthy and positive pregnancy and postpartum period. The COVID-19 pandemic forced women to adapt and seek support in different ways.
Sub-theme 3.1: Accessing support through different avenues (Moderate confidence)
Support from family and friends was accessed in different ways, for example, utilising video call technologies to be able to see faces helped with the grief of not being able to be present [16]. Women who were able to establish pregnancy and mother’s groups during the pandemic were grateful that they had these supports. Alternatively, women created or sought support through online social media platforms [61, 68, 70, 81], to share a sense of camaraderie that they were not alone in their experiences [52, 77]. In these forums, women shared information about COVID-19 developments, updates to hospital policies, and utilised others as sounding boards for advice. Some women reported greater support from partners who had transitioned to working from home [51, 62, 64, 66, 75]. Although virtual technologies allowed women to bridge the gap of social distancing, they wanted the physical connection with others.
Sub-theme 3.2: Desiring connection with family and friends (High confidence)
Women felt they needed intergenerational support to raise their newborns, and this was especially important during difficult times. Many had planned for parents to come and support them [81], as they believed that, “the older generation have more experience on what babies need or what they feel… with my other two [children]… they knew exactly what would make them feel better” (pregnant, multigravida, Australia) [49]. Some women struggled without the additional support, the lack of sleep impeded their physical wellbeing [61, 73, 75], and the isolation from family impacted their mental health [9, 49, 56, 60, 61, 73]. In some cases, women were able to “quarantine with family”, providing women with a “strong support network” (postpartum, Canada) as they transitioned into motherhood [59]. Gradually, as public health restrictions eased, women from the UK felt government responses did not consider new mothers and babies and they called for “social bubbles” for families to receive the additional support [62, 72]. The loss of informal support networks was apparent for some CALD women. As this woman said, “it was really hard during COVID. In Syria I had my family… but to give birth here with no one with me?! I needed someone with me, my neighbours, my friends… I felt like I was drowning” (postpartum, multiparous, Canada) [80].
Theme 4: Dealing with impacts on their own mental health
The COVID-19 pandemic placed a significant toll on pregnant and postpartum women’s mental health at all stages of the pandemic. Public health strategies failed to include protective measures for mental health, as such many women reported increased levels of fear, anxiety, stress, loneliness and depression.
Sub-theme 4.1: Managing anxiety due to virus-related fears and concerns (Moderate confidence)
Women often experienced anxiety exacerbated by the pandemic, for example, “as a new mom you are already so nervous, so adding a pandemic to that pile of anxiety and worry” (postpartum, Canada) [70]. This was related to possibility of infection, particularly in hospital and healthcare settings [9, 56, 57, 69, 82], and the need to protect their unborn or newborn baby [50, 72, 80]. Some faced additional challenges as migrants from another country, “I found it very hard when you’re coming to the country without knowing anyone and the coronavirus, lockdown was very difficult, I was very depressed. I was very anxious… I feel worried a lot” (UK) [63].
Sub-theme 4.2: Feeling lonely and isolated (High confidence)
Loneliness and isolation were commonly reported as women faced motherhood alone without their usual support systems. One woman said, “it was quite sad that I couldn’t even share my pregnancy experience with anyone, and I feel like I missed out” (postpartum, Australia) [54]. Feelings of loneliness was especially felt by mothers who were not able to have their partners present during birth or postnatally [61]. Women were not able to build supportive peer networks in their antenatal and postnatal periods [49, 62, 73,74,75, 78, 81], with one woman saying, “there’s nothing like just meeting people or, just naturally building friendships when you go to baby groups” (postpartum, multiparous, UK) [62] emphasising the importance of developing social relationships. Cancellation of appointments and lack of face-to-face care added to feelings of “abandonment” and “being forgotten” [9, 60, 62, 70, 72, 73].
Theme 5: Managing new and changing information
Due to the novelty of COVID-19 and lack of information about adverse effects, maternity care services had to rapidly adapt as new data came to light. Women described the need to search, access and filter useful information, a process which was challenging for many.
Sub-theme 5.1: Constantly changing advice and information (High confidence)
The constantly changing advice was distressing [82]. These changes meant a lot of uncertainty, one woman said, “at 34 weeks I had a telephone appointment and I tried to ask what the changes in hospitals were, because of COVID and talk about the birth plan. She basically said, ‘everything is changing so quickly there is no point in us even talking about that now. Wait until your next appointment’” (postpartum, primiparous, UK) [77]. This limited women’s ability to adequately plan and prepare for the birth. Some women described following the updates from government officials and hospitals overwhelming [66]. As restrictions eased, women described the frustrations they had with the slow adaptations by health services, “when I got to the hospital, they didn’t know about the restrictions having been lifted … That was really frustrating because I was like why? Why does this hospital not know?” (Australia) [82] and the differences between health services, “restrictions have still not been lifted in ‘Hospital A’ whereas they have been eased in both ‘Hospital B’ and ‘Hospital C’” (pregnant, multiparous, Ireland) [9].
Sub-theme 5.2: Inadequate information from healthcare providers (Moderate confidence)
Women felt there was not enough information from healthcare providers, “I think there was a lot of confusion; there was no good communication about what was happening to appointments. You weren’t really sure; were they happening on the phone [telehealth], when were you going to get the call? There was very little communication. So, I always felt a bit uneasy about that…” (postpartum, primiparous, UK) [77]. Some information was contradictory [60] for example, “I’ve found the disconnect between the information that my GP was getting and that the [hospital] was getting – they weren’t getting the same” (Australia) [82]. Women wanted clear information that was easily accessed by the lay person [9, 16, 54, 61, 65,66,67,68, 75]. They also wanted uncertainty to be acknowledged, “it would have been useful to have some generic information that went out to women in that situation… statements from a medical professional to put people’s minds at ease” (postpartum, Australia) [54].
Theme 6: Being resilient and optimistic
Many women were self-reliant and took it upon themselves to remain positive and proactive throughout the perinatal period.
Sub-theme 6.1: Self-help strategies to overcome challenges of the pandemic (High confidence)
Women developed their own strategies to find solace and support [77]. When asked what advice they had for other women in similar situations, advocacy for oneself was frequently reported [66, 67, 70, 71, 77, 79, 81, 82]. In contrast, another woman regretted not voicing her concerns, “I have naively trusted that the hospital gives me the information I need … Then I realized afterwards that there were many moms who were much angrier than me and said much more; insisted much more… and I simply did not; I regret it a bit” (postpartum, Norway) [67]. Women reported coping using different strategies, such as being outdoors and active [16, 52, 54], limiting news and access to social media platforms [54, 69, 70, 81], seeking professional help [58, 73], informing themselves about the virus [58, 71], drawing on their own faith and religion [52, 69] and self-reassurance [50, 52, 62]. Many complied with public health restrictions, however there were some women that decided their mental health and physical wellbeing was more of a priority and broke public health restrictions to seek support from family and friends [62, 66, 73]. Despite the challenges faced during the pandemic, some women reported high resilience, positive childbirth and postnatal experiences, and feeling empowered by their ability to overcome challenging circumstances [54, 58, 74].
Sub-theme 6.2: Making the most out of the positive encounters (Moderate confidence)
The lack of visitors on the postnatal ward and in homes was described by women as “pleasant”, “relaxing” and a “blessing in disguise” as women were able to recover and establish undisrupted routines with their newborns [54, 71, 72]. A commonly reported positive outcome of limiting social obligations was the ability to establish successful breastfeeding, one woman said, “I was inundated with visitors with my first child and often could not feed responsively… With my second child, there is none of that pressure and I can really see an enormous difference both is his feeding and in my mental health” (postpartum, UK) [51]. Women also described health services as “peaceful”, as there were fewer people in waiting rooms, appointments were quick, social distancing was enforced and use of PPE limited the possibility of transmission [16, 49, 71, 75, 81, 82].
Sub-theme 6.3: Information seeking and desire for more information (Moderate confidence)
Women obtained information from official government documents, guidelines released by professional bodies, the news, social media and platforms run by professional academics [53, 66, 68, 72, 81]. Reasons to seek information included: to clarify any uncertainties about risk and infection, keep up to date with COVID-19 guidelines and to be informed about changes to hospital policies [49, 52, 66, 69, 77]. Even once women were provided with information, poor communication and follow up left women feeling dissatisfied [54]. One woman shared advice about engaging with different information sources – “you can’t just trust them – you’ve got to decipher through what’s true and what’s not… Is that actually having a positive influence on me, and my mental and physical health, or not? And if it’s a no, well why am I engaging in this?” (Australia) [81].
Discussion
This QES synthesised data from 36 sampled studies on pregnant and postpartum women’s experiences from high income countries during the COVID-19 pandemic. Findings were categorised under six overarching themes and 17 review findings to understand their experiences as the pandemic unfolded. Women had to navigate the transition from pregnancy to motherhood, whilst also adapting to the complexities of the COVID-19 pandemic. High to moderate confidence was placed in these review findings, indicating the strength of the evidence.
This review highlights that pregnant and postnatal women across high-income countries faced similar yet inherently unique experiences and challenges. During the pandemic, primiparous women faced moderate-to-high prenatal stress levels, as they recounted their first pregnancy experience during a time of significant uncertainty [85,86,87]. On the other hand, some evidence highlighted that multiparous women were ‘adaptive’ and felt ‘prepared’ [66, 71, 77]. However this was not experienced universally - many experienced mothers facing difficulties [9, 73, 80]. The COVID-19 pandemic and associated public health restrictions across high-income countries disrupted access and quality of care for many pregnant and postpartum women.
Reduced health service capacity and the transition to remote and virtual care due to pandemic restrictions have been heavily criticised [8, 88]. In many contexts, women had not received high quality maternity care during the pandemic and described overtly negative experiences [35, 89, 90]. Women were unable to access usual supports, had limited birth choices and reduced postpartum care which resulted in stress and anxiety. These are clearly widespread experiences, regardless of context, and highlights some of the structural weaknesses and vulnerabilities of maternity care systems. This was evident in the findings for pregnant and postpartum women of culturally and linguistically diverse backgrounds. The lack of culturally appropriate care, including access to interpretation services, doulas and being unable to have their support person present are known to impair maternal health and wellbeing [56, 63, 80]. These factors are key elements of respectful maternity care as they help provide information, enable women’s agency and ensure emotional and social support is available [91, 92]. Health restrictions should not limit this service for women during times of unrest, as women and babies thrive in culturally respectful maternity services [93]. We note however that CALD women continue to be an under-represented group - only three of the 36 sampled studies reported evidence specifically for CALD groups [56, 63, 80]. The lack of diverse perspectives included in the evidence base makes it more difficult for culturally sensitive and community-responsive policies to be developed. Further research with women from diverse backgrounds are warranted to ensure they are not unduly disadvantaged in future pandemics [94].
A key finding was the reduced presence of partner and social support throughout the pregnancy and postpartum periods. Partner support and strong connections with extended support networks reduces stress and anxiety, and can be a positive influence on the woman and her experience [95,96,97]. In the trade-off between the risk of transmission and spread of disease, expectant fathers and partners were frequently left out [98, 99]. Similarly, studies of families and partners of intensive care unit patients during the COVID-19 pandemic reported being physically and emotionally unable to support partners and families [100, 101]. Close family members are essential to the recovery of patients upon discharge and partners are integral to a safe and positive pregnancy, intrapartum and postpartum experience for mothers. To ensure that maternity care services can adequately respond in the future, recommendations for some degree of flexibility for women given the long-term psychosocial impact that a negative experience would have on the woman and family unit has been sought [8, 87, 88].
Pregnant and postpartum women’s experiences were not universally negative. Another key finding in this review highlights the resilience and optimism that some women felt. Some women perceived this time as a “blessing in disguise” – referencing the ability to stay at home, having fewer disruptions to breastfeeding, and embracing newfound time as a family unit [64, 66, 71]. Coping strategies reported in this study are supported by other evidence of protective factors against stressors of the COVID-19 pandemic [102,103,104].
Maternity care services need to continue delivering care during public health emergencies. There is no possibility of delaying or postponing care; and women require care over an extended period of time. Enforced lockdowns limited movement and fear of contracting the virus in hospitals lead to delays in healthcare seeking (e.g. when there is reduced fetal movements). The pandemic altered the provision of services and women’s access to care and, as a result, some countries have reported changes to the incidences of stillbirth and preterm birth [105,106,107].
Understanding women’s experiences, their preferences and satisfaction with maternity care services are essential to a safe and positive pregnancy, labour and childbirth and postpartum period. Many maternity models of care such as woman-centred and midwifery-led care places the woman at the centre of care and her experience, focusing on woman’s health needs, expectations and aspirations [108, 109]. These models have proven to return high levels of satisfaction and are beneficial to the psychological and physiological recovery of the woman [110, 111]. The COVID-19 pandemic has disrupted these models of care for women who were pregnant and gave birth during the pandemic. Pressures on the maternity care system and service delivery did not facilitate the midwife-woman relationship, resulting in poorer clinical outcomes [112]. Supporting women throughout their perinatal period is essential so women and their babies are able to emerge from the experience feeling prepared, safe and satisfied [113, 114].
Moving forward, as maternity care systems adapt to a post-pandemic structure, considerations need to be made to ensure maternity services can adequately respond to future health crises. Our QES has shown that the impacts of COVID-19 went far beyond the direct impacts on women who were infected with SARS-COV2. All women giving birth over the pandemic, especially in the first two years, were indirectly impacted and as a result experienced a lack of autonomy during their pregnancy and childbirth, barriers to accessing face-to-face care and loss of social supports. This highlights the need to consider women’s views and experiences in developing policies for future responses to pandemics or public health emergencies.
We recommend that policy makers and maternity care services should: 1) optimise care delivery to maintain face-to-face care when possible and facilitate the presence of chosen support people; 2) enhance communication channels between maternity care services and women to minimise misinformation, stress and anxiety; and 3) support social and mental wellbeing to ensure women have access to adequate social support and mental health services are well resourced.
Strengths and limitations
The rigorous and systematic methodology of this QES in selecting studies for inclusion allowed us to analyse experiences of a heterogenous cohort of pregnant and postpartum women during the COVID-19 pandemic. When we started the review, the abundance of published work of women’s experiences was overwhelming, therefore strict eligibility criteria were used to ensure that findings could be obtained and compared across studies. This study was therefore limited to experiences of women in high-income countries and cannot be generalised to low- and middle-income countries.
Studies were subject to a sampling framework to ensure that a diverse, yet data rich sample of studies contributed to the development of review findings. This had its own set of limitations as the sampling framework is not a validated tool and may be biased by the user’s own interpretation. Additionally, the search strategy was limited to the first two years of the pandemic. While it is possible research was published outside of this two-year period, we felt that it was unlikely that different experiences would be reported. An updated search (December 2022) was conducted to determine if any new themes emerged, however no new themes emerged and therefore did not warrant the addition of any new studies. Almost all studies that used interviews to collect qualitative data did so via remote methods. Telephones and video conferencing tools were popular methods to conduct interviews, adhering to social distancing guidelines. Whilst this increased accessibility for participants from diverse geographical locations, there may be concerns about the depth of data obtained and exclusion of participants that are unable to access these technologies. A further consideration is the limited number of studies exploring the experiences of women from diverse backgrounds. This prevented us from more critically examining what factors and circumstances shape women’s experiences and responses.
Conclusion
Women’s pregnancy and postpartum experience during the COVID-19 pandemic showcased similarities despite different contexts. This QES has collated the experiences of women from high income countries sharing insight into the challenges faced and resilience of pregnant and postpartum women. The COVID-19 pandemic has exacerbated many systemic shortfalls of the maternal and newborn health system – a system that is essential to the health and wellbeing of women and babies. The review findings have highlighted areas within this period where strategies to inform policy and practice could be optimised to allow for better access to care and support for women in their journey to motherhood. Future pandemic preparedness strategies need to maximise face-to-face care, optimise communication channels to combat misinformation and anxiety, include a flexible approach to public health restrictions for women and their families by allowing formal and informal support networks to be readily available and accessible, and to ensure maternal mental health is a priority.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files]. Additional information is available from the corresponding author on reasonable request.
References
World Health Organization (WHO). WHO Coronavirus (COVID-19) Dashboard World Health Organization; 2021. Available from: https://covid19.who.int/.
Fisk M, Livingstone A, Pit SW. Telehealth in the Context of COVID-19: Changing Perspectives in Australia, the United Kingdom, and the United States. J Med Internet Res. 2020;22(6):e19264.
Montagnoli C, Zanconato G, Ruggeri S, Cinelli G, Tozzi AE. Restructuring maternal services during the covid-19 pandemic: Early results of a scoping review for non-infected women. Midwifery. 2021;94:102916.
Zaigham M, Linden K, Sengpiel V, Mariani I, Valente EP, Covi B, et al. Large gaps in the quality of healthcare experienced by Swedish mothers during the COVID-19 pandemic: A cross-sectional study based on WHO standards. Women and Birth. 2022;35(6):619–27.
Coxon K, Turienzo CF, Kweekel L, Goodarzi B, Brigante L, Simon A, et al. The impact of the coronavirus (COVID-19) pandemic on maternity care in Europe. Midwifery. 2020;88:102779.
Javaid S, Barringer S, Compton SD, Kaselitz E, Muzik M, Moyer CA. The impact of COVID-19 on prenatal care in the United States: Qualitative analysis from a survey of 2519 pregnant women. Midwifery. 2021;98:102991.
Galle A, Semaan A, Huysmans E, Audet C, Asefa A, Delvaux T, et al. A double-edged sword—telemedicine for maternal care during COVID-19: findings from a global mixed-methods study of healthcare providers. BMJ Global Health. 2021;6(2): e004575.
Kotlar B, Gerson E, Petrillo S, Langer A, Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reproductive Health. 2021;18(1):10.
Meaney S, Leitao S, Olander EK, Pope J, Matvienko-Sikar K. The impact of COVID-19 on pregnant womens’ experiences and perceptions of antenatal maternity care, social support, and stress-reduction strategies. Women and Birth. 2021;35(3).
Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370: m3320.
Villar J, Ariff S, Gunier RB, Thiruvengadam R, Rauch S, Kholin A, et al. Maternal and Neonatal Morbidity and Mortality Among Pregnant Women With and Without COVID-19 Infection: The INTERCOVID Multinational Cohort Study. JAMA Pediatrics. 2021;175(8). Available from: https://jamanetwork.com/journals/jamapediatrics/fullarticle/2779182.
Basu A, Kim HH, Basaldua R, Choi KW, Charron L, Kelsall N, et al. A cross-national study of factors associated with women’s perinatal mental health and wellbeing during the COVID-19 pandemic. PloS one. 2021;16(4):e0249780-e.
Yue C, Liu C, Wang J, Zhang M, Wu H, Li C, et al. Association between social support and anxiety among pregnant women in the third trimester during the coronavirus disease 2019 (COVID-19) epidemic in Qingdao, China: The mediating effect of risk perception. Int J Soc psychiatry. 2020;67(2):120–7.
Vazquez-Vazquez A, Dib S, Rougeaux E, Wells JC, Fewtrell MS. The impact of the Covid-19 lockdown on the experiences and feeding practices of new mothers in the UK: Preliminary data from the COVID-19 New Mum Study. Appetite. 2021;156: 104985.
Jacob CM, Briana DD, Di Renzo GC, Modi N, Bustreo F, Conti G, et al. Building resilient societies after COVID-19: the case for investing in maternal, neonatal, and child health. The Lancet Public Health. 2020;5(11):e624–7.
Anderson E, Brigden A, Davies A, Shepherd E, Ingram J. Pregnant women’s experiences of social distancing behavioural guidelines during the Covid-19 pandemic “lockdown” in the UK, a qualitative interview study. BMC Public Health. 2021;21(1):1202.
Sanders J, Blaylock R. “Anxious and traumatised”: Users’ experiences of maternity care in the UK during the COVID-19 pandemic. Midwifery. 2021;102:103069.
Cooper M, King R. Women’s experiences of maternity care during the height of the COVID-19 pandemic in Australia. researchnowflinderseduau [Internet]. 2020 [cited 2021 Aug 30]. Available from: https://researchnow.flinders.edu.au/en/publications/womens-experiences-of-maternity-care-during-the-height-of-the-cov.
Mortazavi F, Ghardashi F. The lived experiences of pregnant women during COVID-19 pandemic: a descriptive phenomenological study. BMC Pregnancy and Childbirth. 2021;21(1):193.
Chivers BR, Garad RM, Boyle JA, Skouteris H, Teede HJ, Harrison CL. Perinatal Distress During COVID-19: Thematic Analysis of an Online Parenting Forum. J Med Internet Res. 2020;22(9): e22002.
Schaming C, Wendland J. Postnatal mental health during the COVID-19 pandemic: Impact on mothers’ postnatal sense of security and on mother-to-infant bonding. Midwifery. 2023;117: 103557.
Bradfield Z, Wynter K, Hauck Y, Vasilevski V, Kuliukas L, Wilson AN, et al. Experiences of receiving and providing maternity care during the COVID-19 pandemic in Australia: A five-cohort cross-sectional comparison. PLOS ONE. 2021;16(3): e0248488.
Vasilevski V, Sweet L, Bradfield Z, Wilson AN, Hauck Y, Kuliukas L, et al. Receiving maternity care during the COVID-19 pandemic: Experiences of women’s partners and support persons. Women and Birth. 2021;35(3).
Lalor JG, Sheaf G, Mulligan A, Ohaja M, Clive A, Murphy-Tighe S, et al. Parental experiences with changes in maternity care during the Covid-19 pandemic: A mixed-studies systematic review. Women and Birth. 2023;36(2):e203–12.
Almeida M, Shrestha AD, Stojanac D, Miller LJ. The impact of the COVID-19 pandemic on women’s mental health. Archives of Women’s Mental Health. 2020;23(6):741–8.
Flaherty SJ, Delaney H, Matvienko-Sikar K, Smith V. Maternity care during COVID-19: a qualitative evidence synthesis of women’s and maternity care providers’ views and experiences. BMC Pregnancy Childbirth. 2022;22(1):438.
Al-Mutawtah M, Campbell E, Kubis H-P, Erjavec M. Women’s experiences of social support during pregnancy: a qualitative systematic review. BMC Pregnancy and Childbirth. 2023;23(1):782.
Zheng X, Zhang J, Ye X, Lin X, Liu H, Qin Z, et al. Navigating through motherhood in pregnancy and postpartum periods during the COVID-19 pandemic: A systematic review and qualitative meta-synthesis. J Nurs Manag. 2022;30(8):3958–71.
Noyes J BA, Cargo M, Flemming K, Harden A, Harris J, Garside R, Hannes K, Pantoja T, Thomas J,. Chapter 21: Qualitative evidence. . 2022. In: Cochrane Handbook for Systematic Reviews of Interventions version 63 (updated February 2022) [Internet]. Cochrane. Available from: http://www.training.cochrane.org/handbook.
Flemming K, Noyes J. Qualitative Evidence Synthesis: Where Are We at? International Journal of Qualitative Methods. 2021;20:1609406921993276.
Popay J, Rogers A, Williams G. Rationale and Standards for the Systematic Review of Qualitative Literature in Health Services Research. Qualitative Health Research. 1998;8(3):341–51.
Flemming K, Booth A, Garside R, Tunçalp Ö, Noyes J. Qualitative evidence synthesis for complex interventions and guideline development: clarification of the purpose, designs and relevant methods. BMJ Global Health. 2019;4(Suppl 1): e000882.
Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Medical Research Methodology. 2012;12(1):181.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
World Health Organization (WHO). WHO Technical Consultation on Postpartum and Postnatal Care. Geneva: WHO; 2010.
Organisation for Economic Co-operation and Development. List of OECD Member countries - Ratification of the Convention on the OECD: OECD; 2023. Available from: https://www.oecd.org/about/document/ratification-oecd-convention.htm.
World Population Review. Human Development Index (HDI) by Country 2022-2023. Available from: https://worldpopulationreview.com/country-rankings/hdi-by-country.
Greyling T, Rossouw S, Adhikari T. The good, the bad and the ugly of lockdowns during Covid-19. PLOS ONE. 2021;16(1): e0245546.
Bu F, Steptoe A, Fancourt D. Loneliness during a strict lockdown: Trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Social Science & Medicine. 2020;265: 113521.
Coronavirus Pandemic (COVID-19). 2020 Available from: https://ourworldindata.org/coronavirus.
Covidence. Covidence. Available from: https://www.covidence.org/.
Bohren MA. Qualitative evidence synthesis & GRADE-CERQual. University of Melbourne. Cochrane Australia. 2021.
Downe S, Finlayson KW, Lawrie TA, Lewin SA, Glenton C, Rosenbaum S, et al. Qualitative Evidence Synthesis (QES) for Guidelines: Paper 1 – Using qualitative evidence synthesis to inform guideline scope and develop qualitative findings statements. Health Research Policy and Systems. 2019;17(1):76.
Benoot C, Hannes K, Bilsen J. The use of purposeful sampling in a qualitative evidence synthesis: A worked example on sexual adjustment to a cancer trajectory. BMC Medical Research Methodology. 2016;16(1):21.
Ames H, Glenton C, Lewin S. Purposive sampling in a qualitative evidence synthesis: a worked example from a synthesis on parental perceptions of vaccination communication. BMC Medical Research Methodology. 2019;19(1):26.
Critical Appraisal Skills Program. CASP Qualitative Studies Checklist. 2018. Available from: https://casp-uk.net/casp-tools-checklists/.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101.
Lumivero. NVivo (Version 13,2020), QSR International Pty Ltd; 2020. Available from: www.lumivero.com.
Atmuri K, Sarkar M, Obudu E, et al. Perspectives of pregnant women during the COVID-19 pandemic: A qualitative study. Women and Birth. 2022;35(3):280–8.
Aydin R, Aktaş S. An investigation of women’s pregnancy experiences during the COVID-19 pandemic: A qualitative study. Int J Clin Pract. 2021;75(9).
Brown A, Shenker N. Experiences of breastfeeding during COVID-19: Lessons for future practical and emotional support. Maternal & Child Nutrition. 2021;17(1): e13088.
Charvat E, Horstman HK, Jordan E, Leverenz A, Okafor B. Navigating Pregnancy during the COVID-19 Pandemic: The Role of Social Support in Communicated Narrative Sense-making. Journal of Family Communication. 2021;21(3):167–85.
Costa B, McWilliams D, Blighe S, Hudson N, Hotton M, Swan MC, et al. Isolation, Uncertainty and Treatment Delays: Parents’ Experiences of Having a Baby with Cleft Lip/Palate During the Covid-19 Pandemic. Cleft Palate Craniofac J. 2021;105566562110550.
Davis JA, Gibson LY, Bear NL, Finlay-Jones AL, Ohan JL, Silva DT, et al. Can Positive Mindsets Be Protective Against Stress and Isolation Experienced during the COVID-19 Pandemic? A Mixed Methods Approach to Understanding Emotional Health and Wellbeing Needs of Perinatal Women. Int J Environ Res Public Health. 2021;18(13):6958.
DeJoy SB, Mandel D, McFadden N, Petrecca L. Concerns of Women Choosing Community Birth During the COVID-19 Pandemic: A Qualitative Study. Journal of Midwifery & Women’s Health. 2021;66(5):624–30.
Dove-Medows E, Davis J, McCracken L, et al. A Mixed-Methods Study of Experiences During Pregnancy Among Black Women During the COVID-19 Pandemic. J Perinat Neonatal Nurs. 2022;36(2):161–72.
Farrell RM, Pierce M, Collart C, Craighead C, Coleridge M, Chien EK, et al. The impact of the emergence of COVID-19 on women's prenatal genetic testing decisions. Prenat Diagn. 2021;41(8):1009–17.
Fumagalli S, Omaghi S, Borrelli S, et al. The experiences of childbearing women who tested positive to COVID-19 during the pandemic in northern Italy. Women and Birth. 2022;35(3):242–53.
Green SM, Furtado M, Inness BE, Frey BN, McCabe RE. Characterizing Worry Content and Impact in Pregnant and Postpartum Women with Anxiety Disorders During COVID-19. Clin Psychol Psychother. 2022;29(3):1144–57.
Harrison S, Alderdice F, McLeish J, et al. You and your baby: a national survey of health and care during the 2020 Covid-19 pandemic. Oxford: National Perinatal Epidemiology Unit, University of Oxford; 2021.
Jackson L, De Pascalis L, Harrold JA, Fallon V, Silverio SA. Postpartum women's experiences of social and healthcare professional support during the COVID-19 pandemic: A recurrent cross-sectional thematic analysis. Women and Birth. 2022;35(5):511–20.
Jackson L, De Pascalis L, Harrold JA, Fallon V, Silverio SA. Postpartum women’s psychological experiences during the COVID-19 pandemic: a modified recurrent cross-sectional thematic analysis. BMC Pregnancy and Childbirth. 2021;21(1):625.
John JR, Curry G, Cunningham-Burley S. Exploring ethnic minority women’s experiences of maternity care during the SARS-CoV-2 pandemic: a qualitative study. BMJ Open. 2021;11(9): e050666.
Joy P, Aston M, Price S, Sim M, Ollivier R, Benoit B, et al. Blessings and Curses: Exploring the Experiences of New Mothers during the COVID-19 Pandemic. Nursing Reports. 2020;10(2):207–19.
Keating NE, Dempsey B, Corcoran S, McAuliffe FM, Lalor J, Higgins MF. Women’s experience of pregnancy and birth during the COVID-19 pandemic: a qualitative study. Ir J Med Sci. 2022;191(5):2177–84.
Kolker S, Biringer A, Bytautas J, Blumenfeld H, Kukan S, Carroll JC. Pregnant during the COVID-19 pandemic: an exploration of patients’ lived experiences. BMC Pregnancy and Childbirth. 2021;21(1):851.
Kynø NM, Fugelseth D, Knudsen LMM, Tandberg BS. Starting parenting in isolation a qualitative user-initiated study of parents’ experiences with hospitalization in Neonatal Intensive Care units during the COVID-19 pandemic. PloS one. 2021;16(10): e0258358.
Linden K, Domgren N, Zaigham M, Sengpiel V, Andersson ME, Wessberg A. Being in the shadow of the unknown — Swedish women's lived experiences of pregnancy during the COVID-19 pandemic, a phenomenological study. Women and Birth. 2022;35(5):440–6.
Mizrak Sahin B, Kabakci EN. The experiences of pregnant women during the COVID-19 pandemic in Turkey: A qualitative study. Women and birth. 2021;34(2):162–9.
Ollivier R, Aston DM, Price DS, Sim DM, Benoit DB, Joy DP, et al. Mental Health & Parental Concerns during COVID-19: The Experiences of New Mothers Amidst Social Isolation. Midwifery. 2021;94: 102902.
Panda S, O’Malley D, Barry P, Vallejo N, Smith V. Women’s views and experiences of maternity care during COVID-19 in Ireland: A qualitative descriptive study. Midwifery. 2021;103: 103092.
Rhodes A, Kheireddine S, Smith AD. Experiences, Attitudes, and Needs of Users of a Pregnancy and Parenting App (Baby Buddy) During the COVID-19 Pandemic: Mixed Methods Study. JMIR mHealth and uHealth. 2020;8(12): e23157.
Rice K, Williams S. Women’s postpartum experiences in Canada during the COVID-19 pandemic: a qualitative study. CMAJ Open. 2021;9(2):E556–62.
Rice K, Williams S. Making good care essential: The impact of increased obstetric interventions and decreased services during the COVID-19 pandemic. Women and Birth. 2022;35(5):484–92.
Riley V, Ellis N, Mackay L, Taylor J. The impact of COVID-19 restrictions on women’s pregnancy and postpartum experience in England: A qualitative exploration. Midwifery. 2021;101: 103061.
Saleh L, Canclini S, Greer K, Mathison C, Combs SM, Dickerson B, et al. Mothers’ Experiences of Pregnancy, Labor and Birth, and Postpartum During COVID-19 in the United States: Preliminary Results of a Mixed-Methods Study. The Journal of Perinatal & Neonatal Nursing. 2022;36(1):55–67.
Silverio SA, De Backer K, Easter A, von Dadelszen P, Magee LA, Sandall J. Women’s experiences of maternity service reconfiguration during the COVID-19 pandemic: A qualitative investigation. Midwifery. 2021;102: 103116.
Snyder K, Worlton G. Social Support During COVID-19: Perspectives of Breastfeeding Mothers. Breastfeed Med. 2021;16(1):39–45.
Spatz DL, Froh EB. Birth and Breastfeeding in the Hospital Setting during the COVID-19 Pandemic. MCN The American Journal of Maternal Child Nursing. 2021;46(1):30–5.
Stirling Cameron E, Ramos H, Aston M, Kuri M, Jackson L. “COVID affected us all:” the birth and postnatal health experiences of resettled Syrian refugee women during COVID-19 in Canada. Reproductive Health. 2021;18(1):256.
Sweet L, Bradfield Z, Vasilevski V, Wynter K, Hauck Y, Kuliukas L, et al. Becoming a mother in the ‘new’ social world in Australia during the first wave of the COVID-19 pandemic. Midwifery. 2021;98: 102996.
Sweet L, Wilson AN, Bradfield Z, Hauck Y, Kuliukas L, Homer CSE, et al. Childbearing women’s experiences of the maternity care system in Australia during the first wave of the COVID-19 pandemic. Women and Birth. 2022;35(3):223–31.
Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implementation Science. 2018;13(1):2.
iSoQ: Grade-CERqual [Internet]. 2023 [cited 2022]. Available from: https://www.cerqual.org/isoq/.
Ataman H, Tuncer M. The effect of COVID-19 fear on prenatal distress and childbirth preference in primipara. Rev Assoc Med Bras. 2023;69(5):e20221302.
Preis H, Mahaffey B, Heiselman C, Lobel M. Vulnerability and resilience to pandemic-related stress among US women pregnant at the start of the COVID-19 pandemic. Social science & medicine. 2020;266: 113348.
Boekhorst MG, Muskens L, Hulsbosch LP, Van Deun K, Bergink V, Pop VJ, et al. The COVID-19 outbreak increases maternal stress during pregnancy, but not the risk for postpartum depression. Arch Womens Ment Health. 2021;24(6):1037–43.
Reingold RB, Barbosa I, Mishori R. Respectful maternity care in the context of COVID-19: A human rights perspective. Int J Gynaecol Obstet. 2020;151(3):319–21.
Tunçalp Ӧ, Pena-Rosas JP, Lawrie T, Bucagu M, Oladapo OT, Portela A, Metin Gülmezoglu A. WHO recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG. 2017;124(6):860–2.
World Heath Organization (WHO) Standards for improving quality of maternal and newborn care in health facilities [Internet]. Available from: https://www.who.int/publications-detail-redirect/9789241511216.
Khaw SML, Homer CSE, Dearnley RE, O’Rourke K, Akter S, Bohren MA. A qualitative study on community-based doulas’ roles in providing culturally-responsive care to migrant women in Australia. Women and Birth. 2023;36(5):e527–35.
Essén B, Eriksson L. Paradoxes in the cultural doula concept for migrant women: Implications for gender-inclusive care versus migrant-friendly maternity care. Midwifery. 2023;126: 103805.
Asefa A. Unveiling respectful maternity care as a way to address global inequities in maternal health. BMJ Glob Health. 2021;6(1):e003559.
Murray K, Nebeker C, Carpendale E. Responsibilities for ensuring inclusion and representation in research: A systems perspective to advance ethical practices. Australian & New Zealand Journal of Psychiatry. 2019;53(9):835–8.
Rini C, Schetter CD, Hobel CJ, Glynn LM, Sandman CA. Effective social support: Antecedents and consequences of partner support during pregnancy. Personal Relationships. 2006;13(2):207–29.
Racine N, Plamondon A, Hentges R, Tough S, Madigan S. Dynamic and bidirectional associations between maternal stress, anxiety, and social support: The critical role of partner and family support. Journal of Affective Disorders. 2019;252:19–24.
Kroelinger CD, Oths KS. Partner Support and Pregnancy Wantedness. Birth. 2000;27(2):112–9.
Wells MB, Svahn J, Svedlind K, Andersson E. A qualitative study of Swedish fathers’ experiences of becoming a father during the COVID-19 pandemic. Eur J Midwifery. 2022;6:15.
Lista G, Bresesti I. Fatherhood during the COVID-19 pandemic: an unexpected turnaround. Early Hum Dev. 2020;144: 105048.
Menzel A. The coronavirus pandemic: exploring expectant fathers’ experiences. Journal for Cultural Research. 2022;26(1):83–101.
Digby R, Manias E, Haines KJ, Orosz J, Ihle J, Bucknall TK. Family experiences and perceptions of intensive care unit care and communication during the COVID-19 pandemic. Australian Critical Care. 2023;36(3):350–60.
Roberto A, Sellon A, Cherry ST, Hunter-Jones J, Winslow H. Impact of spirituality on resilience and coping during the COVID-19 crisis: A mixed-method approach investigating the impact on women. Health Care Women Int. 2020;41(11–12):1313–34.
Kinser PA, Jallo N, Amstadter AB, Thacker LR, Jones E, Moyer S, et al. Depression, Anxiety, Resilience, and Coping: The Experience of Pregnant and New Mothers During the First Few Months of the COVID-19 Pandemic. Journal of Women’s Health. 2021;30(5):654–64.
Barbosa-Leiker C, Smith CL, Crespi EJ, Brooks O, Burduli E, Ranjo S, et al. Stressors, coping, and resources needed during the COVID-19 pandemic in a sample of perinatal women. BMC Pregnancy and Childbirth. 2021;21(1):171.
Hui L, Marzan MB, Potenza S, Rolnik DL, Pritchard N, Said JM, et al. Increase in preterm stillbirths in association with reduction in iatrogenic preterm births during COVID-19 lockdown in Australia: a multicenter cohort study. Am J Obstet Gynecol. 2022;227(3):491.e1–17.
De Mario C, Leonardo V, Arianna P. Increase of stillbirth and decrease of late preterm infants during the COVID-19 pandemic lockdown. Arch Dis Child Fetal Neonatal Ed. 2021;106(4):456.
Calvert C, Brockway M, Zoega H, Miller JE, Been JV, Amegah AK, et al. Changes in preterm birth and stillbirth during COVID-19 lockdowns in 26 countries. Nature Human Behaviour. 2023;7(4):529–44.
Fahy K. What is woman-centred care and why does it matter? Women and Birth. 2012;25(4):149–51.
Leap N. Woman-centred or women-centred care: does it matter? British Journal of Midwifery. 2009;17(1):12–6.
Watkins V, Nagle C, Kent B, Street M, Hutchinson AM. Labouring Together: Women’s experiences of “Getting the care that I want and need” in maternity care. Midwifery. 2022;113: 103420.
Macpherson I, Roqué-Sánchez MV, Legget BNFO, Fuertes F, Segarra I. A systematic review of the relationship factor between women and health professionals within the multivariant analysis of maternal satisfaction. Midwifery. 2016;41:68–78.
Vermeulen J, Bilsen J, Buyl R, De Smedt D, Gucciardo L, Faron G, et al. Women’s experiences with being pregnant and becoming a new mother during the COVID-19 pandemic. Sex Reprod Healthc. 2022;32: 100728.
Homer CSE. Models of maternity care: evidence for midwifery continuity of care. Medical Journal of Australia. 2016;205(8):370–4.
Davison C. Woman-centred care. British Journal of Midwifery. 2021;29(5):246–8.
Acknowledgments
Not applicable.
Funding
The primary author is funded by Deakin University Postgraduate Research Scholarship as a PhD Candidate. AB is supported by the Australian Government Research Training Program, CSEH is supported by the Australian National Health and Medical Research Council Leadership Investigator Grant, and JPV is supported by the Australian National Health and Medical Research Council Emerging Leadership Investigator Grant. The funding bodies had no role in the conceptualisation of the study design and data collection, data analysis, interpretation and writing of the manuscript.
Author information
Authors and Affiliations
Contributions
AT: Conceptualisation, Methodology, Data Collection, Formal Analysis, Writing – Original Draft. AB: Secondary Reviewer, Data Collection, Formal Analysis, Writing – Reviewing and Editing. RD: Supervision, Data Analysis, Writing – Reviewing and Editing. JPV: Supervision, Data Analysis, Writing – Reviewing and Editing. CSEH: Supervision, Data Analysis, Writing – Reviewing and Editing. TB: Primary Supervision, Methodology, Data Analysis, Writing – Reviewing and Editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All data included are publicly available and therefore did not require ethical approval.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tan, A., Blair, A., Homer, C.S. et al. Pregnant and postpartum women’s experiences of the indirect impacts of the COVID-19 pandemic in high-income countries: a qualitative evidence synthesis. BMC Pregnancy Childbirth 24, 262 (2024). https://doi.org/10.1186/s12884-024-06439-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06439-6