Abstract
Purpose
The purpose of this study was to investigate the risk factors for umbilical artery thrombosis (UAT) and the relationship between umbilical artery thrombosis and perinatal outcomes.
Methods
This was a retrospective study that enrolled singleton pregnant women who were diagnosed with umbilical artery thrombosis. The control group recruited pregnant woman with three umbilical vessels or those with isolated single umbilical artery (iSUA) who were matched with umbilical artery thrombosis group. The risk factors and perinatal outcomes were compared between the groups.
Results
Preconception BMI (OR [95%CI]: 1.212 [1.038–1.416]), abnormal umbilical cord insertion (OR [95%CI]: 16.695 [1.333-209.177]) and thrombophilia (OR [95%CI]: 15.840 [1.112-223.699]) were statistically significant risk factors for umbilical artery thrombosis. An elongated prothrombin time (OR [95%CI]: 2.069[1.091–3.924]) was strongly associated with the occurrence of UAT. The risks of cesarean delivery, preterm birth, fetal growth restriction, neonatal asphyxia, and intraamniotic infection were higher in pregnancies with UAT than in pregnancies with three umbilical vessels or isolated single umbilical artery (P<0.05). Additionally, the incidence of thrombophilia was higher in pregnant women with umbilical artery thrombosis than those with isolated single umbilical artery (P = 0.032). Abnormal umbilical cord insertion was also found to be associated with an elevated risk of iSUA (OR [95%CI]: 15.043[1.750-129.334]).
Conclusions
Abnormal umbilical cord insertion was the risk factor for both umbilical artery thrombosis and isolated single umbilical artery. The pregnancies with umbilical artery thrombosis had a higher risk of the adverse perinatal outcomes.
Similar content being viewed by others
What is known
-
Umbilical artery thrombosis was a rare pregnancy complication, and due to its low incidence, the majority of relevant literature consisted of case reports.
-
The diagnosis of Umbilical artery thrombosis could only be confirmed through postpartum umbilical cord pathological examination, as the ultrasound findings typically revealed the presence of only one umbilical artery during pregnancy.
What is New
-
The risk factors for umbilical artery thrombosis included preconception BMI, abnormal umbilical cord insertion and thrombophilia.
-
Abnormal umbilical cord insertion was the risk factor for both umbilical artery thrombosis and isolated single umbilical artery.
-
Pregnant women with umbilical artery thrombosis were at an increased risk of adverse perinatal outcomes such as fetal growth restriction and preterm birth.
Induction
The umbilical cord, serving as the link between mother and fetus, normally contains two arteries and one vein. In 0.5-2.0% of pregnancies [1, 2], one of the umbilical arteries may not develop or regresses progressively. The condition characterized by absence of one of the umbilical arteries is referred to as single umbilical artery (SUA). The most widely accepted underlying explanations for the causes of SUA include the primary agenesis, later atrophy of one umbilical artery or persistence of the original single allantoic artery of the body stalk [3]. Structural and chromosomal anomalies are considered to be closely related to the occurrence of SUA. It had been reported that approximately 33% of fetuses with SUA have additional structural anomalies, and 10% are affected with aneuploidy [4,5,6,7], implying that SUA severs as a soft marker for adverse pregnant outcomes. However, approximately 65% of cases with SUA are an isolated finding without fetal malformations or chromosomal abnormalities, which are referred to as isolated single umbilical artery (iSUA) [7].
Umbilical artery thrombosis (UAT) is a rare complication of pregnancy strongly associated with poor fetal and perinatal outcomes, such as intrauterine asphyxia, fetal growth restriction, and stillbirth [8,9,10]. UAT is considered to be a special type of single umbilical artery, since the ultrasound manifestation of UAT is the presence of only one umbilical artery during pregnancy and most pregnancies with UAT have no specific clinical symptoms or signs [8]. The diagnosis of UAT can only be confirmed by pathological examination of umbilical cord after delivery. Previous studies have shown an incidence of UAT between 0.025% and 0.045% [8, 9]. However, the scarcity of research on UAT is mainly attributed to the low incidence rate of UAT and the predominance of case report-based literature, which limits further investigation in the field.
Furthermore, many risk factors have been reported to be associated with the occurrence of SUA in pregnant women, including sex, multiple births, ethnicity, older maternal age, multiparity, and smoking, as well as the presence of maternal medical and pregnancy complications, maternal drug use [11,12,13]. However, it is worth noting that the existing literature lacks comprehensive reports that specifically investigate the precise risk factors of UAT.
Therefore, the purpose of this study was to investigate the risk factors for UAT, as well as the relationship between UAT and perinatal outcomes, which identify high-risk pregnancies with UAT earlier and provide evidence for perinatal health care of women with abnormal umbilical artery detected by ultrasound during pregnancy, thereby reducing the potential complications.
Methods
Study design
This was an observational retrospective study performed in four hospitals from January 1, 2016 to December 31, 2022. All pregnant women with umbilical artery thrombosis (UAT) identified during the study period were included as cases, while the pregnant women with isolated single umbilical artery (iSUA) or the pregnant women with three umbilical vessels during the same period were included as two distinct control group. All participants were between 20 and 45 years old and had singleton pregnancies conceived naturally. Exclusion criteria were women with twin pregnancies, fetal malformation, fetal chromosome aneuploidy, genetic abnormalities, assisted reproductive techniques or with incomplete medical histories and laboratory data. The Research Ethics Committees of the four participating hospitals approved this study.
Diagnosis of UAT and iSUA
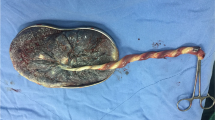
Umbilical artery thrombosis (UAT) was diagnosed when Ultrasonography revealed the presence of only one visible umbilical artery, whereas previous ultrasounds had indicated bilateral umbilical arteries. Additionally, the ultrasound identified a suspicious intraluminal low-echogenic substance within the umbilical artery, leading to the diagnosis of umbilical artery thrombosis. Subsequent pathological examination of the umbilical cord post-delivery confirmed the presence of umbilical artery thrombosis [14] (Fig. 1).
An isolated single umbilical artery (iSUA) was diagnosed at the time that during fetal anatomical scanning, the transverse section of the fetal pelvis revealed the presence of only a single umbilical artery encircling the fetal bladder, and color Doppler ultrasound confirmed the existence of a single umbilical artery without any fetal malformations or chromosomal abnormalities. Subsequent pathological examination of the umbilical cord post-delivery confirmed the presence of a single umbilical artery [15] (Fig. 2). All ultrasound examinations were carried out transabdominally by experienced operators using uniform high-resolution ultrasound equipment.
Data collection
We conducted a review of computerized medical records for enrolled pregnant women to gather information on baseline maternal characteristics and associated perinatal complications, including maternal age, gravidity, parity, preconception body mass index (BMI), abnormal umbilical cord insertion (including velamentous cord insertion and marginal cord insertion), thrombophilia (a condition resulting from postnatal or genetically inherited factors causing blood abnormalities), meconium-stained amniotic fluid (characterized by green or yellowish appearance, indicating the presence of meconium), gestational diabetes mellitus (GDM, defined as fasting plasma glucose (FPG) ≥ 5.1 mmol/L, or 1-hour plasma glucose ≥ 10.0 mmol/L, or 2-hour plasma glucose ≥ 8.5 mmol/L at 24–28 weeks of gestation), and hypertensive disorders of pregnancy (HDP, including gestational hypertension defined as systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg after 20 gestational weeks, and preeclampsia defined as hypertension after 20 gestational weeks with proteinuria, uteroplacental dysfunction, or organ damage; this group also includes women with conditions related to HDP, such as the HELLP syndrome) [16]. We also reviewed the coagulation profile in pregnant women at admission, including D-dimer, blood platelet count, prothrombin time (PT), activated partial thromboplastin time (APTT), and fibrinogen.
Perinatal outcomes included the rate of cesarean delivery, gestational age at delivery, preterm birth (defined as gestational age ≥ 28 weeks and < 37 weeks (196–258 days)), stillbirth, placental weight, fetal weight, fetal growth restriction (FGR, defined as birth weight less than the 10th percentile), macrosomia (defined as birth weight ≥ 4000 g), oligohydramnios (defined as amniotic fluid volume ≤ 300 ml, or the vertical depth of the maximum dark area of amniotic fluid under ultrasound was ≤ 2 cm or the amniotic fluid index was ≤ 5 cm in the third trimester of pregnancy), polyhydramnios (defined as amniotic fluid volume > 2000 ml), neonatal asphyxia (defined as low Apgar score or abnormal umbilical cord blood gas analysis or both), Apgar score at 1 min (based on heart rate, respiration, muscle tone, laryngeal reflex, and skin color within one minute after birth), Apgar score at 5 min (based on heart rate, respiration, muscle tone, laryngeal reflex, and skin color within five minutes after birth), intraamniotic infection (IAI, defined by standard clinical criteria, including maternal fever (≥ 38.0 °C) and at least one symptom such as maternal tachycardia > 100 bpm, fetal tachycardia > 160 bpm, uterine tenderness, maternal leukocytosis > 15,000 cells/mm3, and/or foul odor of the amniotic fluid) [16]. Additionally, we reviewed placentae and gestational membranes for histologic evidence of infection by postpartum pathology.
Statistical analysis
Data were analyzed using SPSS 26.0 software (SPSS, Chicago, IL, USA). Normally distributed variables were presented as mean ± standard deviation and were analyzed by Student’s t test or one-way ANOVA. Nonnormally distributed variables were expressed as median and interquartile range and were analyzed by Mann-Whitney U test. Categorical variables were presented as number (%) and were analyzed by Pearson’s Chi-square test. Each variable was initially evaluated by univariate analysis including the chi-square test or one-way ANOVA. To identify risk factors for iSUA and UAT, multivariable logistic regression analysis was performed with a backward stepwise method for variables with P value < 0.2 in univariate analyses. Odds ratios (OR) and 95% confidence intervals (CI) were calculated. A power analysis with multiple regression model demonstrated that this study had a power of 95% in variable at significant level of 0.05. P value < 0.05 for multivariate regression analysis and perinatal outcomes was considered to be statistically significant.
Results
A total of 46 pregnant women with umbilical artery thrombosis were identified during the study period, as well as 100 pregnant women with isolated single umbilical artery and 95 pregnant women with three umbilical vessels were selected as control group during the same period. The median gestational age at which umbilical artery thrombosis was detected in pregnancies was 29.71 weeks, with a quartile range of 22.96 to 34.29 weeks.
Risk factors associated with UAT
As shown in Table 1, the proportions of abnormal cord insertion and thrombophilia were significantly higher in the UAT group compared to the three umbilical vessels group (P < 0.05). But there were no significant differences in maternal age, gravidity, parity, preconception BMI, GDM and HDP (P > 0.05). Table 2 showed the association between the coagulation profile and UAT. Blood platelet count, PT and fibrinogen in the UAT group were higher than those in three umbilical vessels group (P < 0.05). D-dimer and APTT were no different between the groups (P > 0.05).
Univariate analysis identified preconception BMI, abnormal umbilical cord insertion, thrombophilia, blood platelet count, PT, and fibrinogen as significant predictors for subsequent multiple logistic regression analysis (P < 0.2) (Tables 1 and 2). The multiple logistic regression analysis showed that preconception BMI (OR [95%CI]: 1.212 [1.038–1.416], P = 0.015), abnormal umbilical cord insertion (OR [95%CI]: 16.695 [1.333-209.177], P = 0.029), thrombophilia (OR [95%CI]: 15.840 [1.112-223.699], P = 0.041) and PT (OR [95%CI]: 2.069 [1.091–3.924], P = 0.026) were statistically significant risk factors for UAT (Table 3).
Maternal characteristics and coagulation profile were compared between the iSUA and UAT populations in Tables 1 and 2. The results showed that the incidence of thrombophilia was higher in UAT group compared to iSUA group (P = 0.032). There were no significant differences in maternal age, gravidity, parity, preconception BMI, abnormal umbilical cord insertion, thrombophilia, GDM, HDP, D-dimer, platelet count, PT, APTT, and fibrinogen between iSUA and UAT groups (P > 0.05).
Risk factors associated with iSUA
As shown in Table 1, compared to pregnancies with three umbilical vessels, the incidence of abnormal cord insertion was increased in iSUA group (P = 0.006), but there was no difference in maternal age, gravidity, parity, preconception BMI, thrombophilia, GDM and HDP between two groups (P > 0.05). As shown in Table 2, a comparative analysis of the coagulation profile was conducted between the iSUA group and three umbilical vessels group. PT and APTT of pregnant women at admission were higher in iSUA group than three umbilical vessels group (P < 0.05), while D-dimer, blood platelet count and fibrinogen were no difference between the groups (P > 0.05).
Univariate analysis identified abnormal cord insertion, HDP, blood platelet count, PT, APTT and fibrinogen as significant predictors for subsequent multiple logistic regression analysis (P < 0.2) (Tables 1 and 2). The multiple logistic regression analysis showed that abnormal umbilical cord insertion (OR [95%CI]: 15.043 [1.750-129.334], P = 0.014) were statistically significant risk factors for iSUA (Table 4).
Perinatal outcomes of pregnancies with UAT
Perinatal outcomes of pregnancies with UAT were reviewed and analyzed (Table 5). Compared with pregnancies with three umbilical vessels, pregnancies with UAT had a higher risk of cesarean delivery, preterm birth, oligohydramnios and IAI, and a lower weight of placenta and gestational age at delivery, and a greater likelihood of FGR as well as neonatal asphyxia in their newborns (P < 0.05). Compared with pregnancies with iSUA, pregnancies with UAT had a higher risk of cesarean delivery, preterm birth and IAI, and a lower weight of placenta and gestational age at delivery, and a greater likelihood of FGR and neonatal asphyxia in their newborns (P < 0.05). In addition, one stillbirth had occurred in the UAT group during the study period.
Association of iSUA with perinatal outcomes
Perinatal outcomes of pregnancies with iSUA were reviewed and analyzed (Table 5). The risks of FGR and IAI were higher and the gestational age at delivery was lower in the iSUA group than in the three umbilical vessels group (P < 0.05), but there was no statistically significant difference in cesarean section, premature delivery, stillbirth, placental weight, macrosomia, oligohydramnios, meconium-stained amniotic fluid and neonatal asphyxia (P > 0.05).
Discussion
This study demonstrated that preconception BMI, abnormal umbilical cord insertion, and thrombophilia were identified as risk factors for UAT, and an elongated prothrombin time (PT) was strongly associated with the occurrence of UAT. The risks of cesarean delivery, preterm birth, FGR, neonatal asphyxia, and IAI were higher in pregnancies with UAT than in pregnancies with three umbilical vessels or iSUA. Additionally, abnormal umbilical cord insertion was found to be associated with an elevated risk of iSUA, as well as an increased likelihood of FGR and IAI in pregnancies with iSUA compared to those with three umbilical cord vessels.
In this study, abnormal umbilical cord insertion, including velamentous and marginal cord insertions, was found to be a prevalent risk factor for both iSUA and UAT. The presence of abnormal placental umbilical cord insertion in pregnant women with UAT has been consistently reported by the majority of previous investigators. The abnormal insertion of the umbilical cord indeed has the potential to disrupt normal blood flow and increase the risk of thrombosis, both of which are considered potential causes of UAT [17]. Therefore, it is crucial to closely monitor pregnant women with abnormal umbilical cord insertion in order to promptly detect umbilical artery thrombosis.
Obesity stands as an independent risk factor for both arterial and venous thrombosis [18]. The mothers who are overweight prior to pregnancy were more prone to experiencing postpartum venous thrombosis [19]. The results of our study have also indicated that an elevated preconception BMI serves as a significant risk factor for UAT. Consequently, it suggests that pregnant women with an elevated preconception BMI face an increased susceptibility to UAT.
Our results indicated that thrombophilia was a risk factor for UAT. A case of inherited thrombophilia who developed UAT was reported [20]. During the pregnancy, a series of physiological alterations induce a hypercoagulable environment, which is deemed to be protective. However, the presence of inherited or acquired thrombophilia during gestation can disturb this intricate equilibrium, leading to an augmented inclination towards unwarranted thrombotic occurrences [21]. Therefore, it is imperative for expectant women with thrombophilia to exercise heightened vigilance regarding the potential risk of UAT.
An elongated PT may indicate abnormalities in certain factors within the coagulation system, which could increase the patient’s risk of thrombosis [22]. In this study, we observed a significant association between the prolongation of PT and the occurrence of UAT. Given the retrospective design of our study and the limitation of collecting PT measurements only at the time of admission, we were unable to establish a definitive causal relationship between PT prolongation and UAT. On the one hand, the elongation of PT in pregnant women may potentially indicate abnormalities in the coagulation system, which could increase the risk of UAT. On the other hand, it is also possible that the formation of UAT itself leads to PT prolongation. Nevertheless, the precise causal relationship between PT prolongation and UAT in pregnant women remains largely unexplored within the existing body of research. Further researches are needed to comprehensively investigate the potential causal relationship between PT and UAT, including examining the impact of PT values at different stages of pregnancy on the risk of UAT occurrence in pregnant women.
Diabetes and HDP are both conditions that can lead to endothelial injury, heightened inflammatory response, and platelet deposition on the vascular walls, thereby promoting thrombus formation. The presence of diabetes can also result in compromised blood flow within the small vessels and microcirculatory dysfunction. This, in turn, contributes to the development of thrombosis [23]. Thus, GDM and HDP may be independent risk factors for UAT [8, 24]. However, our study did not find a significant association between UAT and either HDP or GDM. This contradictory result may be attributed to differences in study design, study populations, and the severity of diabetes or hypertension. For instance, a considerable proportion of pregnant women with diabetes or HDP in this study exhibited well-controlled blood glucose or blood pressure level. Indeed, the precise timing of occurrence of UAT in relation to the onset of GDM and HDP in this study remains elusive due to the potential for ultrasound detection to indicate pre-existing thrombi.
Our study supported the existing literature regarding the association between iSUA and adverse pregnancy outcomes such as FGR and preterm birth [2, 25, 26]. Furthermore, we found that pregnancies with UAT had a higher risk of adverse perinatal outcomes, including cesarean delivery, FGR, preterm birth, neonatal asphyxia, stillbirth, and IAI compared to pregnancies with iSUA. These results indicate that UAT pregnancies are more susceptible to experiencing adverse perinatal outcomes than iSUA pregnancies, despite both populations presenting with a single umbilical artery on ultrasound examination and the absence of specific clinical symptoms or signs. Therefore, UAT poses a greater risk compared to iSUA, highlighting the importance of timely detection and early intervention in UAT pregnancies.
The umbilical blood vessels play a crucial role in transporting oxygen and essential substances to the fetus. The formation of a thrombus in the umbilical artery can result in reduced oxygen supply to the placental vessels, leading to a state of hypoxia [27]. This hypoxic condition can cause swelling of the intima, endothelial necrosis, and ultimately result in the occlusion of stem villi vessels and abnormal peripheral placental villi [27]. Many adverse pregnancy outcomes, such as FGR, preterm birth, neonatal asphyxia and stillbirth, can be attributed to abnormalities in placental trophoblast cells and placental dysfunction [28, 29]. This was why UAT was associated with adverse perinatal outcomes such as cesarean section, fetal growth restriction (FGR), preterm birth, neonatal asphyxia, and stillbirth [9, 10, 17, 27], which was consistent with our findings.
It is interesting to note that we observed a significant increase in the incidence of IAI and oligohydramnios in the UAT group, which has not been reported in other relevant studies. This may be that the impaired placental circulation caused by UAT could disrupt the normal exchange of nutrients and waste products between the mother and fetus, creating an environment conducive to infection or inadequate amniotic fluid production [30, 31]. Therefore, pregnant women who have UAT should be alert to the potential risks of oligohydramnios and IAI.
One of the strengths of this study is the inclusion of two control groups, allowing for comparisons of pregnant women with UAT to both the population with a normal three umbilical vessels and the population with iSUA. Additionally, our study was conducted as a multicenter study, which enhances the generalizability of the findings. However, it is important to acknowledge that our study was limited by its retrospective design. Therefore, to address this limitation, future research will focus on conducting prospective studies to further investigate the pregnancies with UAT.
Conclusions
In conclusion, abnormal umbilical cord insertion serves as a common risk factor for both pregnancies with UAT and those with iSUA. Compared to pregnancies with iSUA or three-vessel umbilical cord, UAT pregnancies are associated with a higher risk of adverse perinatal outcomes.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- APTT:
-
Activated partial thromboplastin time
- BMI:
-
Body mass index
- CI:
-
Confidence intervals
- FGR:
-
Fetal growth restriction
- FPG:
-
Fasting plasma glucose
- GDM:
-
Gestational diabetes mellitus
- HDP:
-
Hypertensive disorders of pregnancy
- IAI:
-
Intraamniotic infection
- iSUA:
-
Isolated single umbilical artery
- OR:
-
Odds ratios
- PT:
-
Prothrombin time
- SUA:
-
Single umbilical artery
- UAT:
-
Umbilical artery thrombosis
References
Hua M, Odibo AO, Macones GA, Roehl KA, Crane JP, Cahill AG. (2010)Single umbilical artery and its associated findings. Obstet Gynecol 115 (5), 930-934.10.1097/AOG.0b013e3181da50ed.
Contro E, Larcher L, Lenzi J, Valeriani M, Farina A, Jauniaux E. Changes in artery diameters and fetal growth in cases of isolated single umbilical artery. Diagnostics (Basel Switzerland). 2023;13(3). https://doi.org/10.3390/diagnostics13030571.
Vafaei H, Rafeei K, Dalili M, Asadi N, Seirfar N, Akbarzadeh-Jahromi M. Prevalence of single umbilical artery, clinical outcomes and its risk factors: a cross-sectional study. Int J Reproductive Biomed. 2021;19(5):441–8. https://doi.org/10.18502/ijrm.v19i5.9253.
Ebbing C, Kessler J, Moster D, Rasmussen S. Single umbilical artery and risk of congenital malformation: population-based study in Norway. Ultrasound Obstet Gynecol. 2020;55(4):510–5. https://doi.org/10.1002/uog.20359.
Soma H. Messages from the placentae across multiple species: a 50 years exploration. Placenta. 2019;84:14–27. https://doi.org/10.1016/j.placenta.2019.06.376.
Granese R, Coco C, Jeanty P. The value of single umbilical artery in the prediction of fetal aneuploidy: findings in 12,672 pregnant women. Ultrasound Q. 2007;23(2):117–21. https://doi.org/10.1097/01.ruq.0000263848.07808.02.
Voskamp BJ, Fleurke-Rozema H, Oude-Rengerink K, Snijders RJ, Bilardo CM, Mol BW, Pajkrt E. (2013)Relationship of isolated single umbilical artery to fetal growth, aneuploidy and perinatal mortality: systematic review and meta-analysis. Ultrasound Obstet Gynecol 42 (6), 622 – 8.10.1002/uog.12541.
Wu X, Wei C, Chen R, Yang L, Huang W, Huang L, Yan X, Deng X, Gou Z. Fetal umbilical artery thrombosis: prenatal diagnosis, treatment and follow-up. Orphanet J Rare Dis. 2022;17(1):414. https://doi.org/10.1186/s13023-022-02563-8.
Sato Y, Benirschke K. Umbilical arterial thrombosis with vascular wall necrosis: clinicopathologic findings of 11 cases. Placenta. 2006;27(6–7):715–8. https://doi.org/10.1016/j.placenta.2005.05.008.
Li H, Qufeng W, Wei W, Lin X, Zhang X. (2019)Umbilical artery thrombosis: Two case reports. Medicine (Baltimore) 98 (48), e18170.10.1097/md.0000000000018170.
Leung AK, Robson WL. Single umbilical artery. A report of 159 cases. Am J Dis Child (1960). 1989;143(1):108–11. https://doi.org/10.1001/archpedi.1989.02150130118030.
Lilja M. Infants with single umbilical artery studied in a national registry. 3: a case control study of risk factors. Paediatr Perinat Epidemiol. 1994;8(3):325–33. https://doi.org/10.1111/j.1365-3016.1994.tb00466.x.
Murphy-Kaulbeck L, Dodds L, Joseph KS, Van den Hof M. (2010)Single umbilical artery risk factors and pregnancy outcomes. Obstet Gynecol 116 (4), 843-850.10.1097/AOG.0b013e3181f0bc08.
Ebbing C, Rasmussen S, Kessler J, Moster D. Association of placental and umbilical cord characteristics with cerebral palsy: national cohort study. Ultrasound Obstet Gynecol. 2023;61(2):224–30. https://doi.org/10.1002/uog.26047.
Li TG, Guan CL, Wang J, Peng MJ. Comparative study of umbilical cord cross-sectional area in foetuses with isolated single umbilical artery and normal umbilical artery. J Obstet Gynaecol. 2022;42(5):935–40. https://doi.org/10.1080/01443615.2021.1962818.
Pan S, Lan Y, Zhou Y, Chen B, Zhou F, Dai D, Hua Y. Associations between the size and duration of asymptomatic subchorionic hematoma and pregnancy outcomes in women with singleton pregnancies. BMC Pregnancy Childbirth. 2023;23(1):555. https://doi.org/10.1186/s12884-023-05831-y.
Tanaka K, Tanigaki S, Matsushima M, Miyazaki N, Hashimoto R, Izawa T, Sakai K, Yazawa T, Iwashita M. Prenatal diagnosis of umbilical artery thrombosis. Fetal Diagn Ther. 2014;35(2):148–50. https://doi.org/10.1159/000355601.
Pettigrew R, Hamilton-Fairley D. Obesity and female reproductive function. Br Med Bull. 1997;53(2):341–58. https://doi.org/10.1093/oxfordjournals.bmb.a011617.
Blondon M, Harrington LB, Boehlen F, Robert-Ebadi H, Righini M, Smith NL. (2016)Pre-pregnancy BMI, delivery BMI, gestational weight gain and the risk of postpartum venous thrombosis. Thrombosis research 145, 151 – 6.10.1016/j.thromres.2016.06.026.
Juras J, Ivanisević M, Oresković S, Mihaljević S, Vujić G, Delmis J. Successful delivery of fetus with fetal inherited thrombophilia after two fetal deaths. Coll Antropol. 2013;37(4):1353–5.
Patnaik MM, Haddad T, Morton CT. Pregnancy and thrombophilia. Expert Rev Cardiovasc Ther. 2007;5(4):753–65. https://doi.org/10.1586/14779072.5.4.753.
Guerrero B, López M. Overwiew of the Coagulation System and laboratory tests for its study]. Invest Clin. 2015;56(4):432–54.
Gorar S, Alioglu B, Ademoglu E, Uyar S, Bekdemir H, Candan Z, Saglam B, Koc G, Culha C, Aral Y. Is there a tendency for thrombosis in gestational diabetes Mellitus? J Lab Physicians. 2016;8(2):101–5. https://doi.org/10.4103/0974-2727.180790.
de Almeida LGN, Young D, Chow L, Nicholas J, Lee A, Poon MC, Dufour A, Agbani EO. (2022)Proteomics and Metabolomics Profiling of Platelets and Plasma Mediators of Thrombo-Inflammation in Gestational Hypertension and Preeclampsia. Cells 11 (8).10.3390/cells11081256.
Battarbee AN, Palatnik A, Ernst LM, Grobman WA. Association of isolated single umbilical artery with small for gestational age and Preterm Birth. Obstet Gynecol. 2015;126(4):760–4. https://doi.org/10.1097/aog.0000000000001037.
Mailath-Pokorny M, Worda K, Schmid M, Polterauer S, Bettelheim D. Isolated single umbilical artery: evaluating the risk of adverse pregnancy outcome. Eur J Obstet Gynecol Reprod Biol. 2015;184:80–3. https://doi.org/10.1016/j.ejogrb.2014.11.007.
Klaritsch P, Haeusler M, Karpf E, Schlembach D, Lang U. Spontaneous intrauterine umbilical artery thrombosis leading to severe fetal growth restriction. Placenta. 2008;29(4):374–7. https://doi.org/10.1016/j.placenta.2008.01.004.
Polettini J, Dutta EH, Behnia F, Saade GR, Torloni MR, Menon R. (2015)Aging of intrauterine tissues in spontaneous preterm birth and preterm premature rupture of the membranes: A systematic review of the literature. Placenta 36 (9), 969 – 73.10.1016/j.placenta.2015.05.003.
Zhu HL, Shi XT, Xu XF, Zhou GX, Xiong YW, Yi SJ, Liu WB, Dai LM, Cao XL, Xu DX, Wang H. Melatonin protects against environmental stress-induced fetal growth restriction via suppressing ROS-mediated GCN2/ATF4/BNIP3-dependent mitophagy in placental trophoblasts. Redox Biol. 2021;40:101854. https://doi.org/10.1016/j.redox.2021.101854.
Pettker CM, Buhimschi IA, Magloire LK, Sfakianaki AK, Hamar BD, Buhimschi CS. (2007)Value of placental microbial evaluation in diagnosing intra-amniotic infection. Obstet Gynecol 109 (3), 739 – 49.10.1097/01.Aog.0000255663.47512.23.
Chen S, Shenoy A. (2022)Placental Pathology and the Developing Brain. Seminars in pediatric neurology 42, 100975.10.1016/j.spen.2022.100975.
Funding
This work is supported by funding from the National Natural Science Foundation of China (No. 81601319); Project of Wenzhou Science and Technology (No. Y20210026); the Obstetrics and gynecology of combine traditional Chinese and Western medicine of Zhejiang Province (2017-XK-A42); Wenzhou Key Laboratory of Precision General Practice and Health Management.
Author information
Authors and Affiliations
Contributions
S.P., A.X.: Drafting the article and revising it critically for important intellectual content; X.L., B.C., C.X.: Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; Y.H.: Final approval of the version to be published.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki and was approved by the Research Ethics Committee of the four participating hospitals. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pan, S., Xu, A., Lu, X. et al. Umbilical artery thrombosis risk factors and perinatal outcomes. BMC Pregnancy Childbirth 24, 137 (2024). https://doi.org/10.1186/s12884-024-06335-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06335-z