Abstract
Background
When a pregnant woman experiences unusual circumstances during a vaginal delivery, an unplanned cesarean section may be necessary to save her life. It requires knowledge and quick assessment of the risky situation to decide to perform an unplanned cesarean section, which only occurs in specific obstetric situations. This study aimed to develop and validate a risk prediction model for unplanned cesarean sections among laboring women in Ethiopia.
Method
A retrospective follow-up study was conducted. The data were extracted using a structured checklist. Analysis was done using STATA version 14 and R version 4.2.2 software. Logistic regression was fitted to determine predictors of unplanned cesarean sections. Significant variables were then used to develop a risk prediction model. Performance was assessed using Area Under the Receiver Operating Curve (AUROC) and calibration plot. Internal validation was performed using the bootstrap technique. The clinical benefit of the model was assessed using decision curve analysis.
Result
A total of 1,000 laboring women participated in this study; 28.5% were delivered by unplanned cesarean section. Parity, amniotic fluid status, gestational age, prolonged labor, the onset of labor, amount of amniotic fluid, previous mode of delivery, and abruption remained in the reduced multivariable logistic regression and were used to develop a prediction risk score with a total score of 9. The AUROC was 0.82. The optimal cut-off point for risk categorization as low and high was 6, with a sensitivity (85.2%), specificity (90.1%), and accuracy (73.9%). After internal validation, the optimism coefficient was 0.0089. The model was found to have clinical benefits.
Conclusion
To objectively measure the risk of an unplanned Caesarean section, a risk score model based on measurable maternal and fetal attributes has been developed. The score is simple, easy to use, and repeatable in clinical practice.
Similar content being viewed by others
Introduction
Cesarean section (CS) delivery is the delivery of the fetus, placenta, and membranes by an abdominal and uterine wall incision at or after 28 weeks of pregnancy [1]. If pregnant women face unusual conditions during a vaginal delivery, unplanned CS can be a life-saving operation [2].
World Health Organization (WHO) recommends the ideal rate of CS to be between 5 and 15%. Despite this recommendation, the CS rate is rapidly increasing; even the causes for the continuous increase in CS rates are not fully understood [3, 4]. Each year, 20 million CS are performed globally [3], with rates ranging from 7.1% in Sub-Saharan Africa to 63.4% in Eastern Asia [5]. In Ethiopia CS the prevalence was 39.1% [6]. On the contrary, there is research that indicates that, over a certain period, rising unplanned CS rates may be related to higher rates of maternal and neonatal morbidity [7, 8].
Unplanned CS, is associated with increased maternal morbidity and mortality, compared to a scheduled CS [9]. Severe hemorrhage, complications with the quick administration of general anesthesia, and inadvertent damage to the mother and child are among the morbidity linked with unplanned CS [8, 10]. Intrapartum variables such as labor dystocia, fetal distress, and umbilical cord prolapse are reasons for unplanned CS [1]. The most common predictors of unplanned CS were parity, residency, antepartum hemorrhage, prior cesarean section, number of visits Antenatal care(ANC), induction of labor, hypertensive disorder, and induction of labor [4, 6, 10,11,12,13,14,15]
A trial of vaginal labor should be done for expecting women who show no clear indicators of CS. It is also critical to monitor changes in maternal and fetal health status in order to protect mothers and babies and prepare for unplanned CS. It is only performed in specific obstetric situations and requires knowledge and a timely assessment of the dangerous situation for unplanned CS as soon as possible. Identifying an urgent scenario that could be potentially life-threatening is one of the most difficult challenges in obstetrics. Risk prediction of obstetric conditions demanding unplanned CS could be very helpful for both clients' and healthcare providers’ preparedness and timely responses. It helps clinicians, in decision-making with the hope of decreasing maternal and neonatal morbidity and mortality and lowering personal and institutional healthcare costs. It might be beneficial, especially in areas with limited resources. Despite this huge problem, few studies indicate unplanned CS in Ethiopia. Previous studies have focused on determining the associated factors that contribute to unplanned CS. A predictive model enables real-time mothers’ unplanned CS risk stratification, which guides primary attention to care for maternal and neonatal health good health outcomes. There are no studies on prediction models related to unplanned CS based on clinical and demographic variables in Ethiopia. Therefore, this study aims to develop and validate of risk prediction model to predict unplanned CS using easily available variables.
Method and materials
Study design, setting, and population
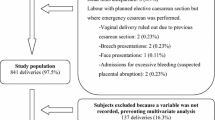
A retrospective follow-up study was conducted at Debre Markos Comprehensive and Specialized Hospital (DMCSH) from January 1, 2020, to May 30, 2022, and data were extracted (collected) from September 1, 2022, to October 2022. Debre Markos Comprehensive and Specialized Hospital is located in Debre Markos Town, which is 299 km from Addis Ababa, Ethiopia's capital city, and 265 km from Bahir-Dar, the capital city of Amhara Regional State. The hospital is one of the largest tertiary-level referral facilities in the Amhara region. (1) All laboring women who give birth from January 1, 2020, to May 30, 2022; (2) A vaginal examination was done before birth, (3) There was no sign of fetal distress. While, multiple pregnancies, breech and transverse presentation, severe fetal malformation-related problems, failure to deliver vaginally in an outside hospital and transfer to our hospital, and direct CS with specific indications were excluded.
Sample size and sampling technique
Sample size calculation using a Rule of thumb of at least 10 events per predictor was used [16]. In the prediction model, each predictor needs at least ten events (dependent variable) we had a total of fourteen predictors (independent variables). To get the estimated sample size, we have used the previous incidence of unplanned CS (13.7%). Therefore, fourteen predictors are multiplied by ten events (rule of thumb) divided by the incidence. Finally, the calculated sample size was 1,021 participants. After all, 1000 participants were included in this study, and 21 were missed data. We have used a previous study incidence of unplanned CS is 13.7% [17].
A simple random sampling technique (method) was employed to select participants using the medical registration number of a delivered mother from the delivery registration book.
Study variables and measurements
Dependent variable
The dependent variable for this study was the mode of delivery. Normal vaginal delivery (NVD) and unplanned CS. Unplanned CS was defined as a case in which the procedure of vaginal delivery was discontinued due to the occurrence of fetal distress or other reasons [1].
Independent variables
The independent variable demographic characteristics of delivered women (Maternal age, weight, and residence), pregnancy history (Gravidity, parity, previous mode of delivery, number of ANC), perinatal complications (amniotic fluid, hypertensive disorders of pregnancy, placental abruption, anemia (hemoglobin < 11 g/dl), PROM, comorbidity(chronic hypertension, DM, heart diseases, etc.), neonatal characteristics(Birth weight, gestational age), and Labor process( Onset of labor(labor starting by inducing or spontaneous), prolonged labor(labor was longer than 24 h)).
Data collection and quality assurance
A data extraction checklist was prepared on the Kobo Toolbox web-based tool for the collection of data from the mother's medical records. The checklist was arranged into demographic characteristics, pregnancy history, perinatal complications, neonatal features, and labor process. Data collectors were trained for two days by the principal investigator. Frequent and timely supervision of data collectors was undertaken.
Statistical analysis
Data were collected using the Kobo Toolbox. Collected data were exported to STATA version 14 and R Software version 4.2.2 for data management and analysis. Missing data were handled by multiple imputations missing handling technique by assuming missing at random. Multi-collinearity among independent predictors was checked by the Variance Inflation Factor (VIF).
Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis Or Diagnosis (TRIPOD) guideline used for developing and reporting prediction model [18]. Tables and figures were used to describe the characteristics of the study participants.
Logistic regression analysis was used to evaluate which variables are the most powerful to predict unplanned CS [19]. A bivariable regression analysis was used to obtain insight into the association of each potential determinant of unplanned CS and for inclusion in multivariable regression analysis. Variables with p-value < 0.25 in the bivariable analysis were fitted to the multivariable regression analysis. After a stepwise backward elimination technique was used, the role of each predictor in the multivariable analysis was assessed by the likelihood ratio test. The unplanned CS prediction model was developed from significant variables in the reduced multivariable regression model. Regression coefficients of the reduced model were used as a measure of the effect of predictor variables on the probability of unplanned CS.
A risk score was developed using identified coefficients for which the weights were defined as the quotient of the corresponding estimated coefficient from a reduced multivariable regression analysis divided by the smallest beta-coefficient and rounded to the nearest integer. We determined the total score for each individual by assigning the points for each variable present and adding them up. The score was transformed to a dichotomous; allowing each pregnant woman to be classified as a high or low risk of unplanned CS. The model performance was assessed using discrimination power and calibration. The area under the receiver operating characteristic curve was used to evaluate the discrimination power of the developed prediction model. Model calibration was assessed using a calibration plot and p-value to ensure the reliability of the prediction models. To choose the optimal cut-off point to separate the risk score of the patients as high and low, the Youden index method was used [20]. For evaluation of the predictive efficiency of the optimal cut-off values of the models, sensitivities, specificities, PPV (Positive Predictive Value), NPV (Negative Predictive Value), likelihood ratio, and accuracy were used. Internal validation was performed using the bootstrap procedure replicating the sample 1,000 times to estimate how the performance of the prediction model developed on the development set would be on a hypothetical set of new patients. Decision curve analysis was used to assess the clinical benefit of the prediction model.
Results
Demographic characteristics of delivered women
A total of 1,000 laboring women were included in this study with a response rate of 97.9%. The median age of mothers was 27 with an Interquartile Range (IQR) of 24 to 30 years and the majority of them were aged between 20–34 years. More than three-fourths of the mothers were urban residents from them 23.4% of mothers had delivered by unplanned CS and almost all of the mothers were married (Table 1).
Perinatal and intrapartum characteristics
Nearly two-thirds (59.8%) of the study participants were multigravida. More than half (54.6%) of the study subjects were multipara, and the majority (76.56%) of the 546 multiparous women gave birth vaginaly. Concerning the previous mode of delivery, about 71 of the study participants gave birth via CS and a considerable proportion (46.48%) of them delivered vaginally despite previous CS scar. Seventy-one (7.8%) of the participants underwent induction of labor for the indexed childbirth (Table 2).
Development of prediction model for unplanned CS
Predictor selection for prediction of unplanned CS
From routinely collected data on demographic, perinatal, and intrapartum characteristics of laboring women, 20 potential predictors were considered for further evaluation to be included in the prediction model. 17 predictors were identified using univariate regression analysis. The variables including age, weight, MUAC, hemoglobin, PIH, PROM, birth weight, and number of ANC were excluded for insignificant association. Those predictors with P < 0.25 were incorporated in the multivariate logistic regression analysis. By using backward stepwise selection, predictors with P < 0.15 with likelihood ratio test for their role on the regression model were finally seven predictors left in the reduced model and selected as candidates for prediction model development; including Parity, amount of AF, Gestational age, Prolonged labor, onset of labor, Amniotic fluid status, previous mode of delivery, and Abruption(yes) (Table 3).
Prediction Model development for unplanned CS
The theoretical design of this study found to be
Based on the regression coefficients of predictors in the reduced model, the linear predictor model for estimated probability unplanned CS of laboring women could be calculated as:
Linear prediction model of unplanned CS
The equation provided above estimates the probability of unplanned CS based on the status they have on the predictors. Laboring women had 2 possible values in each predictor. If the risk presents for the predictors corresponding beta coefficients will be added otherwise will be taken as zero if the risk is absent.
The AUC of the reduced model was 0.830(95% CI: 0.804–0.858) (Fig. 1). As the calibration plots and test; a P-value of 0.076, the estimated probability of unplanned CS agreed very well with the observed probability which indicates the model does not misrepresent the data.
Validation of the model using the bootstrap technique revealed little evidence of undue influence by particular observations, with an optimism coefficient of 0.00087 and an AUC of 0.80 (adjusted 95% CI: 0.77–0.84).
Risk score development
For simplicity of clinical use and to avoid sophisticated risk calculation, a Simplified risk score predictor model for the estimated risk of unplanned CS was developed by rounding the regression coefficients to the nearest integer after weighting with the least coefficient.
The estimated risk score of unplanned CS was calculated as
Developed prediction models using original beta and simplified risk score had similar discrimination ability (AUC of simplified risk score was 0.820(95% CI: 0.790–0.849)) as well as comparable sensitivity and specificity for their optimal cut-off points. The possible minimum and maximum scores for laboring women can be 0 and 18, respectively. The optimal cutoff point was suggested by the Youden index [20] to dichotomize the risk of unplanned CS as high risk and low risk found to be 6. Patients with a score less than 6 were low risk and those with 6 and above were at high risk of unplanned CS.
Table 4 shows the predictive efficiency of different possible cut-off points of the simplified risk score. The cut-off points 6 had a sensitivity of 85.2%, specificity of 90.1%, Positive predictive value of 66.1%, Negative predictive value of 75.4%, and Accuracy of 73.9%.
Risk classification
According to the developed risk score, of all the laboring women included in the study, 618 were categorized under the low-risk group and the proportion of unplanned CS was 10.5%. 384 laboring women were found to be high risk with a percentage of unplanned cesarean delivery of 18.0% (Table 5).
Decision curve analysis
The aim of developing this prediction model is for early differentiation of those who will be delivered by unplanned CS so that they will be given critical attention to receive timely and appropriate care. As Fig. 2 shows, the model has the highest net benefit across the entire range of threshold probabilities, which indicates that the model has the highest clinical and public health value. Hence, surgical decision made using the model has a higher net benefit than not doing for all or doing for all regardless of their risk threshold (Fig. 2).
Discussion
The present study was designed to develop and validate risk scores to predict unplanned cesarean section using maternal and fetal characteristics among laboring women who gave birth. Thus, predicting the probability of unplanned CS in laboring women is critical in order to take appropriate action. The unplanned CS scores could be used in combination with other clinical information to assist laboring mothers with guidance, expectations, and decision-making.
This study developed a novel risk score in the country for categorizing laboring women's risk of unplanned CS at the time of admission to labor. Demographic and clinical characteristics of laboring women were considered to determine predictors of risk of unplanned CS and to develop a risk prediction model. After the assessment of the association between predictors and unplanned CS, nulliparous, AF status, gestational age, prolonged labor, onset of labor, amount of amniotic fluid, previous mode of delivery, and abruption were selected as predictors.
This score is built up with predictors, widely available in current practice, simple to investigate, and quite affordable. Some of these parameters had already proven to be predictors of unplanned CS in previously published studies. Nulliparous was among the set of predictors studies done in China [2], Columbia [10], United Kingdom [21], Germany [22], Palestinian [15], Tanzania [23]. oligohydraous AF amount (Abnormal) has become part of a risk factor for unplanned CS evidenced by studies done in China [2] and Palestinian [15]. This is in agreement with the results of research and review articles [2, 14, 22, 24]. Prolonged labor China [25], wollo [11], Addis Ababa 2019(33), Palestinian (52). The onset of labor (induced) China [2], United Kingdom [21], United States [26], Addis Ababa 2019(33), and Palestinian [15], Amniotic fluid (abnormal) China [2], United Kingdom [21]. Previous cesarean delivery was a significant factor in predicting unplanned CS. This finding is consistent with the results of other studies in China [2], Germany [22], wollo [11], Addis Ababa [14], Addis Ababa 2019 [24], Palestinian [15], and Debre Tabor [6]. Abruption is also a predictor of PTB in line with other studies conducted in China [2], Nigeria [27], the United Kingdom [21], and wollo [11].
Combining the above predictors the developed risk score results AUC of 0.82 which is a good accuracy [28]. The prediction accuracy to differentiate laboring women's risk of unplanned CS is 82% which is determined by the status of each predictor. This discrimination ability of our model was higher compared to the AUC of the prediction model in China [2] with AUC of 0.787, the Netherlands with an AUROC of 0.58 [29], and another study with AUC of 0.74 [10]. The difference in discrimination ability might be because the scores were developed with different combinations of demographic and clinical parameters.
In ordinary clinical and public health practice, the simplified risk score generated using the regression models is more convenient to use than the regression models and has equivalent discrimination. Without any advanced laboratory or imaging testing, this study measured the predicted performance of a model based on maternal features during pregnancy and labor. Furthermore, By using the Yoden index as an ideal cut point, we found that this prediction model's sensitivity, specificity, PPV, NPV, and accuracy achieved 85.15%, 90.12%, 75.44%, 66.11%, and 73.9%, respectively, at a score cutoff of 6.
The developed model was well calibrated which shows its reliability and showed similar discrimination performance after internal validation which indicates it is capable of predicting unplanned cesarean in independent sets of women with similar accuracy. The decision curve analysis revealed the developed risk score for early categorization of risk-laboring women for unplanned cesarean section has better clinical benefit compared to doing for none and doing for all laboring women in a wide range of threshold probabilities. Therefore, priority focus should be given based on the prediction model that had a greater cost–benefit ratio than doing for none and doing for all laboring women regardless of the prediction probability.
Strength and limitations
The strengths of the study were, first that it was conducted with an adequate number of participant outcomes for predicting unplanned CS, which helped construct the model using a sufficient number of predictor variables and protect overfitting. Second, we have developed a simple risk score for unplanned CS which enables clinicians and patients to make personalized predictions easily and quickly. In addition, our prediction tool can serve as a guide for local governments and health departments to improve labor and delivery outcomes. The study was not without limitations, it would have been better if it had been conducted using a prospective follow-up study design. In retrospectively collected data, some variables for the prediction of unplanned CS might have been missed. However, a risk score developed using retrospectively collected data is still important in resource-limited settings like Ethiopia. Besides, the model was not externally validated using an independent dataset. It would have been better if it had gone through external validation to ensure its prediction capability when applied to other contexts.
Conclusions and recommendations
The developed prediction model includes nulliparous, AF status, gestational age, prolonged labor, the onset of labor, amount of amniotic fluid, previous mode of delivery, and abruption as predictors of Unplanned CS. The risk score was able to predict unplanned CS of laboring women with good discrimination ability and clinical benefit. Hence, this prediction score offers an opportunity to give appropriate and timely intervention which therefore improves maternal and fetal outcomes. We recommended that clinicians use it may assist in clinical decision-making and that researchers validate the prediction tool in another context.
Availability of data and materials
The data sets used and analyzed during the current study were available from the corresponding author upon reasonable request.
References
Ministry of Health. Obstetrics management protocol, January 2021, in Ethiopia. 2021.
Guan P, et al. Prediction of emergency cesarean section by measurable maternal and fetal characteristics. J Investig Med. 2020;68(3):799–806.
Betran AP, et al. WHO statement on caesarean section rates. BJOG. 2016;123(5):667–70.
WHO. WHO recommendations non-clinical interventions to reduce unnecessary caesarean sections. Geneva: World Health Organization; 2018.
Betran AP, et al. Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health. 2021;6(6):e005671.
Taye MG, et al. Prevalence and factors associated with caesarean section in a comprehensive specialized hospital of Ethiopia: a cross-sectional study; 2020. Ann Med Surg (Lond). 2021;67:102520.
Miseljic N, Ibrahimovic S. Health implications of increased cesarean section rates. Mater Sociomed. 2020;32(2):123–6.
Darnal N, Dangal G. Maternal and fetal outcome in emergency versus elective caesarean section. J Nepal Health Res Counc. 2020;18(2):186–9.
Sharma A, et al. Elective versus emergency caesarean section: differences in maternal outcome. Int J Reprod Contracept Obstet Gynecol. 2019;8(8):3207–13.
Tun MH, et al. Prediction of odds for emergency cesarean section: a secondary analysis of the CHILD term birth cohort study. PLoS ONE. 2022;17(10):e0268229.
Ayalew M, et al. Magnitude of cesarean section delivery and its associated factors among mothers who gave birth at public hospitals in Northern Ethiopia: institution-based cross-sectional study. J Multidiscip Healthc. 2020;13:1563–71.
Batieha A, et al. Cesarean section: incidence, causes, associated factors and outcomes: a national prospective study from Jordan. Gynecol Obstet Case Rep. 2017;3(3):55.
Burke N, et al. Prediction of cesarean delivery in the term nulliparous woman: results from the prospective, multicenter Genesis study. Am J Obstet Gynecol. 2017;216(6):598. e1-598. e11.
Tsegaye H, et al. Prevalence and associated factors of caesarean section in Addis Ababa hospitals, Ethiopia. Pan Afr Med J. 2019;34:136.
Zimmo M, et al. Differences in rates and odds for emergency caesarean section in six Palestinian hospitals: a population-based birth cohort study. BMJ Open. 2018;8(3):e019509.
Riley RD, et al. Calculating the sample size required for developing a clinical prediction model. BMJ. 2020;368:m441.
Shit S, Shifera A, Eyado R. Prevalence of cesarean section and associated factor among women who give birth in the last one year at Butajira General Hospital, Gurage Zone, SNNPR, Ethiopia, 2019. Int J Pregn Chi Birth. 2020;6(1):16–21.
Collins GS, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. J Br Surg. 2015;102(3):148–58.
Steyerberg EW, Vergouwe Y. Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J. 2014;35(29):1925–31.
Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–5.
Johnson R, Slade P. Does fear of childbirth during pregnancy predict emergency caesarean section? BJOG. 2002;109(11):1213–21.
David M, et al. Does an immigrant background affect the indication, incidence or outcome of emergency cesarean section? Results of the prospective data collection of 111 births. Geburtshilfe Frauenheilkd. 2018;78(2):167–72.
Mdegela MH, et al. How rational are indications for emergency caesarean section in a tertiary hospital in Tanzania? Tanzan J Health Res. 2012;14(4):236–42.
Gebreegziabher Hailu A, et al. Determinants of cesarean section deliveries in public hospitals of Addis Ababa, Ethiopia, 2018/19: a case-control study. Obstet Gynecol Int. 2020;2020:1–7.
WHO. WHO Statement on Caesarean Section Rates. 2015.
Danilack VA, et al. Development and validation of a risk prediction model for cesarean delivery after labor induction. J Womens Health (Larchmt). 2020;29(5):656–69.
Swende T. Emergency caesarean section in a Nigerian tertiary health centre. Niger J Med. 2008;17(4):396–8.
Swets JA. Measuring the accuracy of diagnostic systems. Science. 1988;240(4857):1285–93.
Lagendijk J, et al. Validation of a prognostic model for adverse perinatal health outcomes. Sci Rep. 2020;10(1):1–7.
Acknowledgements
The authors are very grateful to the University of Gondar, College of Medicine and Health Science, School of Midwifery for the approval of the ethical clearance. Finally, we would like to extend our appreciation to DMCSH staff members, study participants, and data collectors.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
BM conceived the study BM and GA analyzed the data, BM drafted the manuscript, and BM, MM, TW, MS and GA reviewed the article. MM, TW and MS extensively reviewed the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were conducted according to the ethical standards of the declarations of Helsinki.
The Institutional Review Board (IRB) of the University of Gondar approved the study and waived the need for informed consent with reference number (30/2015).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fente, B.M., Asaye, M.M., Gudayu, T.W. et al. Prediction of unplanned cesarean section using measurable maternal and fetal characteristics, Ethiopia, a retrospective cohort study. BMC Pregnancy Childbirth 24, 161 (2024). https://doi.org/10.1186/s12884-024-06308-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06308-2