Abstract
Background
Contraceptive use is a key indicator of improving the health and well-being of women, mothers and their families, preventing unwanted pregnancies, and reducing maternal and child mortalities. Despite a lot of investments from the Government of Guinea to improve contraceptive use, studies reveal that contraceptive use still remains low in Guinea. However, the intention to use contraceptives in Guinea has not been well examined. Therefore, this study seeks to examine the factors associated with the intention to use contraceptives among women of reproductive age in Guinea.
Methods
The study made use of data from the Guinea Demographic and Health Survey (GNDHS) conducted in 2018. For this study, we included a weighted sample of 6,948 women who were either married or cohabiting and responded to all the variables of interest. The data were analyzed using Stata version 14.2. Descriptive and multilevel logistic regression were carried out to examine the factors associated with the intention to use contraceptives. The results of multilevel logistic regression were presented using adjusted odds ratios at 95% confidence intervals and p-value < 0.05 to determine the significant associations.
Results
The prevalence of intention-to-use contraceptives among women was 19.8% (95% CI18.3%–21.5%). Women with secondary/higher educational levels [aOR = 1.58, 95% CI = 1.26–1.99], women whose partners had secondary/higher educational level [aOR = 1.26, 95% CI = 1.04–1.52], women who were cohabiting [aOR = 1.74, 95% CI = 1.13–2.68] and were exposed to mass media [aOR = 1.60, 95% CI = 1.35–1.89] were likely to have higher intentions to use contraceptives. Additionally, women from the Kankan Region [aOR = 4.26, 95% CI = 2.77–6.54] and women who belong to the richer wealth quintile [aOR = 1.36, 95% CI = 0.91–1.89] were likely to have higher odds of intentions to use contraceptives. However, women aged 45–49 years, those from the Peulh ethnic group, and those who lack the competence to make healthcare decisions alone had lower odds of intention to use contraceptives.
Conclusion
The study revealed a low prevalence of intention to use contraceptives among women of reproductive age in Guinea. The study has highlighted that both individual-level and household/community-level factors were significantly associated with the intention to use contraceptives. Therefore, policymakers and stakeholders need to consider these factors discussed in this paper when developing policies and interventions to promote and enhance intention-to-use contraceptives among women of reproductive age in Guinea. The findings call on the Government of Guinea and all stakeholders in Guinea to ensure that female education is promoted to help improve their social status, decision-making on fertility, and reduce fertility rates and maternal mortality.
Similar content being viewed by others
Background
Population growth is a major concern in many low-and-middle-income countries (LMICs), especially in sub-Saharan Africa (SSA) [1]. The population of SSA is estimated to increase more than expected in the next three decades, and it is projected to account for more than half of the world’s total population [1,2,3,4]. On average, SSA countries have fertility rates exceeding five children per woman [2]. It has been demonstrated that using contraceptives is an effective medical method for controlling fertility and enhancing mother-and-child health. [5].
The beginning of the 21st century saw a remarkable increase in the use of contraceptives in all parts of the world, including SSA [5]. The availability, accessibility, and utilization of contraceptives have contributed to more freedom independence and promoted gender equality through the sexual and reproductive health and rights of women [6]. Contraceptive methods, including pills, intrauterine devices, and condoms, which account for more than three-quarters of global contraceptive use, allow couples to have sex without any fear of pregnancies, sexually transmitted infections (STIs), or having to opt for abortion [6, 7].
Contraceptive use is a key indicator of increasing female education, women’s empowerment, improving the health and well-being of mothers and their families, and reducing maternal and child deaths [2, 8, 9]. Scholarly information has revealed that the intention to use contraceptives is a measure for women to better visualize their fertility needs and is more likely to translate to actual practice [10].
There have been a lot of investments and funding from local governments, community-based organizations, and extraterritorial organizations including non-governmental agencies and charity organizations, to improve contraceptive use in the last two decades [11, 12]. Specifically, the Government of Guinea has enacted a law called “The Reproductive Health” that details strategies that stakeholders can adopt to improve health standards and procedures for reproduction, the plan for securing reproductive health products, and the plan for repositioning family planning [13]. The government has received funding the from United Nations Population Fund (UNFPA), the United States Agency for International Development (USAID), the International Parenthood Federation (IPPF), and other donor partners to help execute intentions to use contraceptives and contraceptive-related initiatives and interventions [13].
The government has also created family planning access points at health facilities, established a budgeted 2019-2023 action plan, and created a 2015–2019 Strategic Plan for Health and Development of Adolescents and Youth that seeks to improve contraceptive use. These programs advocate for free family planning services for young people [14]. Despite these interventions, studies have revealed that contraceptive use still remains low in Guinea [15, 16].
Intention to use contraceptives among women of reproductive age is one of the key pathways to monitor the progress of Sustainable Development Goals three and five (SDGs 3 & 5) [17]. This supports universal access to sexual and reproductive healthcare services, including family planning, and achieving gender equality and empowering all women and girls by 2030 [18, 19].
One of the most effective ways to limit family size and unwanted pregnancies has been the intention to use contraceptives [20]. Although the intention to use contraceptives is recognised to be beneficial to the health of the mother and child, the family, and society [21], fertility is still high in Guinea [13]. The fertility rate in Guinea has not witnessed a significant decline. That is, the fertility rate of Guinea in 2005 has decreased from 5.7 births per woman of reproductive age to 4.8 births per woman of reproductive age in 2018 [13].
High fertility is a persistent problem for women of reproductive age, stakeholders, governments, and their agencies [20]. Empirical studies have shown that intention to use contraceptives among women of reproductive age in SSA has been affected by their partners’ preferences for fertility and other sociodemographic factors like age, educational level, exposure to mass media, marital status, place of residence, the number of children, distance to a health centre, the ideal number of children, employment status, and religion [20,21,22,23].
Studies on contraceptives in Guinea have focused on adolescents and young women [15, 16, 24, 25] and married women [26]. However, there is a paucity of studies focusing on the multilevel prevalence and factors associated with the intention to use contraceptives among women of reproductive age in Guinea. The multilevel factor approach will help to improve our understanding of both individual and household/community level factors that are statistically significant to the intention to use contraceptives among women of reproductive age in Guinea. Hence, this research seeks to fill the gap by examining the prevalence and factors associated with the intention to use contraceptives among women of reproductive age in Guinea. Therefore, this current study will provide up-to-date evidence for policymakers and other program managers to design and implement programs that may be appropriate interventions to increase the intention of contraceptive use among women of reproductive age in Guinea.
Materials and methods
Data source and study population
The study made use of data from the most recent Guinea Demographic and Health Survey (GNDHS), conducted in 2018. The DHS is a countrywide representative survey undertaken over a five-year period in several LMICs in Asia and Africa [27]. It focuses on demographic and health issues by interviewing women in their reproductive years (15–49 years). The DHS follows standardized procedures in areas such as sampling, questionnaires, data collection, cleaning, coding, and analyses, which allow for comparison across countries. Details of the methodology, instruments, pretesting of the instruments, training, and recruitment of enumerators are documented in the final report of the 2018 GNDHS [13]. The dataset is freely available for download at: https://dhsprogram.com/data/dataset/Guinea_Standard-DHS_2018.cfm?flag=1. We relied on the “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) statement in writing the manuscript [28].
Study population and inclusion criteria
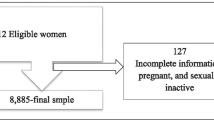
For this study, we used the women’s recode file with a weighted sample of 6,948 reproductive-age women who were either cohabiting or married and had complete cases on the variable of interests [Fig. 1]. The study excluded women with infecundity, who are currently contraceptive users, and who are currently pregnant [3, 21].
Description of variables
Outcome variables
The outcome variable for the study was the intention to use contraceptives among reproductive-age women who are either cohabiting or married. This variable has three responses: “use later,” “unsure about use,” and “does not intend to use.” For this study, the response categories were recoded as ”do not intend to use” = “no,” which included do not intend to use and unsure about use, while ”intend to use” = “yes” was intend to use. Other DHS studies employed similar coding [3, 22, 29].
Independent variables
Based on the literature, sixteen independent variables were investigated as factors associated with the intention to use contraceptives among women of reproductive age. These variables were considered based on literature [3, 30,31,32]. The variables were grouped as individual and household/community-level factors. The individual-level variables included age (15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49); education (no education, primary education, secondary/higher); partner education (no education, primary school, secondary school/higher); marital status (married, cohabiting); employment status (not working, working). Additionally, parity (no birth, one birth, two births, three births, four or more births), mass media (no, yes), age at first sex (< 20, \(\ge 20\)) and religion (Muslim, Christian, Traditional, no/other religion).
The household/community-level factors are healthcare decision-making capacity (alone, not alone); ethnicity (Soussou, Peulh, Malinké, Forestier/others); region (Boke, Conakry, Faranah, Kankan, Kindia, Labe, Mamou, N’zerekore); wealth (poorest, poorer, middle, richer, richest); place of residence (urban, rural); community literacy level (low, medium, high); and community socioeconomic status (low, moderate, high). The community literacy level is measured as the proportion of women who completed at least primary education, and community socioeconomic variables were obtained by aggregating the individual-level variables into clusters.
Statistical analysis
The data were processed and analyzed using Stata version 14.2. First, a descriptive analysis was used to describe the prevalence of the intention to use contraceptives. This was followed by a bivariate result on the distribution of the independent variables against the outcome variable using chi-square [χ2] test of independence. Variables that showed statistical significance at a p-value of 0.05 were moved into the multilevel logistic regression analysis. Therefore, women were nested within clusters and considered as random effects to cater for the unexplained variability at the household/community level [9, 32]. Using the variance inflation factor (VIF), the multicollinearity test showed that there was no evidence of collinearity among the explanatory variables (mean VIF = 2.02).
In the multilevel logistic regression, which has fixed and random effects, there are 4 models. The first model (Model 0) was an empty model where no explanatory variable was used and the result showed the variance of intention to use contraceptives attributable to the distribution of the primary sampling units. Model 1 took into account only individual -level variables, while Model 2 had only household/community-level variables. Model 3, which was the complete model, had both the individual and household/community-level variables. The results were presented as adjusted odds ratios (aORs) with their corresponding 95% confidence intervals, signifying their level of precision. The STATA command ‘melogit’ was used in fitting these models. Model comparison was done using the log-likelihood ratio (LLR) and Akaike’s Information Criterion (AIC). The complex nature of the sampling structure of the data was adjusted using the Stata Survey command ‘svyset v021 [pweight = wt], strata (v023)’.
Results
Prevalence
From the study, the prevalence of intention to use contraceptives among women of reproductive age is 19.8% (95% CI:0.18–0.21) (see Fig. 2).
Socio-demographic characteristics of women of reproductive age
The results (Table 1) showed that 21.2% of the respondents were aged 25–29; 81.0% had no formal education; 74.2% of respondents’ partners had no formal education; and 97.8% of the participants were married. More than two-thirds (74.9%) were working, 43.5% had four or more births, 63.2% indicated that they had access to mass media, and 89.1% were Muslims. More than three-quarters (88.1%) of the respondents had their first sex before age 20 years; 41.2% were Peulh; and 15.2% reside in Kindia Region. With regard to healthcare decision-making capacity, 90% indicated that they do not make decisions alone; 23.7% were in the poorest wealth quintile 72.1% resided in rural areas; 40.5% and 65.8% had low community literacy levels and low community socioeconomic status, respectively.
The result shows the highest prevalence of intention to use contraceptives among women aged 15–19 (27.9%), those with secondary/higher education (33.7%), partners with secondary/higher education (28.2%), cohabiting women (38.7%), and working women (20.2%). Women with one birth (22.0%), women who had exposure to mass media (24.4%), and women who make healthcare decisions alone (25.7%) had the highest prevalence of the intention to use contraceptives. With regards to religion, and age at first sex, the highest prevalence was found among Christians (21.9%) and women who had sex before the age of 20 (20.3%), respectively. The highest prevalence of intention to use contraceptive was found among women who were in the richest wealth quintile (25.0%), women residing in an urban setting (25.0%), women affiliated with the Malinké ethnic group (26.6%), women who reside in Kankan Region (34.2%), women in high community literacy level (24.2%), and women with moderate community socioeconomic status (25.8%).
Multilevel logistic regression analysis of intention to use contraceptives
In Table 2, Model 3 presents the results of the multilevel logistic analysis on the factors associated with the intention to use contraceptives among women of reproductive age. With regards to age, women aged 45–49 years had lower odds of intention to use contraceptives [aOR = 0.23, 95% CI = 0.17–0.33] compared to women aged 15–19 years. Women with secondary/higher educational levels [aOR = 1.58, 95% CI = 1.26–1.99] had higher odds of intention to use contraceptives compared with women with no education. Partners with secondary/higher education had a greater likelihood of contraceptive use [aOR = 1.26, 95% CI = 1.04–1.52] than those with no education. Women who were cohabiting had higher intention to use contraceptives [aOR = 1.74, 95% CI = 1.13–2.68] than married women. It was found that women who were exposed to mass media were likely to have higher intention to use contraceptives [aOR = 1.60, 95% CI = 1.35–1.89].
With regards to healthcare decision-making capacity, intention to use contraceptives was lower among women who do not have the capacity to make healthcare decisions alone [aOR = 0.69, 95% CI = 0.55–0.86] compared to those who have the capacity to make healthcare decisions alone. Women affiliated with the Peulh ethnic group had lower odds of intention to use contraceptives [aOR = 0.49, 95% CI = 0.37–0.64] compared to those affiliated with Soussou ethnic groups. Women who live in the Kankan Region had higher odds of intention to use contraceptives [aOR = 4.26, 95% CI = 2.77–6.54] compared to those who live in the Boke Region. Regarding wealth quintiles, women in the richer wealth quintile had higher odds of intention to use contraceptives [aOR = 1.36, 95% CI = 0.91–1.89] than their counterparts who are in the poorest wealth quintile (See Table 2).
Random effects (measures of variation) results
The result of the random effect (Table 2) indicates that there was a statistically significant variation in the intention to use contraceptives across the clusters. In the empty model, there were substantial variations in the likelihood of intention to use contraceptives across the clustering of the PSUs [σ2 = 0.94, 95% CI 0.74–1.19]. The ICC value for Model 0 shows that 22% of the variation in the intention to use contraceptives was attributed to the between-cluster variations of the characteristics. The variation between clusters then decreased to 18% in Model 1, which was the individual-level only model. The ICC further decreased to 13% in Model 2, which had only household/community-level factors model. In the final model (Model 3), the between-cluster variation further decreased to 11%. This can be attributed to the differences in the clustering of the PSUs, which account for the variations in the intention to use contraceptives. From the model specification analysis, Model 3, which is the complete model with individual-level and household/community-level factors, had the lowest AIC compared to the other models, affirming the goodness of the model (see Table 2).
Discussion
This study examined the prevalence and factors associated with intention to use contraceptives among women of reproductive age in Guinea, a country in West Africa that is noted to have a history of low contraceptive use and high maternal and child mortalities [15, 33]. The study revealed that two out of ten women in Guinea had the intention to use contraceptives (19.8%). The study results further indicated that women’s age, educational level, partners educational level, marital status, mass media, healthcare decision-making capacity, ethnicity, region, and wealth were significantly associated with the intention to use contraceptives among women of reproductive age in Guinea.
The prevalence found in this present study is higher than a prevalence of 18.2% in western Ethiopia [34]. However, it is lower than those reported by studies conducted in Mozambique [22], southern Ethiopia [35], and SSA [3]. The low prevalence of the intention to use contraceptives demonstrates that the use of contraceptives to regulate fertility and improve mother and child health may still be a significant problem in Guinea. The difference in prevalence could be due to variation in the study design, access to information and services, myths, fear of side effects, socio-economic status, and community norms and factors [34,35,36].
In this study, women aged 45–49 had lower odds of intention to use contraceptives in Guinea. This finding is consistent with other studies conducted in Ethiopia [18], Nigeria [28], Malawi [29], and SSA [3]. However, studies conducted in the north and northwest of Ethiopia [37, 38] were contrary to the finding of this study. The plausible reason for our finding could be that older women may have experienced a decline in coital frequency. Additionally, these older women may be unwilling and uncomfortable discussing their reliance on other conventional methods, including string ties. This could have resulted in a lower intention to use contraceptives [3, 29].
The study found a significant association between the educational level of respondents and their intention to use contraceptives. Compared to women with no formal education, women with secondary/higher educational levels were found to have higher odds of having the intention to use contraceptives. The finding resonates with other studies conducted in SSA [3, 29, 35, 37, 39]. However, this finding is inconsistent with other studies done in Ethiopia [17, 40]. This could be attributed to the fact that educated women had access to different sources of information on contraceptives and were empowered. This will not only increase women’s social status but also their decision-making on fertility issues, and reduce fertility rates, and maternal mortality [21, 41].
The education of the respondent’s partner was one of the key factors associated with the intention to use contraceptives. This investigation is consistent with other studies conducted in northern Ethiopia [17], Cameroon [42], and Nigeria [43]. However, another study in Ethiopia [39] revealed that the education of the respondent’s partner and their intention to use contraceptives were not significant. The possible explanation could be that an educated partner may motivate and support their wife’s intention to use contraceptives since they may be well informed about the importance of contraceptives.
The likelihood of an intention to use contraceptives among women cohabiting was higher than that of women who were married. The finding of this study is in agreement with a previous study across the SSA [3]. This evidence suggests that cohabiting women may choose to delay having children because of the sociocultural norms that most SSA cultures have about births outside of marriage [44].
Consistent with previous studies in SSA [3], Uganda [45], West Africa [46], and Pakistan [47], this study reveals that women who were exposed to mass media were more likely to have intentions to use contraceptives. This is an indication that women trust the various mass media channels and, hence receive the health benefits of contraceptive use. That is, mass media, including radio, television, and newspapers, have been channels for promoting desirable lifestyles, knowledge, healthy behavior, and attitudes towards contraceptives [47].
Furthermore, women who did not make healthcare decisions alone reported a lower likelihood of intending to use contraceptives. The finding contradicts other studies in Ethiopia [10, 34], Mozambique [22], and Pakistan [47]. This result shows the pivotal role that partners or family members play in influencing the intention of women to use contraceptives in Guinea. Given the importance of healthcare decision-making capacity, the promotion of and education about contraceptives should not only focus on women but should include their partners and immediate family members. This will help women gain autonomy in their healthcare decision-making capacity.
In agreement with previous studies done in SSA [16, 30], this study found that ethnicity is significantly associated with the intention to use contraceptives. Sidibé et al., [16] similarly found that women of reproductive age who belong to the Peulh ethnic group had a lower likelihood of intention to use contraceptives in Guinea. In explaining the plausible reason accounting for this observation, Ahinkorah et al., [48] contended that women of reproductive age belonging to the Peulh ethnic group had little or no support from their partners and may be restricted by their religious beliefs.
Another important factor that significantly influenced the intention of contraceptive use in this study was region. The odds of an intention to use contraceptives were higher among those women living in the Kankan region. This finding is similar to studies conducted in Guinea [16, 24]. This might be due to residual confounding, as data have shown that women from the Conakry region have the highest level of education, access to the contraceptives, and high health service coverage [49]. This finding calls for further studies to understand the reasons for higher odds of intention to use contraceptives in the Kankan region.
Finally, we found the wealth quintile to be significantly associated with the intention to use contraceptives among women of reproductive age in Guinea. The odds of an intention to use contraceptives were higher among women in the richer and richest wealth quintiles. This finding is supported by studies done in Guinea [16], SSA [21], Mozambique [50], Ethiopia [51], and Ghana [52]. It is possible that women who belong to the richer and richest wealth quintiles could pay for the costs associated with contraceptive uptake [53].
Strengths and limitations
This study used the most current nationally representative data from the Guinea Demographic and Health Survey to examine the factors associated with the intention to use contraceptives. Additionally, the authors estimated the cluster effect on intention to use contraceptives among women of reproductive age using a mixed-effects analysis, an appropriate statistical approach. The methods employed in sampling and data collection also support the representativeness of the study. Thus, the findings and recommendations can be applied to all women of reproductive age in Guinea. Also, the cross-sectional nature of this study does not allow for causality to be inferred from the findings. Furthermore, the data were collected retrospectively which may have a recall bias and could lead to over-or under-reporting.
Conclusions and recommendations
The study revealed a low prevalence of intention to use contraceptives among women of reproductive age in Guinea. The study has highlighted that both individual-level and household/community-level factors were significantly associated with the intention to use contraceptives. Therefore, policymakers and stakeholders need to consider these factors when developing policies and interventions to promote and enhance intention-to-use contraceptives among women of reproductive age in Guinea. The findings call on the Government of Guinea and all stakeholders in Guinea to ensure that female education is promoted. This could help improve their social status, decision-making on fertility and reduce fertility rates, and maternal mortality. To improve the intention to use contraceptives among women in Guinea, health education programs through the various channels of mass media should focus on women of all ages and Peulh ethnic group. These findings also support a call for contraceptive strategies that target the involvement of their partners. This is an essential tool that ensures that women have sexual autonomy.
Data Availability
Data is available on https://dhsprogram.com/data/dataset/Guinea_Standard-DHS_2018.cfm?flag=1. Other authors would be able to access or request these data in the same manner as we did from DHS program. Authors did not have any special access or request privileges that others would not have.
Abbreviations
- LMICs:
-
Low-and-middle-income countries
- SSA:
-
Sub-Saharan Africa
- STIs:
-
Sexual Transmitted Infections
- GNDHS:
-
Guinea Demographic and Health Survey
- aOR:
-
Adjusted odds ratio
- CI:
-
Confidence intervals
References
O’Regan A, Thompson G. Indicators of young women’s modern contraceptive use in Burkina Faso and Mali from demographic and Health Survey data. Contracept Reproductive Med. 2017;2(1):1–8.
Adedini SA, Omisakin OA, Somefun OD. Trends, patterns and determinants of long-acting reversible methods of contraception among women in sub-saharan Africa. PLoS ONE. 2019;14(6):e0217574. https://doi.org/10.1371/journal.
Budu E, Ahinkorah BO, Seidu AA, Armah-Ansah EK, Salihu T, Aboagye RG, Yaya S. Intention to use contraceptives among married and cohabiting women in sub-saharan Africa: a multilevel analysis of cross-sectional data. BMJ open. 2022;12(11):e060073.
Atake EH, Ali PG. Women’s empowerment and fertility preferences in high fertility countries in Sub-saharan Africa. BMC Womens Health. 2019;19(1):54.
Haq I, Sakib S, Talukder A. Sociodemographic factors on contraceptive use among ever-married women of reproductive age: evidence from three demographic and health surveys in Bangladesh. Med Sci. 2017;5(4):31.
Gebre MN, Edossa ZK. Modern contraceptive utilization and associated factors among reproductive-age women in Ethiopia: evidence from 2016 Ethiopia demographic and health survey. BMC Womens Health. 2020;20(1):1–14.
Hubacher D, Trussell J. A definition of modern contraceptive methods. Contraception. 2015;92(5):420–1.
Namasivayam A, Lovell S, Namutamba S, Schluter PJ. (2020). Predictors of modern contraceptive use among women and men in Uganda: a population-level analysis. BMJ open, 10(2), e034675.
Solanke BL. Factors influencing contraceptive use and non-use among women of advanced reproductive age in Nigeria. J Health Popul Nutr. 2017;36(1):1–14.
Abraha TH, Belay HS, Welay GM. Intentions on contraception use and its associated factors among postpartum women in Aksum town, Tigray region, northern Ethiopia: a community-based cross-sectional study. Reproductive Health. 2018;15(1):1–8.
Fagbamigbe AF, Afolabi RF, Idemudia ES. Demand and unmet needs of contraception among sexually active in-union women in Nigeria: distribution, associated characteristics, barriers, and program implications. SAGE Open. 2018;8(1):2158244017754023.
Mercer LD, Lu F, Proctor JL. Sub-national levels and trends in contraceptive prevalence, unmet need, and demand for family planning in Nigeria with survey uncertainty. BMC Public Health. 2019;19(1):1–9.
Institut National de la Statistique/INS et ICF. Enquête Démographique et de Santé en Guinée 2018. Guinée, et Rockville, Maryland, USA: INS et ICF: Conakry; 2018.
Ministère de la Sante. Direction Nationale de la Sante familiale et de Nutrition. Plan d’Action national budgétisé de planification familiale 2019–2023 de Guinée. 2018.
Bangoura C, Dioubaté N, Manet H, Camara BS, Kouyaté M, Douno M, Delamou A. (2021). Experiences, Preferences, and Needs of Adolescents and Urban Youth in Contraceptive Use in Conakry, 2019, Guinea. Frontiers in global women’s health, 2.
Sidibé S, Delamou A, Camara BS, Dioubaté N, Manet H, Ayadi E, Kouanda AM, S. Trends in contraceptive use, unmet need and associated factors of modern contraceptive use among urban adolescents and young women in Guinea. BMC Public Health. 2020;20(1):1–10.
Gebremariam A, Addissie A. Intention to use long acting and permanent contraceptive methods and factors affecting it among married women in Adigrat town, Tigray, Northern Ethiopia. Reproductive Health. 2014;11(1):1–9.
Coll CDVN, Ewerling F, Hellwig F, de Barros AJD. Contraception in adolescence: the influence of parity and marital status on contraceptive use in 73 low-and middle-income countries. Reproductive Health. 2019;16(1):1–12.
Dockalova B, Lau K, Barclay H, Marshall A. (2016). Sustainable development goals and family planning 2020. The International Planned Parenthood Federation (IPPF). United Kingdom, 1–12.
Ahuja M, Frimpong E, Okoro J, Wani R, Armel S. Risk and protective factors for intention of contraception use among women in Ghana. Health Psychol Open. 2020;7(2):2055102920975975.
Negash WD, Eshetu HB, Asmamaw DB. Intention to use contraceptives and its correlates among reproductive age women in selected high fertility sub-saharan Africa countries: a multilevel mixed effects analysis. BMC Public Health. 2023;23(1):1–10.
Mboane R, Bhatta MP. Influence of a husband’s healthcare decision making role on a woman’s intention to use contraceptives among Mozambican women. Reproductive Health. 2015;12(1):1–8.
Gilano G, Hailegebreal S. Assessment of intention to use contraceptive methods with spatial distributions and associated factors among women in Ethiopia: evidence from EDHS 2016. Archives of Public Health. 2021;79(1):1–13.
Sidibe S, Delamou A, Camara BS, Camara N, Manet H, Ayadi AME, Kouanda S. (2020). Levels and trends in family planning method use among urban adolescents and young women in Guinea: analysis of demographic and health surveys from 1999 to 2018.
Dioubaté N, Manet H, Bangoura C, Sidibé S, Kouyaté M, Kolie D, Delamou A. Barriers to contraceptive use among urban adolescents and youth in Conakry, in 2019, Guinea. Front Global Women’s Health. 2021;2:655929.
Sidibe S, Camara BS, Dioubaté N, Grovogui FM, Delamou A, Kouanda S. (2020). Non-use of Contraceptive Methods Among Married: Analysis of the 2018 Guinea Demographic and Health Survey.
Dickson KS, Ameyaw K, Akpeke E, Mottey M, Adde BE, K. S., Esia-Donkoh K. (2023). Socio-economic disadvantage and quality Antenatal Care (ANC) in Sierra Leone: evidence from demographic and Health Survey. PLoS ONE, 18(1), e0280061.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Strobe Initiative. The strengthening the reporting of Observational studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9.
Idowu A, Deji SA, Ogunlaja O, Olajide SO. Determinants of intention to use post partum family planning among women attending immunization clinic of a tertiary hospital in Nigeria. Am J Public Health Res. 2015;3(4):122–7.
Forty J, Rakgoasi SD, Keetile M. Patterns and determinants of modern contraceptive use and intention to use contraceptives among Malawian women of reproductive ages (15–49 years). Contracept Reproductive Med. 2021;6(1):1–12.
Nyarko SH. (2020). Spatial variations and socioeconomic determinants of modern contraceptive use in Ghana: a bayesian multilevel analysis. PLoS ONE, 15(3), e0230139.
Ahinkorah BO, Budu E, Aboagye RG, Agbaglo E, Arthur-Holmes F, Adu C, Seidu AA. Factors associated with modern contraceptive use among women with no fertility intention in sub-saharan Africa: evidence from cross-sectional surveys of 29 countries. Contracept Reproductive Med. 2021;6(1):1–13.
Zegeye B, Ahinkorah BO, Ameyaw EK, Budu E, Seidu AA, Olorunsaiye CZ, Yaya S. Disparities in use of skilled birth attendants and neonatal mortality rate in Guinea over two decades. BMC Pregnancy Childbirth. 2022;22(1):1–13.
Tekelab T, Sufa A, Wirtu D. Factors affecting intention to use long acting and permanent contraceptive methods among married women of reproductive age groups in Western Ethiopia: a community based cross sectional study. Fam Med Med Sci Res. 2015;4(158):2.
Meskele M, Mekonnen W. Factors affecting women’s intention to use long acting and permanent contraceptive methods in Wolaita Zone, Southern Ethiopia: a cross-sectional study. BMC Womens Health. 2014;14(1):1–9.
Oyinlola FF, Bamiwuye SO, Ilesanmi BB, Oyeleye OJ, Ekundayo OO, Adewole OE. Neighbourhood factors associated with future use of contraceptives among non-users in Nigeria and Rwanda. Int J Multidisciplinary Thought. 2018;7:487–512.
Syum H, Kahsay G, Huluf T, Beyene B, Gerensea H, Gidey G, Haile K. Intention to use long-acting and permanent contraceptive methods and associated factors in health institutions of Aksum Town, North Ethiopia. BMC Res Notes. 2019;12(1):1–6.
Abajobir AA. Intention to use long-acting and permanent family planning methods among married 15–49 years women in Debremarkos Town, Northwest Ethiopia. Fam Med Med Sci Res. 2014;3(145):2.
Tiruneh FN, Chuang KY, Ntenda PA, Chuang YC. Factors associated with contraceptive use and intention to use contraceptives among married women in Ethiopia. Women Health. 2016;56(1):1–22.
Takele A, Degu G, Yitayal M. Demand for long acting and permanent methods of contraceptives and factors for non-use among married women of Goba Town, Bale Zone, South East Ethiopia. Reproductive Health. 2012;9(1):1–11.
Alemayehu GA, Fekadu A, Yitayal M, Kebede Y, Abebe SM, Ayele TA, Biks GA. Prevalence and determinants of contraceptive utilization among married women at Dabat Health and demographic Surveillance System site, northwest Ethiopia. BMC Womens Health. 2018;18(1):1–7.
Egbe TO, Ketchen SA, Egbe EN, Ekane GEH, Belley-Priso E. Risk factors and barriers to male involvement in the choice of family planning methods in the Buea Health District, south west region, Cameroon: a cross-sectional study in a semi-urban area. Women Health Open J. 2016;1(3):82–90.
Ijadunola MY, Abiona TC, Ijadunola KT, Afolabi OT, Esimai OA, OlaOlorun FM. (2010). Male involvement in family planning decision making in Ile-Ife, Osun State, Nigeria. Afr J Reprod Health, 14(4).
Ahinkorah BO. (2020). Predictors of unmet need for contraception among adolescent girls and young women in selected high fertility countries in sub-saharan Africa: a multilevel mixed effects analysis. PLoS ONE, 15(8), e0236352.
Gupta N, Katende C, Bessinger R. Associations of mass media exposure with family planning attitudes and practices in Uganda. Stud Fam Plann. 2003;34(1):19–31.
Jacobs J, Marino M, Edelman A, Jensen J, Darney B. Mass media exposure and modern contraceptive use among married west African adolescents. Eur J Contracept Reproductive Health Care. 2017;22(6):439–49.
Nguyen TT, Neal S. (2021). Contraceptive prevalence and factors influencing utilization among women in Pakistan: a focus on gender-based Violence. Fulbright Rev Econ Policy.
Ahinkorah BO, Seidu AA, Appiah F, Budu E, Adu C, Aderoju YBG, Ajayi AI. Individual and community-level factors associated with modern contraceptive use among adolescent girls and young women in Mali: a mixed effects multilevel analysis of the 2018 Mali demographic and health survey. Contracept Reproductive Med. 2020;5:1–12.
Epdc. (2023) https://www.epdc.org/sites/default/files/documents/Guinea_coreusaid.pdf Accessed 17th May, 2023.
Dias JG, de Oliveira IT. (2015). Multilevel effects of wealth on women’s contraceptive use in Mozambique. PLoS ONE, 10(3), e0121758.
Lakew Y, Reda AA, Tamene H, Benedict S, Deribe K. Geographical variation and factors influencing modern contraceptive use among married women in Ethiopia: evidence from a national population based survey. Reproductive Health. 2013;10:1–10.
Crissman HP, Adanu RM, Harlow SD. Women’s sexual empowerment and contraceptive use in Ghana. Stud Fam Plann. 2012;43(3):201–12.
Asresie MB, Fekadu GA, Dagnew GW. (2020). Contraceptive use among women with no fertility intention in Ethiopia. PLoS ONE, 15(6), e0234474.
Acknowledgements
The author is grateful to MEASURE DHS for granting access to the datasets used in this study.
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Contributions
EKA-A conceived the study, conducted the analysis, drafted the methods, discussion and conclusion. BB drafted the background, and EKI supervised the drafting of the manuscript. All authors reviewed the manuscript critically for important intellectual content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical consideration
The study used Demographic and Health Survey (DHS) datasets, which did not require further approval since the data is freely available in public domain. Further information about Guinea DHS data usage and ethical standards are available at: https://dhsprogram.com/publications/publication-FR353-DHS-Final-Reports.cfm
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Armah-Ansah, E.K., Bawa, B. & Igonya, E.K. Prevalence and factors associated with intention to use contraceptives among women of reproductive age: a multilevel analysis of the 2018 Guinea demographic and health survey. BMC Pregnancy Childbirth 24, 8 (2024). https://doi.org/10.1186/s12884-023-06204-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-06204-1