Abstract
Background
Despite its benefit in promoting maternal health and the health of her developing fetus, little is known about preconception care practice and its associated factors in Ethiopia. Moreover, preconception care utilization in private hospitals is not known. The purpose of this study, therefore, is to determine the utilization of preconception health care services and its associated factors among pregnant women following antenatal care in the private Maternal and Child Health hospitals in Addis Ababa.
Methods
A Hospital based cross-sectional study was conducted from April 1 to April 30,2022 among 385 women attending ANC in private MCH hospitals. Bestegah and Hemen MCH hospitals were selected by convenience method. Data were collected by a pretested self-administered semi-structured questionnaire. To identify the factors associated with the utilization of preconception care, bivariable and multivariable logistic regression analysis were performed. Adjusted odds ratios with 95% confidence interval were estimated to assess the strength of associations, and statistical significance was declared at a p-value < 0.05.
Results
The utilization of preconception care among the pregnant mothers according to our study was 40%. Professional/technical/managerial occupation (AOR = 4.3, 95%CI = 1.13, 16.33, P < 0.032), having good knowledge on preconception care (AOR = 3.5, 95%CI = 1.92, 6.53, P < 0.000), having unintended pregnancy (AOR = 0.1, 95%CI = 0.03, 0.42, P < 0.001), history of family planning use before conception (AOR = 3.9, 95%CI = 1.20, 12.60, P < 0.023), having pre-existing medical disease(s) (AOR = 8.4, 95%CI = 2.83, 24.74, P < 0.002), and having adverse pregnancy outcome(s) in previous pregnancies (AOR = 3.2, 95%CI = 1.55, 6.50, P < 0.000) were significantly associated with preconception care utilization.
Conclusions
This study found out that the utilization of preconception care in the private MCH hospitals is still low i.e., only 40%. Occupation, level of knowledge, having unintended pregnancy, history of family planning use before conception, having adverse pregnancy outcome(s) in previous pregnancy and having pre-existing medical disease(s) were independently associated with preconception care utilization. Lack of awareness about the availability of the services and having an unintended pregnancy were the main reasons for not utilizing preconception care.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Preconception care(PCC) is defined as a set of interventions that aim to identify and modify biomedical, behavioral, and social risks to a woman’s health or pregnancy outcome through prevention and management [1]. Research has found that while interventions during pregnancy and childbirth are essential for improving outcomes, they are inadequate for realizing on going international improvements in perinatal health and achieving equitable outcomes for all people. The shift toward preconception health was put into motion over a decade ago to challenge this paradigm and focus attention, intervention, and support on the person before pregnancy [2].
Ethiopia has achieved remarkable success in reducing neonatal and maternal mortality in recent decades, but still has very high neonatal mortality rates (29 deaths per 1,000 live births) and maternal mortality ratios (412 deaths per 100,000 live births) [3]. One of the main reasons why maternal mortality is high in Sub-Saharan Africa is high rates of child marriage and unintended pregnancies apart from inadequate quality health care in time to address complications [4]. Ethiopia has one of the highest rate of teenage pregnancy 23.59% [5] and unintended pregnancy among reproductive age group 28% [6]. Therefore, there is little doubt that preconception care would make a significant improvement for our country in these regards [7].
Several studies conducted to look at the level of PCC across the world found the levels to be generally low. Utilization of preconception in China, Malaysia, and Sir Lanka is 40.0% [8], 44% [9], and 27.2% [10] respectively. Preconception care utilization in African countries like Nigeria and Ethiopia 10.3% [11], and 16.27% [12] respectively, which is much lower than the rest of the other developed countries. Moreover, preconception care utilization in private setup is generally not well studied. One study in Kenya found that preconception care utilization in private hospital was 35.% compared to 16.1% in rural public hospital [13].
Based on different articles findings, utilization of preconception care is influenced by age, gender, educational status, income, marital status, history of family planning use, health condition, history of ANC visit, parity, pregnancy intention, and gravidity [8,9,10,11,12,13].
In Ethiopia, several studies have been conducted to assess the utilization rate of preconception health care services among reproductive age women, pregnant and delivered women in community settings and public institutions, and the utilization rate was found to be low [12]. However, similar studies in private institutions are lacking. Hence, this study intends to determine the utilization of preconception health care services in private institutions.
Methods
Study setting and study period
A Hospital based study was conducted in two selected private MCH hospitals in Addis Ababa from April 1–30, 2022. As of 2018, the city has a total estimated population size of 7,823,600. Regarding health facilities and health services, there are 994 clinics, 99 health centers and 42 hospitals. Of the hospitals, 15 are registered public and 27 are registered private hospitals. Of the private hospitals, 8 are maternity specialty hospitals i.e., Maternal and Child Health hospitals.
Study participants
Source population were all pregnant women who have been following ANC at Bestegah and Hemen MCH hospitals in Addis Ababa.
Study population were all sampled pregnant women who came for ANC at Betsegah and Hemen MCH hospitals in Addis Ababa during the data collection period.
Exclusion criteria
Pregnant women who moved to Addis Ababa after conceiving were excluded from the study.
Sample size determination
The sample size was calculated by using a single population proportion formula = Z2p(p-1)/d2 with assumptions of 35.1%, from Kenyan study [13] the population proportion of preconception care utilization in private institution, assuming 95% confidence interval, marginal error of 5% (0.05) and 10% non-response rate.
Adding 10% of no respondent participants; 350 + 0.1 × 350 = 385.
Secondly, factors associated with utilization of preconception care sample size was calculated using Open Epi Version 7 statistical software for two population proportions (Table 1).
When reviewed many studies done in a different part of the world and in Ethiopia, most of them revealed that women’s education status, age of the women, multiparity and knowledge on PCC are the most determinant factors for utilization of preconception care.
After using the EPI-INFO version 7 to calculate the sample size using the above assumption with factors associated utilization of preconception care, maternal age was taken as it gives the maximum sample size i.e., 260 (by one-to-one ratio). Adding 10% non-response, the final sample size is 286.
By comparing the two sample sizes calculated using single proportion and double population formula, the larger sample size, which is 385 as the total sample for the study participants, was taken.
Sampling technique and procedure
Of the Private MCH hospitals, Betsegah and Hemen MCH hospitals were selected by convenience method (Fig. 1). In selected hospitals, all pregnant women attending antenatal clinic within the study period were recruited and participants were selected consecutively until the desired sample size was achieved to ensure that the entire population of antenatal attendees seen at each facilities who consented to participate were involved.
Study variables
The dependent variable in this study was utilization of preconception care services among pregnant women following ANC. The independent variables were socio-demographic variables, previous adverse pregnancy outcome(s), preexisting medical disease(s), the knowledge level on preconception care, accessibility of health facilities, availability of preconception services, affordability of preconception care services and partner’s support.
Operational definition and terms
Unintended pregnancy:
a pregnancy either mistimed or unwanted at a time of conception [6].
Adverse Pregnancy outcome: patient-reported history of one or more of the following outcomes in a previous pregnancy; preterm delivery, low birth weight, stillbirth, abortion or birth defect [17].
Cigarette smoking:
had a history of smoking or currently smoke regardless of amount [18].
Alcohol consumption:
intake of alcoholic drinks of any amount or type other than holidays and culturally special ceremony days [18].
Good knowledge:
those who have scored above or equal to 50% of the correct responses to preconception care knowledge questions [19].
Poor knowledge:
those who have scored less than 50% of the correct responses to preconception care knowledge questions [19].
Preconception care:
any interventions either advice or treatment, and lifestyle modification women received regarding components of preconception care before being pregnant [20].
Preconception care utilization:
if women received at least one type of intervention, either advice or treatment, and lifestyle modification care i.e., mentioned above at least once before being pregnant will be considered as mother utilized PCC.
Private MCH hospitals:
women’s and children’s specialty hospitals managed by individuals or groups, and which is not funded by the State, a public body or Non-governmental Organization.
Data collection procedures and quality assurance
A data from pregnant woman following ANC were collected by a self-administered semi-structured questionnaire developed from previous published literature after modification to fit the research objective. The questionnaire was initially prepared in English and then translated into Amharic (local language) by different language experts of both languages and then to English to check its consistency. The questionnaire was used to elicit information regarding sociodemographic characteristics, knowledge about PCC, utilization of PCC prior to the current pregnancy and factors affecting the utilization of PCC. The questionnaires were administered by nurses. The questionnaire was pretested two weeks before the actual data collection with 5% of the sample size (20 pregnant women) at Zewditu Memorial Hospital in Addis Ababa, and the necessary amendments were done on the questionnaire per the pretest result. To minimize recall bias, the respondents were informed to provide information on events related to 3 months prior to the current pregnancy, and a calendar was provided to assist their recall. The overall activities of data collection were supervised and coordinated by the investigators. The collected data were checked for consistency, completeness, and relevance daily during the entire data collection by the principal investigator. After the data were collected from the respondents, it was translated back to English and analyzed using the statistical package SPSS version 26.
Data processing and analysis
The collected data were entered to Statistical Package for Social Science (SPSS) version 26.0 for analysis. Descriptive statistics were done to describe the data. Binary logistic regression analysis was employed to examine the statistical association between utilization of preconception care and every single independent variable. Variables that showed statistical significance during bivariable analysis at (p-value < 0.25) were entered into multivariable logistic regression to identify statistically significant variables. Multicollinearity was tested by using the variance inflation factor and tolerance test. The Hosmer-Lemeshow test was used to check the model fitness for analysis, with a significance level of 0.310 indicating a good fit model. Adjusted odds ratios (AOR) with 95% CI were estimated to assess the strength of associations and statistical significance was declared at a p-value < 0.05. Tables, figures, and texts were used to present the results.
Results
Sociodemographic characteristics the study participants
Of the 385 participants studied, majority of the respondents (67.8%) were in the age group of 25–34 years, with the mean age and SD being 30.65 and ±4.87, respectively. Three-fourths of the participants completed tertiary level of education. More than 94.5% of them were married. The detailed sociodemographic characteristic are depicted in Table 2.
Obstetric and medical characteristics of the study participants
Regarding obstetric characteristics, 56% of the participants were multiparous followed by nulliparous (40.5%). With regard to ANC booking, 93.5% of them booked at gestational age less than 16 weeks. The detailed obstetric and medical characteristics of study participants are depicted in (Table 3).
Knowledge about preconception care
The findings of this study showed that, 58% (223) of the participants had good knowledge on preconception care. Concerning the specific knowledge, 91% had ever heard about preconception care. About 52.5% (202) of them mentioned screening for infectious disease like HIV, Syphilis, Hepatitis B virus as a components of preconception care. Furthermore, 76.4% (294) of the pregnant participants know that a woman should stop using alcohol and smoking cigarette before conception, and 68.1% (262) of them know that a woman should be on a healthy diet and use folic acid before conception (Table 4).
Utilization of preconception care services
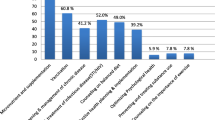
In this study, 40% (154) of the study participants received preconception care before the current pregnancy. No significant differences were noted in the sociodemographic characteristics between the two MCH hospitals except for religion, the level of income, and previous adverse pregnancy outcome(s) (Table 5). The utilization of preconception care was almost similar between the hospitals i.e.,37.3% and 42.7% for Betsegah and Hemen MCH Hospital, respectively.The most frequently used types of preconception care service in this study was family planning 219 (56.88%) and the least utilized preconception service was vaccination 51(13.2%) (Fig. 2).
Other findings in this study were 20.3% (78) of the pregnant were drinking alcohol before conception, of which forty-five of them still drinking alcohol until the end of the first trimester. Similarly, 1.8% [7] of the pregnant women were smoking cigarette before conception and five of them were still smoking cigarette until the end first trimester. On the contrary, only 30.6% (118) the pregnant women were advised on cessation of alcohol consumption and smoking cigarette during preconception period (Table 6).
Partner support and heath facility
In this study 94% (362) of mothers make a decision about maternal health services with their partner. In addition, the cost of PCC services was considered fair by 75.3% (290) of the pregnant women. The most common reasons for not receiving PCC among the pregnant women who did not receive were lack of awareness about the availability of the services 64.8% (136) followed by because their pregnancy wasn’t expected 28.1% (65) and only 11.7% (27) did not acknowledge the importance of PCC (See Table 7).
Factors associated with utilization of preconception care
The strength of association between independent variables and outcome variable (preconception care utilization) were measured using odds ratio and 95% confidence interval using binary logistics regression model. Accordingly, maternal age, educational status, marital status, occupation, monthly income, knowledge on preconception care, parity, use of family planning, unintended pregnancy, adverse pregnancy outcome(s) in previous pregnancy and preexisting medical condition had a p-value of ≤ 0.25 in the bivariable analysis and taken into the final model for multivariable analysis. In multivariable logistic regression analysis, occupation, knowledge on preconception care, use of family planning, unintended pregnancy, adverse pregnancy outcome(s) in previous pregnancy and preexisting medical condition(s) were significantly associated with utilization of PCC at p-value of ≤ 0.05 (Table 8).
Pregnant woman whose occupation is professional/technical/managerial were 4.3 times more likely to receive preconception care when compared to the housewives (AOR = 4.3, 95%CI = 1.13, 16.33, P < 0.032).
Those pregnant women who had good knowledge on PCC were 3.5 times more likely to utilize PCC than those having poor knowledge (AOR = 3.5, 95%CI = 1.92, 6.53, P < 0.000).
Pregnant mothers who had an unintended pregnancy were 90% less likely to utilize PCC compared to whose pregnancy were intended and those who were using family planning before conception were 3.9 times more likely to seek preconception care than mothers who weren’t using family planning before conception (AOR = 0.10, 95%CI = 0.03,0.42, P < 0.001).and (AOR = 3.9, 95%CI = 1.20, 12.60, P < 0.023).
Lastly, those having pre-existing medical disease(s) and adverse pregnancy outcome(s) in previous pregnancy were 8.4 and 3.2 times more likely to utilize PCC than those who had not (AOR = 8.4, 95%CI = 2.83, 24.74, P < 0.000) and (AOR = 3.2, 95%CI = 1.55, 6.50, P < 0.002).
Discussion
Preconception care is an approach to optimize pregnancy outcomes which is crucial for many Sub-Saharan African countries, such as Ethiopia, where maternal and perinatal mortality remains alarmingly high.
This study found that the prevalence of preconception care utilization among the study participants was 40%. Our study findings showed higher utilization of preconception care compared to other community-based studies conducted in Ethiopia (Debre Birhan Town 13.4%, Mekelle City 18.2%, West Guji 22.3%) [15, 21, 22]. It also showed higher utilization of preconception care than studies done in Nigeria by Ekem et al. 10.3% and Adeyemo et al. 18.8% [11, 23], Siri Lanka by Patabendige M. et al. 27.2% [10]. The difference could be due to the different study setting and differences in the sociodemographic characteristics of the study participants. However; it was comparable with findings from China(40%) [8], Malaysia (44%) [9] and Kenya(35.1%) [13].
The most common types of preconception services utilized by the pregnant women was family planning 219 (56.88%) and the least utilized preconception service was vaccination 51(13.2%). This finding is different from a study done Mekelle city in which the most common utilized component of PCC was micronutrient supplementation (i.e., iron, folic acid) [22].
In addition, this study found that pregnant women whose occupation is professional/technical/managerial were 4.3 times more likely to receive preconception care when compared to housewives. This is consistent with the study done in France [24] and Nigeria [23]. This might be because of individuals working at professional/technical/managerial position are more likely to have better knowledge regarding preconception care and might have also better access to information than the housewives.
Awareness and knowledge were significantly associated with the utilization of preconception care in several studies [15, 22, 23, 25]. In this study, 90.9% (350) of the respondents had heard of preconception care. The main source of information was healthcare providers in 62.6% (221/), mass media in 22.7% (80), community in 12.7% (45) and internet 2% [7]. Similarly, 58% (223) of the participants had good knowledge on preconception care. This finding is different from studies done in Ethiopia [15, 18] and Nigeria [25] which showed lower awareness and knowledge about preconception care among pregnant women, which might be due the different study setting and different sociodemographic background of the study population.
In this study, pregnant women who had good knowledge about PCC were 3.5 times more likely to utilize PCC when compared to their counterparts who had poor knowledge about preconception care (AOR = 3.5, 95%CI = 1.92, 6.53, P < 0.000). This finding is consistent with two studies done in Ethiopia, Hosanna Town, which showed 82% reduced odds of utilizing preconception care among women, who had poor knowledge on preconception care than their counterparts [26] and West Guji which also showed 2.43 times odds of utilizing PCC among women having good knowledge compared to their counterparts [15]. Study in Malaysia [9],also showed positive association between good knowledge about preconception care and PCC utilization. This might be because good knowledge about preconception care helps them know about the importance of services. In addition to that, knowledge about PCC might improve attitudes towards PCC, which might in turn improve the utilization of preconception care.
Similarly, pregnant mothers who had an unintended pregnancy were 90% less likely to utilize PCC compared to whose pregnancy were intended and those using family planning before conception were 3.9 times more likely to seek preconception care than mothers who weren’t using family planning before conception. This finding is consistent with studies done in Hosanna Town [26] which showed that the odds of utilizing preconception care in women who had used family planning before current pregnancy were 2.45 times higher than those women who had not used family planning before current pregnancy.
Another study in Los Angeles [17] also showed among women with adverse pregnancy outcomes, having unintended pregnancy was associated with 70% lower odds of not utilizing preconception care. This is because those pregnant mothers who planned their pregnancy are more likely to visit a health facility to seek family planning services, hence, might have broader opportunities to receive preconception counselling services.
Furthermore, pregnant women having preexisting medical disease(s) and adverse pregnancy outcome(s)(s) in previous pregnancy were 8.4 and 3.2 times more likely to utilize PCC than those who had not. These findings are consistent with studies done in Malaysia [9],Los Angeles [17] and Mekelle City [22]. It can be assumed that these patients are more likely to have frequent health facility visits because of their medical conditions, hence, more likely to have adequate information regarding the effect of their medical diseases on pregnancy. In the same line, those pregnant mothers with previous adverse pregnancy outcome(s) are more likely to be concerned and might have heightened risk awareness compared to those who had not.
Moreover, about 75% of the study participants found no problem accessing health facilities. This is similar to studies done in Hosanna Town and West Guji where majority of women found no problem accessing health facilities [15, 26]. In addition, 75.3% of the pregnant women cited the cost of preconception care services as fair.
Lastly, among the pregnant mothers who did not receive PCC services, when asked their reasons for not receiving the care, two-thirds stated, they were not aware that the service was available, one-thirds stated their pregnancy was not expected and about 11.7% thought it was not important to them. This finding is similar to studies done in Los Angeles [17] which found that the common reason for not receiving PCC was not having a pregnancy intended. This shows that even though the awareness and knowledge is good and only few of them had poor attitude toward preconception care, only less than half utilized PCC services. Lack of awareness regarding the availability of the services and having unintended pregnancy could be the plausible explanation for the low utilization of preconception care in this study.
Strength of the study
It is one of the very few studies conducted in Ethiopia in the area of PCC in private setting.
Limitation of the study
Recall bias is a limitation of the study due to the nature of problem under the study requiring the potential ability of respondents to remember information retrospectively.
Selection bias is also a limitation as the study hospitals were chosen by the convenience sampling method.
The impact of husband’s educational attainment on PCC utilization was not included.
Certain components of preconception care, like optimization of psychological health, screening and management of intimate partner violence, and genetic counseling were not studied.
Conclusions
This study found that the utilization of preconception care in the private MCH hospitals is still low i.e., only 40%. Occupation, level of knowledge, having unintended pregnancy, history of family planning use before conception, having adverse pregnancy outcome(s)(s) in previous pregnancy and having pre-existing medical condition(s) were independently associated with preconception care utilization.
Lack of awareness regarding the availability of PCC services and having unintended pregnancy were the obstacles for not receiving PCC.
Recommendations
Health education regarding the importance and the availability of PCC services should be given to women of reproductive age in private MCH hospitals.
Interventions aimed at increasing the proportion of intended pregnancies will also be critical to promote the utilization of preconception care services in these hospitals.
Therefore, health education and providing information in the form of posters and displays about the components and importance of PCC in hospitals could potentially improve utilization of preconception care.
Data Availability
The dataset generated during/or analyzed during the current study are not publicly available due to the papers written using this dataset have not been published but are available from corresponding authors on reasonable request.
Abbreviations
- AA:
-
Addis Ababa
- AKUH:
-
Aga Khan University Hospital
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted Odds Ratio
- BMCH:
-
Betsegah Maternity and Children Hospital
- CI:
-
Confidence Interval
- HBV:
-
Hepatitis B Virus
- HIV:
-
Human Immunodeficiency Virus
- HMCH:
-
Hemen Maternity and Children Hospital
- GA:
-
Gestational Age
- IOM:
-
Institute of Medicine
- MCH:
-
Maternal and Child Health
- MLFH:
-
Maragua Level Four Hospital
- OR:
-
Odds Ratio
- PCC:
-
Preconception Care
- PI:
-
Principal Investigator
- SLE:
-
Systemic Lupus Erythematosus
- SPSS:
-
Statistical Package for Health sciences
- WHO:
-
World Health Organization
References
Center for Desease Control and Prevention. Morbidity and Mortality Weekly Report Recommendations and Reports Recommendations to Improve Preconception Health and Health Care-United States A Report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care Centers for. 2006;55.
Shawe J, Steegers EAP. Preconception Health and Care: A Life Course Approach. Preconception Health and Care: A Life Course Approach. 2020.
USAID. Ethiopia Fact sheet maternal and Child Health. Nurs Midwifery Board Aust. 2019;035(September):1–3.
Why Maternal Mortality Is So. High in Sub-Saharan Africa. [cited 2023 Apr 7]. Available from: https://www.globalcitizen.org/en/content/maternal-mortality-sub-saharan-africa-causes/
Mamo K, Siyoum M, Birhanu A. Teenage pregnancy and associated factors in Ethiopia: a systematic review and meta-analysis. Int J Adolesc Youth. 2021;26(1):501–12. https://doi.org/10.1080/02673843.2021.2010577
Alene M, Yismaw L, Berelie Y, Kassie B, Yeshambel R, Assemie MA. Prevalence and determinants of unintended pregnancy in Ethiopia: A systematic review and meta-analysis of observational studies. PLoS One. 2020;15(4):1–15. https://doi.org/10.1371/journal.pone.0231012
Johnson-mallard V, Kostas-polston EA, Woods NF, Simmonds KE, Alexander IM, Taylor D. Unintended pregnancy: a framework for prevention and options for midlife women in the US. 2017;1–15.
Ding Y, Li X, Xie F, Yang Y. Surv Implement Preconception Care in. 2015;492–500.
Abu Talib R, Idris IB, Sutan R, Ahmad N, Abu Bakar N. Patterns of pre-pregnancy care usage among reproductive age women in kedah, malaysia. Iran J Public Health. 2018;47(11):1694–702.
Patabendige M, Goonewardene IMR. Preconception care received by women attending antenatal clinics at a Teaching Hospital in Southern Sri Lanka. 2013;(March):3–9.
Ekem NN, Lawani LO, Onoh RC, Iyoke CA, Ajah LO, Onwe EO et al. Utilisation of preconception care services and determinants of poor uptake among a cohort of women in Abakaliki Southeast Nigeria. J Obstet Gynaecol (Lahore). 2018;38(6):739–44. https://doi.org/10.1080/01443615.2017.1405922
Ayele AD, Belay HG, Kassa BG, Worke MD. Knowledge and utilisation of preconception care and associated factors among women in Ethiopia: systematic review and meta-analysis. Reprod Health. 2021;18(1):1–15. https://doi.org/10.1186/s12978-021-01132-9
Okemo J, Temmerman M, Mwaniki M, Kamya D. Preconception care among pregnant women in an urban and a rural health facility in Kenya: a quantitative study. Int J Environ Res Public Health. 2020;17(20):1–11.
Goshu YA, Liyeh TM, Simegn Ayele A. Preconception Care utilization and its Associated factors among pregnant women in Adet, North-Western Ethiopia (implication of Reproductive Health). J Women’s Heal Care. 2018;07(05).
Amaje E, Fikrie A, Utura T. Utilization of Preconception Care and its Associated factors among pregnant women of West Guji Zone, Oromia, Ethiopia, 2021: a community-based cross-sectional study. Heal Serv Res Manag Epidemiol. 2022;9:1–10.
Demisse TL, Aliyu SA, Kitila SB, Tafesse TT, Gelaw KA, Zerihun MS. Utilization of preconception care and associated factors among reproductive age group women in Debre Birhan town, North. 2019;1–10.
Batra P, Higgins C, Chao SM. Previous adverse infant outcomes as predictors of Preconception Care Use: an analysis of the 2010 and 2012 Los Angeles Mommy and Baby (LAMB) surveys. Matern Child Health J. 2016;20(6):1177–84.
Ayalew Y, Mulat A, Dile M, Simegn A. Women’s knowledge and associated factors in preconception care in adet, west gojjam, northwest Ethiopia: A community based cross sectional study. Reprod Health. 2017;14(1):1–10. https://doi.org/10.1186/s12978-017-0279-4
Kassa A, Yohannes Z. Women’s knowledge and associated factors on preconception care at Public Health Institution in Hawassa City, South Ethiopia. BMC Res Notes. 2018;11(1):1–6. https://doi.org/10.1186/s13104-018-3951-z
WHO. Meeting to develop a global consensus on preconception care to reduce maternal and childhood mortality and morbidity. WHO Headquarters, Geneva Meet report Geneva …. 2012;78. Available from: http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Meeting+to+Develop+a+Global+Consensus+on+Preconception+Care+to+Reduce+Maternal+and+Childhood+Mortality+and+Morbidity#0%5Cnhttp://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Meeting+t.
Demisse TL, Aliyu SA, Kitila SB, Tafesse TT, Gelaw KA, Zerihun MS, Beebe K, Lee K, Carrieri-Kohlman V, Humphreys J. The effects of childbirth self-efficacy and anxiety during pregnancy on prehospitalization labor.J Obstet Gynecol Neonatal Nurs. 2007;36(5):410–8. 2019;1–10.
Asresu TT, Hailu D, Girmay B, Abrha MW, Weldearegay HG. Mothers’ utilization and associated factors in preconception care in northern Ethiopia: a community based cross sectional study. BMC Pregnancy Childbirth. 2019;19(1):1–7.
Adeyemo AA, Bello OO. Preconception care: What women know, think and do. 2021;20(February):18–26.
Paradis S, Ego A, Bosson JL. Preconception care among low-risk mothers in a French perinatal network: Frequency of utilization and factors associated. J Gynecol Obstet Hum Reprod. 2017;46(7):591–6. https://doi.org/10.1016/j.jogoh.2017.05.002
Ezegwui HU, Dim C, Dim N, Ikeme AC. Preconception care in South Eastern Nigeria. J Obstet Gynaecol (Lahore). 2008;28(8):765–8.
Wegene MA, Gejo NG, Bedecha DY, Kerbo AA, Hagisso SN, Damtew SA. Utilization of preconception care and associated factors in Hosanna Town, Southern Ethiopia. PLoS One. 2022;17(1 January):1–16. https://doi.org/10.1371/journal.pone.0261895
Acknowledgements
We would like acknowledge Addis Ababa University College of health science for allowing us to conduct this study. We would also like to thank the participants and Betsegah and Hemen MCH hospital administrators for their cooperation.
Funding
The authors have no support or funding to report.
Author information
Authors and Affiliations
Contributions
Conceptualization of the study was done A.G with help of A.B and S.K. A.B and S.K played supervision role during the study processes. A.G carried out the investigation and formal analysis of the data with help of A.B. A.G prepared the original draft of manuscript. All the authors contributed in reviewing and editing of the manuscript. All authors have read and agreed on the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by ethical review board of Department of Obstetrics and Gynecology, Addis Ababa University in accordance with Declaration of Helsinki and official letter of permission was obtained from each private Hospital’s administration before data collection. Before participating in the study, the purpose of the study was explained to the study participants and written informed consent was obtained. The collected information was kept confidential through coding. All methods were carried out in accordance with relevant international and local ethical guidelines for research.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Girma, A., Bedada, A. & Kumbi, S. Utilization of preconception care and associated factors among pregnant women attending ANC in private MCH Hospitals in Addis Ababa, Ethiopia. BMC Pregnancy Childbirth 23, 649 (2023). https://doi.org/10.1186/s12884-023-05955-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05955-1