Abstract
Background
This study aims to investigate the risk factors for not returning to postpartum blood pressure (BP) follow-up visit at different time points in postpartum discharged hypertensive disorders of pregnancy (HDP) patients. Likewise, females with HDP in China should have a BP evaluation continuously for at least 42 days postpartum and have BP, urine routine, and lipid and glucose screening for 3 months postpartum.
Methods
This study is a prospective cohort study of postpartum discharged HDP patients. Telephone follow-up was conducted at 6 weeks and 12 weeks postpartum, the maternal demographic characteristics, details of labor and delivery, laboratory test results of patients at admission, and adherence to BP follow-up visits postpartum were collected. While logistic regression analysis was used to analyze the factors associated with not returning to postpartum BP follow-up visit at 6 weeks and 12 weeks after delivery, the receiver operating characteristic (ROC) curve was drawn to evaluate the model’s predictive value for predicting not returning to postpartum BP visit at each follow-up time point.
Results
In this study, 272 females met the inclusion criteria. 66 (24.26%) and 137 (50.37%) patients did not return for postpartum BP visit at 6 and 12 weeks after delivery. A multivariate logistic regression analysis identified education level of high school or below (OR = 3.71; 95% CI = 2.01–6.85; p = 0.000), maximum diastolic BP during pregnancy (OR = 0.97; 95% CI = 0.94–0.99; p = 0.0230)and delivery gestational age (OR = 1.12; 95% CI = 1.005–1.244; p = 0.040)as independent risk factors in predicting not returning to postpartum BP follow-up visit at 6 weeks postpartum, and education level of high school or below (OR = 3.20; 95% CI = 1.805–5.67; p = 0.000), maximum diastolic BP during pregnancy (OR = 0.95; 95% CI = 0.92–0.97; p = 0.000), delivery gestational age (OR = 1.13; 95% CI = 1.04–1.24; p = 0.006) and parity (OR = 1.63; 95% CI = 1.06–2.51; p = 0.026) as risk factors for not returning to postpartum BP follow-up visit at 12 weeks postpartum. The ROC curve analysis indicated that the logistic regression models had a significant predictive value for identify not returning to BP follow-up visit at 6 and 12 weeks postpartum with the area under the curve (AUC) 0.746 and 0.761, respectively.
Conclusion
Attendance at postpartum BP follow-up visit declined with time for postpartum HDP patients after discharge. Education at or below high school, maximum diastolic BP during pregnancy and gestational age at delivery were the common risk factors for not returning for BP follow-up visit at 6 and 12 weeks postpartum in postpartum HDP patients.
Similar content being viewed by others
Introduction
Hypertensive disorders of pregnancy (HDP) represents one of the worldwide leading causes of maternal and perinatal mortality and a major cause of postpartum morbidity, mortality, and readmission [1,2,3,4,5,6,7], accounting for 6.9% of maternal deaths in the United States between 2011 and 2016, and with a high associated cost burden [6, 8−9]. HDP are a group of diseases, including gestational hypertension, preeclampsia, severe preeclampsia, chronic hypertension, chronic hypertension with superimposed preeclampsia, chronic hypertension with superimposed severe preeclampsia, eclampsia, or hemolysis elevated liver enzymes and low platelets (HELLP) syndrome [1–2]. Females that develop HDP are at a 2–4 fold increased risk for chronic hypertension after the pregnancy and a doubling of the risk of cardiovascular disease later in life [10,11,12,13,14].
Postpartum BP monitoring and follow-up after discharge is an essential component of pregnancy care for females with HDP, as most females with HDP are discharged 72 h after delivery [7]. The American College of Obstetricians and Gynecologists (ACOG) has previously recommended that females with HDP should be monitored for BP no later than 3–10 days after delivery and comprehensive postnatal visits and transition to women’s care should be provided 4–12 weeks postpartum, timing individualized and woman-centered [15]. In China, according to Chinese guidelines for the diagnosis and treatment of hypertension and preeclampsia in pregnancy [16, 17], BP should be closely monitored within 72 h after delivery, at least 4 to 6 times a day, and postpartum women with gestational hypertension should regularly monitor their BP and monitor it for at least 42 days. Moreover, all females with HDP should measure BP, and perform other exams, including urine routine, and lipid and glucose screening 3 months postpartum, which should also be followed up for life [16, 17].
Only 52.3–63.0% of the postpartum HDP patients attended a postpartum BP visit around 6 weeks postpartum [18–19], and 24.0–49.0% attended a visit around 12 weeks postpartum [19–20]. It is therefore prudent to identify who will be less likely to monitor BP, so that interventions to increase compliance may be attempted. Then, health care providers may have a better opportunity to early identify the disease and intervene before serious consequences occur. However, to date, the extent of adherence to postpartum BP follow-up and the influence factors in postpartum discharged HDP patients in China remain unclear. The aim of this study was to identify the risk factors that associated with failure to returning for postpartum BP follow-up visit at different time points within 3 months of hospital discharge in postpartum HDP patients.
Methods
Study design, population, and data collection
This prospective cohort study was conducted on postpartum discharged HDP patients at the Affiliated Suzhou Hospital of Nanjing Medical University from September 2017 to December 2019. The ethics committee of the hospital approved this study (K2017037). Postpartum females with HDP were received targeted discharge education. The frequency of BP monitoring, correct home BP monitoring method, and BP goals were provided in discharge education checklist for postpartum females with HDP (see the Supplementary Appendix). Return visits were recommended at 6 and 12 weeks postpartum to monitor and record blood pressure, and for medical personnel to decide whether to adjust the antihypertensive treatment regimen, including dose reduction, discontinuation, dose increase or medication change, and to determine the need for further haematological and biochemical monitoring and management. The value of BP monitoring should be recorded in the blood pressure record book. The record should also include: the date the blood pressure was measured and the specific time the antihypertensive medication was taken (if it was being used).
The inclusion criteria of this study include (1) Patients with HDP as the discharge diagnosis. (2) Postpartum patients. (3) Patients that cooperate with telephone follow-up. The exclusion criteria were: (1) Patients who were not followed up after discharge. (2) Patients with cognitive impairment. (3) Patients with incomplete or missing clinical and laboratory information.
Telephone follow-up was conducted at 6 and 12 weeks postpartum in the discharged females with HDP. Postpartum follow-up information included if they performed a BP monitoring according to the frequency and method in the targeted discharge education, whether return postpartum BP visits were made at 6 and 12 weeks after delivery, whether BP monitored and recorded at the return visit was normal (< 140/90 mmHg), and whether antihypertensive medication was discontinued at the time of the return visit. Meanwhile, the electronic medical records of each patient were reviewed and collected, record data included maternal demographic information, hypertensive diagnosis, combined diagnosis, BP, delivery method, newborn information, and laboratory information relevant to HDP, including urine protein, platelet count (PLT), total bilirubin (TBil), serum creatinine, aspartate aminotransferase (AST), alanine aminotransferase (ALT), lactate dehydrogenase, and uric acid at admission. Then, at each follow-up time point, women with HDP who did not return for postpartum BP visit were compared to women with HDP who did return. The International Classification of Diseases (ICD-10-CM) was used for all the clinical diagnoses.
Statistical analysis
All statistical analyses were performed using the Statistical Package for Social Sciences, version 22 (SPSS Inc. Chicago, IL, United States). The categorical variables are summarized as frequencies and proportions (%), and the Pearson’s chi-square test or the Fisher’s exact test was used to analyze categorical data. In contrast, all the continuous variables were checked for normality using the Kolmogorov-Smirnov test. While the continuous variables were summarized as the medians and interquartile ranges (IQR), the Mann-Whitney U test was used to analyze continuous data when these were not normally distributed. Continuous variables of the normal distribution are summarized as mean ± SD, and a t-test was used to analyze these continuous data. Univariate and multivariate logistic regression analyses were used to explore potential risk factors for not returning to postpartum BP visit at each follow-up time point in discharged patients with HDP, and two-tailed P values of < 0.05 was considered statistically significant. Variates with P values of < 0.1 on the univariate analyses were included in the multivariate logistic regression analysis (backward procedure, based on the p-value of the predictor removed) [21]. A multivariate logistic regression analysis was used to screen for independent risk factors. The odds ratio (OR) and 95% confidence intervals (CI) were also calculated, and the independent risk factor variables were used to establish a logistic regression model and calculate prediction probabilities. While the receiver operating characteristic (ROC) curves of independent risk factors were drawn, the area under the curve (AUC), cut-off point, Youden index, sensitivity, and specificity were used to evaluate their predictive value for predicting not returning to postpartum BP visit at each follow-up time point in discharged patients with HDP [22].
Results
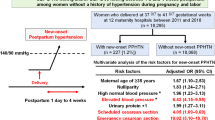
The postpartum discharged HDP patients (n = 272) were enrolled and there were 66 (24.26%) and 137 (50.37%) patients who did not return for postpartum BP visit at 6 and 12 weeks after delivery (Fig. 1). The characteristics of the study population stratified by time point of return postpartum BP visits are shown in Table 1. Women who did not return for postpartum BP visit at 6 and 12 weeks after delivery had significantly lower education levels, more parity, lower diastolic BP at admission, and lower maximum diastolic BP during pregnancy. Moreover, these patients were less likely to have been diagnosed with severe pre-eclampsia, to have given birth at a later median gestational age, and to have higher TBiL levels at admission, with statistically significant differences compared to women who did return. Also, females who did not return for BP visit at 12 weeks postpartum were more likely to be diagnosed with gestational hypertension and less likely to be combined with HELLP syndrome, whereas women who did not return at 6 weeks post-delivery were less likely to be combined with other diagnosis (P < 0.05) (Table 1).
The results of the univariate and multivariable logistic regression indicated that the variables independently associated with not returning to postpartum BP follow-up visit at 6 weeks postpartum were the education level of high school or below (OR = 3.71; 95% CI = 2.01–6.85; p = 0.000), maximum diastolic BP during pregnancy (OR = 0.97; 95% CI = 0.94–0.99; p = 0.0230) and delivery gestational age (OR = 1.12; 95% CI = 1.005–1.244; p = 0.040). Those factors that were independently associated with not returning to postpartum BP follow-up visit at 12 weeks after childbirth included: education level of high school or below (OR = 3.20; 95% CI = 1.805–5.67; p = 0.000), maximum diastolic BP during pregnancy (OR = 0.95; 95% CI = 0.92–0.97; p = 0.000), delivery gestational age (OR = 1.13; 95% CI = 1.04–1.24; p = 0.006) and parity (OR = 1.63; 95% CI = 1.06–2.51; p = 0.026). Education level of high school or below, maximum diastolic BP during pregnancy and delivery gestational age were the common risk factors for not returning to BP follow-up visit at 6 and 12 weeks postpartum (Tables 2 and 3).
The specificity and sensitivity of the resulting logistic regression model were calculated for each independent risk factor of the continuous variables. This was done by constructing ROC curves and calculating the AUC to estimate the models’ ability to identify not returning to BP follow-up visit at 6 and 12 weeks postpartum (Table 4). The area under the ROC curve of the predicted probability of not returning to postpartum BP follow-up at 6 weeks after delivery was 0.746, higher than the other independent risk factors, the Youden index was 0.410, and the sensitivity and specificity were 56.1 and 85.0%, respectively. While the area under the ROC curve of the predicted probability of not returning at 12 weeks postpartum was 0.761, the Youden index was 0.413, and the sensitivity and specificity were 64.2 and 77.0% (Fig. 2). Moreover, the results showed less likelihood to return to postpartum BP visit at 6 weeks after delivery when maximum diastolic BP during pregnancy ≤ 92 mmHg or the delivery gestational age ≥ 36.36 weeks. And when the maximum diastolic BP during pregnancy was ≤ 101 mmHg, the delivery gestational age was ≥ 33.50 weeks or the parity ≥ 2, it was also less likely to return for postpartum BP follow-up visit at 12 weeks postpartum.
(a) ROC curve of the predicted probability for not returning to postpartum BP follow-up visit at 6 weeks after delivery in discharged patients with HDP. The area under the ROC curve of the predicted probability was 0.746 with sensitivity (56.1%) and specificity (85.0%), Youden index 0.410. (b) ROC curve of the predicted probability for not returning to postpartum BP follow-up visit at 12 weeks after delivery in discharged patients with HDP. The area under the ROC curve of the predicted probability was 0.761 with sensitivity (64.2%) and specificity (77.0%), Youden index 0.413
Discussion
In this study, we identified the risk factors associated with failure to return to postpartum BP visit at 6 and 12 weeks after delivery in patients discharged with HDP, respectively. The univariate and multivariate analysis demonstrated that the education level of high school or below, maximum diastolic BP during pregnancy and delivery gestational age were identified as the significant co-variables for not returning to BP follow-up visit at 6 and 12 weeks postpartum in postpartum patients with HDP within 3 months after the discharge from the hospital.
The majority of cases of postpartum strokes and heart failure, which are often complications of hypertensive disease, have been reported to occur within 10–11 days after discharge postpartum [23], and more than 60% of deaths due to gestational hypertensive disease occur during the first 6 weeks postpartum [9]. The recommendations for monitoring hypertension in the postpartum period have started to emerge over the past decades, emphasizing the importance of postpartum follow-up [1–2, 15, 17, 24,25,26]. Therefore, short-interval visits to review BP logs and assess for signs or symptoms of a severe disease after delivery, so that providers can identify and address the disease before it occurs, are essential and practical.
Until now, various studies have identified predictors of 6–week postpartum visit attendance [18,19,20, 27,28,29,30,31,32,33,34]. It is widely recognized that postpartum visit attendance at 6 weeks is lowest among females who are non-Hispanic Black, of ethnic-minority groups, younger, multiparous, unmarried, low-income, have inadequate prenatal care use, publicly insured or uninsured, and vaginal delivery [18,19,20, 27,28,29,30,31,32,33,34]. However, no 12–week postpartum BP follow-up visit predictors have been reported to date. The present study adds to the sparse literature on this topic and reveals new factors affecting the return of postpartum BP follow-up visit. Lower maximum diastolic BP during pregnancy and delivery at a later median gestational age were first identified in our study as common independent risk factors at 6– and 12–week postpartum BP follow-up. Females with lower maximum diastolic BP during pregnancy and later gestational age at delivery indicate a lower severity of their HDP. It intuitively makes sense that women with less severe HDP tend not to pay enough attention to the BP follow-up visit after discharge. The results of the ROC curve analysis showed that the cut-off point of maximum diastolic BP during pregnancy at the 12–week postpartum follow-up time point was higher than that at 6–week time point, and the cut-off point of the delivery gestational age at the 12–week postpartum follow-up time point was lower than the cut-off point at 6–week time point. This suggests that even though the disease is more severe, patients with HDP place less importance on postpartum BP follow-up visit as time progresses, prompting the necessity to identify women who are less likely to return for postpartum BP visit as early as possible, so that better target interventions to improve follow up may be attempted.
The main strengths of the present study are as follows. First, this is the first prospective cohort study to report on the predictors of non-return of postpartum BP follow-up visit at each follow-up time point in postpartum discharged HDP patients and the significant data obtained through regression analysis. Second, the present results are useful for clinical practice. These results are useful to quickly identify patients who may be less likely to return for postpartum BP follow-up visit at each follow-up time point; thus, more targeted discharge education may be attempted for these patients to improve their adherence to postpartum BP follow-up.
There are, however, a few limitations to this study: (1) Our study analyzed risk factors associated with not returning to postpartum BP visit at 6 and 12 weeks after delivery in discharged patients with HDP, but it is possible that not all impact factors were included, such as data on prenatal care utilization, which was unavailable and had been identified as predictors of 6-week postpartum BP follow-up [18,19,20, 27,28,29,30,31,32,33,34,35,36]. (2) There was a population selection bias in our study. It is possible that those who had telephone follow up were also more likely to follow the targeted discharge education, and the region of this study was an eastern and urban area of China where people were more willing to pay more for health expenditures [37], which may also be a potential reason for the high follow-up rate in this study’s patient population. (3) This is a single-center clinical study, the demographic diversity of our cohort was narrow and these findings have limited generalizability to populations that differ demographically or geographically. (4) In this study, follow-up was conducted mainly by telephone, with limited follow-up time and patient cooperation. Therefore, due to the small sample size used, it was not possible to observe the occurrence of cardiovascular events and readmission of patients after discharge.
However, the above does not significantly affect the main results and conclusions of this study, in the future better follow-up methods will be used, such as telehealth technology, to carry out multicenter clinical cohort studies with more impact factors included to analyze and evaluate the risk factors of the adherence to BP monitoring after discharge from the hospital and to assess the long-term outcomes such as hospital readmissions, maternal mortality, and future cardiovascular health in postpartum discharged HDP patients. Reported telehealth technologies for postpartum care include call-center driven BP management [38], combining home BP cuffs with text message reminders for remote postpartum BP monitoring, or providing a Genesis Touch tablet, automatic BP cuff, scale, and pulse oximeter that allow Bluetooth transmission of all home vitals synced on a daily basis to a central monitoring platform for 2–6 weeks [39,40,41]. Data from these pilot studies indicated that remote BP monitoring is fully feasible and acceptable to patients and providers. It results in higher quality-adjusted years, a significant reduction in postpartum readmissions, 3.7% (8/214) versus 0.5% (1/214) [42]. Moreover, the average cost of telehealth was reported to be $309 per patient, and was cost–effective to a cost of $420 per patient. Meanwhile, telehealth could reduce health care costs in the US by approximately $31 million a year. [42].
Conclusion
In our population, there are several risk factors associated with failure to return for BP follow-up visit at 6 and 12 weeks postpartum in discharged females with HDP. Education level at or below high school, maximum diastolic BP during pregnancy and gestational age at delivery were the common risk factors for not returning for BP follow-up visit at 6 and 12 weeks postpartum. These findings not only help to quickly identify patients who may be less likely to adhere to return for postpartum BP visits, but also suggest that we have a long way to go in improving BP follow-up attendance. Given the long-term cardiovascular risk and increased mortality in females with HDP, targeted discharge education of females before discharge to increase adherence to postpartum BP follow-up and visits are fundamental.
Data availability
The data of this study is available from the corresponding authors on reasonable request.
Abbreviations
- ACOG:
-
The American College of Obstetricians and Gynecologists
- ALT:
-
alanine aminotransferase
- AST:
-
aspartate aminotransferase
- AUC:
-
the area under the curve
- BP:
-
blood pressure
- CI:
-
confidence intervals
- HDP:
-
hypertensive disorders of pregnancy
- HELLP:
-
hemolysis elevated liver enzymes and low platelets
- IQR:
-
interquartile ranges
- OR:
-
odds ratio
- PLT:
-
platelet count
- ROC:
-
receiver operating characteristic
- SD:
-
standard deviation
- TBil:
-
total bilirubin.
References
Hypertensive Disorders in Pregnancy Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. Diagnosis and treatment of hypertension and pre-eclampsia in pregnancy: a clinical practice guideline in China. (2020). Chin J Obstet Gynecol. 2020;55(4):227–238.https://doi.org/10.3760/cma.j.cn112141-20200114-00039.
American College of Obstetricians and Gynecologists (ACOG). ACOG practice bulletin no. 202 summary: gestational hypertension and preeclampsia. Obstet Gynecol. 2019;133(1):211–4. https://doi.org/10.1097/AOG.0000000000003019. PMID: 30575668.
Clapp MA, Little SE, Zheng J, Robinson JN. A multi-state analysis of postpartum readmissions in the United States. Am J Obstet Gynecol. 2016;215(1):113e. 1-113.e10.
Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006–2010. Obstet Gynecol. 2015;125(1):5–12. https://doi.org/10.1097/AOG.0000000000000564.
Bernstein PS, Martin JN Jr, Barton JR, et al. National Partnership for maternal safety: Consensus Bundle on severe hypertension during pregnancy and the Postpartum Period. Anesth Analg. 2017;125(2):540–7. https://doi.org/10.1213/ANE.0000000000002304.
Mogos MF, Salemi JL, Spooner KK, McFarlin BL, Salihu HH. Hypertensive disorders of pregnancy and postpartum readmission in the United States: national surveillance of the revolving door J. Hypertens. 2018;36(3):608–18. https://doi.org/10.1097/HJH.0000000000001594.
American College of Obstetricians and Gynecologists. Task force on hypertension in pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol. 2013;122(5):1122–31. https://doi.org/10.1097/01.AOG.0000437382.03963.88.
Stevens W, Shih T, Incerti D, et al. Short-term costs of preeclampsia to the United States health care system. Am J Obstet Gynecol. 2017;217(3):237–248e16. https://doi.org/10.1016/j.ajog.2017.04.032.
Petersen EE, Davis NL, Goodman D, et al. Vital signs: pregnancy-related deaths, United States, 2011–2015, and strategies for Prevention, 13 States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019;68(18):423–9. https://doi.org/10.15585/mmwr.mm6818e1.
Brouwers L, van der Meiden-van Roest AJ, Savelkoul C, et al. Recurrence of pre-eclampsia and the risk of future hypertension and cardiovascular disease: a systematic review and meta-analysis. BJOG. 2018;125(13):1642–54. https://doi.org/10.1111/1471-0528.15394.
Stuart JJ, Tanz LJ, Missmer SA, et al. Hypertensive Disorders of pregnancy and maternal Cardiovascular Disease risk factor development: an Observational Cohort Study. Ann Intern Med. 2018;169(4):224–32. https://doi.org/10.7326/M17-2740.
Fox R, Kitt J, Leeson P, Aye CYL, Lewandowski AJ, Preeclampsia. Risk Factors, Diagnosis, Management, and the Cardiovascular Impact on the Offspring. J Clin Med. 2019;8(10):1625. Published 2019 Oct 4. https://doi.org/10.3390/jcm8101625.
Direkvand-Moghadam A, Khosravi A, Sayehmiri K. Predictive factors for preeclampsia in pregnant women: a receiver operation character approach. Arch Med Sci. 2013;9(4):684–9. https://doi.org/10.5114/aoms.2013.36900.
Wenger NK, Arnold A, Bairey Merz CN, et al. Hypertension across a woman’s life cycle. J Am Coll Cardiol. 2018;71(16):1797–813. https://doi.org/10.1016/j.jacc.2018.02.033.
American College of Obstetricians and Gynecologists (ACOG). ACOG Committee Opinion No. 736: optimizing Postpartum Care. Obstet Gynecol. 2018;131(5):e140–50. https://doi.org/10.1097/AOG.0000000000002633.
Women′s Heart Health Group of Chinese Society of Cardiology of Chinese Medical Association; Hypertension Group of Chinese Society of Cardiology of Chinese Medical Association. Expert consensus on blood pressure management in hypertensive disorders of pregnancy (2019). Chin J Cardiol. 2020;48(3):195–204. https://doi.org/10.3760/cma.j.cn112148-20191024-00652.
Hypertensive Disorders in Pregnancy Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. Chinese expert consensus on blood pressure management during pregnancy. Chin J Obstet Gynecol. 2021;56(11):737–45. https://doi.org/10.3760/cma.j.cn112141-20210506-00251.
Levine LD, Nkonde-Price C, Limaye M, Srinivas SK. Factors associated with postpartum follow-up and persistent hypertension among women with severe preeclampsia. J Perinatol. 2016;36(12):1079–82. https://doi.org/10.1038/jp.2016.137.
Wilcox A, Levi EE, Garrett JM. Predictors of non-attendance to the Postpartum Follow-up visit. Matern Child Health J. 2016;20(Suppl 1):22–7. https://doi.org/10.1007/s10995-016-2184-9.
Thiel de Bocanegra H, Braughton M, Bradsberry M, Howell M, Logan J, Schwarz EB. Racial and ethnic disparities in postpartum care and contraception in California’s Medicaid program. Am J Obstet Gynecol. 2017;217(1):47. https://doi.org/10.1016/j.ajog.2017.02.040.
Hammitt LL, Etyang AO, Morpeth SC, et al. Effect of ten-valent pneumococcal conjugate vaccine on invasive pneumococcal disease and nasopharyngeal carriage in Kenya: a longitudinal surveillance study. Lancet. 2019;393(10186):2146–54. https://doi.org/10.1016/S0140-6736(18)33005-8.
Tang L, Ding XY, Duan LF, et al. A regression model to predict augmented renal clearance in critically ill obstetric patients and Effects on Vancomycin Treatment. Front Pharmacol. 2021;12:622948. https://doi.org/10.3389/fphar.2021.622948.
Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002;186(6):1174–7. https://doi.org/10.1067/mob.2002.123824.
Hypertension in pregnancy: diagnosis and management. London: National Institute for Health and Care Excellence (NICE); June 25, 2019.
Writing Group of 2018 Chinese Guidelines for the Management of Hypertension, Chinese Hypertension League, Chinese Society of Cardiology, Chinese Medical Doctor Association Hypertension Committee, Hypertension Branch of China International Exchange and Promotive Association for Medical and Health Care, Hypertension Branch of Chinese Geriatric Medical Association. 2018 Chinese guidelines for the management of hypertension. Chin J Cardiovasc Med. 2019;24(1):24–56. 10. 3969 / j. issn. 1007–5410. 2019. 01. 002.
Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine. Electronic address: smfm@smfm.org, Gibson KS, Hameed AB. Society for Maternal-Fetal Medicine Special Statement: Checklist for postpartum discharge of women with hypertensive disorders. Am J Obstet Gynecol. 2020;223(4):B18-B21. https://doi.org/10.1016/j.ajog.2020.07.009.
Baldwin MK, Hart KD, Rodriguez MI. Predictors for follow-up among postpartum patients enrolled in a clinical trial. Contraception. 2018;98(3):228–31. https://doi.org/10.1016/j.contraception.2018.04.016.
Rodin D, Silow-Carroll S, Cross-Barnet C, Courtot B, Hill I. Strategies to promote Postpartum visit Attendance among Medicaid participants. J Womens Health (Larchmt). 2019;28(9):1246–53. https://doi.org/10.1089/jwh.2018.7568.
DiBari JN, Yu SM, Chao SM, Lu MC. Use of postpartum care: predictors and barriers. J Pregnancy. 2014;2014:530769. https://doi.org/10.1155/2014/530769.
Battarbee AN, Yee LM. Barriers to Postpartum Follow-Up and glucose tolerance testing in women with gestational diabetes Mellitus. Am J Perinatol. 2018;35(4):354–60. https://doi.org/10.1055/s-0037-1607284.
Bennett WL, Chang HY, Levine DM, et al. Utilization of primary and obstetric care after medically complicated pregnancies: an analysis of medical claims data. J Gen Intern Med. 2014;29(4):636–45. https://doi.org/10.1007/s11606-013-2744-2.
Chen MJ, Hsia JK, Hou MY, Wilson MD, Creinin MD. Comparing Postpartum visit attendance with a scheduled 2- to 3-Week or 6-Week visit after delivery. Am J Perinatol. 2019;36(9):936–42. https://doi.org/10.1055/s-0038-1675623.
Masho SW, Cha S, Karjane N, et al. Correlates of Postpartum visits among Medicaid recipients: an analysis using Claims Data from a Managed Care Organization. J Womens Health (Larchmt). 2018;27(6):836–43. https://doi.org/10.1089/jwh.2016.6137.
Weir S, Posner HE, Zhang J, Willis G, Baxter JD, Clark RE. Predictors of prenatal and postpartum care adequacy in a medicaid managed care population. Womens Health Issues. 2011;21(4):277–85. https://doi.org/10.1016/j.whi.2011.03.001.
Romagano MP, Williams SF, Apuzzio JJ, Sachdev D, Flint M, Gittens-Williams L. Factors associated with attendance at the postpartum blood pressure visit in pregnancies complicated by hypertension. Pregnancy Hypertens. 2020;22:216–9. https://doi.org/10.1016/j.preghy.2020.10.003.
Campbell A, Stanhope KK, Platner M, Joseph NT, Jamieson DJ, Boulet SL. Demographic and clinical predictors of Postpartum Blood pressure screening attendance. J Womens Health (Larchmt). 2022;31(3):347–55. https://doi.org/10.1089/jwh.2021.0161.
Xu X, Wang Q, Li C. The impact of Dependency Burden on Urban Household Health expenditure and its Regional Heterogeneity in China: based on Quantile Regression Method. Front Public Health. 2022;10:876088. https://doi.org/10.3389/fpubh.2022.876088.
Hauspurg A, Lemon LS, Quinn BA, et al. A Postpartum Remote Hypertension Monitoring Protocol implemented at the Hospital Level. Obstet Gynecol. 2019;134(4):685–91. https://doi.org/10.1097/AOG.0000000000003479.
Thomas NA, Drewry A, Racine Passmore S, Assad N, Hoppe KK. Patient perceptions, opinions and satisfaction of telehealth with remote blood pressure monitoring postpartum. BMC Pregnancy Childbirth. 2021;21(1):153. https://doi.org/10.1186/s12884-021-03632-9.
Hoppe KK, Williams M, Thomas N, et al. Telehealth with remote blood pressure monitoring for postpartum hypertension: a prospective single-cohort feasibility study. Pregnancy Hypertens. 2019;15:171–6. https://doi.org/10.1016/j.preghy.2018.12.007.
Rhoads SJ, Serrano CI, Lynch CE, et al. Exploring implementation of m-Health monitoring in Postpartum Women with Hypertension. Telemed J E Health. 2017;23(10):833–41. https://doi.org/10.1089/tmj.2016.0272.
Niu B, Mukhtarova N, Alagoz O, Hoppe K. Cost-effectiveness of telehealth with remote patient monitoring for postpartum hypertension [published online ahead of print, 2021 sep 1]. J Matern Fetal Neonatal Med. 2021;1–7. https://doi.org/10.1080/14767058.2021.1956456.
Acknowledgements
Not applicable.
Funding
This work was supported by the Suzhou Science and Technology Development Program (SS202075); Jiangsu Pharmaceutical Association. Hospital Pharmacy Research Project (H202121). Funders had no influence on the design of the study, the data collection and analysis, and the manuscript writing.
Author information
Authors and Affiliations
Contributions
Design of the study: JJL, LT, YXY; Data aquisition: YXW, LP, LPZ, QZ; Data analysis: JJL, LT, YXW, YXY; Draft the manuscript: JJL, LT, YXW, YXY; Manuscript revise and final version approval: YXY. LT and LP contributed equally to this work. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethic approval and consent to participate
The study was approved by the ethics committee of Suzhou Municipal Hospital (K2017037). Verbal informed consent was obtained by telephone from all participants. All procedures were performed according to the Declaration of Helsinki. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, J., Zhou, Q., Wang, Y. et al. Risk factors associated with attendance at postpartum blood pressure follow-up visit in discharged patients with hypertensive disorders of pregnancy. BMC Pregnancy Childbirth 23, 485 (2023). https://doi.org/10.1186/s12884-023-05780-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05780-6