Abstract
Background
Laparoscopic cholecystectomy at the time of cesarean section is novel in medicine. It is safe, feasible, and cost-effective.
Case presentation
A 29-year-old G3P2 + 0 woman had two previous cesarean sections. She was pregnant at 32 weeks. The fetus had anencephaly. She had acute cholecystitis. Laparoscopic cholecystectomy done at the time of termination of pregnancy by cesarean section.
Conclusions
In a critical period, such as acute cholecystitis, the combination of laparoscopic cholecystectomy immediately post cesarean section is effective if the surgeon is highly qualified and experienced.
Similar content being viewed by others
Background
The second most frequent surgical emergency during pregnancy, behind appendicitis, is acute cholecystitis [1]. Obstetric ultrasonography detects gallstones in 2–4% of pregnant women, while symptomatic cholelithiasis and cholecystitis during pregnancy only happen in 5–10 of every 10,000 gestational women [2]. Concurrent cholecystectomies at the time of cesarean section is cost-effective because it avoids rehospitalization and frequent exposure to anesthesia [2, 3]. Herein, the author reports that a pregnant woman complained of acute cholecystitis, and at the same sitting, she had a laparoscopic cholecystectomy accompanied by a lower segment cesarean section. To the best of our knowledge, this is the second reported laparoscopic cholecystectomy post-cesarean due to acute cholecystitis. Sánchez et al. (2011) described the first combined approach to treating acute cholecystitis [1].
Case presentation
A 29-year-old G3P2 + 0 woman with two previous cesarean sections at 32 weeks of gestation. The woman was informed that the fetus had a congenital anomaly (anencephaly) that wasn’t suitable for life in addition to polyhydramnios. Because of her previous two cesarean sections, she was prepared to terminate her pregnancy via elective cesarean section. Then a woman developed pain in the right upper quadrant and epigastric areas for 24 h. She had nausea and vomiting but no fever or jaundice.
Physical examination refers to a gravid uterus large for dates by 4 weeks. She had tenderness on palpation in the right upper quadrant and epigastric areas referred to the tip of the right shoulder with a positive Murphy’s sign. WBCs were 13,000 nmol/mm3, and normal results from other tests such as amylase, liver, and kidney function tests were found in the laboratory. Abdominal ultrasonography confirmed an anencephalic fetus at 32 ± 1 weeks’ gestation, cholelithiasis and pericholecystic collection, and no biliary tract dilatation.
The symptoms didn’t improve with conservative treatment like hydration, antibiotics, and analgesics for 48 h. So, the decision to perform a laparoscopic cholecystectomy concurrent with an immediate post-cesarian section was taken by an experienced surgeon.
Under general endotracheal intubation, the caesarian section was done first through the previous Pfannenstiel incision. Then comes the transverse hysterotomy incision, pregnancy termination, and repair of the uterine and anterior abdominal wall Pfannenstiel incision (the same as a standard cesarean section) (Fig. 1).
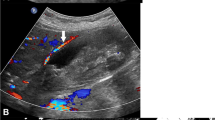
A laparoscopic camera port (10 mm) was inserted just supraumbilical; another port canula was on the right upper quadrant at the midclavicular line (5 mm), the third port was in the epigastric area (10 mm); and the last port was at the right anterior axillary line (5 mm). Pneumoperitoneum was established with CO2 at a pressure of 12 mmHg. The camera video showed an enlarged and congested gallbladder (Fig. 2). Dissection of the gallbladder and ligation of the cystic artery and cystic duct were done in the ordinary way with a metal clip without any difficulty. The gallbladder was placed inside a plastic retrieval bag before its withdrawal from the epigastric port site. The sites of the laparoscopic ports were then closed after we were assured that there was no intraabdominal bleeding. The total operating time was 1 h and 35 min.
Follow-up with the patient involves simply visualizing the amount of vaginal bleeding to detect uterine hemorrhage and frequent blood pressure monitoring by the circulating nurse to detect any non-visualized intraabdominal bleeding. The patient continued on good hydration, analgesics, and Ampicillin-Sulbactam 1.5 g every 12 h for 48 h. The antibiotic Ampicillin-Sulbactam 750 mg film-coated tablet was then started every 8 h for 5 days. The patient was discharged on the third postoperative day with a good outcome. The stitches were removed with clean wounds on the tenth postoperative day.
Discussion and conclusions
Concurrent laparoscopic cholecystectomy with cesarean section is a newly introduced procedure in the surgical field. There are few cases reported in the literature [1, 3,4,5]. However, Mushtaque et al. (2012) reported that 32 pregnant women were subjected to open cholecystectomy post-cesarean Sect [6]. In 2019, Mushtaque et al. reported that eight women were subjected to laparoscopic cholecystectomy at the time of cesarean Sect [2].
In symptomatic gallbladder disease in pregnancy, considering the short duration of pregnancy, patients should be treated conservatively until there is strong evidence of complications such as acute cholecystitis [2, 7]. Laparoscopic surgery seems to be a safe alternative to open surgery during pregnancy and at the time of a cesarean section. It allows the surgeons to operate through small incisions and reduce the risks of surgical infection, blood loss, and incisional hernia [2, 6,7,8].
It is important to secure the repair of the anterior abdominal wall Pfannenstiel incision to prevent the occurrence of parietal emphysema resulting from passage of gases through the incision of the cesarean section. We repaired the abdominal wall in layers used continuous sutures like water tight closure. Also, pneumoperitoneum was established at low pressure 12mmgh.
Pelosi et al. (1999) reported hand-assisted laparoscopic cholecystectomy through the cesarean laparotomy incision, which was left open, and, under direct visual and manual guidance, laparoscopic cannulas were placed [3]. This operative technique needs a pneumo-sleeve system for protection of the laparotomy incision from infection.
We recommend a comparison study between laparoscopic, minilaparotomy, and hand-assisted laparoscopic cholecystectomy immediately post-cesarean section. Laparoscopic cholecystectomy immediately after cesarean section in one sitting is safe, cost-effective, has low morbidity, and keeps the benefit of using minimally invasive techniques.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Weber Sánchez A, García-Benítez CQ, Bravo Torreblanca C, Garteiz Martínez D, Carbo Romano R, Vega Rivera F, Ortiz Reyes H. Colecistectomía laparoscópica poscesárea por hidrocolecisto. Reporte de un caso [case report. Post cesarean section laparoscopic cholecystectomy for hydrocholecystitis]. Ginecol Obstet Mex. 2011;79(4):230–4 (Spanish. PMID: 21966811).
Mushtaque M, Khanday SA, Sheikh J, et al. Laparoscopic cholecystectomy at cesarean section. World J Lap Surg. 2019;12(1):25–8.
Pelosi MA, Pelosi MA 3rd, Villalona E. Hand-assisted laparoscopic cholecystectomy at cesarean section. J Am Assoc Gynecol Laparosc. 1999;6(4):491–5. https://doi.org/10.1016/s1074-3804(99)80017-6. PMID: 10548711.
Pelosi MA 3rd, Pelosi MA, Villalona E. Laparoscopic cholecystectomy at cesarean section. A new surgical option. Surg Laparosc Endosc. 1997;7(5):369–72 PMID: 9348614.
Bernard A, Butler L, Crump S, Meier J. Concurrent cesarean section and hand port-assisted laparoscopic cholecystectomy: a safe approach. Surg Laparosc Endosc Percutan Tech. 2005;15(5):283–4. https://doi.org/10.1097/01.sle.0000183259.78852.a7. PMID: 16215488.
Mushtaque M, Guru IR, Malik TN, Khanday SA. Combined lower segment cesarean section and cholecystectomy in single sitting-our initial experience. J Turk Ger Gynecol Assoc. 2012;13(3):187–90. https://doi.org/10.5152/jtgga.2012.26. PMID: 24592036; PMCID: PMC3939239.
Mendez-Sanchez N, Chavez-Tapia NC, Uribe M. Pregnancy and gallbladder disease. Ann Hepatol. 2006;5(3):227–30 PMID: 17060890.
Nasioudis D, Tsilimigras D, Economopoulos KP. Laparoscopic cholecystectomy during pregnancy: a systematic review of 590 patients. Int J Surg. 2016;27:165–75. https://doi.org/10.1016/j.ijsu.2016.01.070. Epub 2016 Jan 28 PMID: 26826612.
Acknowledgements
None.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
SMA wrote the manuscript, data analysis, interpretation and follow up of the patient. MMZ the surgeon assistant and follow up of the patient.SSF the obstetrics surgeon.ASB the main general surgeon.
Corresponding author
Ethics declarations
Ethical approval and consent to participant
The institutional Ethics committee (Aswan faculty of a medical ethical committee) had reviewed and approved my case report. EC Ref NO: asw 710123.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abdelmohsen, S.M., Zidan, M.M., Fahmy, S.S.E. et al. Post-cesarean section laparoscopic cholecystectomy: a case report. BMC Pregnancy Childbirth 23, 452 (2023). https://doi.org/10.1186/s12884-023-05767-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05767-3