Abstract
Background
Childhood mortality and morbidity has become a major public health issue in low-middle-income countries. However, evidence suggested that Low birth weight(LBW) is one of the most important risk factors for childhood deaths and disability.This study is designed to estimate the prevalence of low birth weight (LBW) in India and to identify maternal correlates associated with LBW.
Methods
Data has been taken from National Family Health Survey 5 (2019–2021) for analysis. 149,279 women belonging to reproductive age group (15–49) year who had last recent most delivery preceding the NFHS-5 survey.
Results
Mother's age, female child, birth interval of less than 24 months, their low educational level, low wealth index, rural residence, lack of insurance coverage, women with low BMI, anaemia, and no ANC visits during pregnancy are predictors that contribute to LBW in India. After adjusting for covariates, smoking and alcohol consupmtion is strongly correlated with LBW.
Conclusion
Mother’s age, educational attainment and socioeconomic status of living has a highly significant with LBW in India. However, consumption of tobacco and cigarrettes are also associated with LBW.
Similar content being viewed by others
Background
The Global public health system continues to face significant obstacles, particularly in low-middle-income countries (LMICs), regarding maternal and child healthcare [1, 2]. One of the main objectives of the Sustainable development goals(SDGs) known as the health goal (goal No. 3) is to "ensure healthy lives and promote well-being for all at all ages," with family planning, information and education, and the inclusion of reproductive health into national strategies and programs being the key targets [3].Low birth weight has become the new public health threat at global level as it is one of the strongest risk factor associated with neonatal mortality and morbidity [4, 5]. LBW contributes 60–80% of neonatal deaths across the globe [6]. According to statistics, more than 20 million infants worldwide in 2015 weighed less than 2500 g at birth, making up at least 15%-20% of all children [7, 8]. The World Health Organization(WHO) has defined Low Birth Weight (LBW) as “a birth weight of less than 2,500 g at the time of birth, regardless of the gestational age” [9, 10]. The newborn must be weighed within the first hour of life before the physiological weight loss begins. Their birth weight determines how vulnerable they are to the risk of childhood illnesses and dying during their early childhood [11]. Preterm birth (28 to 37 weeks) or intrauterine growth restriction (babies that are tiny for gestational age and weigh less than the 10th percentile at mature) can also result in cases of LBW [12].Studies reflect that adolescent pregnancies have adverse effects on both mother and child health [13]. Infants born with LBW are more vulnerable and have higher chances of recurrent hospitalization, neurodevelopmental disorders, chronic morbidities, and under-5 moratalities [14,15,16,17]. Children with LBW are four-fold higher at risk of neonatal death when compared with their counterparts [18].
Studies have shown that LBW is the key predictor for neonate and infant mortality [19]They are more likely to develop congenintal heart anomalies and complications such as sepsis, respiratory distress syndrome and metabolic disturbances [20, 21]. Higher the growth impairment, the higher the risk of childhood death. Conditions such as insulin resistance, dyslipidemia, and high blood pressure are intensely related to LBW, resulting in increased rates of cardiovascular, metabolic and renal diseases and henceforth adult chronic diseases [22]. Research says that children with preterm births and LBW have resulted in developmental disabilities such as cerebral palsy, autism spectrum disorder and learning disability [23]. Also, they are likely to be poor in academic performance during their schooling years [14,15,16,17] Studies conducted in population-attributable-fractions in US populations have included an assessment of the Georgia Pregnancy Risk Assessment Monitoring System that has estimated 42% of Cerebral Palsy (CP) cases and 13% of ID cases were attributable to LBW, an assessment of Autism and Development Disabilities Monitoring Network that estimated 12% of ASD cases are attributable to Pre-term-birth (PTB), LBW and Caesarean delivery [23].
Advancements in medical technologies have enhanced the survival rates of infants with LBW. However, this have also increased the health care costs of bringing up these children [24]. Children with LBW are more susceptible to the length of stay(LOS) in hospitals, especially in the NICU. This creates a financial burden on the payer [25]. Research says that the LOS of the child in NICU depends on the ability of the payer to pay and this determines the discharge of the child [26]. Also, mothers of preterm births have a traumatic experience during LOS of the child in NICU [27]. This resulted in increased rates of stress and anxiety among those mothers as compared to mothers of full-term children [28]. They become emotionally vulnerable and the risk for psychological distress increases. Negative outcomes, such as childhood behavioral and emotional issues and neurodevelopmental delay, are in turn associated with psychological distress, which is characterized in this context as varied degrees of symptoms of depression, anxiety, and perinatal-specific post-traumatic stress [26]. Studies have shown that there is a strong association between maternal stress and LOS of children in the NICU [24].
A report published by UNICEF-WHO on LBW stated the prevalence as 26.4% in Southern Asia which was five times higher than Eastern Asia 5.1% in 2015. Member States of the World Health Assembly (WHA) 65th session employed the goal of a 30% worldwide decline in low birthweight between 2012 and 2025. Reporting on progress continues to be challenging, though. Since 2000, there has been no significant improvement in the rate of LBW babies, especially from 2010 to 2015. Without accelerated preventative measures, we will not be able to reduce LBW by 30% by 2025. Due to unavailability of data, the regional prevalence for India has not been evaluated in that report [29].
According to WHO (2004), prematurity and LBW account for 18.3 million disability-adjusted life years (DALYs) in the South-East Asian Region [30]. In order to measure population health, disability adjusted life years (DALYs), a summary metric, integrate mortality, morbidity, and disability [31]. In order to find accomplishments, unmet requirements, and possibly unanticipated rising risks to population health, this statistic explains the causes and predictors of mortality and morbidity. Studies have explained the ranks of the age-standardized DALYs and the shifts in ranks of various causes and discussed the comparative burden of communicable, maternal, neonatal and nutritional and non-communicable diseases.
Rational for the study
There has not been much studies published on the prevalence of low birth weight in India and there is a dearth of national-level source for birth weight statistics, even though India has the greatest burden of LBW data are available either in birth certificate forms or in hospital discharge data forms. The NFHS of India, equivalent to the Demographic Health Survey (DHS), in its third round (NFHS-3, conducted in 2005–06) collected data on the birth weight of infants by the maternal recall, while asking mothers who had institutional deliveries to show their health cards, where the birth weight of the child is recorded. Similarly, during the NFHS round 5, the birth weight of the child has been recorded.
Several changes have taken place since 2005–06, thereby there is a need for a new study explaining on the current scenario of the country regarding LBW. There is also a need for studies investigating potential factors contributing to the high prevalence of LBW in India. There must be a portal for LBW as soon as the child is born, his weight should be recorded and he should be under supervision up to five years of age to prevent under-5 mortality. Findings from such studies can be used to develop interventions and policies focusing LBW in India.
Objectives
Primary objectives
-
1. To estimate the prevalence of Low birth weight for institutional births in India
Secondary objectives
-
2. To identify the maternal correlates and their association with LBW.
-
3. To determine the association between lifestyle factors such as consumption of alcohol, tobacco, and cigarettes with LBW.
Material and methods
Source of information
This study is based on the data from the National Family Health Survey (NFHS) 5, a nationwide survey to scientifically investigate health and its social determinants and related economics in India. It gives information for 707 disticts, 28 states and 8 union territories. The nationwide data collection spanned from Phase I from 17 June 2019 to 30 January 2020 covering 17 states and 5 UTs and Phase-II from 2 January 2020 to April 2021 covering 11 states and 3 UTs [32].
Study design
India is the world's second-most populous country (1.3 billion population), with 28 states and eight union territories (UTs). Each state and UT are further divided into districts. Districts are subdivided into census enumeration blocks and wards in urban areas and villages/taluks in rural areas. For this dissertation, data collected through the women individual schedules were used to create the dependent and independent variables. As the data had been collected as a part of an observational study, the study design for this research is also similar to a cross-sectional study.
Study population
NFHS 5 gathered information from 636,699 households, 724,115 women, and 101,839 men. Two stages of stratification were used to create the NFHS-5 sample. The sampling frame used to choose the PSUs(Population Sample Units) was the census from 2011. PSUs were Census Enumeration Blocks (CEBs) in urban regions and villages in rural areas. Less than 40-household PSUs were connected to the PSU that was closest to them. Villages were chosen from the sample frame inside each rural stratum with a probability proportionate to size (PPS). Prior to the main survey, a thorough household mapping and listing operation was carried out in each chosen rural and urban PSU. Selected PSUs with at least 300 estimated households were divided into pieces with 100 to 150 households each. The survey used systematic sampling with probability proportional to segment size, and two of the segments were randomly chosen. An NFHS-5 cluster is thus either a PSU or a PSU section. In the second step, 22 homes were randomly chosen using systematic sampling from each chosen rural and urban cluster. Volume II of the national report provides a thorough explanation of sample design, weight computation, standard error estimation, and techniques to improve data quality measurements. In this present study a total of 149,279 women aged 15–59 years were included for the analysis who were interviewed by individual schedule [33], the detailed sample derivation has been given in the Fig. 1.
Inclusion criteria-
-
• The most recent child born in the family, to minimize the possibility of change in several maternal correlates over time.
-
• Children delivered in healthcare institutions in India, to eliminate the imprecision of birth weight taken at home.
-
• Single born child, because multiple births such as twins, and triplets (more than one child in one delivery) have an influence on the birth weight of the children.
Birth weight data were collected from health cards or hospital discharge cards or mother’s self-reported data.
Sampling technique
Villages and census enumeration blocks were chosen from districts in rural and urban areas, respectively, through a two-stage sampling procedure. Data collection was done using CAPI (Computer-assisted personal interview) from June 2019 to April 2021 with an inbuilt schedule and proper maintenance of confidentiality of respondents’ answers. NFHS-5 methodology, including selecting households and data collection procedures, has been meticulously described and published [32].
Study procedure and sample size
A total number of women participants in the entire study design is 724115 out of which only 176843 (24.42%) participants had most recent birth history preceding the survey. Participants who delivered in healthcare facilities 155624 (21.49%) were considered for further analysis. Women who delivered single child 154129 (21.29%) with evidence of numeric birth weight 149279 (20.61%) was the confirmed study population.
Women with previous child birth history 547272 (75.58%), home deliveries 21219 (2.93%), with data of twins 1477(0.95%) and triplets 18 (0.01%) and child not weighted at birth 2714 (1.76%) or don’t know the exact weight 2136 (1.39%) were dropped from the study Fig. 1.
Dependent variable
Children were classified to have LBW if their birth weight was less than 2500 g.
Independent variable
Among the sociodemographic characteristics of mother or family are the mother's age, level of education, wealth index, marital status, religious background, and location of residence. Age of mother, birth order, birth interval, complications during pregnancy, and health behaviours such as smoking and alcohol use were among the reproductive characteristics of the mother. These variables were taken into analysis from the conceptual framework Fig. 2
ANC status comprised the initial ANC visit's timing, the total number of ANC visits, the participant's pregnant tetanus shot, the location of the birth, and service accessibility. ANC status has been divided into three sub-categories namely no ANC visits, ≤ 4 ANC visits and > 4 ANC visits [34].
Among the anthropometric measurements are the mother's body mass index was categorized as “Underweight” (less than 18.5 kg/m2), “Normal” (18.5– 24.9 kg/m2), “Overweight” (25.0–29.9 kg/m2), and “Obese” (≥ 30.0 kg/m2) [35]. Anemia was classified as blood hemoglobin level < 12.0 g/ dL, for nonpregnant women aged 15–49 years, which was further categorized as “mild” (11.0–11.9 g/dL), “moderate” (8.0–10.9 g/dL), and “severe anemia” (< 8.0 g/dL); any anemia was defined as blood hemoglobin level < 11 g/dL,for pregnant women and further categorized as “mild” (10.0–10.9 g/dL), “moderate” (7.0–9.9 g/dL), and “severe anemia” (< 7.0 g/dL) [36].
Data analysis
STATA 16.0 was used to clean and analyse the data (Stata Corp., Texas). For a continuous variable like age, we determined the mean and standard deviation. Additionally, we looked at weighted profiles in both sexes and reported them as percentages and figures [32]. The frequency (n, n%) and p-value of the prevalence of low birth weight among other categorical factors (such as age group, gender, area of residence, educational attainment, life partner, caste, employment status, national region, and wealth index) were shown. A p-value of 0.05 or below was considered statistically significant. We used multivariate logistic regression analysis to further evaluate the statistically relevant factors. The adjusted odds ratio (AOR) with a 95% confidence interval (CI) was used to express the weighted association from regression analysis.
Ethical consideration
This study is based on secondary data obtained from NFHS 5 (2019–21) with no personal identifiers and hence there is no participant risk. The data were requested from International Institute of Population Sciences (IIPS), Mumbai through proper channel and appropriate permission was taken. The same have been properly acknowledged and referenced wherever required.
As a result of literature review, we have identified potential confounders of LBW and its association among different independent variables. We have found that these confounders are also common risk factors of LBW providing were selected and adjusted for it. Variables include place of residence, marital status, birth interval, birth order and alcohol consumption.
Results
After applying the inclusion criteria, the number of participants involved were 149,279 within the age range from 15 to 49 years (Table 1). The mean age of the participants was 27.02 and (± 4.93) years. The majority of the study population belonged to 25–34 years age-group (58.43%), in rural setup (70.19%). However, nearly half of the population was from OBC category (45.62%) and had completed their secondary level of education (53.87%). The Hindu female (80.33%) and women with normal BMI (60.49%) were large in number.
Supplementary: 1 represents the prevalence of LBW infants among the most recent deliveries in healthcare facilities in India by states and its union territories. Nearly, one fifth (17.06%) of the infants had LBW. States like Punjab (21.36%) and Delhi (20.11) had the highest prevalence of LBW followed by Madhya Pradesh (19.47%), Uttar Pradesh (19.20%) and Daman Diu and Dadar and Nagar Haveli (19.07%). Whereas states like Nagaland (3.38%) and Mizoram (3.36%) had the lowest prevalence of LBW.
Figure 3 represents the prevalence of low-birth-weight across Indian states and Union territories. Low prevalence refers to the n% distribution across states i.e., < 5%, 5%-10%, 10%-15%, 15%-20% and > 20%.
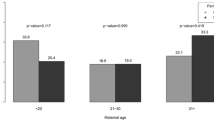
Table 2 represents the prevalence of LBW among different correlates of the mother. Variables such as the age of the mother, gender of the child, birth order, birth interval in months, educational attainment, wealth quintile, caste, place of residence, BMI status, anaemia status, number of ANC visits, iron supplementations and tetanus injection during pregnancy were significantly associated with LBW of infants (P < 0.05). Correlates such as pregnancy complications, caesarean mode of delivery, employment status, and marital status were not significantly associated with our outcome variable. The findings of the chi-square confirmed disparities between the two groups, which were distinguished by the presence or absence of LBW, in terms of the mother's socioeconomic status, educational attainment and caste group.
Among the infants with LBW, women of 15 to 24 years had the highest prevalence of LBW 19.09% (95%CI: 18.74–19.44). Women with higher levels of education (13.20%) had a lower prevalence of LBW as compared to women with no primary education (19.37%). Scheduled caste (18.66%) and scheduled tribe (17.81%) women were considered to be vulnerable to LBW infants. Underweight mothers (21.37%) had higher prevalence for LBW as compared to obese (14.48%) and normal BMI (16.70%) of the mother. Women with pregnancy complications had a 16.87% of LBW prevalence. Mothers with no ANC visits (18.90%), no iron supplementations (18.90%), and no tetanus injections during pregnancy (20.10%) had the highest prevalence among any other variables. However, modifiable lifestyle habits such as consuming cigarettes, tobacco (20.29%) and alcohol (18.77%) are other risk factors associated with LBW.
Supplementary 2 and Table 3 summarize the results of univariate and multivariate logistic regression of various factors associated with LBW among single child born in healthcare facilities of India, based on NFHS-5 (2019–2021). There were twenty-one independent variables, both continuous and categorical (characteristics of interest) out of which sixteen independent variables were significantly associated with LBW.
The univariate regression shows that the age of the mother, gender of the child, place of residence, insurance coverage, BMI status of the mother, wealth index, educational attainment, number of ANC visits, birth order, birth interval, caste, anaemia status, iron supplementation and tetanus injections during pregnancy were significantly associated with LBW (Table 4).
Modifiable lifestyle habits such as the consumption of cigarettes and tobacco and the frequency of alcohol consumption were significantly associated with LBW. Whereas consumption of alcohol (p-value 0.3) was not significantly associated with LBW. However, mother having history of daily alcohol intake had greater chances of delivering LBW infants as compared to occasional drinkers and non-drinkers.
Table 3 shows that women with primary education had higher risk of delivering LBW infant (AOR:1.58 (95% CI: 1.42–1.76)) followed by mothers with no formal education (AOR:1.45 (95% CI: 1.31–1.61)). Mothers belonging to poorest (AOR: 1.22(95% CI: 1.10–1.35)) and poorer (AOR:1.14 (95% CI:1.03–1.25)) wealth quintile had higher odds of delivering LBW child with reference to mothers belonging to richest quintile. Underweight mothers (AOR: 1.35(95% CI:1.19–1.55)) were more likely to have LBW infants keeping obese mothers as reference. With the increase in severity of anaemia, the risk of having LBW infant also increases(AOR: 1.27(95% CI: 1.09–1.46)). As compared to male children, female children (AOR: 1.28 (95% CI: 1.22–1.35) had higher risk of having LBW. Mothers with history of no ANC visits during their last pregnancy (AOR: 1.19(95% CI: 1.08–1.33) had higher chances of having LBW babies.
Table 4 estimates the multivariable logistic regression with LBW as the outcome and cigarettes, tobacco and alcohol consumption as the exposure of interest. Here the outcome variable and exposure variable were adjusted for age of the mother, place of residence, caste group, and health insurance coverage. The adjusted multi- variable model revealed that women using cigarettes and tobacco had a higher risk of delivering low birth weight child (AOR:1.24 (95% CI: 1.12–1.37)) than those who were not using cigarettes and tobacco. It was significantly associated with LBW for the recent most child deliveries (p-value < 0.01), whereas LBW was not significant for women with history of alcohol consumption(p-value 0.473).
Discussion
The aim of the study was to identify potential predictors of low birth weight (LBW) in India, and specifically to investigate how maternal age associated with the likelihood of LBW. The study found that several variables were potentially associated with LBW, including maternal age, the sex of the child, maternal education level, wealth index, religion, insurance coverage, location of residence, maternal body mass index (BMI), anemia status, history of stillbirths, birth spacing, and adequate antenatal care (ANC) visits. The majority of these variables, such as maternal age, education, insurance coverage, BMI, anemia, appropriate birth intervals, and sufficient ANC visits, were identified as modifiable factors that could potentially be improved in order to reduce the risk of LBW..
The results of this study support other studies that show female new-borns have a greater risk of LBW than male neonates. Studies confirmed that this might be caused by female foetuses having greater levels of maternal glucose intolerance, which may have an influence on their birth weight [37, 38].
According to studies, singleton pregnancy women (women giving birth for the first time) were more susceptible than multiparous women (women who have given birth previously) with inadequate birth gaps to have a kid who is LBW. The study's results were consistent with this hypothesis. Further research revealed that moms with birth intervals of less than two years were most likely to produce LBW children than mothers with birth intervals of two or more years. These results supported those of earlier investigations, as well [39,40,41].
Based on the study's findings, mothers with higher educational attainment were less likely to deliver an LBW baby than uneducated mothers. We noticed a dose–response relationship between maternal education level and the likelihood of delivering an LBW infant i.e., the risk of having LBW child decreases with an increase in educational level of mothers. This was in line with the outcomes of other research conducted in India utilizing the NFHS-3 data [5, 30]. In accordance with the findings, babies born to mothers from lower income families (belonging to poorest and poorer wealth quintile) were more likely than babies born to mothers from higher-income families to be born LBW. Women with no education and/or understanding were likely to adapt in unhealthy behaviours (such as smoking, using drugs, tobacco or alcohol, etc.). Additionally, they could not afford access to necessary healthcare resources (such as antenatal care, tetanus injections or iron supplements), which would likely have had an impact on foetal growth. Interventions to raise the educational level of women and young girls were therefore crucial to reducing the prevalence of LBW in India [5]. These results coincided with those of previous studies [5, 42].
Insurance coverage had a crucial role in LBW in India. The National Health Mission (NHM) in India has been working for more than 15 years with the goals of expanding service coverage, maximising equity in the health sectors, and improving health outcomes, while focusing solely on reducing out-of-pocket expenditure (OOPE) and catastrophic health spending (CHS), particularly among the most disadvantaged, deprived, and vulnerable groups. However, no such insurance policies were available that can uptake the financial hardship for LBW child or sick child [43, 44]. Compared to mothers without insurance, those who gave birth to LBW children had a lower likelihood of doing so. Given the conflicting findings of earlier investigations, this was a novel finding of the study. Women with insurance coverage were less likely to deliver an LBW child as compared to those without health insurance. Research done in Arizona revealed that the lack of insurance was significantly associated with increased chances of having an LBW infant, in contrast to a study conducted in Cambodia that found no association between insurance coverage and LBW [41, 45].
Rural mothers had a protective factor of having an LBW baby, which was different from NFHS-3 findings. This outcome might be attributed to better dietary habits and novel prenatal care procedures [46,47,48].
Low micronutrient intake was associated with a low BMI. Foetal development may be hampered by pregnant mothers having low nutritional levels. According to research by Ramana and colleagues, consuming 30% to 50% more protein overall might lower the risk of having a baby that is underweight. Increased low birth weight and infant death were a result of the mother's low BMI. Low birth weight had been more common in moms who were underweight. According to the research, birth weight among the various castes had been associated to rising BMI and maternal weight growth during pregnancy. As per the World Health Organization and United Nations Children's Fund,96% of LBW births, are caused by low socioeconomic situations, poor diet, infections, and physical labour during pregnancy [49,50,51,52].
Evidences has shown that inadequate antenatal care (ANC) visits can have significant implications for the course of pregnancy and the health of new born. Studies have also found a strong association between LBW and inadequate ANC visits during pregnancy, which increases the likelihood of having a baby with LBW [53,54,55]. Notably, the association of mother's education with ANC and delivery care weakened in the NFHS-4 compared to the NFHS-3. After the NRHM was introduced in 2005, there may have been a sharp rise in institutional delivery and ANC care in NFHS-4. Additionally, a major increase in ANC quality over the past ten years may be attributable to a number of NRHM-related programmes, such as the Janani Suraksha Yojana (Safe Motherhood Scheme). Institutional delivery became the societal norm as a result of this growth in maternal health service use, which was especially pronounced among underprivileged groups (IIPS and ICF, 2017) [56].
Less than 5% of the mothers in the current research used cigarettes, compared to more than 50% of the fathers. There is dearth of evidence to suggest that smoking during pregnancy is statistically significantly associated with an increased odds ratio of delivering a low birth weight (LBW) baby. However, Kramer discovered that indoor smoke, cigarette smoking, and tobacco chewing were potentially significant and that their causal influence was proven in his meta-analysis [57]. Based on study findings, consumption of smoking and tobacco were significantly associated with LBW. However, numerous research had revealed a statistically significant association between LBW and cigarette use [58,59,60]. A Taiwan Birth Cohort Study demonstrates a strong association between maternal smoking and LBW and premature birth. 57.3% of the LBW babies in this research were born preterm, and 44% were small for gestational age(SGA). Birth weight was adversely affected by preterm delivery, and intrauterine growth restriction (IUGR) also increases low birth weight (LBW). In utero development and birth weight may be impacted by maternal smoking via the following potential processes. The concentration of nicotine, the key tobacco ingredient, is 15% greater in the placenta than it is in the mother's blood. Nicotine stimulates the release of maternal catecholamines, which constricts the uterus. Additionally, maternal smoking raises the amounts of carboxyhaemoglobin in the umbilical arteries, which causes hypoxia in the featus. Smoking by mothers may have an impact on LBW by lowering leptin levels [61,62,63,64]. The final trimester of pregnancy had the greatest impact on the birth weight of the child, particularly for mothers who smoke heavily (more than 8–10 cigarettes per day) [64,65,66].
Strength and limitations
This study utilized a representative sample of women in India, obtained from nationally representative data, which allowed us to conduct an analysis that is representative of the country as a whole, and to provide a comprehensive understanding of LBW. Recall bias and reporting errors might be associated particularly with the LBW, and other variables, such as age, education level etc.
Conclusion and recommendation
The determinants of LBW in India were evaluated in this study. The study's findings on LBW predictors can be utilised to both pinpoint high-risk individuals and forecast LBW trends. Further research is required to assess the possible causative impact of various indicators detected during pregnancy, such as BMI, anaemia, smoking, alcohol use, history of LBW, and others. The relationship between mothers age and LBW among new born in India was also examined in this study. According to the study findings, adolescent mothers are more likely to deliver children who have LBW. This evidence can inform intervention strategies for healthcare workers, providers, NGOs, policymakers, and public health professionals in India. In addition to that, there is a need of setting up a portal for LBW as soon as the children is born, their weight should be recorded and should be under supervision up to five years of age to prevent under-5 mortality. Similarly, the home-based neonatal care set-ups should be different for LBW child and child with normal weight. Awareness campaign and behaviour change communication strategies need to be revised for LBW child.
Availability of data and materials
All data are publicly available and can be accessed through The DHS Program, https://dhsprogram.com/data/.
References
Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: executive summary. https://apps.who.int/iris/handle/10665/327596. Accessed 11 Feb 2023
Sobhy S, Arroyo-Manzano D, Murugesu N, et al. Maternal and perinatal mortality and complications associated with caesarean section in low-income and middle-income countries: a systematic review and meta-analysis. Lancet. 2019;393:1973–82.
Health - United Nations Sustainable Development. https://www.un.org/sustainabledevelopment/health/. Accessed 11 Feb 2023
Lawn JE, Cousens S, Zupan J. 4 Million neonatal deaths: when? where? why? Lancet. 2005;365:891–900.
Kader M, Perera NKP. Socio-economic and nutritional determinants of low birth weight in India. N Am J Med Sci. 2014;6:302.
World Health Organization (2022) WHO recommendations for care of the preterm or low-birth-weight infant.
United Nations Children’s Fund (UNICEF), World Health Organization. LOW BIRTHWEIGHT ESTIMATES Levels and trends 2000–2015. Lancet Glob Heal. 2019;7:e849–60.
Goyal N, Canning D. The association of in-utero exposure to ambient fine particulate air pollution with low birth weight in India. Environ Res Lett. 2021;16:054034.
Low birthweight - UNICEF DATA. https://data.unicef.org/topic/nutrition/low-birthweight/. Accessed 11 Feb 2023
Wilson PJ. Filcher of good names: an enquiry into anrhropology and gossip. Man. 1974. https://doi.org/10.2307/2800038.
Muchemi OM, Echoka E. Makokha A Factors associated with low birth weight among neonates born at Olkalou district hospital central region Kenya. PAMJ. 2015;20:108. https://doi.org/10.11604/PAMJ.2015.20.108.4831.
Park K 2015 Chapter 9: Demogrphy and Family planning of Park’s Textbook of Preventive and Social Medicine.
de la Calle M, Bartha JL, Lopez CM, Turiel M, Martinez N, Arribas SM, Ramiro-Cortijo D. Younger age in adolescent pregnancies is associated with higher risk of adverse outcomes. Int J Environ Res Public Heal. 2021;18:8514 18:8514.
Groen-Blokhuis MM, Middeldorp CM, Van Beijsterveldt CEM, Boomsma DI. Evidence for a causal association of low birth weight and attention problems. J Am Acad Child Adolesc Psychiatry. 2011;50:1247-1254.e2.
Mccormick MC, Brooks Gunn J, Workman Daniels K, Turner J, Peckham GJ. The health and developmental status of very low-birth-weight children at school age. JAMA. 1992;267:2204–8.
Vohr BR, Wright LL, Dusick AM, et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the national institute of child health and human development neonatal research Network, 1993–1994. Pediatrics. 2000;105:1216–26.
Aureen M, Ack H, Lannery AJF, Ark M, Chluchter S, Ydia L, Artar C, Laine E, Orawski B, Lein AK. Outcomes in young adulthood for very-low-birth-weight infants. N Engl J Med. 2002;346:149–57. https://doi.org/10.1056/NEJMoa010856.
Eshete A, Alemu A, Zerfu TA. Magnitude and risk of dying among low birth weight neonates in Rural Ethiopia: a community-based cross-sectional study. Int J Pediatr (United Kingdom). 2019. https://doi.org/10.1155/2019/9034952.
Alexander GR, Wingate MS, Bader D, Kogan MD. The increasing racial disparity in infant mortality rates: composition and contributors to recent US trends. Am J Obstet Gynecol. 2008;198:51.e1-51.e9.
Apoorva MS, Thomas V, Kiranmai B. A cross sectional study on socio-demographic and maternal factors associated with low birth weight babies among institutional deliveries in a tertiary care hospital, Hyderabad, Telangana. Int J Commun Med Public Heal. 2018;5:4901–4.
Tellapragada C, Eshwara VK, Bhat P, Acharya S, Kamath A, Bhat S, Rao C, Nayak S, Mukhopadhyay C. Risk factors for preterm birth and low birth weight among pregnant Indian women: A hospital-based prospective study. J Prev Med Public Heal. 2016;49:165–75.
Leeson CPM, Kattenhorn M, Morley R, Lucas A, Deanfield JE. Impact of low birth weight and cardiovascular risk factors on endothelial function in early adult life. Circulation. 2001;103:1264–8.
Schieve LA, Tian LH, Rankin K, Kogan MD, Yeargin-Allsopp M, Visser S, Rosenberg D. Population impact of preterm birth and low birth weight on developmental disabilities in US children. Ann Epidemiol. 2016;26:267–74.
Lee HC, Bennett MV, Schulman J. Gould JB (2013) Accounting for variation in length of NICU stay for extremely low birth weight infants. J Perinatol. 2013;3311(33):872–6.
Doyle LW. Economic outcome for intensive care of infants of birthweight 500–999 g born in Victoria in the post surfactant era. J Paediatr Child Health. 1997;33:202–8.
Manktelow B, Draper ES, Field C, Field D. Estimates of length of neonatal stay for very premature babies in the UK. Arch Dis Child - Fetal Neonatal Ed. 2010;95:F288–92.
Jotzo M, Poets CF. Helping parents cope with the trauma of premature birth: an evaluation of a trauma-preventive psychological intervention. Pediatrics. 2005;115:915–9.
Trumello C, Candelori C, Cofini M, Cimino S, Cerniglia L, Paciello M, Babore A. Mothers’ depression, anxiety, and mental representations after preterm birth: A study during the infant’s hospitalization in a neonatal intensive care unit. Front Public Heal. 2018;6:359.
UNICEF-WHO Low birthweight estimates: Levels and trends 2000–2015 | UNICEF. https://www.unicef.org/reports/UNICEF-WHO-low-birthweight-estimates-2019. Accessed 9 May 2023
Belagodu MN, Khachadourian V. Prevalence and predictors of low birth weight in India: Findings from the 2015–2016 National Family Health Survey (NFHS-4). Unpubl. master’s thesis). Armen: Gerald Patricia Turpanjian Sch. Public Heal; 2018.
WHO - The Global Burden of Disease 2004 The global burden of disease 2004. Updat World Heal Organ 146.
James KS, Singh SK, Lhungdim H, Shekhar C, Dwivedi LK, Pedgaonkar S, Arnold F 2022 NFHS-5 2019–20 Report. 1:675.
Family N, Survey H 2019 NFHS-5Womans. 20:.
Ministry of Health and Family Welfare 2010 Antenatal Care and Skilled Attendance at Birth for ANMs/LHVs/SNs. 1–140.
Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today. 2015;50:117–28.
Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity.
Voldner N, Frey Frøslie K, Godang K, Bollerslev J, Henriksen T. Determinants of birth weight in boys and girls. Human Ontogenet. 2009;3:7–12.
Momeni M, Danaei M, Nejad Kermani AJ, Bakhshandeh M, Foroodnia S, Mahmoudabadi Z, Amirzadeh R, Safizadeh H. Prevalence and risk factors of low birth weight in the Southeast of Iran. Int J Prev Med. 2017;8:12.
Shah PS. Parity and low birth weight and preterm birth: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2010;89:862–75.
Halileh S, Abu-Rmeileh N, Watt G, Spencer N, Gordon N. Determinants of birthweight: gender based analysis. Matern Child Health J. 2008;12:606–12.
Chhea C, Ir P, Sopheab H. Low birth weight of institutional births in Cambodia: analysis of the demographic and health surveys 2010–2014. PLoS ONE. 2018;13:e0207021.
Borah M, Agarwalla R. Maternal and socio-demographic determinants of low birth weight (LBW): A community-based study in a rural block of Assam. J Postgrad Med. 2016;62:178.
Mohanty SK, Panda BK, Khan PK, Behera P. Out-of-pocket expenditure and correlates of caesarean births in public and private health centres in India. Soc Sci Med. 2019;224:45–57.
Krishnamoorthy Y, Ganesh K, Sakthivel M, Priyan S, Rehman T, Surendran G. Costs incurred and determinants of out-of-pocket payments for child delivery care in India: Evidence from a nationally representative household survey. Int J Health Plann Manage. 2020;35:e167–77.
Schwartz IL. Low-birth-weight effects of demographic and socioeconomic variables and prenatal care in Pima County, Arizona. West J Med. 1990;152:725–8.
Sutan R, Berkat S. Does cultural practice affects neonatal survival- a case control study among low birth weight babies in Aceh Province, Indonesia. BMC Pregnancy Childbirth. 2014;14:1–13.
Subramanyam MA, Ackerson LK, Subramanian SV. Patterning in Birthweight in India: analysis of maternal recall and health card data. PLoS ONE. 2010;5:e11424.
Mukhopadhyay S, Sarkar A. Pregnancy-related food habits among women of rural Sikkim, India. Public Health Nutr. 2009;12:2317–22.
Sen J, Roy A, Mondal N. Association of maternal nutritional status, body composition and socio-economic variables with low birth weight in India. J Trop Pediatr. 2010;56:254–9.
Upadhyay S, Biccha RP, Sherpa MT, Shrestha S, Panta PP. Association between maternal body mass index and the birth weight of neonates. Nepal Med Coll J. 2011;13:42–5.
Neggers Y, Goldenberg RL. Some thoughts on body mass index, micronutrient intakes and pregnancy outcome. J Nutr. 2003;133:1737S-1740S.
Dubey DK, Nath DC, Dubey DK, Nath DC. An epidemiological model investigating the association between mothers nutritional status and low birth weight in India. Health (Irvine Calif). 2016;8:251–61.
Kristensen P, Keyes KM, Susser E, Corbett K, Mehlum IS, Irgens LM. High birth weight and perinatal mortality among siblings: a register based study in Norway, 1967–2011. PLoS ONE. 2017;12:e0172891.
Doku DT, Neupane S. Survival analysis of the association between antenatal care attendance and neonatal mortality in 57 low- and middle-income countries. Int J Epidemiol. 2017;46:1668–77.
Yaya S, Bishwajit G, Ekholuenetale M, Shah V, Kadio B, Udenigwe O. Timing and adequate attendance of antenatal care visits among women in Ethiopia. PLoS ONE. 2017;12:e0184934.
Khan N, Mozumdar A, Kaur S. Determinants of low birth weight in India: an investigation from the national family health survey. Am J Hum Biol. 2020;32:e23355.
Kramer MS. Determinants of low birth weight: Methodological assessment and meta-analysis. Bull World Health Organ. 1987;65:663–737.
Krisshna K. TOBACCO CHEWING IN PREGNANCY. BJOG An Int J Obstet Gynaecol. 1978;85:726–8.
Monawar Hosain GM, Chatterjee N, Begum A, Saha SC. Factors associated with low birthweight in rural Bangladesh. J Trop Pediatr. 2006;52:87–91.
Deshmukh JS, Motghare DD, Zodpey SP, Wadhva SK. Low birth weight and associated maternal factors in an urban area. Indian Pediatr. 1998;35:33–6.
Mantzoros CS, Varvarigou A, Kaklamani VG, Beratis NG, Flier JS. Effect of birth weight and maternal smoking on cord blood leptin concentrations of full-term and preterm newborns. J Clin Endocrinol Metab. 1997;82:2856–61.
Lambers DS, Clark KE. The maternal and fetal physiologic effects of nicotine. Semin Perinatol. 1996;20:115–26.
Horta BL, Victora CG, Menezes AM, Halpern R, Barros FC. Low birthweight, preterm births and intrauterine growth retardation in relation to maternal smoking. Paediatr Perinat Epidemiol. 1997;11:140–51.
Ko TJ, Tsai LY, Chu LC, Yeh SJ, Leung C, Chen CY, Chou HC, Tsao PN, Chen PC, Hsieh WS. Parental smoking during pregnancy and its association with low birth weight, small for gestational age, and preterm birth offspring: a birth cohort study. Pediatr Neonatol. 2014;55:20–7.
Bernstein IM, Mongeon JA, Badger GJ, Solomon L, Heil SH, Higgins ST. Maternal smoking and its association with birth weight. Obstet Gynecol. 2005;106:986–91.
England LJ, Kendrick JS, Wilson HG, Merritt RK, Gargiullo PM, Zahniser SC. Effects of smoking reduction during pregnancy on the birth weight of term infants. Am J Epidemiol. 2001;154:694–701.
Acknowledgements
We sincerely thank Demographic and Health Surveys (DHS) and the Ministry of Health and Family Welfare (MoHFW) for providing the NFHS-5 dataset
Informed consent
The informed consent was obtained from the participants during the survey.
Funding
No funds were received to conduct the present research.
Author information
Authors and Affiliations
Contributions
TR, SK and SP conceived the study. TR and SK developed the analytical framework. SM, DS and MB performed the analysis, produced results and drafted manuscript. SK monitored analysis and edited manuscript. SP provided overall guidance and supervised the study. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary 1. Distribution of low birth weight among Indian states and its Union Territories of the recent child born in healthcare facilities (NFHS-5). Supplementary 2. Univariate Logistic Regression of maternal correlates with LBW <2500grams as outcome variable among the recent most child delivered in healthcare facilities of India.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Singh, D., Manna, S., Barik, M. et al. Prevalence and correlates of low birth weight in India: findings from national family health survey 5. BMC Pregnancy Childbirth 23, 456 (2023). https://doi.org/10.1186/s12884-023-05726-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05726-y