Abstract
Background
We aimed to evaluate the impact of recommending supplementation to pregnant women with serum ferritin (SF) < 20 µg/L in early pregnancy on use of supplements, and to explore which factors were associated with changes in iron status by different iron indicators to 14 weeks postpartum.
Methods
A multi-ethnic population-based cohort study of 573 pregnant women examined at mean gestational week (GW) 15 (enrolment), at mean GW 28 and at the postpartum visit (mean 14 weeks after delivery). Women with SF < 20 µg/L at enrolment were recommended 30-50 mg iron supplementation and supplement use was assessed at all visits. Change of SF, soluble transferrin receptor and total body iron from enrolment to postpartum were calculated by subtracting the concentrations at the postpartum visit from that at enrolment. Linear and logistic regression analyses were performed to assess associations between use of supplements in GW 28 and changes in iron status and postpartum iron deficiency/anaemia. Change of iron status was categorized into ‘steady low’, ‘improvement’, ‘deterioration’, and ‘steady high’ based on SF status at enrolment and postpartum. Multinomial logistic regression analyses were performed to identify factors associated with change of iron status.
Results
At enrolment, 44% had SF < 20 µg/L. Among these women (78% non-Western European origin), use of supplements increased from 25% (enrolment) to 65% (GW 28). Use of supplements in GW 28 was associated with improved iron levels by all three indicators (p < 0.05) and with haemoglobin concentration (p < 0.001) from enrolment to postpartum, and with lower odds of postpartum iron deficiency by SF and TBI (p < 0.05). Factors positively associated with ‘steady low’ were: use of supplements, postpartum haemorrhage, an unhealthy dietary pattern and South Asian ethnicity (p ≤ 0.01 for all); with ‘deterioration’: postpartum haemorrhage, an unhealthy dietary pattern, primiparity and no use of supplements (p < 0.01 for all), and with ‘improvement’: use of supplements, multiparity and South Asian ethnicity (p < 0.03 for all).
Conclusions
Both supplement use and iron status improved from enrolment to the postpartum visit among women recommended supplementation. Dietary pattern, use of supplements, ethnicity, parity and postpartum haemorrhage were identified as factors associated with change in iron status.
Similar content being viewed by others
Background
Iron is crucial for numerous physiological and cellular processes, and iron deficiency (ID) has diverse health consequences [1]. Persistent ID will lead to depleted iron stores, usually defined by a low serum ferritin (SF) concentration [1], and to iron deficiency anaemia (IDA). Iron needs are tripled during pregnancy due to expansion of maternal red cell mass and growth of the fetus and placenta [2]. ID is associated with maternal fatigue, potentially poorer quality of life, increased risk of postpartum depression, and a higher risk to develop IDA [3]. Gestational anaemia is associated with maternal, perinatal and neonatal mortality, low birth weight and preterm birth [1, 4, 5]. In 2019, the global anaemia prevalence in pregnant women was 36.5%, a slight decrease from 2000 [6], and ID is estimated to account for half of the cases of anaemia [7]. In pregnancy, interpretations of SF values can be hampered by infections, inflammation and pregnancy related changes [3, 8], and soluble transferrin receptor (sTfR) and total body iron (TBI) have been suggested as more valid iron indicators [9, 10].
Iron supplementation programs are implemented in low-income countries to meet the WHO Global Nutrition Target from 2012 to reduce the prevalence of anaemia with 25% by 2025 [7]. There is international consensus to prevent gestational anaemia, and WHO recommends daily or intermittent iron supplementation, depending on the populations’ risk of maternal anaemia [11]. In high-income countries the guidelines differ, some recommend universal supplements from early pregnancy [12], while others recommend supplements only to women with ID or anaemia [5, 13,14,15]. The Norwegian recommendations for antenatal care have changed several times over the last decades. From 1995, women in early pregnancy were recommended to be screened by SF and haemoglobin (Hb) concentration, and iron supplementation was recommended if the SF concentration was below 60 µg/L [16]. In 2005, the guidelines were revised, and recommended to screen women by Hb concentration only, and further to recommend supplementation if anaemia was detected [17]. These were the guidelines during the data collection period of the present study. In 2018 guidelines were revised again, now recommending women to be screened by SF and Hb concentration at their first antenatal visit, and to recommend supplementation if SF concentration is below 70 µg/L [14]. The current guideline aims to prevent gestational and postpartum ID and IDA, and is supported by a Nordic systematic review concluding that 40 mg iron supplementations from gestational week (GW) 18-20 is an effective strategy to prevent ID in more than 90% and IDA in more than 95% of women at delivery and at 6-8 weeks postpartum [1]. How to ensure that women follow the recommendations and increase their use of iron supplements is less clear. Previous studies have shown that maternal age, socioeconomic status, parity, body mass index (BMI) and ethnic origin are factors affecting the use of iron supplements during pregnancy [18, 19].
The STORK-G study included hard-to-reach-women, as all information, material and questionnaires were translated into eight languages, and about 20% of women with non-Western European origin were assisted by professional interpreters. We have previously described the prevalence of gestational and postpartum ID by different indicators and anaemia in our cohort [8, 20]. We found significantly higher prevalence of ID and anaemia at GW 15 in ethnic minority women compared to Western European women [8], while at the postpartum visit the ethnic disparities had almost disappeared [20]. We therefore wanted to assess factors associated with the change in iron status. Women with SF concentration < 20 µg/L at enrolment (GW 15), were provided written information describing their iron status and recommended 30-50 mg iron supplementation. The aims of this paper were therefore (1) to evaluate the impact of this simple recommendation of supplementation to pregnant women with depleted iron stores (SF < 20 µg/L) in early pregnancy on the self-reported use of supplements later in pregnancy in a population with diverse ethnic origin and socioeconomic status, and (2) to explore which factors were associated with changes in iron status by different iron indicators from enrolment to 14 weeks postpartum in women recommended supplementation or not.
Subjects and methods
Study population and data selection
Data from the population-based multi-ethnic STORK-G cohort were collected at public Child Health Clinics for primary antenatal care in three administrative districts in Oslo, Norway between 2008 and 2010. The study methods have been described in detail elsewhere [21]. In short, information, material and questionnaires were translated into Arabic, English, Sorani, Somali, Tamil, Turkish, Urdu and Vietnamese and quality checked by bilingual health professionals. Pregnant women were eligible if they (I) lived in the district, (II) planned to give birth at one of the two study hospitals, (III) were in < 20 GW, (IV) were not suffering from diseases necessitating intensive hospital follow-up during pregnancy, (V) could communicate in Norwegian or any of the eight specified languages and (VI) were able to provide written informed consent.
In total, 823 healthy women were enrolled at mean GW 15 ± standard deviation (SD) 3.4 in this cohort study; referred to as ‘at enrolment’ with planned follow-up visits in GW 28 (GW 28 ± 1.3) and approximately three months after delivery (13.9 ± 2.4 weeks after delivery), referred to as ‘postpartum visit’. Questionnaire data covering a wide range of health issues were collected through interviews by authorized study personnel, assisted by professional interpreters when needed at all three study visits [21]. In addition, clinical measurements were collected according to the study protocol. Participating women were found representative for the main ethnic groups of pregnant women attending the Child Health Clinics [21]. The study protocol and the consent-forms were approved by The Regional Committee for Medical and Health Research Ethics for South Eastern Norway and The Norwegian Data Inspectorate.
Measurements of iron indicators (SF, sTfR and TBI) and Hb
Blood samples were drawn at all visits (2008-2011) [21] and sent the same day for analyses of SF and Hb at the Department of Multidisciplinary Laboratory Medicine and Medical Biochemistry at Akershus University Hospital, Lørenskog, Norway. SF concentration was measured using an electro-chemiluminescence immunoassay (ECLIA) method (Unicel DxI 800 from Beckman Coulter; inter-assay CV < 7%). Hb was measured using an SLS method (XE 5000 from Sysmex; inter-assay CV < 0.7%).
In 2016, sTfR was analysed by ELISA (Modular P800 from Roche; inter-assay CV < 5%), at the Department of Medical Biochemistry at Oslo University Hospital, Oslo, Norway, using biobanked serum samples. We calculated TBI according to Cook [22] from the ratio of sTfR concentration (by Flowers assay) to SF concentration: − [log10 (sTfR × 1000 ÷ SF) − 2.8229] ÷ 0.1207). To convert our Roche sTfR concentration to Flowers sTfR concentrations, we used the conversion equation Flowers sTfR = 1.5 × Roche sTfR + 0.35 mg/L [22].
Recommendation of supplementation
For ethical reasons, and according to the protocol, women with depleted iron stores (SF < 20 µg/L) at enrolment were provided written information describing their SF concentration, recommended to start iron supplementation 30-50 mg/day, and to consult their General Practitioner (GP) for follow-up. At enrolment, in GW 28, and postpartum, all participants were asked about their intake of iron supplements during the past two weeks and to specify the name of the compounds used, and the number of tablets per day and per week. Of those reporting type of iron supplements, 57% used ferrous gluconate, 39% ferrous sulphate, and 4% ferrous fumarate. However, we were only able to calculate the exact iron intake in GW 28 in about 40% of cases. Iron supplementation was therefore dichotomized as ‘no intake’ and ‘intake of iron supplementation’, covering daily or intermittent iron supplement use.
Outcome measures
Our outcome measures were postpartum ID (defined as SF concentration < 15 μg/L, sTfR concentration > 4.4 mg/L or TBI < 0 mg/kg) and anaemia (defined as Hb < 12.0 g/dL), and changes in SF, sTfR, TBI and Hb concentrations, calculated by subtracting the concentrations at the postpartum visit from that at enrolment for each indicator. Further, according to the SF concentration at enrolment the sample was first dichotomized, as either ‘recommended supplements’ (SF < 20 μg/L) or ‘not recommended supplements’ (SF ≥ 20 μg/L). Second, we further categorized women with SF > 20 μg/L into four groups (20-29, 30-49, 50-69, > 70 μg/L). Third, the sample was categorized based on the postpartum iron status (SF < 15 μg/L or ≥ 15 μg/L), resulting in four distinct groups called ‘steady low’, ‘improvement’, ‘deterioration’, and ‘steady high’, reflecting their change in iron status by SF from enrolment to postpartum.
Sociodemographic variables
Maternal age was calculated from date of birth and date at enrolment in the present study. Parity was dichotomized into primiparous (first pregnancy lasting > 22 weeks) and parous (one or more previous births) women. Pre-pregnancy BMI (kg/m2) was calculated from self-reported weight before pregnancy and height measured at enrolment [21]. GW was primarily derived from the first day of the mother’s last menstrual period (LMP), but ultrasound-derived gestational age was used in 7% of pregnancies where there were reasons to believe the LMP-derived gestational age was uncertain [23]. Ethnicity was defined as the participant’s country of birth, or the participant’s mother’s country of birth if the participant’s mother was born outside Europe or North America [21], and grouped as Western Europeans (Norway, other Western European countries and North America), South Asians (primarily Pakistan and Sri Lanka), Middle Easterners (primarily Iraq, Morocco, and Turkey), East Asians (includes East- and South-East Asian countries, primarily Vietnam and The Philippines), Sub-Saharan Africans (primarily Somalia) and Eastern Europeans (primarily Poland, Kosovo, and Russia). Maternal present socioeconomic position (SEP) was a score derived from a principal component analysis (PCA) of 11 different demographic variables [24]. The variables contributing most to the score were individual level data about education, occupational class and employment status, and household variables as own or renting tenure and rooms per person in the household. The score was standard normally distributed, with a higher score reflecting higher SEP.
Variables potentially associated with iron metabolism
From questions about the women’s medical history, we categorized three groups; (I) no medical conditions associated with anaemia or ID, (II) self-reported chronic illness or medication associated with ID or normochromic, and (III) self-reported chronic illness or medication associated with ID or hypochromic anaemia [8]. Data from a food frequency questionnaire, developed to capture dietary patterns in a multi-ethnic sample, were collected in GW 28. Four clusters were extracted using the Ward’s method [25]. Clusters were referred to as ‘a healthier dietary pattern’ vs. three ‘less healthy dietary patterns’ [25], here dichotomized into ‘healthy’ and ‘unhealthy’. The ‘healthy dietary pattern’ represented more frequent intake of fruit, vegetables, wholegrain bread with pate and meat spread, and meat, i.e. food items representing relatively high iron content (heme and non-heme) and foods rich in vitamin C which again improves the bioavailability of iron compared to the other dietary pattern. After conducting sensitivity analyses excluding women with possible inflammation (elevated C-reactive protein (CRP)) in our previous published papers [8, 20], we found only minor changes in the mean and median values and in the prevalence of ID and anaemia across ethnic groups and concluded that inflammation did not explain the differences observed in our population. We therefore chose not to adjust SF, sTfR or TBI values for CRP to correct for inflammation, as suggested by some others [26,27,28].
Birth-related variables potentially associated with postpartum iron status
We have detailed data on birth complications extracted from hospital birth records. Delivery mode was categorized as normal vaginal delivery, instrumental vaginal delivery (i.e. forceps or vacuum assisted vaginal delivery), elective caesarean section and emergency caesarean section. Blood loss after delivery was dichotomized into < 500 mL and ≥ 500 mL, where the latter was defined as postpartum haemorrhage. We constructed a composite index for birth complications reflecting the presence of at least one of the following complications; episiotomy, third- or fourth-degree perineal tear, obstructed labour and manual removal of placenta, due to small numbers in each of the categories.
Sample size
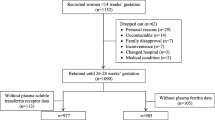
Of the 823 women enrolled in mean GW 15, 644 (78%) women gave birth to a live and singleton baby and attended the postpartum visit. For this study, we included participants with values for SF from both visits, resulting in a total sample of 573 women (Flow chart, Additional file 1, Figure S1). There were no significant differences between the study sample and the 250 excluded women for age, parity, pre-pregnant BMI, and SEP (data not shown). However, the study sample consisted of a slightly larger proportion of ethnic minority women compared to the excluded women, as they were prioritised for fasting blood samples at the postpartum visit due to resource limitations [20].
Statistical analyses
Descriptive statistics are presented as frequencies with proportions for categorical variables and mean with SD or medians with interquartile range for continuous variables. The sTfR and TBI values were approximately normally distributed, and SF skewed to the left. Difference in SF from enrolment to postpartum within the five SF categories at enrolment was assessed by Wilcoxon signed rank test.
We performed multinomial logistic regression analyses to investigate factors associated with belonging to one of the following three groups ‘steady low’, ‘improvement’ and ‘deterioration’, reflecting the women’s iron status at enrolment and postpartum, using ‘steady high’ as the reference. Both unadjusted and adjusted odds ratios (OR) are presented. GW, age, parity, SEP, diet, ethnicity, use of iron supplementation in GW 28 and postpartum, postpartum haemorrhage and birth complications were included in the fully adjusted model.
Furthermore, we stratified the cohort in two subsamples based on whether the women were recommended use of iron supplements at enrolment or not. In each stratum, we performed two sets of regression analyses. Linear regression analyses were performed to assess the association between self-reported use of iron supplementation in GW 28 and changes in SF, sTfR, TBI, and Hb concentrations from enrolment to the postpartum visit. Logistic regression analyses were performed when postpartum ID (defined by SF, sTfR and TBI) and anaemia were the outcome. Adjustments were made for GW, age, parity, SEP, diet, ethnicity, and use of iron supplements in pregnancy. In addition, SF concentration at enrolment was included to reduce dilution of regression to the mean. In a final model we also adjusted for use of supplements postpartum, postpartum haemorrhage, and birth complications although these were not true confounders, but potentially strongly associated with the outcome. The estimates changed marginally by including the last covariates. Results are presented as β-coefficients and ORs with accompanied 95% confidence intervals (CI). SPSS version 28 and Stata version 16 were used for statistical analysis.
Results
At enrolment (mean GW 15.1 (SD ± 3.4), maternal age was 29.7 ± 4.8 years, pre-pregnant BMI was 24.6 ± 4.8 kg/m2, 45% were primiparous and 62% had ethnic origin from countries outside Western Europe (Table 1). Iron supplementation was recommended to 252 (44%) women with depleted iron status (SF < 20 µg/L) at enrolment in early pregnancy, of whom 204 (78%) were of non-Western European origin.
From enrolment in early pregnancy to GW 28, the reported use of iron supplementation increased from 25 to 65% in women recommended supplements, and from 13 to 26% in the group not exposed to our recommendations. Further, the proportion of women reporting use of iron supplements at GW 28 was higher (68%) in the group with ‘improvement’ in iron status from enrolment in early pregnancy to postpartum (mean postpartum week 13.9 (SD ± 2.5), compared to the group with ‘steady low’ iron status (55%). It was also higher in women with ‘steady high’ (29%) compared to the group with ‘deterioration’ (15%) in iron status (Table 1).
The effect of supplemental use
The change in SF concentration from enrolment in early pregnancy to the postpartum visit, stratified into five groups by SF concentration at enrolment, is illustrated in Fig. 1. A moderate increase in median SF concentration was observed in women recommended iron supplementation (p < 0.001), while a reduction was seen in all other groups (p < 0.001 in all). As a consequence, the prevalence of postpartum ID by SF (defined as SF < 15 µg/L) was approximately 40% in all groups, except in women with SF concentration ≥ 70 µg/L at enrolment (24%) (Additional file 2, Table S1). The prevalence of postpartum ID in the group recommended iron supplementation (SF < 20 μg/L at enrolment) was 44% by SF, 25% by sTfR and 28% by TBI, while 31% had postpartum anaemia (Additional file 2, Table S1). The change in SF from enrolment in early pregnancy to the postpartum visit shown in Fig. 1 were similar across the largest ethnic groups (data not shown).
Change in serum ferritin concentration from enrolment in early pregnancy to postpartum in participants with different value at enrolment 1. 1 Data from the STORK-G multi-ethnic pregnancy cohort from Oslo, Norway, 2008-2010. The group with SF < 20 μg/L (depleted iron stores) at enrolment, were recommended supplementation. Enrolment mean gestational week 15.1 ± standard deviation 3.4. Postpartum visit mean postpartum week 13.9 ± 2.4. SF, serum ferritin
Results from the multinomial logistic analysis showed that compared to ‘steady high’ iron status by SF, use of supplements in GW 28 was positively associated with having ‘steady low’ (OR 2.7, 95% CI 1.5-4.8, p < 0.001), but even more strongly with ‘improvement’ (OR 5.2, 95% CI 3.0-9.0, p < 0.001) in iron status by SF, while negatively associated with having ‘deterioration’ in iron status by SF (OR 0.3, 95% CI 0.2-0.6, p < 0.001) (Table 2).
The stratified linear and logistic regression analyses showed that use of iron supplements in GW 28 was associated with improvement in iron status from enrolment in early pregnancy to 14 weeks postpartum by SF, sTfR, TBI, and in Hb concentration (p < 0.05—0.001) (Table 3). Use of supplements were associated with lower odds of postpartum ID by SF and TBI (p < 0.05—0.001) both in women exposed to recommendations and not. However, supplement use in iron depleted women (SF < 20 µg/L at enrolment) was not significantly associated with lower odds of postpartum ID by sTfR, and supplement use was in neither groups significantly associated with lower odds of postpartum anaemia (Table 3). Both SF change and TBI change were consistently associated with supplementation use.
Factors associated with change in iron status
In addition to no use of supplements, an unhealthy dietary pattern (ORs 4.0 and 2.8, p < 0.01) and postpartum haemorrhage (ORs 5.4 and 4.7, p ≤ 0.01) were associated with higher odds of having ‘steady low’ and ‘deterioration’ of iron status by SF (Table 2). Primiparity was associated with lower odds of ‘improvement’ (OR 0.5, p = 0.03) and higher odds of ‘deterioration’ (OR 2.7, p < 0.01) in iron status by SF. Further, South Asian ethnic origin was associated with having high odds of ‘improvement’ in iron status by SF, but higher odds of having ‘steady low’’ in iron status by SF (ORs 2.7 and 3.7, p<0.02) (Table 2).
Discussion
Main findings
In this cohort, iron supplementation was recommended to 44% of the pregnant women due to depleted iron status (SF concentration < 20 µg/L) at enrolment in mean GW 15, of whom the majority (78%) were of non-Western European origin. In the group recommended supplementation, the use of iron supplements increased from 25% at enrolment to 65% at the postpartum visit. Further, in women recommended supplements, median SF concentration increased from 11 to 16 µg/L, while the median SF concentration was substantially reduced in women not exposed to our recommendations. Use of iron supplements in GW 28 was associated with lower odds of ‘deterioration’ and higher odds of ‘improvement’ in iron status by SF, and with lower odds of postpartum ID by SF and TBI, both in women recommended iron supplement and those not exposed to our recommendations. Use of supplements in GW 28 did however not reduce the odds of postpartum anaemia or postpartum ID by sTfR in women with depleted iron stores (SF concentration < 20 µg/L) at enrolment. Primiparity, unhealthy dietary pattern and postpartum haemorrhage were independently associated with ‘steady low’ and ‘deterioration’ in iron status by SF. South Asian ethnic origin was associated with higher odds of both ‘steady low’ and ‘improvement’ of iron status by SF.
This study confirms the widespread prevalence of depleted iron stores in pregnancy and the early postpartum period [29]. Even though the prevalence of gestational anaemia in the total sample was low (5.9%) in a global context [8], as many as 89% had SF < 70 µg/L at enrolment, and would be recommended supplementation according to current Norwegian antenatal guidelines, implemented after this study was performed. We found that women not exposed to our recommendations showed a more adverse iron status development, and that women having SF between 20-70 µg/L at enrolment had a high prevalence of postpartum ID supports the current guidelines [14].
In our multi-ethnic cohort, we observed that 65% of the women recommended supplementation seemed to follow our recommendations and reported use in GW 28, and the median SF and the mean TBI concentration in this group increased from enrolment to 14 weeks postpartum. The compliance in randomized, controlled trials (RCT’s) has been reported to be around 85-90% [29,30,31], however strict follow-ups to encourage and ensure compliance might not reflect real-life settings. Previous studies have found a higher proportion of ID in populations with low socioeconomic status [32] and that pregnant women with ethnic minority background are less likely to follow recommendations regarding supplemental use [18]. Despite our recommendations, the proportion of postpartum ID in women recommended supplementation in our study was still high (33% by SF < 12 µg/L and 44% by SF < 15 µg/L). This is higher than observed in two RCT’s with low-dose iron supplementations, where the prevalence of ID (SF < 15 µg/L) 2-6 months after delivery was 7-16% in the intervention and 29% in the placebo group [29, 30]. Moreover, in an US cross-sectional study, 13% had ID (SF < 12 µg/L) 0-6 months after delivery [33]. There may be several reasons for such discrepancies. Our study was population-based, and it is well-known that participants in RCTs often are highly selected and motivated for the intervention. Furthermore, our cohort consists of many women from ethnic minority- and hard-to-reach groups, and we observed significant ethnic differences in iron status, including Hb levels at enrolment [8]. However, at the postpartum visit, only women of South Asian origin had significantly higher sTfR and lower Hb concentration [20] compared to Western Europeans, suggesting that the simple intervention recommending supplementation to iron depleted women, of whom 78% were ethnic minority women, had an effect on decreasing ethnic differences. The effects of iron supplements on change in SF from enrolment to the postpartum visit showed in Fig. 1 were similar across the largest ethnic groups (data not shown), indicating that these are universal effects.
In line with others, we found that use of supplements reduced the risk of postpartum ID and that women reporting use of iron supplements were more likely to improve their iron status by SF and mean Hb concentration in the postpartum period [1, 5]. We also found that supplementation was associated with improvements of iron status in mean sTfR and TBI. Nevertheless, while use of supplements in GW 28 was strongly associated with postpartum ID by TBI, it did not reduce the odds of postpartum anaemia, nor of postpartum ID by sTfR, in women with depleted iron stores (SF concentration < 20 µg/L) at enrolment. This could possibly suggest that TBI is a better indicator of the effect of supplementation use on ID. However, the test is more expensive, which restricts its general availability, and more data on its use in pregnancy are needed. Furthermore, SF in pregnancy is affected by haemodilution. We can hence not rule out the possibility that some of the increase in SF from enrolment to postpartum in women with depleted iron stores at baseline could be related to changes in blood volume. However, the observed decrease in SF observed in women that were not exposed to our recommendations, does not support this. Further, sTfR and TBI, which are less affected by pregnancy-related factors, show similar pattern, which suggests that changes in iron status measured by SF cannot be explained by pregnancy related changes such as haemodilution alone. Although associated with higher Hb concentration postpartum, use of supplements was in our cohort not associated with reduced risk of anaemia. A study from Burkina Faso, Africa, in a population with a high rate of anaemia while unknown iron status, found that iron supplementation was only associated with increasing Hb from early to late pregnancy if the woman was anaemic [34]. We did not have statistical power to evaluate the effect of iron supplements stratified by anaemia status, as few women were anaemic at enrolment (5.9%). Further, we were primarily interested in change in iron status by different iron indicators, and factors associated with such change.
In high-income countries, haemorrhage is recognized as the most important factor associated with postpartum ID and anaemia [1]. Our study supports that it is important to offer women with haemorrhage a postpartum follow-up to assess iron status. In line with others we found that primiparity appears to be an important factor associated with an adverse iron status development [35], also after adjusting for birth complications, haemorrhage, ethnicity and supplement use. This might suggest that there may be other, unidentified factors related to primiparous pregnancies that could affect the need for iron. We have previously reported significant ethnic differences in crude ID and anaemia prevalence. The prevalence of anaemia ranged from 7-14% in early pregnancy in women with ethnic origin outside Europe [8] and 26-40% postpartum [20]. Wheras in Europeans the prevalence was lower, both in early pregnancy (0-1.8%) [8] and postpartum (14-18%) [20]. Recent studies from the UK found a high proportion of women from ethnic minority groups to be anaemic during pregnancy, and also that severe anaemia was associated with adverse foetal and infant outcomes (stillbirth, perinatal death, small for gestational age infants, low birth weight infants and maternal postpartum haemorrhage [36]), highlighting the importance of preventing anaemia and identifying vulnerable groups, e.g. minority women, which could need extra attention. On the other hand, no existing evidence indicates that preventive iron supplementation has an effect on birth weight or other adverse infant outcomes [37]. In our study, 65% of women with South Asian ethnic origin had depleted iron stores at enrolment and were recommended supplementation. Many of these women benefitted from the simple intervention, having higher odds for being in the ‘improvement’ group, but some did not and developed postpartum ID (‘steady low’ group). This could suggest that language skills and cultural factors not accounted for in our study may also play a role in the compliance to our recommendations. Another possible explanation could be that this ethnic group have a diet richer of phytates, which inhibits iron uptake [38]. Therefore, clinicians should strive to increase the compliance in order to ensure improvement of iron status, prevent anaemia and to prevent associated adverse maternal and neonates outcome [5, 32, 36].
Strength and limitations
The major strength of our multi-ethnic population-based study is that we followed a large number of healthy women from enrolment in early pregnancy to 14 weeks postpartum with measurements of iron status by three different indicators, analysed at the same laboratories. We collected a broad high-quality data set, which enabled us to explore relations between iron status and a wide range of explanatory factors, and to adjust for a range of possible confounders. The questionnaires were translated to eight languages and data collection methods were adapted to facilitate enrolment of ethnic minorities and even illiterate women, who often are excluded in research [21]. Professional interpreters were used to ensure the quality of the interview-administrated questionnaire data. The women were found representative for the main ethnic groups of Oslo. Lastly, this study represents close-to-practice research, addressing the gap between what works in research (RCT) and what works in practice, especially in hard-to-reach-groups.
However, there are also weaknesses to report. We evaluated the impact of giving a simple recommendation of iron supplementation by self-reported use of supplements in GW 28 through a pre-post-test design, not a RCT. We do not know to which extent the women adhered to our recommendations. However, substantially more women reported use of iron supplements in GW 28 among women undergoing this ‘simple intervention’, compared to those not exposed to recommendation, suggesting an effect. In Norway ferrous gluconate, sulphate and fumarate can be bought in grocery stores or pharmacies without prescription. For the majority of women we lack information of the iron dose taken, the frequency and duration of intake, the type of iron supplements as well as of other variables affecting the iron uptake. We assessed the effect of recommending iron supplementation on the women's postpartum status only, and have not evaluated the effect of iron supplementation on the neonates. Further, the number of participants in some ethnic groups was low, and the presence of heterogeneity within relatively broad ethnic groups is possible. As in most studies, we had some loss to follow-up at the postpartum visit, partly due to logistic reasons, but we prioritized ethnic minority women for blood sampling. Further, the collected food-frequency data were used to identify dietary patterns, and we were therefore not able to calculate iron intake. Postpartum haemorrhage was not exactly measured, but based on clinical judgement. On average, the plasma volume increases from about 2.4 L to about 2.8 L from the time before pregnancy to week 19 [39], and we cannot rule out that plasma volume can partly explain some of the differences found during pregnancy. There are no simple biomarkers that provide good estimates of changes in plasma volume [40, 41], however we adjusted for gestational week in our regression models, as a proxy for plasma volume. Furthermore, we have no reason to believe that our explanatory variables of interest will systematically influence the blood volume, and hence affect our results, other than by reducing the precision of our estimates.
Implications
First, our results lend support to recommend iron supplementation to women during pregnancy to prevent gestational and postpartum ID and anaemia, and indicate that there is a need for an enhanced focus on iron supplementation during pregnancy to be incorporated in high risk groups in antenatal care. Further, our findings also suggest that postpartum ID or IDA needs to be addressed, and postpartum counselling that includes measurement of Hb and SF concentrations are required in high-risk women. In addition, as prophylactic iron supplementation during pregnancy is still a subject of international disagreement, further research to examine the effect on ID and IDA in pregnant women should be undertaken.
Conclusion
We evaluated the impact of recommending supplements to pregnant women with depleted iron stores, including women in hard-to-reach-groups, and observed an increase of use of supplements and improved iron status from at enrolment to the postpartum visit. Women not exposed to our recommendations, showed a deteriorated iron status postpartum. Further, factors associated with change in iron status were dietary iron intake, use of iron supplements, ethnicity, parity and postpartum haemorrhage.
Availability of data and materials
The editors can access data in de-identified form used in the manuscript, code book, and analytical code upon request. The project manager Anja Brænd, and co-author Line Sletner, will contribute to the access being provided under appropriate conditions. However, research data for this publication include identifying health information subject to confidentiality. It is therefore not possible to share raw data.
Abbreviations
- BMI:
-
Body mass index
- CRP:
-
C-reactive protein
- CV:
-
Coefficient of variation
- CI:
-
Confidence interval
- ECLIA :
-
Electro-chemiluminescence immunoassay
- HbA1c:
-
Glycated haemoglobin
- Hb:
-
Haemoglobin
- ID:
-
Iron deficiency
- IDA:
-
Iron deficiency anaemia
- PCA:
-
Principal component analysis
- OR:
-
Odds ratio
- SF:
-
Serum ferritin
- SEP:
-
Socioeconomic position
- SD:
-
Standard deviation
- sTfR:
-
Soluble transferrin receptor
- TBI:
-
Total body iron
- WHO:
-
World Health Organization
References
Domellöf M, Thorsdottir I, Thorstensen K. Health effects of different dietary iron intakes: a systematic literature review for the 5th Nordic Nutrition Recommendations. Food Nutr Res. 2013;57:1. https://doi.org/10.3402/fnr.v57i0.21667.
Bothwell TH. Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutr. 2000;72(1 Suppl):257S-264S.
Nutritional anaemias: tools for effective prevention and control. Geneva: World Health Organization; 2017.
Lopez A, Cacoub P, Macdougall IC, Peyrin-Biroulet L. Iron deficiency anaemia. Lancet. 2016;387(10021):907–16.
Pavord S, Daru J, Prasannan N, Robinson S, Stanworth S, Girling J, Committee BSH. UK guidelines on the management of iron deficiency in pregnancy. Br J Haematol. 2020;188(6):819–30.
WHO Global Anaemia estimates. The global health observatory (GHO): World Health Organization, 2021 Edition.
Global nutrition targets 2025: anaemia policy brief (2014). WHO reference number: WHO/NMH/NHD/14.4. Geneva: World Health Organization; 2014.
Naess-Andresen ML, Eggemoen AR, Berg JP, Falk RS, Jenum AK. Serum ferritin, soluble transferrin receptor, and total body iron for the detection of iron deficiency in early pregnancy: a multiethnic population-based study with low use of iron supplements. Am J Clin Nutr. 2019;109(3):566–75.
Mei Z, Cogswell ME, Looker AC, Pfeiffer CM, Cusick SE, Lacher DA, Grummer-Strawn LM. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999–2006. Am J Clin Nutr. 2011;93(6):1312–20.
Pfeiffer CM, Looker AC. Laboratory methodologies for indicators of iron status: strengths, limitations, and analytical challenges. Am J Clin Nutr. 2017;106(Suppl 6):1606s–14s.
Developing and validating an iron and folic acid supplementation indicator for tracking progress towards global nutrition monitoring framework targets. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO.
Sundhedsstyrelsen: Anbefalinger for svangreomsorgen. [Maternity Guidelines]. [https://www.sst.dk/-/media/Udgivelser/2021/Anbefalinger-svangreomsorgen/Anbefalinger-for-svangreomsorgen.ashx?sc_lang=da&hash=E4195822AAB3A79AAC1F10969B8695AD]
Läkemedelsverket. Sjukdomar under graviditet; Anemi. In. 2018/2019; Läkemedelsboken. [The Swedish Medical Products Agency]. [https://lakemedelsboken.se/kapitel/gynekologi/sjukdomar_och_lakemedel_under_graviditet_och_amning.html#i1-2_25]
Helsedirektoratet. Nasjonal faglig retningslinje for svangerskapsomsorgen. [Maternity Guidelines]. Oslo: Helsedirektoratet; 2018
Geimeinsamer Bundesausschuss. Mutterschafts-Richtlinien. [Maternity Guidelines]. [https://www.g-ba.de/downloads/62-492-2676/Mu-RL_2021-09-16_iK-2022-01-01.pdf]
Helsedirektoratet. Veileder i svangerskapsomsorg for kommunehelsetjenesten. [Maternity Guidelines]. Statens helsetilsyn; 1995.
Helsedirektoratet. Retningslinjer for svangerskapsomsorgen (IS-1179). [Maternity Guidelines]. Sosial- og helsedirektoratet; 2005.
Bärebring L, Mullally D, Glantz A, Elllis J, Hulthén L, Jagner Å, Bullarbo M, Winkvist A, Augustin H. Sociodemographic factors associated with dietary supplement use in early pregnancy in a Swedish cohort. Br J Nutr. 2018;119(1):90–5.
Haugen M, Brantsaeter AL, Alexander J, Meltzer HM. Dietary supplements contribute substantially to the total nutrient intake in pregnant Norwegian women. Ann Nutr Metab. 2008;52(4):272–80.
Næss-Andresen M, Jenum A, Berg J, Falk R, Sletner L. Prevalence of postpartum anaemia and iron deficiency by serum ferritin, soluble transferrin receptor and total body iron, and associations with ethnicity and clinical factors: A Norwegian population-based cohort study. J Nutr Sci. 2022;11:e46.
Jenum AK, Sletner L, Voldner N, Vangen S, Morkrid K, Andersen LF, Nakstad B, Skrivarhaug T, Rognerud-Jensen OH, Roald B, et al. The STORK Groruddalen research programme: A population-based cohort study of gestational diabetes, physical activity, and obesity in pregnancy in a multiethnic population. Rationale, methods, study population, and participation rates. Scandinavian J Public Health. 2010;38(5 Suppl):60–70.
Cook JD, Flowers CH, Skikne BS. The quantitative assessment of body iron. Blood. 2003;101(9):3359–64.
Sletner L, Nakstad B, Yajnik CS, Morkrid K, Vangen S, Vardal MH, Holme IM, Birkeland KI, Jenum AK. Ethnic differences in neonatal body composition in a multi-ethnic population and the impact of parental factors: a population-based cohort study. PLoS ONE. 2013;8(8):e73058.
Sletner L, Jenum AK, Morkrid K, Vangen S, Holme IM, Birkeland KI, Nakstad B. Maternal life course socio-economic position and offspring body composition at birth in a multi-ethnic population. Paediatr Perinat Epidemiol. 2014;28(5):445–54.
Sommer C, Sletner L, Jenum AK, Mørkrid K, Andersen LF, Birkeland KI, Mosdøl A. Ethnic differences in maternal dietary patterns are largely explained by socio-economic score and integration score: a population-based study. Food Nutr Res. 2013;57:1. https://doi.org/10.3402/fnr.v57i0.21164.
Rohner F, Namaste SM, Larson LM, Addo OY, Mei Z, Suchdev PS, Williams AM, SakrAshour FA, Rawat R, Raiten DJ, et al. Adjusting soluble transferrin receptor concentrations for inflammation: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am J Clin Nutr. 2017;106(Suppl 1):372S-382S.
Namaste SM, Rohner F, Huang J, Bhushan NL, Flores-Ayala R, Kupka R, Mei Z, Rawat R, Williams AM, Raiten DJ, et al. Adjusting ferritin concentrations for inflammation: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am J Clin Nutr. 2017;106(Suppl 1):359S-371S.
Mei Z, Namaste SM, Serdula M, Suchdev PS, Rohner F, Flores-Ayala R, Addo OY, Raiten DJ. Adjusting total body iron for inflammation: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am J Clin Nutr. 2017;106(Suppl 1):383S-389S.
Makrides M, Crowther CA, Gibson RA, Gibson RS, Skeaff CM. Efficacy and tolerability of low-dose iron supplements during pregnancy: a randomized controlled trial. Am J Clin Nutr. 2003;78(1):145–53.
Milman N, Bergholt T, Eriksen L, Byg KE, Graudal N, Pedersen P, Hertz J. Iron prophylaxis during pregnancy–how much iron is needed? A randomized dose–response study of 20–80 mg ferrous iron daily in pregnant women. Acta Obstet Gynecol Scand. 2005;84(3):238–47.
Sandstad B, Borch-Iohnsen B, Andersen GM, Dahl-Jorgensen B, Froysa I, Leslie C, Aas MH, Eig TR, Sandem SO. Selective iron supplementation based on serum ferritin values early in pregnancy: are the Norwegian recommendations satisfactory? Acta Obstet Gynecol Scand. 2003;82(6):537–42.
Auerbach M, Georgieff MK. Guidelines for iron deficiency in pregnancy: hope abounds: Commentary to accompany: UK guidelines on the management of iron deficiency in pregnancy. Br J Haematol. 2020;188(6):814–6.
Bodnar LM, Cogswell ME, McDonald T. Have we forgotten the significance of postpartum iron deficiency? Am J Obstet Gynecol. 2005;193(1):36–44.
Roberfroid D, Huybregts L, Habicht JP, Lanou H, Henry MC, Meda N, d’Alessandro U, Kolsteren P, Group MS. Randomized controlled trial of 2 prenatal iron supplements: is there a dose-response relation with maternal hemoglobin? Am J Clin Nutr. 2011;93(5):1012–8.
Milman N. Postpartum anemia I: definition, prevalence, causes, and consequences. Ann Hematol. 2011;90(11):1247–53.
Nair M, Churchill D, Robinson S, Nelson-Piercy C, Stanworth SJ, Knight M. Association between maternal haemoglobin and stillbirth: a cohort study among a multi-ethnic population in England. Br J Haematol. 2017;179(5):829–37.
Pena-Rosas J, Viteri F. Effects and safety of preventive oral iron or iron folic acid supplementation for women during pregnancy (Review). Cochrane Database Syst Rev. 2009;4:CD004736.
Brunvand L, Henriksen C, Larsson M, Sandberg A-S. Iron deficiency among pregnant Pakistanis in Norway and the content of phytic acid in their diet. Acta Obstet Gynecol Scand. 1995;74(7):520–5.
de Haas S, Ghossein-Doha C, van Kuijk SM, van Drongelen J, Spaanderman ME. Physiological adaptation of maternal plasma volume during pregnancy: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2017;49(2):177–87.
Lobigs LM, Sottas PE, Bourdon PC, Nikolovski Z, El-Gingo M, Varamenti E, Peeling P, Dawson B, Schumacher YO. The use of biomarkers to describe plasma-, red cell-, and blood volume from a simple blood test. Am J Hematol. 2017;92(1):62–7.
Vricella LK. Emerging understanding and measurement of plasma volume expansion in pregnancy. Am J Clin Nutr. 2017;106(Suppl 6):1620s–5s.
Acknowledgements
We thank the midwives and research staff at the Grorud, Bjerke, and Stovner Child Health clinics and the women who participated in the STORK-G study. We would also like to thank the two laboratories: the Department of Multidisciplinary Laboratory Medicine and Medical Biochemistry in Akershus University Hospital, and the Department of Medical Biochemistry at Oslo University Hospital who performed the analyses of the blood samples.
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital). MNA received funding from The Norwegian Research Fund for General Practice. The data collection was supported by the Norwegian Research Council, the Southern and Eastern Norway Regional Health Authority, the Norwegian Directorate of Health, and collaborative partners in the Stovner, Grorud, and Bjerke administrative districts of the city of Oslo.
Author information
Authors and Affiliations
Contributions
MNA and LS had full access to all data in this study. MNA is responsible for the integrity of data and accuracy of the data analysis. MNA, LS, JPB, and AKJ revised the study concept and design, contributed to analysis and tables. RSF guided the statistical analysis and revised the tables. All authors interpreted the data, and critical revision of the manuscript. AKJ initiated the STORK-G study and was the principal investigator until 2021. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was started after approval from The Regional Ethics Committee, Oslo (Norway). The Regional Ethics Committee (2007/894) and the Norwegian Data Inspectorate (25 October 2007; 07/01355–2/MOF) approved the study protocol. All participants provided written informed consent. The study was carried out according to the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Flow chart of study participants in the STORK-G multi-ethnic cohort from Oslo 2008-2010.
Additional file 2. Table S1.
Average SF, sTfR, TBI and Hb concentration in early pregnancy and postpartum, and prevalence of postpartum iron deficiency/anaemia.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Næss-Andresen, ML., Jenum, A.K., Berg, J.P. et al. The impact of recommending iron supplements to women with depleted iron stores in early pregnancy on use of supplements, and factors associated with changes in iron status from early pregnancy to postpartum in a multi-ethnic population-based cohort. BMC Pregnancy Childbirth 23, 350 (2023). https://doi.org/10.1186/s12884-023-05668-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05668-5