Abstract
Background
The prevalence of preterm birth has been rising, and there is a paucity of nationwide data on the perinatal characteristics and neonatal outcomes of twin deliveries of very preterm infants (VPIs) in China. This study compared the perinatal characteristics and outcomes of singletons and twins admitted to neonatal intensive care units (NICUs) in China.
Methods
The study population comprised all infants born before 32 weeks in the Chinese Neonatal Network (CHNN) between January 2019 and December 2019. Three-level and population-average generalized estimating equation (GEE)/alternating logistic regression (ALR) models were used to determine the association of twins with neonatal morbidities and the use of NICU resources.
Results
During the study period, there were 6634 (71.2%) singletons and 2680 (28.8%) twins, with mean birth weights of 1333.70 g and 1294.63 g, respectively. Twins were significantly more likely to be delivered by caesarean section (p < 0.01), have antenatal steroid usage (p = 0.048), have been conceived by assisted reproductive technology (ART) (p < 0.01), have a higher prevalence of maternal diabetes (p < 0.01) and be inborn (p < 0.01) than singletons. In addition, twins had a lower prevalence of small for gestational age, maternal hypertension, and primigravida mothers than singletons (all p < 0.01). After adjusting for potential confounders, twins had higher mortality rates (adjusted odds ratio [AOR] 1.28, 95% confidence interval [CI] 1.10–1.49), higher incidences of short-term composite outcomes (AOR 1.28, 95% CI 1.09–1.50), respiratory distress syndrome (RDS) (AOR 1.30, 95% CI 1.12–1.50), and bronchopulmonary dysplasia (BPD) (AOR 1.10, 95% CI 1.01–1.21), more surfactant usage (AOR 1.22, 95% CI 1.05–1.41) and prolonged hospital stays (adjusted mean ratio 1.03, 95% CI 1.00–1.06), compared to singletons.
Conclusion
Our work suggests that twins have a greater risk of mortality, a higher incidence of RDS and BPD, more surfactant usage, and longer NICU stays than singletons among VPIs in China.
Similar content being viewed by others
Background
Over the past decade, the rate of very preterm twins has been increasing worldwide mainly due to the development of assisted reproductive technology (ART) and increased maternal childbearing age [1,2,3,4,5,6,7]. Data from the Australian and New Zealand Neonatal Network showed that the incidence of twins in extremely preterm infants increased from 21.6% in 1995–1999 to 25.6% in 2005–2009 [5]. Studies have revealed controversial findings regarding the neonatal outcomes of multiple pregnancies. Some studies have reported an increased risk of infant mortality and morbidity associated with twin pregnancies [4, 5, 7,8,9]. In contrast, other studies did not reveal such differences in multiples compared with singletons [10, 11]. There is a lack of data on the morbidity and mortality of preterm multiples compared with singletons in China, which is important for counselling and decision-making in obstetric practice.
The Chinese Neonatal Network (CHNN) was founded in 2018 and comprises 58 major tertiary hospitals from 25 provinces across China [12]. The purpose of this study was to explore the perinatal characteristics and neonatal outcomes for twins compared with singletons among VPIs in China.
Methods
Data source
This was a retrospective analysis of a prospectively collected cohort study of neonates delivered at < 32 weeks gestation from the CHNN. The CHNN is a collaborative network of 58 major tertiary hospitals providing care management for high-risk neonates, including four national children’s medical centres, four regional children’s medical centres, thirty provincial perinatal or children’s medical centres and nineteen major referral centers in large cities in China. Among them, one hospital was excluded due to incomplete data, and ultimately 57 hospitals collecting full-year data on VPIs admitted to the neonatal unit in 2019 were included in this study. These hospitals accounted for approximately 5% of all VPIs in China. These hospitals included all government-designated neonatal centres of excellence in China. The median number of neonatal intensive care unit (NICU) beds was 40 (interquartile range [IQR], 30–62), and the median number of intermediate-level and continuing care neonatal beds was 66 (IQR, 40–91). For perinatal centres, the median number of annual deliveries was 10 280 (IQR, 6273–15 423). The median number of full-time equivalent neonatologists was 19 (IQR, 12–27), and the median number of NICU nurses was 42 (IQR, 30–65). The CHNN maintains a standardized clinical database to monitor the outcomes and care practices of NICUs in Chinese tertiary hospitals [12].
Trained abstractors prospectively collected data from NICU electronic medical records using a standard manual of variable definitions. A customized database with built-in error checking was applied during data entry. Data were later electronically submitted to the CHNN coordinating centre in the Children’s Hospital of Fudan University with patient anonymity. The accuracy of the data collection was monitored by investigators, and rigorous quality control procedures were performed at each site [13].
Study population
All infants in our study were delivered at less than 32 weeks gestation and admitted to CHNN hospitals from January 2019 to December 2019. Infants with major congenital anomalies, chromosomal defects, and those from multiple pregnancies other than twin pregnancies were excluded. The study population was grouped by plurality (singletons, twins). Readmissions and transfers between participating hospitals were recorded as data from the same infants. Data from infants who were stillborn, died in the delivery room, or were transferred to nonparticipating hospitals within 24 h after birth were not recorded in the database.
Outcomes and definitions
The primary outcome was a composite of mortality or any severe neonatal morbidity and short-term composite outcomes. Severe neonatal morbidity was defined as necrotizing enterocolitis (NEC) ≥ stage 2, bronchopulmonary dysplasia (BPD), severe neurological injury (severe intraventricular haemorrhage [IVH] and cystic periventricular leukomalacia [cPVL]), severe retinopathy of prematurity (ROP), or sepsis. Necrotizing enterocolitis (NEC) was defined according to Bell’s criteria [14, 15]. BPD was defined as a requirement for respiratory support at 36 weeks postmenstrual age or at discharge/transfer/death if before 36 weeks postmenstrual age [16]. Severe IVH was defined as grade 3 or 4 IVH according to Papile’s criteria [17]. cPVL was defined as the presence of periventricular cysts on cranial ultrasound or MRI. Severe ROP was defined as grade 3 or 4 ROP according to the international classification of ROP [18]. Sepsis was defined as a positive blood or cerebrospinal fluid culture and antibiotic therapy or the intent of providing antibiotic therapy for ≥ 3 days [19]. Short-term composite outcomes included early death and neonatal respiratory distress syndrome (RDS). Early death was defined as death occurring less than 7 days after birth. RDS was defined according to a combination of clinical signs and symptoms, laboratory analysis and chest X-ray (CXR) [20]. In addition, the secondary outcome was the use of NICU resources, including the length of NICU stay, surfactant use, breastfeeding, exclusive breastfeeding, and the duration of invasive ventilation. Breastfeeding was defined as an infant receiving their mother’s own milk, independent of the addition of formula or other foods and/or drinks. Exclusive breastfeeding was defined as an infant receiving no foods or drinks other than their mother’s own milk.
Definitions of other covariates
Gestational age (GA) was recorded using the hierarchy of the best obstetric estimate based on prenatal ultrasound, menstrual history, obstetric examination, or all three. If the obstetric estimate was not available or was different from the postnatal estimate of gestation by more than two weeks, gestational age was estimated using the Ballard Score [21]. Small for gestational age (SGA) was defined as a birth weight < 10th percentile for the gestational age according to the Chinese neonatal birth weight values [22]. Prenatal care was defined as ≥ 1 pregnancy-related hospital visit during pregnancy. ART was defined as the use of hormonal therapy, artificial insemination, or any method of in vitro fertilization.
Ethics approval
The conduction of this study was approved by the ethics committee of the Children’s Hospital of Fudan University (Identifier: 2018–296) and recognized by all participating NICUs for the development, compilation, data transfer, hosting, and analysis of the CHNN dataset. Individual consent for this retrospective analysis was waived in all 57 tertiary-level NICUs because this study did not directly intervene in the diagnosis and treatment of individual patients. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Statistical analysis
Perinatal characteristics and neonatal outcomes of singletons and twins were described by descriptive statistics. We also reported the means [standard deviations (SDs)] or medians [interquartile ranges (IQRs)] for continuous variables depending on normality. Chi-square tests, Student’s t tests or Mann‒Whitney U tests were applied to compare infants and maternal characteristics between singletons and twins as appropriate.
Three-level and population-average generalized estimating equation (GEE)/alternating logistic regression (ALR) models were used to determine the association of twins with neonatal morbidities and the use of NICU resources [23,24,25,26]. Adjusted odds ratios were reported after controlling for level-1 infant characteristics (gestational age, sex, SGA, birthplace) and level-2 maternal information (maternal age, antenatal steroid usage, hypertension, diabetes, c-section, ART, primigravida status). To account for the level-3 NICU cluster effect, an exchangeable correlation matrix was used in the multiple GEE/ALR regressions. Stratified analysis was carried out between infants with a GA < 28 weeks and those with a GA of 28–31 weeks to assess whether GA modified the impact of twins on neonatal morbidity and the use of NICU resources. All statistical analyses with data management were conducted by SAS version 9.4. The significance level of all hypothesis tests was 0.05 with a two-sided test.
Results
Study population
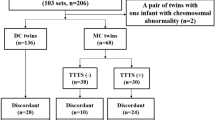
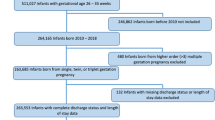
During the study period, 9552 infants were admitted to 57 neonatal intensive care units (NICUs). Among them, 78 infants had congenital anomalies or chromosomal defects, 160 infants were from higher-order multiple pregnancies (triplets and quadruplets), and 9314 infants met the inclusion criteria (6634 singletons (71.2%) and 2680 twins (28.8%)) (Fig. 1). Among them, 302 infants died after active medical treatments in the NICU, 61 infants died after palliative care, and 780 infants were discharged against medical advice. The median (IQR) gestational age for twins was lower than that of singletons, with a median of 29.7 (28.1, 31.0) weeks of GA for twins and 30.0 (28.4, 31.0) weeks of GA for singletons (P < 0.01). Moreover, the mean (SD) birth weight for twins was lower than that of singletons, with a mean of 1294.63 (313.99) g for twins and 1333.70 (323.21) g for singletons. There were 3832 male infants (57.9%) from singleton pregnancies and 1439 male infants (53.7%) from twin pregnancies.
Basic perinatal characteristics
Twins were significantly more likely to have received ART (39.5% vs. 7.3%, p < 0.01), were born to mothers with diabetes (19.7% vs. 16.1%, p < 0.01), had antenatal steroid usage (77.0% vs. 74.9%, p = 0.048), were delivered by caesarean delivery (C-section) (59.6% vs. 52.5%, p < 0.01), and were inborn (66.4% vs. 62.6%, p < 0.01) than singletons. In addition, twins had a lower prevalence of small for gestational age (6.2% vs. 8.3%, p < 0.01), maternal hypertension (10.3% vs. 22.3%, p < 0.01) and primigravida mothers (46.2% vs. 53.0%, p < 0.01) than singletons. There were no significant differences in prenatal visits > 1 and Apgar scores < 7 at 5 min between these two groups (Table 1).
Neonatal outcomes and NICU treatment
The NICU mortality rate was 14.1% for twins and 11.5% for singletons. Twins had higher overall incidences of composite outcomes (49.4% vs. 47.2%, p = 0.046) and short-term composite outcomes than singletons (74.4% vs. 68.3%, p < 0.01). Twins had significantly higher incidences of mortality (14.1% vs. 11.5%, p < 0.01), severe intraventricular haemorrhage (IVH) (8.9% vs. 7.4%, p = 0.02) and RDS (72.8% vs. 66.2%, p < 0.01) than singletons. However, there were no significant differences in NEC ≥ Stage II, BPD, severe neurological injury, cPVL, severe ROP, sepsis, or early death between these two groups (Table 2).
Twins were more likely to have surfactant usage (singletons, 48.3%; twins, 55.5%) and be breastfed (singletons, 48.3%; twins, 55.5%) than singletons (P < 0.01). However, there were no differences in the length of NICU stay [median (IQR) for singletons, 45(33, 59); twins, 46(34, 60)], exclusive breastfeeding (singletons, 17.3%; twins, 17.2%) or the duration of invasive ventilation [median (IQR) for singletons, 4.5(2, 10); twins, 5(2, 11)] between the twin and singleton groups (Table 3).
Impact of twin births on study outcomes
After adjusting for potential confounders, overall, twins had higher odds of short-term composite outcomes (adjusted odds ratio [OR] 1.28, 95% confidence interval [CI] 1.09–1.50), RDS (adjusted OR 1.30, 95% CI 1.12–1.50), mortality (adjusted OR 1.28, 95% CI 1.10–1.49), and BPD (adjusted OR 1.10, 95% CI 1.01–1.21) than singletons. There were no significant differences between singletons and twins in the incidences of NEC ≥ Stage II, severe neurological injury, severe ROP, or early death (Table 4).
Analysis of the use of NICU resources showed that, after adjusting for potential confounders, twins had a higher incidence of surfactant usage (adjusted OR 1.22, 95% CI 1.05–1.41) and longer NICU stay (adjusted mean ratio 1.03, 95% CI 1.00–1.06) than singletons. However, there were no significant differences in breastfeeding, exclusive breastfeeding, or the duration of invasive ventilation between twins and singletons (Table 5).
Discussion
Principal findings
This study was a national-level comprehensive assessment of care practices and health outcomes of 9314 VPIs admitted to 57 Chinese tertiary NICUs from January 2019 to December 2019. It served to fill a gap in our knowledge of Chinese neonatal perinatal characteristics and outcomes between twins and singletons. We found that twins had more adverse neonatal outcomes, including higher incidences of mortality, RDS, and surfactant usage, and a longer NICU stay than singletons.
Maternal characteristics
Our findings were similar to those from other studies showing that twins received more antenatal steroids and were more likely to be delivered by caesarean section, be conceived by ART and be born at a tertiary perinatal centre [1, 5, 7,8,9,10]. Although our study found that twins conceived by ART are substantially higher than singletons (39.5% for twins, 7.3% for singletons), the mortality of twins was slightly higher than that of singletons. Helmerhorst et al. reported that singletons conceived by assisted reproduction have significantly worse perinatal outcomes than those not conceived by assisted reproduction, but this is not the case for twins [27]. An explanation could be the fact that twin pregnancy patients who underwent ART had more early obstetric visits and a higher socioeconomic class than those with spontaneous pregnancy [28]. In our study, we speculated that twin pregnancy patients who had undergone ART may have had more intensive pregnancy surveillance and more planned births in hospitals with NICUs compared with spontaneous twin pregnancy patients, thus decreasing the mortality rate of twins to a certain extent. The possibility of a higher caesarean section rate for twins is due to the higher rate of emergency caesarean section in very preterm twins, which was supported by previous studies [7]. Garg et al. also noted that twins were more likely to be delivered by emergency caesarean sections than singletons (twins, 29.3%; singletons, 16.9%) [7].
Neonatal mortality
We found that twins had a higher rate of mortality than singletons, which was consistent with previously published reports [4, 5, 7,8,9] but contrary to the report written by Kalikkot Thekkeveedu R et al. [29]. In the current study, when infants were stratified into two groups, we also observed a higher perinatal mortality rate in the less than 28 weeks gestation group and the 28 weeks or more gestation group compared with that in singletons. Kalikkot Thekkeveedu R et al. published neonatal birth data of preterm and term singleton, twin, triplet and higher-order births from the United States during the years 2000, 2003, 2006, 2009, 2012, and 2016 and found that the adjusted odds for mortality were similar for twin births compared to singleton births. In this paper, the data included twins and singletons of all gestational ages, not only those less than 32 weeks gestation [29].
A previous study found that neonatal mortality was strongly correlated with gestational age, sex and a lack of prenatal steroid use, whereas ART helped to reduce the rate of mortality [7]. Other studies have shown that monochorionicity, growth discordance or intrauterine growth restriction and prematurity may be possible reasons for the higher mortality rate of twins [9]. Papiernik et al. found that same sex pairs had higher levels of mortality only below 28 weeks of gestation, whereas twins from same sex pairs with nondiscordant growth had outcomes similar to those of singletons [9]. However, data from 124 NICUs in the United States indicated that this difference between twins and singletons is driven primarily by the smaller twin’s weight. Although our study showed that very preterm twins were also less likely than singletons to be from pregnancies complicated by hypertension and SGA and more likely to have received prenatal corticosteroids, they still had higher rates of mortality. For these babies, we speculated that complications specific to twins, such as monochorionicity and growth discordance, may be responsible for the greater risk of adverse outcomes.
Neonatal morbidities
Our results revealed that the risk of RDS was higher in twins than in singletons. Although twins had a higher exposure to antenatal steroids, twins received more surfactant than singletons. Similar observations have been made previously in large population-based studies from Canada, Australia, the USA and South Korea [7, 10, 30, 31]. A retrospective cohort study from Choi SJ et al. including 450 singletons and 117 twins reported that multiple courses of antenatal corticosteroids were associated with a significantly decreased risk of RDS in singleton pregnancies. However, the current standard dose or interval for antenatal corticosteroid administration in singletons did not reduce RDS in twins [31]. Therefore, we speculated that antenatal steroids might have less of an effect on twins than singletons.
Interestingly, there were no significant differences in the rate of BPD and length of NICU stay in the two groups, but after adjusting for multiple variables, twins had slightly higher rates of these two morbidity outcomes than singletons (adjusted OR 1.10 [1.01,1.21] for BPD, adjusted OR 1.03 [1.00,1.06] for length of NICU stay, respectively). In addition, we found that twins were more likely to have RDS, receive more surfactant, and have a higher rate of BPD. It was shown that the major factors of BPD are ventilator-induced barotrauma and volutrauma on the premature lung [16]. In our study, the higher rate of BPD was due to the longer duration of invasive ventilation at and after 28 weeks of GA in twins.
We found no significant difference in breastfeeding between the two groups in the multivariate model, although the rate of breastfeeding for twins was higher than that for singletons. This result is consistent with previous studies [32,33,34]. A national Spanish cohort study reported that multiple preterm infants were more likely to be fed by a combination of both breastfeeding and bottle-feeding than singletons (33% versus 26%) [32]. Antibiotic treatment at delivery, in vitro fertilization and prenatal steroids were associated with a decreased risk for shorter in-hospital breastfeeding durations [32]. In the present study, the rates of ART and prenatal steroid usage in twins were much higher than those in singletons, which may explain the slightly higher rate of breastfeeding in twins.
Available studies on outcomes of twins and singletons have reported conflicting results on the risk for severe IVH, NEC ≥ Stage II and severe ROP. Our data did not show any differences in these three morbidities between twins and singletons, which was supported by other large population and multicentre studies [7, 11]. However, some other studies showed inconsistent results [10, 35]. Friling and colleagues found that singletons with lower GA and BW had a significantly higher rate of advanced ROP (stages II-III) (30.2%) than twins (23.1%), not adjusting for possible risk factors associated with ROP, such as oxygen usage and ventilation [35]. Qiu et al. reported that twins had a lower incidence of ROP than singletons after adjusting for multiple variables for all infants with ROP, not only for those with severe ROP [10], which may be a possible explanation for the inconsistency in our study.
Strengths and limitations
Our retrospective study included a large number of very preterm infants in China with a rigorous protocol for checking the completeness of recruitment. This study allows us to better ascertain the effect of plurality on outcomes, and we can counsel and prognosticate for our patients with our nationwide data.
Our study has several limitations. Our cohort was hospital-based, and it was from a select group of large tertiary NICUs with the highest level of neonatal care in China, which may not be representative of the general population. Pregnant women with foetal death in the delivery room and early pregnancy losses were not included in our study, so we may have underestimated the real mortality rate for each of these groups, which may have led to selection bias. Unfortunately, the database contains limited obstetric data (such as the reasons for delivery, the quality of prenatal care, illicit drug use, and other pregnancy complications of pregnant women), which may affect the neonatal outcomes of infants. However, we recognize this as a limitation of our work and chose information that was recorded completely and accurately for analysis. However, the mothers included in this study were predominantly from tertiary centres and may actually be at a higher risk than the more general population. Both zygosity and chorionicity have been suggested to affect the outcomes of twins. Monozygosity has been associated with higher rates of congenital anomalies, and chorionicity is related to the risk of growth discordance and growth restriction [9, 36, 37]; however, we did not examine these factors because we lack data regarding zygosity and chorionicity.
Conclusion
Overall, our study suggests that very preterm twins are at an increased risk of mortality, RDS, and surfactant usage, and have a longer length of NICU stay compared with singletons. More attention should be given to early severe RDS treatment and respiratory management for twins, which may be helpful to decrease the mortality rate and hospital stay. Further studies adjusting for confounders such as chorionicity, dizygosity, cord anomalies and socioeconomic factors are needed to explore the long-term outcomes of twins.
Availability of data and materials
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
Abbreviations
- ALR:
-
Alternating logistic regression
- AOR:
-
Adjusted odds ratio
- ART:
-
Assisted reproductive technology
- BPD:
-
Bronchopulmonary dysplasia
- CHNN:
-
Chinese Neonatal Network
- CI:
-
Confidence interval
- cPVL:
-
Cystic periventricular leukomalacia
- CXR:
-
Chest X-ray
- GA:
-
Gestational age
- GEE:
-
Generalized estimating equation
- IQRs:
-
Interquartile ranges
- IVH:
-
Intraventricular hemorrhage
- NEC:
-
Necrotizing enterocolitis
- NICUs:
-
Neonatal intensive care units
- RDS:
-
Respiratory distress syndrome
- ROP:
-
Retinopathy of prematurity
- SDs:
-
Standard deviations
- SGA:
-
Small for gestational age
- VPIs:
-
Very preterm infants
References
Isaacson A, Diseko M, Mayondi G, Mabuta J, Davey S, Mmalane M, et al. Prevalence and outcomes of twin pregnancies in Botswana: a national birth outcomes surveillance study. BMJ Open. 2021;11(10):e047553.
Paulson R, Lockwood CJ. Pregnancy outcome after assisted reproductive technology. UpToDate; 2018. p. 1–14. https://www.uptodate.com/contents/pregnancy-outcome-after-assisted-reproductive-technology?source=see_link#H24.
ACOG Practice Bulletin No. 169: Multifetal gestations: twin, triplet, and higher-order multifetal pregnancies. Obstet Gynecol. 2016;128(4):e131–46.
Santana DS, Silveira C, Costa ML, Souza RT, Surita FG, Souza JP, et al. Perinatal outcomes in twin pregnancies complicated by maternal morbidity: evidence from the WHO Multicountry Survey on Maternal and Newborn Health. BMC Pregnancy Childbirth. 2018;18(1):449.
Yeo KT, Lee QY, Quek WS, Wang YA, Bolisetty S, Lui K, et al. Trends in morbidity and mortality of extremely preterm multiple gestation newborns. Pediatrics. 2015;136:263–71.
Deng K, Liang J, Mu Y, Liu Z, Wang Y, Li M, et al. Preterm births in China between 2012 and 2018: an observational study of more than 9 million women. Lancet Glob Health. 2021;9:e1226–41.
Garg P, Abdel-Latif ME, Bolisetty S, Bajuk B, Vincent T, Lui K. Perinatal characteristics and outcome of preterm singleton, twin and triplet infants in NSW and the ACT, Australia (1994–2005). Arch Dis Child Fetal Neonatal Ed. 2010;95:F20–4.
Porta R, Capdevila E, Botet F, Verd S, Ginovart G, Moliner E, et al. Morbidity and mortality of very low birth weight multiples compared with singletons. J Matern Fetal Neonatal Med. 2019;32:389–97.
Papiernik E, Zeitlin J, Delmas D, Blondel B, Künzel W, Cuttini M, et al. Differences in outcome between twins and singletons born very preterm: results from a population-based European cohort. Hum Reprod. 2010;25:1035–43.
Qiu X, Lee SK, Tan K, Piedboeuf B, Canning R. Canadian Neonatal Network: comparison of singleton and multiple-birth outcomes of infants born at or before 32 weeks of gestation. Obstet Gynecol. 2008;111:365–71.
Kirkby S, Genen L, Turenne W, Dysart K. Outcomes and milestone achievement differences for very low-birth-weight multiples compared with singleton infants. Am J Perinatol. 2010;27:439–44.
Cao Y, Jiang S, Sun J, Hei M, Wang L, Zhang H, et al. Assessment of neonatal intensive care unit practices, morbidity, and mortality among very preterm infants in China. JAMA Netw Open. 2021;4(8):e2118904.
Sun J, Cao Y, Hei M, Sun H, Wang L, Zhou W, et al. Chinese neonatal network. Data quality improvement and internal data audit of the Chinese neonatal network data collection system. Front Pediatr. 2021;9:711200.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Walsh MC, Kliegman RM. Necrotizing enterocolitis-treatment based on staging creteria. Pediatr Clin N Am. 1986;33:179–201.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Papile L-A, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Gole GA, Ells AL, Katz X, Holmstrom G, Fielder AR, Capone A, et al. International committee for the classification of retinopathy of prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002;110:285–91.
British Association of Perinatal Medicine. Guidelines for good practice in the management of neonatal respiratory distress syndrome. London: BAPM; 1999.
Ballard JL, Novak KK, Driver M. A simplified score for assessment of fetal maturation of newly born infants. J Pediatr. 1979;95:769–74.
Zhu L, Zhang R, Zhang S, Shi W, Yan W, Wang X, et al. Chinese neonatal birth weight curve for different gestational age. Chin J Pediatr. 2015;53:97–103.
Katz J, Carey VJ, Zeger SL, Sommer A. Estimation of design effects and diarrhea clustering within households and villages. Am J Epidemiol. 1993;138:994–1006.
Carey V, Zeger SL, Diggle P. Modelling multivariate binary data with alternating logistic regressions. Biometrika. 1993;80:517–26.
Bhatnagar SR, Atherton J, Benedetti A. Comparing alternating logistic regressions to other approaches to modelling correlated binary data. J Stat Comput Simul. 2015;85:2059–71.
Wang K, Lee AH, Hamilton G, Yau KK. Multilevel logistic regression modelling with correlated random effects: application to the Smoking Cessation for Youth study. Stat Med. 2006;25:3864–76.
Helmerhorst FM, Perquin DA, Donker D, Keirse MJ. Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ. 2004;328:261.
Olivennes F, Kadhel P, Rufat P, Fanchin R, Fernandez H, Frydman R. Perinatal outcome of twin pregnancies obtained after in vitro fertilization: comparison with twin pregnancies obtained spontaneously or after ovarian stimulation. Fertil Steril. 1996;66:105–9.
Kalikkot Thekkeveedu R, Dankhara N, Desai J, Klar AL, Patel J. Outcomes of multiple gestation births compared to singleton: analysis of multicenter KID database. Matern Health Neonatol Perinatol. 2021;7(1):15.
Hayes EJ, Paul D, Ness A, Mackley A, Berghella V. Very-low-birthweight neonates: do outcomes differ in multiple compared with singleton gestations? Am J Perinatol. 2007;24:373–6.
Choi SJ, Song SE, Seo ES, Oh SY, Kim JH, Roh CR. The effect of single or multiple courses of antenatal corticosteroid therapy on neonatal respiratory distress syndrome in singleton versus twin pregnancies. Aust N Z J Obstet Gynaecol. 2009;49(2):173–9.
Porta R, Capdevila E, Botet F, Ginovart G, Moliner E, Nicolàs M, et al. Breastfeeding disparities between multiples and singletons by NICU discharge. Nutrients. 2019;11:2191.
Geraghty SR, Pinney SM, Sethuraman G, Roy-Chaudhury A, Kalkwarf HJ. Breast milk feeding rates of mothers of multiples compared to mothers of singletons. Ambul Pediatr. 2004;4:226–31.
Hill PD, Aldag JC, Zinaman M, Chatterton RT. Predictors of preterm infant feeding methods and perceived insufficient milk supply at week 12 postpartum. J Hum Lact. 2007;23:32–8.
Friling R, Axer-Siegel R, Hersocovici Z, Weinberger D, Sirota L, Snir M. Retinopathy of prematurity in assisted versus natural conception and singleton versus multiple births. Ophthalmology. 2007;114:321–4.
Dubé J, Dodds L, Armson BA. Does chorionicity or zygosity predict adverse perinatal outcomes in twins? Am J Obstet Gynecol. 2002;186:579–83.
Hack KE, Derks JB, Elias SG, Franx A, Roos EJ, Voerman SK, et al. Increased perinatal mortality and morbidity in monochorionic versus dichorionic twin pregnancies: clinical implications of a large Dutch cohort study. BJOG. 2008;115:58–67.
Acknowledgements
We thank the data abstractors from the Chinese Neonatal Network. We thank all the staff at the Chinese Neonatal Network coordinating center for providing organizational support (Lin Yuan, MD, PhD; Yu-Lan Lu, PhD; Tong-Ling Yang, RN; Hao Yuan, RN; Li Wang, RN).
Chinese Neonatal Network:
Shoo K. Lee8, Chao Chen5, Lizhong Du9, Wenhao Zhou5, Yun Cao3,5, Falin Xu10, Xiuying Tian11, Huayan Zhang12, Yong Ji13, Zhankui Li14, Jingyun Shi15, Xindong Xue16, Chuanzhong Yang17, Dongmei Chen2, Sannan Wang18, Ling Liu19, Xirong Gao20, Hui Wu21, Changyi Yang22, Shuping Han23, Ruobing Shan24, Hong Jiang25,
Gang Qiu26, Qiufen Wei27, Rui Cheng28, Wenqing Kang29, Mingxia Li30, Yiheng Dai31, Lili Wang32, Jiangqin Liu33, Zhenlang Lin34, Yuan Shi35, Xiuyong Cheng36, Jiahua Pan37, Qin Zhang38, Xing Feng39, Qin Zhou40, Long Li41, Pingyang Chen42, Xiaoying Li4, Ling Yang43, Deyi Zhuang44, Yongjun Zhang45, Jianhua Sun6, Jinxing Feng46, Li Li47, Xinzhu Lin48, Yinping Qiu49, Kun Liang50, Li Ma51, Liping Chen52, Liyan Zhang53, Hongxia Song54, Zhaoqing Yin55, Mingyan Hei56, Huiwen Huang57, Jie Yang58, Dong Li59, Guofang Ding60, Jimei Wang1, Qianshen Zhang61, Xiaolu Ma9, Joseph Ting7
Author Affiliations:
8Mount Sinai Hospital, University of Toronto
9Children's Hospital of Zhejiang University School of Medicine
10The Third Affiliated Hospital of Zhengzhou University
11Tianjin Central Hospital of Obstetrics and Gynecology
12Guangzhou Women and Children’s Medical Center
13Children’s Hospital of Shanxi
14Northwest Women's and Children's Hospital
15Gansu Provincial Maternity and Child Care Hospital
16Shengjing Hospital of China Medical University
17Shenzhen Maternity and Child Health Care Hospital
18The Affiliated Suzhou Hospital of Nanjing Medical University
19Guizhou Women and Children’s Hospital/Guiyang Children’s Hospital
20Hunan Children’s Hospital
21The First Bethune Hospital of Jilin University
22Fujian Maternity and Child Health Hospital, Affiliated Hospital of Fujian Medical University
23Nanjing Maternity and Child Health Care Hospital
24Qingdao Women and Children’s Hospital
25The Affiliated Hospital of Qingdao University
26Children’s Hospital of Shanghai
27Women and Children's Hospital of Guangxi Zhuang Autonomous Region
28Children’s Hospital of Nanjing Medical University
29Henan Children’s Hospital
30The First Affiliated Hospital of Xinjiang Medical University
31Foshan Women and Children’s Hospital
32The First Affiliated Hospital of Anhui Medical University
33Shanghai First Maternity and Infant Hospital
34Yuying Children's Hospital Affiliated to Wenzhou Medical University
35Children’s Hospital of Chongqing Medical University
36The First Affiliated Hospital of Zhengzhou University
37The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China
38Shaanxi Provincial People’s Hospital
39Children's Hospital of Soochow University
40Wuxi Maternity and Child Healthcare Hospital
41People's Hospital of Xinjiang Uygur Autonomous Region
42The Second Xiangya Hospital of Central South University
43Hainan Women and Children’s Hospital
44Xiamen Children’s Hospital
45Xinhua Hospital affiliated to Shanghai Jiao Tong University School of Medicine
46Shenzhen Children’s Hospital
47Children's Hospital Affiliated to Capital Institute of Pediatrics
48Women and Children’s Hospital, School of Medicine, Xiamen university
49General Hospital of Ningxia Medical University
50First Affiliated Hospital of Kunming Medical University
51Hebei Provincial Children's Hospital
52Jiangxi Provincial Children’s Hospital
53Fuzhou Children’s Hospital of Fujian Province
54The First Affiliated Hospital of Xi’an Jiao Tong University
55Dehong people's Hospital of Yunnan Province
56Beijing Children's Hospital, Capital Medical University
57Zhuhai Center for Maternal and Child Health Care
58Guangdong Women and Children's Hospital
59Dalian Municipal Women and Children’s Medical Center
60Peking Union Medical College Hospital
61Shenzhen Hospital of Hongkong University
Funding
This work was funded by the Canadian Institutes of Health Research (CTP87518 to Shoo Lee) and Science and Technology Innovation Program of Shanghai (21Y21900802 to Jimei Wang).
Author information
Authors and Affiliations
Consortia
Contributions
Min Yang, Yanchen Wang, Jimei Wang had full access to all the data in this study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Yun Cao, Jianhua Sun, Joseph Ting, Xiafang Chen, Dongmei Chen, Jimei Wang. Acquisition, analysis and interpretation of data: Min Yang, Yanchen Wang. Drafting of Manuscripts: Min Yang, Lingyu Fang. Critical revision of the manuscripts for important intellectual content: All author. Statistical Analysis: Yanchen Wang. Administrative, technical or material support: Xiaobo Fan, Jiale Dai, Xiaomei Tong. Supervision: Yun Cao, Jianhua Sun, Xiaoying Li, Joseph Ting, Xiafang Chen, Dongmei Chen, Jimei Wang. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval was obtained from the ethics review board of Children’s Hospital of Fudan University (2018–296), which was recognized by all participating hospitals. Waiver of informed consent were granted at all sites including 57 Chinese tertiary NICUs for de-identified data. Ethics committees that waived the consent included Ethics Committee of Children's Hospital of Fudan University, Ethics Committee of the Third Affiliated Hospital of Zhengzhou University, Ethics Committee of Tianjin Central Hospital of Obstetrics and Gynecology, Ethics Committee of Guangzhou Women and Children’s Medical Center, Ethics Committee of Children’s Hospital of Shanxi, Ethics Committee of Northwest Women's and Children's Hospital, Ethics Committee of Gansu Provincial Maternity and Child Care Hospital, Ethics Committee of Shengjing Hospital of China Medical University, Ethics Committee of Shenzhen Maternity and Child Health Care Hospital, Ethics Committee of Quanzhou Women and Children’s Hospital, Ethics Committee of the Affiliated Suzhou Hospital of Nanjing Medical University, Ethics Committee of Guizhou Women and Children’s Hospital/Guiyang Children’s Hospital, Ethics Committee of Hunan Children’s Hospital, Ethics Committee of the First Bethune Hospital of Jilin University, Ethics Committee of Fujian Maternity and Child Health Hospital, Ethics Committee of Nanjing Maternity and Child Health Care Hospital, Ethics Committee of Qingdao Women and Children’s Hospital, Ethics Committee of the Affiliated Hospital of Qingdao University, Ethics Committee of Children’s Hospital of Shanghai, Ethics Committee of Women and Children's Hospital of Guangxi Zhuang Autonomous Region, Ethics Committee of Children’s Hospital of Nanjing Medical University, Ethics Committee of Henan Children’s Hospital, Ethics Committee of the First Affiliated Hospital of Xinjiang Medical University, Ethics Committee of Foshan Women and Children’s Hospital, Ethics Committee of the First Affiliated Hospital of Anhui Medical University, Ethics Committee of Shanghai First Maternity and Infant Hospital, Ethics Committee of Yuying Children's Hospital Affiliated to Wenzhou Medical University, Ethics Committee of Children’s Hospital of Chongqing Medical University, Ethics Committee of the First Affiliated Hospital of Zhengzhou University, Ethics Committee of the First Affiliated Hospital of USTC, Ethics Committee of Shaanxi Provincial People’s Hospital, Ethics Committee of Children's Hospital of Soochow University, Ethics Committee of Wuxi Maternity and Child Healthcare Hospital, Ethics Committee of People's Hospital of Xinjiang Uygur Autonomous Region, Ethics Committee of the Second Xiangya Hospital of Central South University, Ethics Committee of Children’s Hospital Affiliated to Shandong University, Ethics Committee of Hainan Women and Children’s Hospital, Ethics Committee of Xiamen Children’s Hospital, Ethics Committee of Xinhua Hospital affiliated to Shanghai Jiao Tong University School of Medicine, Ethics Committee of Shanghai Children’s Medical Center, Jiao Tong University School of Medicine, Ethics Committee of Shenzhen Children’s Hospital, Ethics Committee of Children's Hospital Affiliated to Capital Institute of Pediatrics, Women and Children’s Hospital, School of Medicine, Xiamen university, Ethics Committee of General Hospital of Ningxia Medical University, Ethics Committee of the First Affiliated Hospital of Kunming Medical University, Ethics Committee of Hebei Provincial Children's Hospital, Ethics Committee of Jiangxi Provincial Children’s Hospital, Ethics Committee of Fuzhou Children’s Hospital of Fujian Province, Ethics Committee of the First Affiliated Hospital of Xi’an Jiao Tong University, Ethics Committee of Dehong people's Hospital of Yunnan Province, Ethics Committee of Beijing Children's Hospital, Ethics Committee of Zhuhai Center for Maternal and Child Health Care, Ethics Committee of Guangdong Women and Children's Hospital, Ethics Committee of Dalian Municipal Women and Children’s Medical Center, Ethics Committee of Peking Union Medical College Hospital, Ethics Committee of Obstetrics & Gynecology Hospital of Fudan University, Ethics Committee of Shenzhen Hospital of Hongkong University, and Ethics Committee of Children's Hospital of Zhejiang University School of Medicine.
Consent for publication
Not required.
Competing interests
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, M., Fang, L., Wang, Y. et al. Perinatal characteristics and neonatal outcomes of singletons and twins in Chinese very preterm infants: a cohort study. BMC Pregnancy Childbirth 23, 89 (2023). https://doi.org/10.1186/s12884-023-05409-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05409-8