Abstract
Background
The rates of successful vaginal birth after previous cesarean section (VBAC) have been increasing with minimal complication. Successful vaginal birth after cesarean section improves maternal and fetal outcomes by shortening the length of hospital stay, avoiding abdominal surgery, decreasing the risk of infections and hemorrhage, and decreasing injury of the bladder and bowel. Despite a few single studies stating different predictors of successful VBAC, there is a lack of nationwide data to show the determinants of successful VBAC. Thus, this meta-analysis aimed to determine the predictors of successful VBAC in Ethiopia.
Methods
A systematic literature search was performed from PubMed, Web of Sciences, EMBASE, CINAHL, and Google scholar until July 25, 2022. The quality of included studies was evaluated using the Joanna Briggs Institute (JBI) critical appraisal checklist. The analysis was executed using Stata 14 statistical software. Heterogeneity was evaluated statistically using Cochran’s Q-statistic and quantified by the I2 value. A random-effects model was used to estimate the determinants of successful vaginal birth after a cesarean section if substantial heterogeneity was detected across included studies; otherwise, a fixed-effects model was used.
Results
Women living in rural residence (AOR: 2.14; 95% CI: 1.01, 4.52), history of previous spontaneous vaginal delivery (AOR: 2.92; 95% CI: 2.02, 4.23), previous successful vaginal birth after previous cesarean section (AOR: 5.29; 95% CI: 2.20, 12.69), history of stillbirth (AOR: 1.57; 95% CI: 1.20, 2.04), cervical dilation of ≥ 4 cm at admission (AOR: 2.14; 95% CI: 1.27, 3.61), spontaneous ruptured membranes at admission (AOR: 1.32; 95% CI: 1.17, 1.48) were independent determinants of successful vaginal birth after previous cesarean section.
Conclusion
The results of this meta-analysis showed that successful VBAC was influenced by past and present obstetric conditions and other predictors. Thus, it is recommended that obstetric care providers should emphasize those factors that lead to successful vaginal birth during counseling and optimal selection of women for the trial of labour after cesarean section.
Systematic review and meta-analysis registration
PROSPERO CRD42022329567.
Similar content being viewed by others
Introduction
The World Health Organization (WHO) has reported that the cesarean section (CS) rate has increased in the world [1]. Cesarean section is significantly increasing though the WHO recommended the optimal rate of cesarean section to be between 5 and 15% [2]. Worldwide, about 21.1% of women gave birth by cesarean Sect. [3]. In Ethiopia, the prevalence of cesarean section among women who gave birth at health institutions was 29.55% [4].
Repeated cesarean section is associated with increased maternal complications, such as placenta previa, hysterectomy, adhesions, blood transfusions, and surgical injury [5]. Furthermore, the risk of postpartum death is higher in mothers who gave birth by cesarean Sect. [6, 7].
Despite cesarean section a life-saving medical procedure and intervention, the reasons for the continued increase are not completely understood [8, 9]. However, obstetricians’ uncertainty about the safety of the trial of vaginal birth after a previous caesarean section (VBAC), and unwilling of women to accept the trial of VBAC results in an increased cesarean delivery rate [10, 11]. Moreover, the decline in the rate of vaginal birth after cesarean section is the main reason for the rise in cesarean section rate [12, 13].
Vaginal birth after a previous caesarean section is an intended trial of vaginal birth by a woman who has had a previous cesarean Sect. [14]. Choosing the route of delivery after one previous cesarean section depends on the preferences of women, and past and present obstetric history [15, 16]. Candidates for a VBAC are women with low transverse hysterotomy, and singleton pregnancy with no contraindication for vaginal delivery [17, 18]. Careful selection of women for trial of labour after cesarean section delivery (TOLAC) remains a wise clinical decision as failed VBAC has the worst maternal outcomes [15, 19, 20].
Existing evidence have shown that the rates of successful VBAC among women with one cesarean section scar have been increasing with minimal complication [21,22,23]. Literature has also indicated that successful VBAC has improved maternal and fetal outcomes compared with delivery by repeated cesarean Sect. [24, 25]. Furthermore, a successful VBAC shortens the length of hospital stay, avoids abdominal surgery, decreases the risk of infections and hemorrhage, and decreases injury of the bladder and bowel [23, 26, 27].
The chance of vaginal birth after a previous cesarean section is determined by predictors such as maternal age, history of previous vaginal delivery, cervical dilatation at admission, rupture of membrane at admission, cephalo-pelvic disproportion, and birth weight > 4 kg [28,29,30,31,32]. Existing systematic review and meta-analysis shows that age, obesity, labor induction, birth weight, Bishop score, indications for the previous CS and previous vaginal birth were identified factors related to the success of VBAC [33].
Despite a few individual studies reporting different predictors of successful VBAC, there is a lack of nationwide data to show the determinants of successful VBAC. Thus, this meta-analysis aimed to determine the predictors of successful VBAC in Ethiopia. Accordingly, the population, intervention, comparator, outcome, study design (PICOS) framework was as follows: (P) Pregnant women, (I) trial of labour after cesarean section, (C) failed VBAC, (O) Determinants of successful VBAC among women with prior caesarean section.
Methods
The study was conducted and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines (Supplementary file 1). The review was registered on the International Prospective Register of Systematic Reviews (PROSPERO) with the unique number CRD42022329567.
Eligibility criteria
Observational studies involving women of child-bearing ages that were candidates for attempted vaginal birth with previous cesarean section in Ethiopia were considered. Articles that reported odds ratio (OR) with a 95% confidence interval (CI) for the binary factors in women with successful VBAC were included. Studies conducted only in Ethiopia, and published in or written in English were included. Whereas, studies that did not address determinants of successful vaginal birth after previous cesarean section were excluded. In addition, editorial reports, abstracts, letters, reviews, and commentaries were excluded from the study.
Information sources and search strategy
A systematic literature search was performed from PubMed, Web of Sciences, EMBASE, CINAHL, and Google scholar until July 25, 2022. Medical Subject Headings, keywords, different boolean operators, and truncations were used in the search strategy. The following search keywords were used: "Vaginal Birth After Cesarean" OR "Vaginal birth*" OR "vaginal deliver*" OR "trial of labor*" OR "trial of labour" OR "active labor" OR "active labour" AND "Caesarean section" OR CS OR "abdominal deliver*" OR "uterine scar*" AND Determinant* OR Predictor* AND "Ethiopia". For instance, the search detail for PubMed Advanced search: ((((("Vaginal Birth After Cesarean"[All Fields] OR "vaginal birth*"[All Fields] OR "vaginal deliver*"[All Fields] OR "trial of labor*"[All Fields] OR "trial of labour"[All Fields] OR "active labor"[All Fields] OR "active labour"[All Fields]) AND "Caesarean section"[All Fields]) OR ("chemical synthesis"[MeSH Subheading] OR ("chemical"[All Fields] AND "synthesis"[All Fields]) OR "chemical synthesis"[All Fields] OR "cs"[All Fields]) OR "abdominal deliver*"[All Fields] OR "uterine scar*"[All Fields]) AND "determinant*"[All Fields]) OR "predictor*"[All Fields]) AND "Ethiopia"[All Fields]. Furthermore, bibliographies of selected articles were reviewed for additional potentially relevant studies. Moreover, Institutional Digital Libraries were searched to find grey literature.
Outcome
The main outcomes of this meta-analysis were predictors of successful VBAC in Ethiopia. A successful VBAC is defined as spontaneous or instrumental assisted delivery to a woman undergoing a trial of labour after caesarean section delivery. In the meta-analysis, all of the pregnant women had experienced a trial of labour after a caesarean section.
Study selection
All retrieved articles were exported to the EndNote X7.2.1 (Thomson Reuters, New York, USA) software citation manager to manage the screening process. Studies were initially reviewed based on their titles and abstracts. Then those studies deemed relevant were retrieved and reviewed in full text. The PRISMA 2020 flow diagram for new systematic reviews was used to summarize the study selection processes.
Data extraction
Two reviewers (BDM and AAA) independently extracted pertinent data from each included article using a Microsoft Excel sheet. The following data were extracted from included articles: first author, year of publication, study setting, and design, sample size, and different determinants of successful VBAC.
Assessment of risk of bias
The quality of included studies was evaluated by two reviewers (BDM and AAA) independently using the Joanna Briggs Institute (JBI) critical appraisal checklist adapted for case–control and cross-sectional studies. Any unclear information or disagreements between the two reviewers were resolved through discussion. Case–control studies were evaluated based on comparability and matching of groups, standard measurement, strategies to deal with cofounders, and statistical analysis, and rated from zero to ten-point scales. Cross-sectional studies were evaluated based on addressing the target population, adequacy of sample size, data collection methods, the definition of the variables, data collection tools, statistical analysis tests, study objectives, adequacy of response rate, and statistical analysis, and rated from zero to eight-point scales. Scores above five indicate low risk.
Data synthesis
From each included study, the odds ratio (OR) for each factor with the 95% confidence intervals (CI) was extracted. Two reviewers (BDM and AAA) performed the data synthesis. We executed the effects of summary estimates with command “metan” using Stata 14.0 statistical program. Heterogeneity was evaluated statistically using Cochran’s Q-statistic and quantified by the I2 value. A random-effects model was used to estimate the determinants of successful vaginal birth after a cesarean section if substantial heterogeneity was detected across included studies; otherwise, a fixed-effects model was used. Publication bias was not evaluated because of the few numbers of studies for each factor.
Results
Study selection
A total of 10,632 records were identified from different databases. About 3,868 duplicate records were removed before the screening. Two reviewers (BDM and AAA) independently evaluated the remaining 6,764 records based on their titles and abstracts, which result in the further exclusion of 6,707 records. Additionally, 49 articles were excluded after reviewing 57 full texts articles. Lastly, a total of 8 studies were included in the final analysis (Fig. 1).
Study characteristics
From a total of 8 studies were included, five were case–control studies, and three were cross-sectional studies. The sample size in the included studies ranged from 169 to 419. The Joanna Briggs Institute Critical Appraisal Checklist revealed a score of seven to eight in cross-sectional studies and seven to nine in case–control studies. In total, 2,100 women who attempted a vaginal birth after a cesarean section were included. Regarding geographical distribution, three of the studies were from Oromia [34,35,36], two from SNNPR [37, 38], two from Addis Ababa administrative city [39, 40], and one from Harari and Dire Dawa [41] (Table 1).
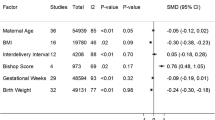
Determinants of successful vaginal birth after previous cesarean section
Three studies indicated that women living in rural residence had a higher chance of successful VBAC. The pooled odds ratio indicated that the likelihood of successful VBAC was twice more likely among women living in rural residence (AOR: 2.14; 95% CI: 1.01, 4.52) than those women from urban residence (Fig. 2).
Six studies indicated that women with a history of previous spontaneous vaginal delivery had a higher chance of successful VBAC. The pooled odds ratio indicated that the odds of successful VBAC were almost three times higher among women with a history of previous spontaneous vaginal delivery (AOR: 2.92; 95% CI: 2.02, 4.23) compared to women who had no past spontaneous vaginal delivery (Fig. 3).
Seven studies indicated that women with previous successful VBAC had a higher chance of successful VBAC. Accordingly, mothers with previous successful VBAC have 5.29 times higher odds of having successful VBAC (AOR: 5.29; 95% CI: 2.20, 12.69) compared to their counterparts (Fig. 4).
Three studies indicated that women with a history of stillbirth had a higher chance of successful VBAC. The pooled odds ratio indicated that the likelihood of having successful VBAC was 1.57 times more likely among women with a history of stillbirth (AOR: 1.57; 95% CI: 1.20, 2.04) than those who had no history of stillbirth (Fig. 5).
Four studies indicated that women with cervical dilation of ≥ 4 cm at admission had a higher chance of successful VBAC. Accordingly, the pooled odds ratio indicated that the odds of having successful VBAC were twice more likely among mothers with cervical dilation of ≥ 4 cm at admission (AOR: 2.14; 95% CI: 1.27, 3.61) compared to those women with cervical dilation of < 4 cm at admission (Fig. 6).
Four studies indicated that women who had spontaneous ruptured membranes at admission had a higher chance of successful VBAC. Accordingly, mothers who had spontaneous ruptured membranes at admission were 1.32 times more likely (AOR: 1.32; 95% CI: 1.17, 1.48) to have successful VBAC compared to mothers with intact membranes at admission (Fig. 7).
Heterogeneity and publication bias and sensitivity analysis
Heterogeneity (I2 > 50%) was detected in the following meta-analysis: OR of rural residence, OR of history of previous spontaneous vaginal delivery, OR of previous successful birth after previous cesarean section, and OR of cervical dilation of ≥ 4 cm at admission. The rest two meta-analysis had ≤ 50% heterogeneity: OR of history of still birth, and OR of spontaneous ruptured membranes at admission. The number of included studies in each identified determinant of successful VBAC was limited. As a result, publication bias and sensitivity analysis were not evaluated in this meta-analysis.
Discussion
The chance of VBAC for mothers varies based on obstetric and demographic characteristics [33, 42, 43]. This meta-analysis investigated the predictors of successful VBAC among women with prior cesarean section. Accordingly, rural residence, history of previous spontaneous vaginal delivery, previous successful VBAC, cervical dilation of ≥ 4 cm at admission, history of stillbirth, and spontaneous ruptured membranes at admission were significant determinants of successful VBAC. This implies that understanding the influencing predictors on VBAC could help to appraise chances for attaining a successful vaginal birth among women with prior CS.
Results of this meta-analysis indicated that mothers who live in rural residences were more likely to have successful VBAC than those who live in urban residences. The reason could be explained by the fact that women from rural residents would prefer vaginal birth because of fear of surgery and their lifestyles. This finding is supported by a study conducted in Turkey [44]. This meta-analysis also indicated that women with a history of stillbirth were more likely to have successful VBAC than those who had no history of stillbirth. This implies that having a history of poor pregnancy outcomes such as stillbirth can determine the mode of delivery [45]. Previous studies documented that adverse birth experiences have been identified as a strong predictor for a mode of delivery preference [46, 47].
This meta-analysis identified that women with a history of previous spontaneous vaginal delivery were more likely to have successful VBAC than those who had no past spontaneous vaginal delivery. This finding is supported by a previous systematic review [33]. The reason could be that multiparous mothers will develop effective uterine contractions in labour that will decrease subsequent problems [42]. Furthermore, previous vaginal delivery is associated with a reduced risk of uterine rupture, which further reduces the indication of CS [48]. Furthermore, mothers with previous successful VBAC were more likely to have successful VBAC compared to their counterparts. This could be attributed to the fact that a prior successful VBAC shortens the progress of labor and lowers the risk of subsequent rupture of the uterus [49]. Prior vaginal delivery following the prior CS was identified as a predictive indicator of successful VBAC [43].
This meta-analysis also identified that mothers with cervical dilation of ≥ 4 cm at admission were more likely to have successful VBAC compared to those with cervical dilation of < 4 cm at admission. The reason might be that mothers might be progressing to full dilation much more rapidly once they are in the active phase of labor, with faster progress of labor [50]. Evidence indicated that the prediction of the trial of labour after caesarean section delivery success was highly dependent on the initial cervical examination at the time of admission [33, 51]. Similarly, mothers who had spontaneous ruptured membranes at admission were more likely to have successful VBAC compared to those mothers with intact membranes at admission. The literature revealed that spontaneous ruptured membranes on admission were the most significant and strongest predictor for successful VBAC [52].
This review has the following potential limitations: the possible sources of heterogeneity were not addressed though heterogeneity between studies was exhibited. Furthermore, the studies included in this review represented only four regions of the country. Nevertheless, this meta-analysis provided the first quantitative evaluation of predictors of successful vaginal birth among women with prior cesarean section in Ethiopia, to the best of the authors’ knowledge.
This meta-analysis provides vital evidence to inform policy-makers, and other relevant stakeholders to understand the chances for achieving a successful vaginal birth among women with prior cesarean section. Some factors have been identified as being associated with an increased likelihood of successful VBAC. Hence, it could help healthcare providers to provide evidence-based counseling regarding VBAC, which has significant implications for avoiding repeated cesarean section.
Conclusions
The results of this meta-analysis showed that living in rural residence, a history of previous spontaneous vaginal delivery, previous successful VBAC, cervical dilation of ≥ 4 cm at admission, a history of stillbirth, and spontaneous ruptured membranes at admission were factors significantly associated with successful VBAC. Therefore, hospitals and obstetric care providers should prepare a decision tool for the success of VBAC by considering past and present obstetric conditions and other predictors. It is also recommended that obstetric care providers should emphasize those factors that lead to a higher likelihood of successful vaginal birth during counseling and optimal selection of women for the trial of labour after caesarean section.
Availability of data and materials
All relevant data is included within the manuscript file.
Abbreviations
- AOR:
-
Adjusted odds ratio
- CBCS:
-
Community-based cross-sectional
- CI:
-
Confidence intervals
- JBI:
-
Joanna Briggs Institute
- OR:
-
Odds ratio
- VBAC:
-
Vaginal birth after previous cesarean section
- WHO:
-
World Health Organization
References
Betrán AP, Torloni MR, Zhang J-J, Gülmezoglu A, Aleem H, Althabe F, et al. WHO statement on caesarean section rates. BJOG. 2016;123(5):667.
Mirteymouri M, Ayati S, Pourali L, Mahmoodinia M, Mahmoodinia M. Evaluation of maternal-neonatal outcomes in vaginal birth after cesarean delivery referred to maternity of academic hospitals. J Family Reprod Health. 2016;10(4):206.
Betran AP, Ye J, Moller A-B, Souza JP, Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health. 2021;6(6):e005671.
Gedefaw G, Demis A, Alemnew B, Wondmieneh A, Getie A, Waltengus F. Prevalence, indications, and outcomes of caesarean section deliveries in Ethiopia: a systematic review and meta-analysis. Patient Saf Surg. 2020;14(1):1–10.
Marshall NE, Fu R, Guise JM. Impact of multiple cesarean deliveries on maternal morbidity: a systematic review. Am J Obstetr Gynecol. 2011;205(3):262 e1-e8.
Subedi S. Rising rate of cesarean section-a year review. J Nobel Med College. 2011;1(2):50–6.
Yamuna R. A comparitive study of indications and fetomaternal outcomes in primary cesarean section in primi and multi gravida: Government Mohan Kumaramangalam Medical College, Salem. 2018.
Batieha A, Al-Daradkah S, Khader Y, Basha A, Sabet F, Athamneh T, et al. Cesarean section: incidence, causes, associated factors and outcomes: a national prospective study from Jordan. Gynecol Obstet Case Rep. 2017;3(3):55.
Xiao X, Wu Z-C, Chou K-C. A multi-label classifier for predicting the subcellular localization of gram-negative bacterial proteins with both single and multiple sites. PLoS ONE. 2011;6(6):e20592.
Luo ZC, Liu X, Wang A, Li JQ, Zheng ZH, Guiyu S, et al. Obstetricians’ perspectives on trial of labor after cesarean (TOLAC) under the two-child policy in China: a cross-sectional study. BMC Pregnancy Childbirth. 2021;21(1):1–11.
Hussein K, Gari A, Kamal R, Alzharani H, Alsubai N, Aljuhani T, et al. Acceptance of trial of labor after cesarean (Tolac) among obstetricians in the western region of Saudi Arabia: a cross-sectional study. Saudi J Biol Sci. 2021;28(5):2795–801.
Obstetricians ACo, Gynecologists. ’Committee on Practice Bulletins—Obstetrics in collaboration with William Grobman, MD (2019) ACOG Practice Bulletin No. 205: vaginal birth after cesarean delivery. Obstet Gynecol. 2019;133(2):e110–e27.
Li Y-X, Bai Z, Long D-J, Wang H-B, Wu Y-F, Reilly KH, et al. Predicting the success of vaginal birth after caesarean delivery: a retrospective cohort study in China. BMJ Open. 2019;9(5):e027807.
Ryan GA, Nicholson SM, Morrison JJ. Vaginal birth after caesarean section: current status and where to from here? Eur J Obstet Gynecol Reprod Biol. 2018;224:52–7.
Lundgren I, Healy P, Carroll M, Begley C, Matterne A, Gross MM, et al. Clinicians’ views of factors of importance for improving the rate of VBAC (vaginal birth after caesarean section): a study from countries with low VBAC rates. BMC Pregnancy Childbirth. 2016;16(1):1–10.
Metz TD, Berghella V, Barss V. Choosing the route of delivery after cesarean birth. U: UpToDate, Post TW ur UpToDate Waltham, MA: UpToDate. 2019.
Rezai S, Labine M, Gottimukkala S, Karp S, Sainvil L. Trial of labor after cesarean (TOLAC) for vaginal birth after previous cesarean section (VBAC) versus repeat cesarean section: a review. Obstet Gynecol Int J. 2016;4(6):00135.
Dy J, DeMeester S, Lipworth H, Barrett J. No. 382-trial of labour after caesarean. J Obstet Gynaecol Can. 2019;41(7):992–1011.
Tilden EL, Cheyney M, Guise JM, Emeis C, Lapidus J, Biel FM, et al. Vaginal birth after cesarean: neonatal outcomes and United States birth setting. Am J Obstet Gynecol. 2017;216(4):403 e1-e8.
Lundgren I, Smith V, Nilsson C, Vehvilainen-Julkunen K, Nicoletti J, Devane D, et al. Clinician-centred interventions to increase vaginal birth after caesarean section (VBAC): a systematic review. BMC Pregnancy Childbirth. 2015;15(1):1–9.
Mooney SS, Hiscock R, Clarke IDA, Craig S. Estimating success of vaginal birth after caesarean section in a regional Australian population: validation of a prediction model. Aust N Z J Obstet Gynaecol. 2019;59(1):66–70.
Levin G, Meyer R, Mor N, Yagel S, David M, Yinon Y, et al. Trial of labor after cesarean in adolescents–a multicenter study. J Pediatr Adolesc Gynecol. 2020;33(4):398–402.
Uno K, Mayama M, Yoshihara M, Takeda T, Tano S, Suzuki T, et al. Reasons for previous Cesarean deliveries impact a woman’s independent decision of delivery mode and the success of trial of labor after Cesarean. BMC Pregnancy Childbirth. 2020;20(1):1–8.
Tahseen S, Griffiths M. Vaginal birth after two caesarean sections (VBAC-2)—a systematic review with meta-analysis of success rate and adverse outcomes of VBAC-2 versus VBAC-1 and repeat (third) caesarean sections. BJOG. 2010;117(1):5–19.
Ali IJA, Neamah DA, Hussein MN. Successful vaginal birth after caesarian section and maternal outcome. 2019.
Habak PJ, Kole M. Vaginal birth after cesarean delivery. StatPearls: StatPearls Publishing; 2020.
Kurtz CM, Picker AR. Risks and benefits of trial of labor after cesarean when compared to elective repeat cesarean section in rural facilities. 2019.
Sahin S, Ozkaya E, Eroglu M, Sanverdi I, Celik Z, Cakıroglu A. Predictors of successful vaginal birth after a caesarean in women with a previous single caesarean delivery. Eur Rev Med Pharmacol Sci. 2022;26(5):1594–600.
Eleje GU, Okam PC, Okaforcha EI, Anyaoku CS. Rates and determinants of successful vaginal birth after a previous caesarean section: a prospective cohort study. ARC J Gynecol Obstet. 2019;4:1–8.
Grobman WA, Sandoval G, Rice MM, Bailit JL, Chauhan SP, Costantine MM, et al. Prediction of vaginal birth after cesarean delivery in term gestations: a calculator without race and ethnicity. Am J Obstet Gynecol. 2021;225(6):664 e1-e7.
Smithies M, Woolcott CG, Brock JAK, Maguire B, Allen VM. Factors associated with trial of labour and mode of delivery in Robson group 5: a select group of women with previous caesarean section. J Obstet Gynaecol Can. 2018;40(6):704–11.
Vishesha Y, Vidyadhar B, Sai B, Neha Y. Predictors of successful vaginal birth after caesarean section. Indian J Basic Appl Med Res. 2017;6(4):380–8.
Wu Y, Kataria Y, Wang Z, Ming W-K, Ellervik C. Factors associated with successful vaginal birth after a cesarean section: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019;19(1):1–12.
Girma HT, Mekonnen H, Sendo EG, Deressa JT. Factors associated with successful vaginal birth after cesarean section and its outcome in Asella referral and teaching Hospital, Ethiopia. Int J. 2021;7(1):39.
Mekonnin FT, Bulto GA. Determinants of successful vaginal birth after caesarean section at public hospitals in Ambo Town, Oromia Region, Central Ethiopia: a case-control study. Risk Manag Healthc Policy. 2021;14:4083.
Dereje L, Tilahun T, Markos J. Determinants of successful trial of labor after a previous cesarean delivery in East Wollega, Western Ethiopia: A case–control study. SAGE open medicine. 2022;10:20503121221097596.
Siraneh Y, Assefa F, Tesfaye M. Feto-maternal outcome of vaginal birth after cesarean and associated factors among mothers with previous cesarean scar at Attat Lord Merry Primary Hospital, Gurage Zone, South Ethiopia. J Pregnancy Child Health. 2018;5(5):390.
Girma Y, Menlkalew Z, Destaw A. Vaginal delivery after caesarean section and its associated factors in Mizan Tepi University Teaching Hospital, Southwest Ethiopia. Heliyon. 2021;7(11):e08276.
Misgan E, Gedefaw A, Negash S, Asefa A. Validation of a vaginal birth after cesarean delivery prediction model in teaching hospitals of Addis Ababa University: a cross-sectional study. BioMed Res Int. 2020;2020:1540460.
Birara M, Gebrehiwot Y. Factors associated with success of vaginal birth after one caesarean section (VBAC) at three teaching hospitals in Addis Ababa, Ethiopia: a case control study. BMC Pregnancy Childbirth. 2013;13(1):1–6.
Tefera M, Assefa N, Teji Roba K, Gedefa L. Predictors of success of trial of labor after cesarean section: a nested case–control study at public hospitals in Eastern Ethiopia. Womens Health. 2021;17:17455065211061960.
Kalok A, Zabil SA, Jamil MA, Lim PS, Shafiee MN, Kampan N, et al. Antenatal scoring system in predicting the success of planned vaginal birth following one previous caesarean section. J Obstet Gynaecol. 2018;38(3):339–43.
Trojano G, Damiani GR, Olivieri C, Villa M, Malvasi A, Alfonso R, et al. VBAC: antenatal predictors of success. Acta Bio Medica: Atenei Parmensis. 2019;90(3):300.
Senturk MB, Cakmak Y, Atac H, Budak MS. Factors associated with successful vaginal birth after cesarean section and outcomes in rural area of Anatolia. Int J Women’s Health. 2015;7:693.
Rossi A, Prefumo F. Pregnancy outcomes of induced labor in women with previous cesarean section: a systematic review and meta-analysis. Arch Gynecol Obstet. 2015;291(2):273–80.
Eide KT, Morken N-H, Bærøe K. Maternal reasons for requesting planned cesarean section in Norway: a qualitative study. BMC Pregnancy Childbirth. 2019;19(1):1–10.
Ryding EL, Lukasse M, Kristjansdottir H, Steingrimsdottir T, Schei B, Group BS. Pregnant women’s preference for cesarean section and subsequent mode of birth–a six-country cohort study. J Psychosom Obstet Gynecol. 2016;37(3):75–83.
La Verde M, Cobellis L, Torella M, Morlando M, Riemma G, Schiattarella A, et al. Is uterine myomectomy a real contraindication to vaginal delivery? Results from a prospective study. J Invest Surg. 2022;35(1):126–31.
Alani WY, Dayoub N. Factors influencing successful vaginal birth after cesarean delivery. Bahrain Med Bull. 2017;158(5879):1–5.
Nicholas SS, Orzechowski KM, Berghella V, Baxter JK. Second trimester cervical length and its association with vaginal birth after cesarean delivery. Am J Perinatol. 2016;2(01):020–3.
Metz T, Stoddard G, Henry E, Jackson M, Holmgren C, Esplin S. Simple, validated vaginal birth after cesarean delivery prediction model for use at the time of admission. Obstet Anesth Dig. 2014;34(3):158–9.
Durnwald CP, Mercer BM. Vaginal birth after Cesarean delivery: predicting success, risks of failure. J Matern Fetal Neonatal Med. 2004;15(6):388–93.
Acknowledgements
Not applicable
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
BDM hypothesized and designed the review, developed the proposal, was involved in the data extraction, performed data analysis, and drafted the manuscript. AAA assisted in the design of the review, writing the proposal, quality appraisal, data extraction, data analysis, and interpretation of the findings. Finally, both authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA 2020 checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mekonnen, B.D., Asfaw, A.A. Predictors of successful vaginal birth after a cesarean section in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth 23, 65 (2023). https://doi.org/10.1186/s12884-023-05396-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05396-w