Abstract
Background
Despite an increase in institutional births and a fall in maternal mortality, the satisfaction of women with their birthing experience in public health institutions is low. Birth Companion (BC) is an important part of the Labour Room Quality Improvement Initiative introduced by the Government of India in 2017. Despite mandates, its implementation has been unsatisfactory. Little is known about the perception of healthcare providers about BC.
Methods
We conducted a facility-based, cross-sectional quantitative study with doctors and nurses in a tertiary care hospital in Delhi, India to gauge their awareness, perception and knowledge about BC. Following universal total population sampling, the participants were administered a questionnaire, which was completed by 96 of 115 serving doctors (response rate of 83%), and 55 of 105 serving nurses (response rate of 52%).
Results
Most (93%) healthcare providers were aware of the concept of BC, WHO’s recommendation (83%) and Government’s instructions (68%) on BC during labour. A woman’s mother was the BC of choice (70%) closely followed by her husband (69%). Ninety-five percent of providers agreed that the presence of a BC during labour will be beneficial, in providing emotional support, boosting the woman’s confidence, providing comfort measures, helping in the early initiation of breastfeeding, reducing post-partum depression, humanizing labour, reducing the need for analgesia and increasing chances of spontaneous vaginal births. Yet, support for the introduction of BC in their hospital was low due to institutional barriers like overcrowding, lack of privacy, hospital policy, risk of infection; privacy issues and costs.
Conclusions
Widespread adoption of the concept of BC would require, besides directives, a buy-in by the providers, and action on their suggestions. These include greater funding for hospitals, creating physical partitions to ensure privacy, sensitization and training of health providers and BC, incentivizing hospitals and birthing women, formulation of guidelines on BC, standards setting and a change in institutional culture.
Similar content being viewed by others
Background
Skilled care in pregnancy and childbirth is considered necessary to improve birth outcomes [1]. Globally, a 31% increase (64% to 84%) [2] in skilled birth attendance during the period 2001–2021 was accompanied by a 38% decline (342 to 211 per 100,000 live births) in maternal mortality during 2000–2017 [3]. In India, the change has been dramatic with institutional births increasing 2.6 times (from 33.6% in 1998–99 [4] to 88.6% in 2019–21 [5]) and the Maternal Mortality Ratio (MMR) dropping by three-quarters during this period from 398 to 99 [6].
Despite this progress, many women face disrespectful treatment from healthcare providers in the form of physical, verbal and emotional abuse, neglect and disrespect [7, 8] leading to a low satisfaction among women birthing in public health institutions [9, 10]. This also negatively influences maternal and newborn outcomes [11]. Fear of being alone in unfamiliar surroundings, in contrast to ‘safe and reassuring environment’ at home, compels some women to give birth at home [12, 13].
Respect for human rights includes the right to self-determination and privacy embodied in the idea of Respectful Maternity Care (RMC), which also includes a companion of choice throughout labour [14, 15]. Presence of a Birth Companion (BC) in labour is known to lead to a shorter duration of labour [16]. Continuous, one‐to‐one intrapartum support during labour can improve outcomes for women and infants, including spontaneous vaginal birth, shorter duration of labour, and less likelihood of caesarean birth, instrumental vaginal birth, use of any analgesia, low five‐minute Apgar score and negative childbirth experience [17]. WHO’s intrapartum guidelines recommend a “positive childbirth experience for all women undergoing labor, which includes a clinically and psychologically safe environment with continuity of practical and emotional support from a birth companion” [15]. WHO strongly advocates for the presence of a BC of choice during childbirth [18,19,20].
BC have been found to be feasible and well accepted by health providers and the birthing women in a pilot study in Tanzania [21]. Another cross-sectional study in Tanzania concluded that health providers are the gatekeepers of companionship, and their work environment influences providers’ allowance of companionship [22]. Concluding that the consultants often decide policy, a Sri Lankan study underlined the need to improve awareness of BC among the practitioners [23]. Hence, many countries like Sri Lanka, [24] Tanzania, [25] Brazil, [26] Kenya [27] have supported BC in their public facilities.
In India, despite the 2016 advisory of the health ministry permitting BC during childbirth in Public Health facilities, [28] only some states like Tamil Nadu (2002), [29, 30] Kerala, [31, 32] and Punjab [33] have supported BC in their public facilities. A Labour Room Quality Improvement Initiative (LaQshya) [34] was thus launched in 2017 in all Medical Colleges, District Hospitals, First Referral Units, and Community Health Centers to ‘fast-track’ the interventions for RMC through a system of certification and monetary incentive to institutions [35]. Though the original plan was to “achieve tangible results within 18 months”, only 27% of the Labour Rooms (410) and Maternity Operation Theatres (337) [36] of the 2805 identified facilities in the country [37] had obtained the National level certification by September, 2021.
Slow progress in the introduction of BC has been globally attributed to several factors. These include a lack of awareness among the healthcare providers of the benefits associated with the practice, concerns among the healthcare providers, health system factors, lack of physical space in the labour room and the volume of work [23]. Other factors include hospital policy, [38] embarrassment, fear of gossip and privacy concerns [39].
Little is known in India about the awareness or the perception of healthcare providers about BC, beyond a few studies [40]. We conducted this facility based study to fill this gap in evidence on the awareness, perception and knowledge among healthcare providers regarding BC. Our study objectives were:
-
1.
To assess the level of awareness among the entire spectrum of caregivers in a tertiary care teaching hospital in India of the concept and benefits of a BC during labour and childbirth.
-
2.
To understand their perception of the barriers to supporting the presence of BC during labour and childbirth in an institutional setting.
-
3.
To gather suggestions from caregivers on how these barriers could be overcome.
Methods
Design
We conducted this facility based, cross-sectional study using quantitative survey methods. The rationale behind this study design was to collect data from a large pool of participants in a limited time period.
Setting
The study was conducted in June and July of 2019 in the Department of Obstetrics & Gynecology, Lok Nayak Hospital, Maulana Azad Medical College, New Delhi, India, which is one of the largest medical institutes in the country. It hosts over 1500 childbirths per month. Around eight to ten women are in labour at any point of time, with two to three doctors posted in each shift, round the clock. The obstetrics ward has forty beds, while the labour room has fifteen beds. Women are triaged at the time of admission. Women in early labour (upto 4 cm of cervical dilatation) are admitted to the wards, and those in an advanced stage of labour are admitted directly to the labour room.
Participants
The study population consisted of all the medical and nursing healthcare providers involved in providing institutional care during labour and birthing, including obstetric Consultants, Senior Residents, Post- Graduate doctors and all grades of nursing Staff.
Sampling involved "Universal total population sampling” [41] whereby all individuals belonging to the study population and present at the time of the study were approached for participation by sharing the Study Participant Information Sheet (Additional file, Annexure 1). This was done to eliminate any selection bias or sampling error. Those healthcare providers who expressed willingness to participate were given the Consent Form (Additional file, Annexure 2) for signature. These respondents were then handed over a printed questionnaire with a request to enter their response. Filled response sheets, along with consent forms, were personally collected from the participants. Since the PI was an Undergraduate student, her involvement in the interview and data collection could not have placed the participants under any coercion.. Of 115 doctors, 96 completed the questionnaire (response rate of 83%), while 55 of 105 nurses completed the questionnaire (response rates of 52%). With a sample of 151, our overall response rate was 69%. Most (95%) of the respondents were females.
Ethical clearance
The Institutional Ethics Committee of Maulana Azad Medical College accorded clearance for the study (order No. F.17/IEC/MAMC/19/No. 125 Dated 27.5.2019). Prior to canvassing of the questionnaire, informed consent of the willing respondents was obtained in writing. Complete confidentiality of the participants and their responses was maintained by giving each respondent an ID number and not sharing any personal identifiers. Participants were given the choice to opt out of the study without any condition.
Study instrument
Based on a thorough literature review, a 15 point study questionnaire was framed, and pre-tested on 10 subjects, before its finalization (Additional file, Annexure 3). The first three questions captured the socio-demographic characteristics and position of participants in the department. Questions 4–10 related to awareness of the concept and benefits of BC. Subsequent questions numbered 11–15 were on their perception of the barriers and suggestions.
Data analysis
The information collected was entered in a Google form, and results downloaded as a Comma Separated Values (csv) file. Data were checked for consistency and completeness; data entry errors were spotted and corrected. Cleaned data were analyzed in Stata 8.0. Labels were assigned to variables. Ordinal variables were coded in a consistent, hierarchical manner with a score of one (1) denoting full awareness, highly beneficial or strong agreement.
Our questionnaire elicited responses on awareness, benefits, barriers, suggestions and applicability of the concept of BC in the hospital. Any systematic differences in outcomes by demographic variables or position in the department were ascertained.
The study data contained responses of participants to various questions – either as binary, or on an ordinal scale of an order of three or five. Since ordinal variables and differences between them are neither uniform nor can be assumed to be normally distributed, standard measurements methods like means, standard deviations and t-test were not suitable [42]. Instead, we used non-parametric tests [43] like Pearson Chi Square statistic, Kendall's tau-b, Kruskal’s gamma statistic and Kruskal–Wallis test that do not rely on the assumption of normal distribution. We also calculated the median and percentages. Fisher’s exact test was applied to tables with cell values less than five, Quantile regression was used for a similar reason. P-value of less than 0.05 was considered significant.
Results
Two third of the respondents (64%) were doctors (10 consultants, 47 Post-Graduates, 39 residents), and the remainder were nurses (15 senior nurses and 40 staff nurses). The participants were aged 21 to 55 years, with a mean age of 31 years (Table 1).
Awareness of birth companion among healthcare providers
Awareness of the concept of BC was high with 53% of respondents being fully aware and 40% being somewhat aware (overall: 93%). Similarly, awareness of WHO’s recommendation of the presence of BC during labour was high with 54% respondents being fully aware and 29% being partially aware (overall: 83%).
Median awareness for both questions was 1, denoting full awareness on a three point scale with 3 being not aware. Sub-group analysis revealed that consultants and staff nurses had the highest level of awareness (mean and median awareness was 1 and close to 1).
The awareness of BC and WHO’s recommendation were highly correlated with a Pearson Chi Square statistic of 55.6 with a p-value of < 0.001 denoting a high level of overlap of the awareness of the concept and the guidelines on it (Table 2).
Similarly, Fisher’s exact test also showed dependence of the response to the two questions (p = 0.00). Kendall's tau-b coefficient to test the strength of the association of cross tabulations showed an Alpha’s Standard Error (ASE) of 0.072 denoting dependence of two sets of responses. Kruskal’s gamma statistic at 0.62 and ASE of 0.091 also similarly showed a material level of association.
On the question of awareness of the Government’s guideline on the presence of BC (Q.6), awareness levels were slightly lower with 39% being fully aware, while 29% were somewhat aware (overall awareness: 68%) and an overall median score of 2. Consultants were still highly aware of this stipulation, while senior nurses were least aware of it.
Of those who were fully aware of the concept of BC, 71% were also fully aware of the WHO’s recommendation (Table 2) and 56% were fully aware that Government of India advocates the presence of BC (Table 3). The association to the responses of awareness of the concept of BC and the Government’s advisory was significant with a Pearson Chi Square statistic (χ2) with 4 degrees of freedom of 29.6 (p-value: 0.00), Fisher’s exact test p-value of 0.00, Kendall's tau-b of 0.37 (ASE: 0.067), Kruskal’s gamma statistic at 0.58 and ASE of 0.091 (Table 3).
Similarly, 62% of respondents were fully aware of WHO’s recommendation as well as the Government’s advisory; these responses were significantly correlated with a Pearson Chi Square statistic (χ2) with 4 degrees of freedom of 64.5 (p-value: 0.00), Fisher’s exact test p-value of 0.00, Kendall's tau-b of 0.56 (ASE: 0.054), Kruskal’s gamma statistic at 0.78 and ASE of 0.057 (Table 4).
Preferred BC of choice
Respondents were asked to choose the preferred BC from a list, allowing multiple selections. A woman’s mother was the BC of choice (70%) closely followed by a husband (69%). Other preferences included sister (46%), nurse (43%), mother-in-law (34%), friend (30%) and doctor (28%).
Pre-requisites for a BC
The pre-requisite for being a BC were identified as wearing clean clothes (95%), not suffering from any communicable disease (91%), and staying with the woman throughout the process of labour (74%). Less than half of the respondents opted for a BC having gone through the process of labour (42%), or being a female relative (40%).
Perceived benefits of a BC
Respondents were then asked about their knowledge of the likely benefits of a BC Just over half of the respondents (51%) viewed BC to be highly beneficial; many (44%) felt it was somewhat beneficial (Table 5) with an overall median score of 1. Most Consultants, Post-Graduates and Senior Nurses opined it to be highly beneficial with a median score of 1. Residents and Staff Nurses were muted in their response and believed BC would be somewhat beneficial.
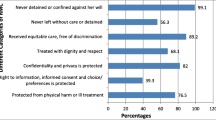
Almost all respondents (99%) were of the opinion that BC would provide emotional support and boost the woman’s confidence (Table 5). More than 90% of participants were of the opinion that the BC would provide comfort, spiritual support, increase satisfaction, help in early initiation of breastfeeding, be an advocate for a woman’s wishes, and reduce postpartum depression. A majority of the respondents thought that BC would lead to humanization of labour, reduce the need for analgesia, unnecessary cesarean sections, and instrumental childbirth, reduce the workload for the hospital staff, increase spontaneous vaginal births and help in enabling a woman birth in her position of choice. Half the respondents thought that it would lead to a higher newborn Apgar score. Some respondents expected BC to lead to a shorter duration of labour (38%), or reduced intra-partum bleeding (36%) or increased use of partograph (26%, Table 5).
Though most respondents thought that BC could be “somewhat beneficial” in dealing with high risk pregnancies, Consultants viewed BC to be “highly beneficial” in this regard.
Readiness for introducing BC in the hospital
Seeking readiness for practice, respondents were asked if the concept of BC should be introduced in their institution. Only 19% of respondents strongly agreed while 40% agreed to this suggestion (Table 6, Fig. 1). The median response was “Agree”. This response was less favorable than to the question on the expected benefits of a BC where the overall perception was “highly beneficial”.
Comparison of perceived benefits versus readiness to introduction
Only 75% of the respondents who indicated that they thought BC as highly beneficial agreed to the suggestion of it being implemented in their hospital (Table 6). A smaller percentage of respondents (45%) who observed BC to be somewhat beneficial agreed to its introduction in their hospital (Table 6). These responses to the questions on expected benefits of BC and introducing it in their hospital were significantly related with a Pearson Chi Square statistic (χ2) with 8 degrees of freedom of 38.9 (p- value: 0.00), Cramér's V of 0.35, Kendall's tau-b of 0.37 (ASE: 0.064), Kruskal’s gamma statistic at 0.56 and ASE of 0.08 (Table 6).
Barriers to BC perceived by healthcare providers
Key barriers to the introduction of a BC at the institution level included overcrowding in the labour room and privacy concerns for other women, especially in the presence of a male companion. Most respondents also “agreed” with the suggestion that hospital policy could be a barrier, and that BC posed a risk of infection; interference in clinical decisions, and issues of confidentiality. Personal barriers included embarrassment in giving birth in front of someone else, lack of access to a trustworthy person and economic loss due to the expense of hiring such a person.
Suggestions from caregivers on overcoming barriers
On overcoming barriers to the introduction of BC, most respondents strongly agreed to the suggestions for increasing awareness among the hospital staff, providing funding to hospitals, creating physical partitions to ensure privacy, prior training of BC on their role, incentivizing women and hospitals, and formulation of guidelines.
Consultants were the most supportive (Fig. 2) while staff nurses were the least approving of the idea of introducing BC in their institution. Kruskal–Wallis one-way analysis of variance to test the null hypothesis that the medians of all groups are equal was rejected with a Chi-Square value of 16.8 (p-0.001). Using quantile regression which estimates the median of the dependent variable, conditional on the values of the independent variable, we found that as we move lower in the healthcare worker hierarchy, the support for the introduction of BC in their hospital falls (coefficient: 0.33, t: 5.59, p: 0.00).
Discussion
Our respondents covered the full spectrum of doctor and nurse healthcare providers who possessed a diverse experience in managing labour and childbirth in a large, tertiary care hospital with a high case load of childbirths. A consensus or broad agreement among such a broad group of care-givers signifies a widely held view and therefore carries a high degree of credibility, and generalizability.
With the advent of the COVID-19 pandemic, maternal and child health services have suffered a setback [44]. The mental health of pregnant women has also been affected [45]. BC can be utilized to minimize avoidable woman-clinician interface, optimize manpower at this critical time and help the birthing women cope with the dual challenge.
Thus, the possibility of improved maternal and neonatal outcomes by supporting the presence of a BC has immense public health importance, particularly in the face of COVID-19 pandemic.
Even though the choice remains with a birthing woman, caregivers in our study identified the mother and husband as the most preferred BC. These findings are similar to those of a study in Nigeria [46]. The Government of India in 2016 suggested that BC be a female relative, preferably one who has undergone the process of labor, be free of communicable diseases, wear clean clothes, not interfere in the work of hospital staff and not attend to other women [34].
Since women’s childbirth satisfaction is closely dependent on ensuring privacy [10], policy and systems for permitting BC should allow for sufficient privacy for other women giving birth in the same ward in the presence of a BC of any gender.
The prerequisites identified for a BC include basics like hygiene, being disease-free and their availability. While introducing the concept of BC, screening for communicable diseases and coaching on maintaining hygiene can be beneficial.
High levels of awareness of BC were matched among 95% of respondents to its expected benefits. Consultants perceived that BC was highly beneficial in high risk pregnancies. In our study, 70% of respondents felt that the presence of a BC would reduce the need for analgesia. Our findings are consistent with those from a study in Kenya [39] and Sri Lanka [23] as well as those from other studies [47] and a Cochrane review [17].
Despite fairly high levels of awareness, usefulness and perceived benefits of BC, only 61% of respondents who perceived BC to be beneficial agreed to its introduction in their hospital. Staff nurses were the least agreeable, with only 40% of those who agreed that BC were beneficial agreed to its introduction. Nurses as a group compared to doctors had a statistically significant disagreement in their response on introducing BC (Z = -2.183; p = 0.03). The reasons for this difference between awareness and willingness to practice, and among the classes of caregivers, points to practical difficulties in introducing BC. These difficulties are captured in response to the questions on barriers and how these can be overcome.
Respondents of all categories strongly agreed that the key barrier to introducing BC in their hospital was overcrowding and privacy concerns for other women. This is similar to other studies from Kenya [39] and Sri Lanka [23]. That lack of physical space leading to privacy issues was the key constraint in introducing BC is supported by funding for hospitals emerging as the most preferred response to the question on overcoming these barriers. Our findings are consistent with WHO’s recommendation on the need for implementing a strategy to sensitize health professionals, community and women towards the acceptance of the concept of BC [20, 39].
The strengths of this study are – universal total sampling with a relatively high response rate thus reducing selection bias; the limitation of our study is that its findings are only generalizable to tertiary care teaching institutions. Larger studies across institutions at all levels of healthcare in different socio-cultural settings are required.
In general, awareness among participants about the concept of BC was fairly high. Awareness, however, needs to be raised further.
There was a broad agreement that the concept of BC should be introduced in a tertiary care institution. For this to happen, barriers to implementation need to be identified, stakeholders engaged [48] and an action plan drawn and implemented.
Based on this study, we make the following recommendations:
-
1.
The concept of BC should be part of the teaching curriculum for postgraduate medical and nursing students, which should be updated from time to time through Continuing Medical Education.
-
2.
All cadres of staff working in labour rooms should be sensitized about the LaQshya program.
-
3.
Pregnant women should be informed during antenatal visits of the benefits of a BC, and their right to have a BC of their choice.
-
4.
A BC should be encouraged to accompany a pregnant woman for antenatal visits, who should be screened and counseled to prepare them for this role.
-
5.
Infrastructure in health facilities should be strengthened so that it is conducive to the presence of BC. Available funds should be used to provide temporary partitions or curtains to create privacy for the women and their BC during birthing.
-
6.
India’s prescribed National Quality Assurance Standards for Public Health facilities already requires (Standard B3) that the facility maintains the privacy, confidentiality & dignity of women. This needs to be implemented diligently. Hospitals that allow BC should be incentivized.
-
7.
Key stakeholders need to be engaged while drawing the action plan, and for its effective implementation.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- BC:
-
Birth Companion
- LaQshya:
-
Labour Room Quality Improvement Initiative
References
Gülmezoglu AM, Lawrie TA, Hezelgrave N, Oladapo OT, Souza JP, Gielen M, Lawn JE, Bahl R, Althabe F, Colaci D and Hofmeyr GJ: Interventions to Reduce Maternal and Newborn Morbidity and Mortality. 2016. p. 115–36. Availabe from https://elibrary.worldbank.org/doi/10.1596/978-1-4648-0348-2_ch7.
UNICEF: Global delivery care coverage and trends: Percentage of births assisted by a skilled birth attendant, by country, 2013–2018. 2019. Available from https://data.unicef.org/topic/maternal-health/delivery-care/.
UNICEF: Maternal mortality declined by 38 per cent between 2000 and 2017. UNICEF DATA. 2022. Available from https://data.unicef.org/topic/maternal-health/maternal-mortality.
IIPS: INDIA National Family Health Survey (NFHS-2). 1999. Available from http://rchiips.org/nfhs/data/india/keyfind.pdf.
IIPS: National Family Health Survey - 5 (2019–21): India Fact Sheet. 2021. Available from http://rchiips.org/nfhs/NFHS-5_FCTS/India.pdf.
Meh C, Sharma A, Ram U, Fadel S, Correa N, Snelgrove JW, Shah P, Begum R, Shah M, Hana T, Fu SH, Raveendran L, Mishra B, Jha P. Trends in maternal mortality in India over two decades in nationally representative surveys. BJOG. 2022;129(4):550–61. https://doi.org/10.1111/1471-0528.16888. Epub 2021 Sep 15.
Bohren MA, Hunter EC, Munthe-Kaas HM, Souza JP, Vogel JP, Gülmezoglu AM. Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis. Reprod Health. 2014;11(1):71. https://doi.org/10.1186/1742-4755-11-71.
Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, Aguiar C, Saraiva Coneglian F, Diniz AL, Tunçalp Ö, Javadi D, Oladapo OT, Khosla R, Hindin MJ, Gülmezoglu AM. The Mistreatment of Women during Childbirth in Health Facilities Globally: A Mixed-Methods Systematic Review. PLoS Med. 2015;12(6):e1001847. https://doi.org/10.1371/journal.pmed.1001847.
Mekonnen ME, Yalew WA, Anteneh ZA. Women's satisfaction with childbirth care in Felege Hiwot Referral Hospital, Bahir Dar city, Northwest Ethiopia, 2014: cross sectional study. BMC Res Notes. 2015;8:528. https://doi.org/10.1186/s13104-015-1494-0.
Jha P, Larsson M, Christensson K, Skoog Svanberg A. Satisfaction with childbirth services provided in public health facilities: results from a cross- sectional survey among postnatal women in Chhattisgarh, India. Glob Health Action. 2017;10(1):1386932. https://doi.org/10.1080/16549716.2017.1386932.
Miller S, Cordero M, Coleman AL, Figueroa J, Brito-Anderson S, Dabagh R, Calderon V, Cáceres F, Fernandez AJ, Nunez M. Quality of care in institutionalized deliveries: the paradox of the Dominican Republic. Int J Gynaecol Obstet. 2003;82(1):89–103; discussion 87-8. https://doi.org/10.1016/s0020-7292(03)00148-6.
Devasenapathy N, George MS, Ghosh Jerath S, Singh A, Negandhi H, Alagh G, Shankar AH, Zodpey S. Why women choose to give birth at home: a situational analysis from urban slums of Delhi. BMJ Open. 2014;4(5):e004401. https://doi.org/10.1136/bmjopen-2013-004401.
Hameed W, Avan BI. Women's experiences of mistreatment during childbirth: A comparative view of home- and facility-based births in Pakistan. PLoS One. 2018;13(3):e0194601. https://doi.org/10.1371/journal.pone.0194601.
WhiteRibbonAlliance: Respectful Maternity Care: The Universal Rights of Childbearing Women. Maternal Health Task Force. 2014. Available from https://www.mhtf.org/document/respectful-maternity-care-the-universal-rights-of-childbearing-women.
WHO: The prevention and elimination of disrespect and abuse during facility-based childbirth. World Health Organization. 2014. p. 1–4. Available from https://www.who.int/publications/i/item/WHO-RHR-14.23.
Yuenyong S, O'Brien B, Jirapeet V. Effects of labor support from close female relative on labor and maternal satisfaction in a Thai setting. J Obstet Gynecol Neonatal Nurs. 2012;41(1):45–56. https://doi.org/10.1111/j.1552-6909.2011.01311.x.
Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017;7(7):CD003766. https://doi.org/10.1002/14651858.CD003766.pub6.
WHO In: WHO, editors. Support During Labour and Childbirth in Counselling for Maternal and Newborn Health Care: A Handbook for Building Skills. WHO; 2013. chap. 10. Available from https://www.who.int/publications/i/item/9789241547628.
Committee GR and WHO: WHO recommendations: intrapartum care for a positive childbirth experience. World Health Organization. 2018. p. 1–238. Available from https://www.who.int/publications/i/item/9789241550215.
WHO: Companion of choice during labour and childbirth for improved quality of care. World Health Organization. 2020:1–7. Available from https://www.who.int/publications/i/item/WHO-SRH-20.13.
Chaote P, Mwakatundu N, Dominico S, Mputa A, Mbanza A, Metta M, Lobis S, Dynes M, Mbuyita S, McNab S, Schmidt K, Serbanescu F. Birth companionship in a government health system: a pilot study in Kigoma, Tanzania. BMC Pregnancy Childbirth. 2021;21(1):304. https://doi.org/10.1186/s12884-021-03746-0.
Dynes MM, Binzen S, Twentyman E, Nguyen H, Lobis S, Mwakatundu N, Chaote P, Serbanescu F. Client and provider factors associated with companionship during labor and birth in Kigoma Region, Tanzania. Midwifery. 2019;69:92–101. https://doi.org/10.1016/j.midw.2018.11.002. Epub 2018 Nov 13.
Senanayake H, Wijesinghe RD, Nayar KR. Is the policy of allowing a female labor companion feasible in developing countries? Results from a cross sectional study among Sri Lankan practitioners. BMC Pregnancy Childbirth. 2017;17(1):392. https://doi.org/10.1186/s12884-017-1578-z.
Ministry#of#Health, Sri Lanka: National Strategic Plan Maternal and Newborn Health (2017 -2025). Accessed from https://srilanka.unfpa.org/sites/default/files/pub-pdf/Maternal%20%26%20Newborn%20Strat%20Plan%20-%20FINAL15-12-17%20%282%29.pdf.
BloombergPhilanthropies: For moms everywhere this Mother's Day: Birth companionship in remote Tanzania vert Bloomberg Philanthropies. 2022. https://www.bloomberg.org/blog/for-moms-everywhere-this-mothers-day-birth-companionship-in-remote-tanzania.
Diniz CS, d'Orsi E, Domingues RM, Torres JA, Dias MA, Schneck CA, Lansky S, Teixeira NZ, Rance S, Sandall J. Implementation of the presence of companions during hospital admission for childbirth: data from the Birth in Brazil national survey. Cad Saude Publica. 2014;30 Suppl 1:S1-14. English, Portuguese. https://pubmed.ncbi.nlm.nih.gov/25167174/.
MinistryofMedicalSciencesKenya: National Guidelines for Quality Obstetrics and Perinatal care, 2010. Available from http://guidelines.health.go.ke/#/category/27/91/meta.
PIB: Health Ministry allows Birth Companions during Delivery in Public Health facilities. 2016. Available from https://pib.gov.in/newsite/PrintRelease.aspx?relid=136801.
Padmanaban P, Raman PS, Mavalankar DV. Innovations and challenges in reducing maternal mortality in Tamil Nadu, India. J Health Popul Nutr. 2009;27(2):202–19. https://doi.org/10.3329/jhpn.v27i2.3364.
WHO-SEARO: Safer Pregnancy in Tamil Nadu: from Vision to Reality. 2009. Available from https://apps.who.int/iris/handle/10665/205877.
TheSwaddle: Kerala Now Allowing Birth Companions in the Delivery Room. 2018. Available from https://theswaddle.com/kerala-now-allowing-birth-companions-in-the-delivery-room/.
Gopinathan S: Women can have a ‘companion’ in the labour room: Kerala starts scheme in govt hospitals. 2018. Available from https://www.thenewsminute.com/article/women-can-have-companion-labour-room-kerala-starts-scheme-govt-hospitals-88885.
ETHealthWorld: PUNJAB : Women to be allowed a companion during delivery. ETHealthworld.com. 2015. Available from https://health.economictimes.indiatimes.com/news/policy/punjab-women-to-be-allowed-a-companion-during-delivery/48031473.
MoHFW: LAQSHYA - Labour Room Quality Improvement Initiative - 2017. 2017.Available from https://nhm.gov.in/New_Updates_2018/NHM_Components/RMNCH_MH_Guidelines/LaQshya-Guidelines.pdf.
PIB: LaQshya program will benefit every pregnant woman and newborn delivering in public health institutions. ‘Aims at achieving tangible results within 18 months’. 2018. Available from https://pib.gov.in/newsite/PrintRelease.aspx?relid=177532.
MoHFW: Annual Report 2021–22 Department of Health & Family Welfare. 2022. Available from https://main.mohfw.gov.in/sites/default/files/FinalforNetEnglishMoHFW040222.pdf.
MoHFW: Annual Report 2020–21 Department of Health & Family Welfare. 2021. Available from https://main.mohfw.gov.in/sites/default/files/Annual%20Report%202020-21%20English.pdf.
Maimbolwa MC, Sikazwe N, Yamba B, Diwan V, Ransjö-Arvidson AB. Views on involving a social support person during labor in Zambian maternities. J Midwifery Womens Health. 2001;46(4):226–34. https://doi.org/10.1016/s1526-9523(01)00134-9.
Afulani P, Kusi C, Kirumbi L, Walker D. Companionship during facility-based childbirth: results from a mixed-methods study with recently delivered women and providers in Kenya. BMC Pregnancy Childbirth. 2018;18(1):150. https://doi.org/10.1186/s12884-018-1806-1.
Singh S, Goel R, Gogoi A, Caleb-Varkey L, Manoranjini M, Ravi T, Rawat D. Presence of birth companion-a deterrent to disrespectful behaviours towards women during delivery: an exploratory mixed-method study in 18 public hospitals of India. Health Policy Plan. 2021;36(10):1552–61. https://doi.org/10.1093/heapol/czab098.
LaerdDissertation: Total population sampling. 2019. Available from http://dissertation.laerd.com/total-population-sampling.php.
Mishra P, Pandey CM, Singh U, Gupta A. Scales of measurement and presentation of statistical data. Ann Card Anaesth. 2018;21(4):419–22. https://doi.org/10.4103/aca.ACA_131_18.
QuestionPro: Ordinal Data: Definition, Analysis and Examples. 2019. Available from https://www.questionpro.com/blog/ordinal-data/.
Ahmed T, Rahman AE, Amole TG, Galadanci H, Matjila M, Soma-Pillay P, Gillespie BM, El Arifeen S, Anumba DOC. The effect of COVID-19 on maternal newborn and child health (MNCH) services in Bangladesh, Nigeria and South Africa: call for a contextualised pandemic response in LMICs. Int J Equity Health. 2021;20(1):77. https://doi.org/10.1186/s12939-021-01414-5.
Liu J, Hung P, Alberg AJ, Hair NL, Whitaker KM, Simon J, Taylor SK. Mental health among pregnant women with COVID-19-related stressors and worries in the United States. Birth. 2021;48(4):470–9. https://doi.org/10.1111/birt.12554. Epub 2021 May 19.
Morhason-Bello IO, Olayemi O, Ojengbede OA, Adedokun BO, Okuyemi OO, Orji B. Attitude and preferences of nigerian antenatal women to social support during labour. J Biosoc Sci. 2008;40(4):553–62. https://doi.org/10.1017/S0021932007002520. Epub 2007 Nov 8.
McGrath SK, Kennell JH. A randomized controlled trial of continuous labor support for middle-class couples: effect on cesarean delivery rates. Birth. 2008;35(2):92–7. https://doi.org/10.1111/j.1523-536X.2008.00221.x.
HealthKNowledge: Stakeholder engagement in policy development, including its facilitation and consideration of obstacles. 2019. Available from https://www.healthknowledge.org.uk/public-health-textbook/organisation-management/5d-theory-process-strategy-development/clinical-guidelines.
Acknowledgements
The authors would like to express sincere gratitude to the respondent healthcare providers in sparing their time for responding to our questionnaire.
Funding
This project was selected by Indian Council of Medical Research under Short Term Studentship (STS) in an open, all India competition among under-graduate medical students (Reference ID 2019- 02931). An assistance of Rs. 20,000/- was provided on successful completion of the study, and approval of the report. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
TS conceived and designed the study, prepared the instrument, administered it and wrote the paper as an undergraduate MBBS student at Maulana Azad Medical College, New Delhi. YS and ST provided inputs on draft versions of the proposal, study protocol and drafts of the paper. RS helped in statistical analysis and wrote the conclusions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional Ethics Committee of Maulana Azad Medical College accorded clearance to the conduct of the study (order No. F.17/IEC/MAMC/19/No.125 Dated 27.5.2019). All methods were performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from all subjects and/or their legal guardian(s). Complete confidentiality on the participants and their responses was maintained. The option to opt out of the study was available without any condition.
Consent for publication
Not applicable for the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sarwal, T., Sarwal, Y., Tyagi, S. et al. Healthcare providers perceptions regarding the presence of Birth Companion during childbirth at a tertiary care hospital in India. BMC Pregnancy Childbirth 23, 159 (2023). https://doi.org/10.1186/s12884-022-05327-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-05327-1