Abstract
Background
International research shows marital status impacts the mental health of pregnant women, with prenatal depression and anxiety being higher among non-partnered women. However, there have been few studies examining the relationship between marital status and prenatal mental disorders among Australian women.
Methods
This is a population-based retrospective cohort study using linked data from the New South Wales (NSW) Perinatal Data Collection (PDC) and Admitted Patients Data Collection (APDC). The cohort consists of a total of 598,599 pregnant women with 865,349 admissions. Identification of pregnant women for mental disorders was conducted using the 10th version International Classification of Diseases and Related Health Problems, Australian Modification (ICD-10-AM). A binary logistic regression model was used to estimate the relationship between marital status and prenatal mental disorder after adjusting for confounders.
Results
Of the included pregnant women, 241 (0.04%), 107 (0.02%) and 4359 (0.5%) were diagnosed with depressive disorder, anxiety disorder, and self-harm, respectively. Non-partnered pregnant women had a higher likelihood of depressive disorder (Adjusted Odds Ratio (AOR) = 2.75; 95% CI: 2.04, 3.70) and anxiety disorder (AOR = 3.16, 95% CI: 2.03, 4.91), compared with partnered women. Furthermore, the likelihood of experiencing self-harm was two times higher among non-partnered pregnant women (AOR = 2.00; 95% CI: 1.82, 2.20) than partnered pregnant women.
Conclusions
Non-partnered marital status has a significant positive association with prenatal depressive disorder, anxiety disorder and self-harm. This suggests it would be highly beneficial for maternal health care professionals to screen non-partnered pregnant women for prenatal mental health problems such as depression, anxiety and self-harm.
Similar content being viewed by others
Background
Depression [1], anxiety [2] and self-harm [3] are among the most prevalent mental health problems during pregnancy. An international umbrella review indicated that the pooled prevalence of antenatal depression was 17% in high-income countries [4], while studies conducted in Australia have reported a prevalence of depression ranging from 7–17% [5, 6]. Also, various epidemiological studies have reported the prevalence of anxiety during pregnancy ranging from 14–59% [7,8,9,10], while a study conducted in Australia have reported a 27% prevalence of antenatal anxiety [5]. These prenatal mental health problems adversely impact the mother's physical and emotional well-being [11, 12] as well as the well-being of infants and children [13]. The 2019 Australian health-economic analysis of the impact of depression and anxiety during the perinatal period estimated the costs at $877 million in the first year [14]. The 2020 Productivity Commission Mental Health Report also estimated the cost of improving perinatal mental health at an additional $18–23 million in direct expenditure [15].
Antenatal depression and anxiety can result in adverse obstetric and foetal outcomes [11, 13, 16,17,18,19], and impaired mother-infant interaction [20,21,22,23]. In addition, prenatal mental health problems have a significant association with substance use thereby potentially resulting in impaired quality of life [2, 24, 25]. Based on reports from published studies, correlates of prenatal anxiety include pregnancy loss [26,27,28], physical abuse [29,30,31], history of mental illness [30,31,32,33,34], substance abuse [27, 30, 35, 36], unplanned pregnancy [37], and low social support [38]. Further, antenatal depression has a significant association with low social support, exposure to stressful events, low income, history of abuse [5, 39, 40], unplanned pregnancy, and history of any mental illness [41, 42].
Epidemiological studies show pregnant women with marital disruption or unmarried have a higher rate of developing prenatal depression [33, 43, 44] and anxiety [33] compared to partnered women. Also, a study conducted in Brazil demonstrated that the likelihood of prenatal suicide was significantly related to lack of a cohabiting partner [45]. Conversely, some studies conducted in Italy [46], UK [47] and US [48] report a non-significant association between marital status and prenatal depression. Further, a study conducted in China reported a non-significant association between marital status and prenatal anxiety [49].
Nonetheless, partnered pregnant women living in poor-quality relationships with their partners also appear to be at greater risk of prenatal mental health problems [38]. Also, a study conducted in Victoria, Australia found single mothers report higher levels of prenatal depressive symptoms than those with unsupportive partners [50]. A review of longitudinal studies conducted in Australia and New Zealand indicated poor partner relationship as the strongest predictor of prenatal anxiety and depression [34]. Also, pregnant women in a violent marital relationship receive less support from their spouses and even cause additional stress and anxiety leading to adverse birth outcomes, including low birth weight and preterm birth [51, 52].
The relationship between marital status and the risk of mental disorders, including depressive disorder, anxiety disorder and self-harm, has received little research attention in Australia and globally. There has also been a lack of studies utilising high quality linked data on this topic, which would create opportunities for more complex and expanded research. Also, it is vital to examine whether non-partnered status poses a particular disadvantage to pregnant women’s mental health in terms of depressive disorder, anxiety disorder and self-harm risk. Understanding such relationships is important to inform approaches for supporting non-partnered pregnant women with a view to enhancing their mental wellbeing.
In direct response to these gaps in the current literature, our large cohort study aimed to assess the association between marital status and prenatal mental disorders among Australian women using linked health administrative data from the State of New South Wales (NSW), Australia. We hypothesized that non-partnered marital status is significantly associated with prenatal depressive disorder, anxiety disorder and self-harm.
Methods
Data source and study population
The current population-based retrospective cohort study used linked data from the NSW Admitted Patients Data Collection (APDC) and the NSW Perinatal Data Collection (PDC) (https://www.cherel.org.au/data-dictionaries) and reported per the guideline of the STROBE checklist (Additional file 1). The APDC contains regularly collected data on inpatient services from all public and private hospitals, and public multi-purpose service centres in NSW. APDC contains the demographic characteristics, clinical diagnosis and other clinical procedures of the patient. The PDC collects data on pregnancy and all births (i.e., hospital and homebirths) of ≥ 20 weeks gestation or birth weight of ≥ 400 g.
Eligibility criteria and sample selection
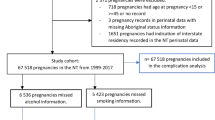
The eligible criteria for inclusion in the current study were; first, women should be pregnant between 2000 and 2011 and resides in NSW. Second, there should be a report on their marital status. Hospital admissions for mental disorders were identified using data from the APDC dataset (2000–2011), which contain 646,233 mothers with 2,624,544 hospital admissions. In the PDC dataset (2000–2011), there were 649,210 mothers and 1,053,819 births. After excluding duplicate records 609,299 mothers from the PDC dataset were linked with 882,238 admissions from APDC dataset. After excluding those women who have no data on marital status, 598,599 pregnant women with 865,349 admissions included in the analyses. The details of the study population selection process and data linkage are presented in Fig. 1.
The Centre for Health Record Linkage (CHeReL) executed the data linkage between the PDC and APDC dataset using probabilistic record linkage methods and Choice-maker software for these two data sources [53], which estimated a false positive rate of 0.3% and a false negative < 0.5% of records.
Diagnoses of mental disorders
The diagnosis of mental health disorders of pregnant women was performed by a doctor at the inpatient department of hospitals in NSW and coded per the criteria of the 10th version International Classification of Diseases and Related Health Problems, Australian Modification (ICD-10-AM) [54]. ICD-10-AM is a diagnostic mental health measure that likely picks up the more severe mental health disorder within the population and misses women with milder mental health disorders compared with screening or self-report measures. The record admission contains one principal diagnosis, one stay diagnosis and 53 other diagnoses [55]. For the current study, only a principal diagnosis of depressive disorder, anxiety disorder or self-harm was considered for participant inclusion. The data for admission was taken from the Admitted Patients Data Collection (APDC) data set. A hospital admission refers to any hospitalisation or admission of a patient to hospital for inpatient service.
If a woman had the principal diagnosis of depressive episode [F32], recurrent depressive disorder [F33], persistent mood (affective) disorder [F34], other mood (affective) disorder [F38], or unspecified mood (affective) disorder [39], her admission was identified as depressive disorder. If a woman had the principal diagnosis of phobic anxiety disorders [F40], other anxiety disorders [F41], or obsessive–compulsive disorder [F42], her admission was identified as anxiety disorder. If a woman had the principal diagnosis of self-injuries and/or self-poisoning [S00-T75] or certain early complications of trauma [T79], her admission was identified as international self-harm.
Exposure and confounding variables
The exposure variable was marital status of pregnant women. The available response options on the marital status were never married, married/de facto relationship, separated, divorced, or widowed. Then, those with a marital status of never married, separated, divorced, and widowed were categorised as “non-partnered”, whilst the remaining response (married and de facto relationship) were grouped as “partnered”. The confounding variables included in the analyses were age, remoteness, socio-economic disadvantage, country of birth, indigenous status, and smoking status.
Statistical analysis
We undertook three steps to analyse the data. First, frequency and percentages were generated to show the prevalence of the outcome variables (depressive disorder, anxiety disorder and self-harm) among admitted pregnant were determined. Then, we cross-tabulated the distribution of the exposure variable (partnered or non-partnered) across the confounding and outcome variables; including using the Pearson’s chi-square test and Student’s t-test to demonstrate statistically significant associations. Further, a binary logistic regression model was employed to determine the association between marital status and mental disorders (i.e. depressive disorder, anxiety disorder and self-harm) after adjusting for confounders. The results of the regression analyses in the final model were described using adjusted odds ratio (AOR) with the respective 95% confidence intervals (CI). The final model was assessed using the Hosmer and Lemeshow goodness of fit test [56]. For all statistical analyses, statistical significance was set at p < 0.05. Analyses was conducted using STATA/MP 16 (Stata Corp, USA).
Results
Among the 609,299 pregnant women who were living in NSW and their babies were firstborn between 2000 and 2011 by linking the APDC dataset and PDC dataset, 1.8% (n = 10,700) did not report their marital status. Pregnant women with missing data on this exposure variable (i.e. marital status) were excluded from the analyses and thus data from 598,599 pregnant women were included in the analyses. A total of 241 pregnant women (0.04%) were with the principal diagnosis of depressive disorder; 107 (0.02%) with the principal diagnosis of anxiety disorder; and 4,359 (0.5%) with the principal diagnosis of intentional self-harm. None of the pregnant women were found to experience two or all of these mental health conditions.
The socio-demographic characteristics of study participants are presented in Table 1. The average age of the pregnant women was 29.6 (SD = 5.8) years, with 31.8% (n = 193,439) of the women were between the age of 30–34 years and 28.1% (n = 171, 373) were aged 25–29 years. The majority of the pregnant women (67.4%) resided in a major city.
Table 1 also provides a comparison between partnered and non-partnered pregnant women, by demographic and health-related characteristics. In comparison to non-partnered women, partnered women were more likely to: be older; reside in a major city; have a lower level of socio-economic disadvantage; be a non-smoker; be born outside of Australia; be non-Indigenous; and/or have full insurance cover (all p < 0.001). In addition, partnered women, in comparison to non-partnered women were more likely to: have gestational diabetes; have gestational hypertension; not have preeclampsia; not have a depressive disorder; not have anxiety; and/or not self-harm (all p < 0.001).
Table 2 shows the association between marital status and mental disorders, after adjusting for the available confounders. The multiple logistic regression model estimated that the odds of depressive disorder was 2.75 times higher among the non-partnered pregnant women, compared with the partnered women (AOR = 2.75; 95%CI: 2.04, 3.70; p < 0.001). In addition, the odds of anxiety disorder during pregnancy was 3.16 times higher among non-partnered women (AOR: 3.16, 95%CI: 2.03, 4.91; p < 0.001). Furthermore, the model estimated that the odds of experiencing self-harm was two times higher among non-partnered pregnant women compared to their counterpart (AOR = 2.0; 95%CI: 1.82, 2.20; p < 0.001).
Discussion
This study identified several important findings regarding the relationship between marital status and prenatal mental disorders among admitted Australian women. In particular, non-partnered pregnant women were more likely to suffer from a depressive disorder, anxiety disorder or self-harm, than partnered pregnant women.
Our study found that prenatal depressive disorder is more likely among non-partnered pregnant women than their partnered counterparts. Various international epidemiological studies also found that non-partnered pregnant women (not married, single or not living together with a partner) have a higher odds of suffering from depressive symptoms during the prenatal period compared to partnered women [33, 43, 44, 57,58,59,60]. Furthermore, our study adds further evidence to the findings of previous research conducted in Victoria, Australia (n = 1578) [50] which found single mothers report higher levels of prenatal depressive symptoms compared to women with supportive partners. Interestingly, the authors also found that single pregnant women reported lower levels of depressive symptoms than those with unsupportive partners [50]. Some studies report a non-significant association between marital status and prenatal depression [46,47,48, 61]. The difference between the current and previous studies might be due to the variation in adjusting potential confounders and study participants' demographic characteristics. For example, a study conducted in UK adjusted for confounders such as marital satisfaction, previous history of mental illness and social support [47], and a study conducted in Italy also adjusted for confounders such as social support, stressful life events and relationship problem with a partner [46]. Furthermore, of the total participants (n = 546) of a study conducted in the US, most were single (91%, n = 497) [48], which can limit the statistical power of analysis and result in a non-significant association.
Our study demonstrated that the likelihood of prenatal anxiety disorder was three-fold higher among non-partnered women. Similarly, other studies conducted in Malaysia, Mexico, and Brazil have also shown that non-partnered pregnant women have a higher level of anxiety during the antenatal period [33, 59, 62] compared to partnered women. Conversely, a facility-based study conducted in China, Shanghai (n = 527) [49] reported a non-significant association between marital status and prenatal anxiety. The possible reason for the non-significant association could be that most of the study participants were married (98.6%, n = 520) [49], which can limit the statistical power of the analyses.
Our study also found that the likelihood of experiencing self-harm was two times higher among non-partnered pregnant women compared to those with partnered marital status. Support for the finding in the current study comes from cross-sectional studies conducted in Brazil (n = 1414) [45] and Ethiopia (n = 423) [63], focusing on pregnant women attending the antenatal care unit demonstrated that the likelihood of suicide was significantly related to lack of a cohabiting partner. A study conducted in Brazil [45] also performed a separate regression analysis for depressed pregnant women and found the odds of suicide was higher among non-partnered (single, divorced or widowed) depressed pregnant women (n = 315) [45]. Studies conducted in South Africa (n = 649) [64], Australia (n = 1507) [65] and US (n = 383) [66] reported a non-significant association between marital status and self-harm during pregnancy. The null result in a study conducted in South Africa could be due to adjusting for important confounders such as social support, marital stress, relationship with a partner, and previous history of mental illness, which was not possible in the current study [64]. Also, the study conducted in Australia which examined predictors of persistent self-harm (thought/attempt) adjusted for confounders such as intimate partner violence and afraid of partner during multivariate logistic regression analysis [65]. In a study conducted in US, Only 1 of the study participants attempted suicide during pregnancy, which might be due to the active participation of all study subjects in mental health treatment and willingly participated in the study, which might help in early identification and intervention of suicidal ideation [66]. Thus, the observed association in the current study could be due to inadequate adjustment of confounders. Further studies confirming this finding are recommended.
Almost 1 in 2500 pregnant women in the current study met the ICD-10-AM diagnostic criteria for depressive disorder. The prevalence in the present study is lower than the pooled prevalence of antenatal depression in high-income countries (17%) [4], as well as the reported prevalence of other studies conducted in Australia 7–17% [5, 6]. The discrepancy in the prevalence of prenatal depression might be due to the use of instruments to examine depression. For example, studies conducted in Australia used 10 item EPDS (10 items) with a score of ≥ 13, suggesting depressive symptoms, which are highly sensitive and inflate positive depression cases [67], whereas in the current study, depressed women were identified using a diagnostic tool (ICD-10-AM).
Our study also found that 1 in 5000 pregnant women diagnosed with anxiety disorder. A higher estimate of antenatal anxiety was reported from a study conducted in Australia (27%) [5] and other epidemiological studies (14–59%) [7,8,9,10]. The possible reason for the discrepancy could be that the study conducted in Australia used Beck Anxiety Inventory (BAI) (i.e., a score of ≥ 16) to screen anxiety symptoms, possibly inflating probable anxiety. In contrast, our study employed ICD-10 AM to diagnose a prenatal anxiety disorder.
Around 1 in 200 pregnant women in the current study diagnosed with intentional self-harm, which is lower than a report of an international review (5–14%) [68] and a study conducted in Australia (n = 1507) (5%) [65] and South Africa (n = 649) (18%) [64]. The discrepancy might be due to the fact that studies conducted in South Africa and Australia examined self-harm (thought/attempt) using a single-item screening tool from the Edinburgh Postnatal Depression Scale (EPDS) [69], which is more likely to inflate prenatal self-harm compared to ICD-10 AM.
Marital status [33, 43, 44] and the quality and length of the marriage relationship significantly affect prenatal mental health problems and the level of prenatal social support [38]. For pregnant women, a marital partner is one of the key sources of emotional and tangible support [70]. For many pregnant women, their marital partner plays a vital role in detecting perinatal depressive and anxiety symptoms and supports in seeking health care professional help [71, 72]. Also, partner support and marital stability are important protective factors for the psychological well-being of pregnant women [73]. Furthermore, partnered women have enormous psychosocial advantages compared to non-partnered women, though much of this may be restricted to women living in a quality marital relationship [74]. Despite the continued debate about the definition, the available evidence in developed countries viewed the quality of marital relationship as a multidimensional concept that measures objective features of marital relationship such as friendship, communication, affection, and trust, along with subjective features like marital satisfaction [75]. Studies have also shown that non-partnered pregnant women have a higher risk of antenatal depression and anxiety than women with a supportive partner [76, 77]. Also, an Australian population-based panel study found a decline in mental health for women who were separated or widowed [78]. Interestingly, partnered pregnant women living in poor-quality relationships with their spouses also appear at greater risk of prenatal anxiety and depression [38, 79, 80] because they are exposed to additional stress and anxiety from their spouses [51]. Besides, stress due to a challenging marital relationship with the spouse makes an adjustment to the current pregnancy difficult for the woman [81], subsequently leading to prenatal and postnatal mental health problem and adverse birth outcome [52]. A review of longitudinal studies examining maternal mental health in Australia and New Zealand indicated poor partner relationship as the strongest predictor of prenatal anxiety and depression [34]. Also, a study conducted in Canada (n = 3021) indicated that poor quality of marital relationships and partner tension significantly predicts prenatal anxiety [30]. Evidence also shown that lack of support from a partner coupled with barriers to health education correlates with decreased prenatal stress coping for low-income women [82]. Even though no study has yet examined the relationship between the mental well-being of the spouse and prenatal mental health problems, it could be a possible risk factor for prenatal mental health problems. Nonetheless, the psychopathology of the spouse played a significant positive role in the postnatal period for the occurrence of maternal depression [83].
Strength and limitation
Our study has a number of important strengths. Our results are based on a large population-based administrative data linked from PDC and APDC sources. Also, it is the first study assessing the relationship between marital status and prenatal mental health problems (depressive disorder, anxiety disorder and self-harm) using high-quality linked data.
However, our study also has limitations. Since we did not have data on the following variables, our study did not adjust for the confounding role of social support, pre-pregnancy mental health problems, partner mental health status, intimate partner violence, length and quality of the marital relationship, which can play a key role in the observed associations. Evidence indicated the possible over-enumeration of admission due to depressive disorder, anxiety disorder, and self-harm might be because admissions could happen due to medical problems related to the perinatal period [84, 85]. During analysis, the overestimation of mental disorders was managed by including only admissions with a principal diagnosis of mental disorder. Lastly, more recent data should be examined to see if the associations identified in our analyses still hold.
Conclusion
The partner status of Australian pregnant women has a significant positive association with prenatal depressive disorder, anxiety disorder and self-harm. This suggests it would be highly beneficial for maternal health care professionals to screen non-partnered pregnant women for prenatal mental health problems such as depression, anxiety and, self-harm. Also, screening non-pregnant women for social support is vital to assess the support level from other social networks. Policy-makers need to consider developing targeted community-based social support programs to enhance pregnant women's mental wellbeing.
Availability of data and materials
All the available data are included in the manuscript.
References
Rich-Edwards JW, Kleinman K, Abrams A, Harlow BL, McLaughlin TJ, Joffe H, et al. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. J Epidemiol Community Health. 2006;60(3):221–7.
Dunkel SC. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62:531–58.
Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–33.
Dadi AF, Miller ER, Bisetegn TA, Mwanri L. Global burden of antenatal depression and its association with adverse birth outcomes: an umbrella review. BMC Public Health. 2020;20(1):173.
Leigh B, Milgrom J. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry. 2008;8:24.
Eastwood J, Ogbo F, Hendry A, Noble J, Page A. Early Years Research Group (EYRG). The Impact of Antenatal Depression on Perinatal Outcomes in Australian Women PLoSOne. 2017;12(1): e0169907.
Rico MAG, Rodríguez AJM, Díez SMU, Real MCM. Análisis de la relación entre riesgo gestacional y ansiedad materna. Prog Obstet Ginecol. 2010;53(7):273–9.
Hernández-Martínez C, Val VA, Murphy M, Busquets PC, Sans JC. Relation between positive and negative maternal emotional states and obstetrical outcomes. Women Health. 2011;51(2):124–35.
Nieminen K, Stephansson O, Ryding EL. Women’s fear of childbirth and preference for cesarean section–a cross-sectional study at various stages of pregnancy in Sweden. Acta Obstet Gynecol Scand. 2009;88(7):807–13.
Teixeira C, Figueiredo B, Conde A, Pacheco A, Costa R. Anxiety and depression during pregnancy in women and men. J Affect Disord. 2009;119(1–3):142–8.
Kurki T, Hiilesmaa V, Raitasalo R, Mattila H, Ylikorkala O. Depression and anxiety in early pregnancy and risk for preeclampsia. Obstet Gynecol. 2000;95(4):487–90.
Nicholson WK, Setse R, Hill-Briggs F, Cooper LA, Strobino D, Powe NR. Depressive Symptoms and Health-Related Quality of Life in Early Pregnancy. Obstet Gynecol. 2006;107(4):798–806.
Hollins K. Consequences of antenatal mental health problems for child health and development. Curr Opin Obstet Gynecol. 2007;19(6):568–72.
PricewaterhouseCoopers. The Cost of Perinatal Depression and Anxiety in Australia: Gidget Foundation Australia; 2019.
Productivity Commission: Mental Health, Report no. 95 Canberra: Commonwealth of Australia. 2020.
Orr ST, Miller CA. Maternal depressive symptoms and the risk of poor pregnancy outcome: review of the literature and preliminary findings. Epidemiol Rev. 1995;17(1):165–71.
Freeman MP. Perinatal psychiatry: risk factors, treatment data, and specific challenges for clinical researchers. J Clin Psychiatry. 2008;69(4):633–4.
Steer RA, Scholl TO, Hediger ML, Fischer RL. Self-reported depression and negative pregnancy outcomes. J Clin Epidemiol. 1992;45(10):1093–9.
Stott D. Follow-up study from birth of the effects of prenatal stresses. Dev Med Child Neurol. 1973;15(6):770–87.
Heron J, O’Connor TG, Evans J, Golding J, Glover V, Team AS. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord. 2004;80(1):65–73.
Murray CJ, Lopez AD, Organization WH. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020: summary. 1996.
Figueiredo B, Costa R, Pacheco A, Pais A. Mother-to-infant emotional involvement at birth. Matern Child Health J. 2009;13(4):539–49.
Hart S, Field T, del Valle C, Pelaez-Nogueras M. Depressed mothers’ interactions with their one-year-old infants. Infant Behav Dev. 1998;21(3):519–25.
Straub H, Qadir S, Miller G, Borders A. Stress and stress reduction. Clin Obstet Gynecol. 2014;57(3):579–606.
Shapiro GD, Fraser WD, Frasch MG, Séguin JR. Psychosocial stress in pregnancy and preterm birth: associations and mechanisms. J Perinat Med. 2013;41(6):631–45.
Gong X, Hao J, Tao F, Zhang J, Wang H, Xu R. Pregnancy loss and anxiety and depression during subsequent pregnancies: data from the C-ABC study. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2013;166(1):30–6.
Bogaerts AF, Devlieger R, Nuyts E, Witters I, Gyselaers W, Guelinckx I, et al. Anxiety and depressed mood in obese pregnant women: a prospective controlled cohort study. Obes Facts. 2013;6(2):152–64.
Woods-Giscombé CL, Lobel M, Crandell JL. The impact of miscarriage and parity on patterns of maternal distress in pregnancy. Res Nurs Health. 2010;33(4):316–28.
Agrati D, Browne D, Jonas W, Meaney M, Atkinson L, Steiner M, et al. Maternal anxiety from pregnancy to 2 years postpartum: transactional patterns of maternal early adversity and child temperament. Arch Womens Ment Health. 2015;18(5):693–705.
Bayrampour H, McDonald S, Tough S. Risk factors of transient and persistent anxiety during pregnancy. Midwifery. 2015;31(6):582–9.
Buist A, Gotman N, Yonkers KA. Generalized anxiety disorder: course and risk factors in pregnancy. J Affect Disord. 2011;131(1–3):277–83.
Byatt N, Hicks-Courant K, Davidson A, Levesque R, Mick E, Allison J, et al. Depression and anxiety among high-risk obstetric inpatients. Gen Hosp Psychiatry. 2014;36(6):644–9.
Fadzil A, Balakrishnan K, Razali R, Sidi H, Malapan T, Japaraj RP, et al. Risk factors for depression and anxiety among pregnant women in H ospital T uanku B ainun, I poh. M alaysia Asia-Pacific Psychiatry. 2013;5:7–13.
Schmied V, Johnson M, Naidoo N, Austin M-P, Matthey S, Kemp L, et al. Maternal mental health in Australia and New Zealand: A review of longitudinal studies. Women and Birth. 2013;26(3):167–78.
Arch JJ. Pregnancy-specific anxiety: which women are highest and what are the alcohol-related risks? Compr Psychiatry. 2013;54(3):217–28.
Rubertsson C, Hellström J, Cross M, Sydsjö G. Anxiety in early pregnancy: prevalence and contributing factors. Arch Womens Ment Health. 2014;17(3):221–8.
van Heyningen T, Honikman S, Myer L, Onah MN, Field S, Tomlinson M. Prevalence and predictors of anxiety disorders amongst low-income pregnant women in urban South Africa: a cross-sectional study. Arch Womens Ment Health. 2017;20(6):765–75.
Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: a systematic review. J Affect Disord. 2016;191:62–77.
Edwards B, Galletly C, Semmler-Booth T, Dekker G. Antenatal psychosocial risk factors and depression among women living in socioeconomically disadvantaged suburbs in Adelaide, South Australia. Aust N Z J Psychiatry. 2008;42(1):45–50.
Ogbo FA, Eastwood J, Hendry A, Jalaludin B, Agho KE, Barnett B, et al. Determinants of antenatal depression and postnatal depression in Australia. BMC Psychiatry. 2018;18(1):49.
Bisetegn TA, Mihretie G, Muche T. Prevalence and Predictors of Depression among Pregnant Women in Debretabor Town, Northwest Ethiopia. PLoS ONE. 2016;11(9): e0161108.
Biratu A, Haile D. Prevalence of antenatal depression and associated factors among pregnant women in Addis Ababa, Ethiopia: a cross-sectional study. Reprod Health. 2015;12:99.
Gemta WA. Prevalence and factors associated with antenatal depression among women following antenatal care at Shashemane health facilities, South Ethiopia. Annals of Global Health. 2015;81(1).
Mossie TB, Sibhatu AK, Dargie A, Ayele AD. Prevalence of antenatal depressive symptoms and associated factors among pregnant women in Maichew, North Ethiopia: an institution based study. Ethiop J Health Sci. 2017;27(1):59–66.
da Silva RA, da Costa OL, Jansen K, da Silva Moraes IG, de Mattos Souza LD, Magalhães P, et al. Suicidality and Associated Factors in Pregnant Women in Brazil. Community Ment Health J. 2012;48(3):392–5.
Agostini F, Neri E, Salvatori P, Dellabartola S, Bozicevic L, Monti F. Antenatal Depressive Symptoms Associated with Specific Life Events and Sources of Social Support Among Italian Women. Matern Child Health J. 2015;19(5):1131–41.
Husain N, Cruickshank K, Husain M, Khan S, Tomenson B, Rahman A. Social stress and depression during pregnancy and in the postnatal period in British Pakistani mothers: a cohort study. J Affect Disord. 2012;140(3):268–76.
Luke S, Salihu HM, Alio AP, Mbah AK, Jeffers D, Berry EL, et al. Risk factors for major antenatal depression among low-income African American women. J Womens Health. 2009;18(11):1841–6.
QIAO YX, Wang J, Li J, Ablat A. The prevalence and related risk factors of anxiety and depression symptoms among Chinese pregnant women in Shanghai. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2009;49(2):185–90.
Bilszta JLC, Tang M, Meyer D, Milgrom J, Ericksen J, Buist AE. Single Motherhood Versus Poor Partner Relationship: Outcomes for Antenatal Mental Health. Aust N Z J Psychiatry. 2008;42(1):56–65.
Hamberger LK, Arnold J. The impact of mandatory arrest on domestic violence perpetrator counseling services. Family Violence Bulletin. 1990;6:10–2.
Bailey BA. Partner violence during pregnancy: prevalence, effects, screening, and management. Int J Women’s Health. 2010;2:183.
Master Linkage Key (MLK) [www.cherel.org.au].
Innes K, Hooper J, Bramley M, DahDah P. Creation of a Clinical Classification: International Statistical Classification of Diseases and Related Health Problems—10th Revision, Australian Modification (ICD-10-AM). Health Inf Manag. 1997;27(1):31–8.
Health AIo, Welfare. Australian hospital statistics 2008–09. Canberra: AIHW; 2010.
Hosmer DW, Lemeshow S. Applied Logistic Regression. New York: John Wiley & Sons; 2000.
Adewuya AO, Ola BA, Aloba OO, Dada AO, Fasoto OO. Prevalence and correlates of depression in late pregnancy among Nigerian women. Depress Anxiety. 2007;24(1):15–21.
Brittain K, Myer L, Koen N, Koopowitz S, Donald KA, Barnett W, et al. Risk factors for antenatal depression and associations with infant birth outcomes: results from a S outh a frican birth cohort study. Paediatr Perinat Epidemiol. 2015;29(6):505–14.
Faisal-Cury A, Menezes PR. Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch Womens Ment Health. 2007;10(1):25–32.
Weobong B, Soremekun S, Ten Asbroek AH, Amenga-Etego S, Danso S, Owusu-Agyei S, et al. Prevalence and determinants of antenatal depression among pregnant women in a predominantly rural population in Ghana: The DON population-based study. J Affect Disord. 2014;165:1–7.
Glazier RH, Elgar FJ, Goel V, Holzapfel S. Stress, social support, and emotional distress in a community sample of pregnant women. J Psychosom Obstet Gynecol. 2004;25(3–4):247–55.
Salgado IV, Mendoza JLM, Zerón HM. Mexican pregnant women show higher depression and anxiety with rising age and in the case of being single. Acta Medica Lituanica. 2019;26(4):227.
Anbesaw T, Negash A, Mamaru A, Abebe H, Belete A, Ayano G. Suicidal ideation and associated factors among pregnant women attending antenatal care in Jimma medical center, Ethiopia. PLoS ONE. 2021;16(8): e0255746.
Redinger S, Pearson R, Houle B, Norris S, Rochat T. Thoughts of self-harm in early and late pregnancy in urban South Africa: Investigating prevalence, predictors and screening options. S Afr Med J. 2021;111(7):627–34.
Giallo R, Pilkington P, Borschmann R, Seymour M, Dunning M, Brown S. The prevalence and correlates of self-harm ideation trajectories in Australian women from pregnancy to 4-years postpartum. J Affect Disord. 2018;229:152–8.
Newport DJ, Levey L, Pennell P, Ragan K, Stowe ZN. Suicidal ideation in pregnancy: assessment and clinical implications. Arch Womens Ment Health. 2007;10(5):181–7.
Thombs BD, Kwakkenbos L, Levis AW, Benedetti A. Addressing overestimation of the prevalence of depression based on self-report screening questionnaires. CMAJ. 2018;190(2):E44–9.
Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77–87.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782–6.
Eaton WW. Life events, social supports, and psychiatric symptoms: A re-analysis of the New Haven data. J Health Soc Behav. 1978;19(2):230–4.
Fonseca A, Canavarro MC. Women’s intentions of informal and formal help-seeking for mental health problems during the perinatal period: The role of perceived encouragement from the partner. Midwifery. 2017;50:78–85.
Atkinson J, Smith V, Carroll M, Sheaf G, Higgins A. Perspectives of partners of mothers who experience mental distress in the postnatal period: A systematic review and qualitative evidence synthesis. Midwifery. 2021;93: 102868.
Freitas G, Botega NJ. Prevalence of depression, anxiety and suicide ideation in pregnant adolescents. Rev Assoc Med Bras (1992). 2002;48(3):245–9.
Kaplan G, DeLongis A, editors. Psychosocial factors influencing the course of arthritis: A prospective study. annual meeting of the American Psychological Association, Anaheim, CA; 1983.
Glenn ND, Quantitative research on marital quality in the,. A critical review. J Marriage Fam. 1980;1990:818–31.
Wahn EH, Nissen E. Sociodemographic background, lifestyle and psychosocial conditions of Swedish teenage mothers and their perception of health and social support during pregnancy and childbirth. Scandinavian journal of public health. 2008;36(4):415–23.
Figueiredo B, Bifulco A, Pacheco A, Costa R, Magarinho R. Teenage pregnancy, attachment style, and depression: A comparison of teenage and adult pregnant women in a Portuguese series. Attach Hum Dev. 2006;8(2):123–38.
Hewitt B, Turrell G, Giskes K. Marital loss, mental health and the role of perceived social support: findings from six waves of an Australian population based panel study. J Epidemiol Community Health. 2012;66(4):308–14.
Gourounti K, Anagnostopoulos F, Sandall J. Poor marital support associate with anxiety and worries during pregnancy in Greek pregnant women. Midwifery. 2014;30(6):628–35.
Nasreen HE, Kabir ZN, Forsell Y, Edhborg M. Prevalence and associated factors of depressive and anxiety symptoms during pregnancy: a population based study in rural Bangladesh. BMC Womens Health. 2011;11(1):22.
Marchesi C, Bertoni S, Maggini C. Major and minor depression in pregnancy. Obstet Gynecol. 2009;113(6):1292–8.
Parrott SD. Psychosocial Support During Pregnancy: A Narrative Inquiry of Low-Income Unmarried Women in Iowa: Walden University; 2021.
Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA. 2010;303(19):1961–9.
Matthey S, Ross-Hamid C. The validity of DSM symptoms for depression and anxiety disorders during pregnancy. J Affect Disord. 2011;133(3):546–52.
Jones I, Heron J, Blackmore ER, Craddock N. Incidence of hospitalization for postpartum psychotic and bipolar episodes. Arch Gen Psychiatry. 2008;65(3):356.
Acknowledgements
First, we want to acknowledge the New South Wales Ministry of Health and the Centre for Health Record Linkage (CheReL) for giving us the data. Second, our whole-hearted gratitude goes to participant women who have provided their data and individuals who participated in the data collection.
Funding
No funding was received for this research work.
Author information
Authors and Affiliations
Contributions
AB, WP and DS conceived the study, planned the study design and performed the analyses. AB performed the report write-up and drafted the manuscript. DS, JA, WP & FX contributed to the analysis, reviewing the draft document and manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our study protocol was approved by the NSW Population and Health Services Research Ethics Committee and the Human Research Ethics Committee of the University of New South Wales and University of Technology Sydney, Australia (Reference Number: 2011/06/328). Our study used personally de-identified existing health records, and as a result, the CHeReL (Centre for Health Record Linkage) enables our ethically approved research to be conducted without consent. All the methods throughout the study were performed in agreement with the approved protocol.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bedaso, A., Adams, J., Peng, W. et al. An examination of the association between marital status and prenatal mental disorders using linked health administrative data. BMC Pregnancy Childbirth 22, 735 (2022). https://doi.org/10.1186/s12884-022-05045-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-05045-8