Abstract
Background
Childbirth experience has been shown to depend on the mode of delivery. However, it is unclear how labour induction influences the childbirth experience in different modes of delivery. Thus, we assessed the childbirth experience among mothers with spontaneous and induced labours.
Design
A retrospective cohort study.
Setting
Childbirths in four delivery hospitals in Helsinki and Uusimaa District, Finland, in 2012-2018.
Sample
95051 childbirths excluding elective caesarean sections.
Methods
Obstetric data combined to maternal childbirth experience measured by Visual Analogue Scale (VAS) was analysed with univariate linear modelling and group comparisons. The primiparas and multiparas were analysed separately throughout the study due to the different levels of VAS.
Main outcome measures
Maternal childbirth experience measured by VAS.
Results
The negative effect of labour induction on the childbirth experience was discovered in each mode of delivery. Operative deliveries were perceived more negatively when they were preceded by labour induction. The rate of poor childbirth experience (VAS≤5) was higher for mothers with labour induction (ORs varying from 1.43 to 1.77) except in emergency caesarean sections. The negative effect of labour induction was smaller than the effect of mode of delivery, while successful vaginal delivery with induction (meanPRIMI=8.00 [95% CI 7.96–8.04], meanMULTI=8.50 [8.47–8.53]) was perceived more positive than operational deliveries with spontaneous labour (meansPRIMI≤7.66 [7.61–7.70], meansMULTI≤7.96 [7.89–8.03]). However, labour induction more than doubled the risk of caesarean section for both primiparas and multiparas.
Conclusions
Labour induction generates more negative experiences for both primiparas and multiparas. The negative effect of labour induction is detected for all modes of delivery, being worst among labour induction resulting in operative delivery. The parturients facing cumulative obstetric interventions require special support and counselling during and after delivery.
Similar content being viewed by others
Introduction
Childbirth as a physical, social and emotional event has essential immediate and long-term implications on the health and wellbeing of a mother and the entire family [1]. It is also shown that poor or traumatic childbirth experiences have an impact on future reproduction [2,3,4]. The visual analogue scale (VAS) as a simple measure for childbirth experience may not fully capture the holistic nature of the childbirth phenomenon, but its validity and reliability as an overall satisfaction measure has been comprehensively demonstrated [5,6,7,8].
During the past decade several meta-analyses and reviews have indicated benefits benefits from labour induction for the neonate without increased risk for the mother in term and post-term gestations [9, 10]. These studies indicated more desirable perinatal outcomes, as induction decreased the numbers of neonate deaths and lowered the need for the neonatal intensive care unit, and decreased the need for caesarean sections as well. However, the data have been criticised on methodological deficiencies due to inappropriate control groups and different timings of compared trials [11,12,13]. The obstetrical arguments for induction in end term or post-term gestations are undeniable [12]. Nevertheless, the association between induction of labour and the maternal experience of childbirth is poorly understood [8, 14]. It has been shown that successfully induced labour resulting in vaginal delivery did not negatively affect birth outcomes but had a partial negative effect on the childbirth experience [15, 16]. In addition, childbirth experience may also depend on the mode of delivery [2, 16,17,18,19].
In this study we investigate how labour induction influences the childbirth experience in different modes of delivery. We distinguish between spontaneous and induced labours and, consequently, address their effects through actual mode of delivery for the childbirth experience.
Data and methods
The childbirth experience is measured by VAS in the postpartum unit of the delivery hospital. The VAS scale in this study is from ‘very negative childbirth experience’ (1) to ‘very positive childbirth experience’ (10). The VAS was collected as a part of a conversation with a midwife before discharge from the postpartum unit. The midwives have been instructed to pursue as safe atmosphere as possible to avoid biased responses. The women rating their childbirth experience with the score of 5 or less on the VAS scale were offered an opportunity to receive additional support.
The VAS is combined with the Medical Birth Register data using the mother’s identification code, given for all citizens and permanent residents of Finland. The Medical Birth Register is a comprehensive medical register kept by the Finnish Institute for Health and Welfare including antenatal, perinatal and postpartum information from all mothers and infants up to 7 days. The data were pseudonymised and therefore parturients’ identities could not be detected in this data.
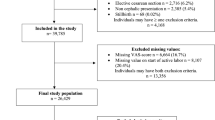
This study includes all singleton live births at term (gestational age ≥37) in Helsinki and Uusimaa District hospitals from January 2012 to December 2018. The childbirth experience and labour induction in mode of delivery groups being the key concepts of this study, the parturients without these variables were excluded (n=11 635) as well as those having elective caesarean sections (n=6 266). The data inclusion criteria are depicted in Fig. 1. There are specific disparities between primiparous and multiparous women when childbirth and mode of delivery are considered [20,21,22] and therefore, these groups are analysed separately throughout the study. The mode of delivery was classified into four categories: unassisted (VD) and instrumental vaginal deliveries (IVD) as well as urgent (UCS) and emergency caesarean sections (ECS).
The Institutional review board gave the permission (HUS/483/2020) to use the data and waived the requirement of the informed consent for the study since it was a register-based study.
Analysis
The analyses of this study were conducted in three phases. First, we used two-way analysis of covariance to discover the effects of labour induction and mode of delivery on the childbirth experience. This method assumes the response variable – the childbirth experience by VAS – as continuous and allows controlling for the effects of both binary and continuous confounding variables. Two insights – considering the childbirth experience continuous by nature and ten-point scale being too wide to be analysed in categories - allowed us to utilise analysis of covariance. Assuring the results being consistent between different analysing methods, parallel analyses using generalized linear methods were conducted. Statistical analyses were performed using IBM SPSS Statistics 25 software.
To clarify the association between two factors – labour induction and mode of delivery – and childbirth experience, several confounding variables were included in the second phase of analysis. Confounding variables associated with the childbirth experience were selected based on the previous research, data availability and initial data analysis. Reasonable categories were discovered using appropriate illustrations and statistical tests according to the association between each variable and the childbirth experience. The main goal of this process was to preserve the salient information while compressing it in a few categories to enable unambiguous interpretation. Chi-Square test was used to detect significant differences between spontaneous and induced labour groups Table 1.
The models of the first phase are constructed using the univariate linear model in three phases separately for primiparous and multiparous women. In model 1 Table 2 the childbirth experience was explained through the main effect of the factor variables, labour induction and mode of birth. The confounding effects are controlled in model 2 adding the background characteristics – maternal age, BMI (Body Mass Index) before pregnancy, cohabitation as a proxy of partner support, gestational age, epidural anesthetic use, prolonged labour, and birth weight – in the model. An additional variable for multiparas was a prior caesarean section which received special attention in previous research [23]. Model 3 involves the interaction terms of labour induction and delivery modes. The coefficient estimates of these distinct models are then compared to comprehend the associations between the childbirth experience and induction in each of the mode of delivery groups. Spontaneous labour resulting in vaginal delivery was used as a reference group in the models. Coefficients in the models indicate the effect of each variable on the childbirth experience when compared to the reference group.
Second, we analysed the risk of low VAS (≤5) between spontaneous and induced labours by each mode of delivery. The childbirth experience has been shown to cause undesirable consequences with low values of VAS. Thus, we pursued to scrutinise the risks of induced and spontaneous labour groups for ending up in this poor experience group. Furthermore, odds ratio (OR) estimates with 95% confidence intervals were calculated and compared between spontaneous and induced labour groups.
Third, we calculated relative risks with 95% confidence intervals to assess the prevalence of each mode of delivery between spontaneous and induced labours. According to the previous studies, each mode of delivery has its specific risks that should be accounted for when the induction trial comes to a decision. The risks of labour induction are emphasised particularly among multiparas with irregular an obstetric history. Taken together, we first assessed the effects of labour induction and mode of delivery on the childbirth experience. Second, we analysed the risk of low VAS between spontaneous and induced labours by each mode of delivery. And finally, we calculated the prevalence of each mode of delivery between spontaneous and induced labours.
Missing values
The register data was complete except that the BMI before pregnancy values were lacking from 1 162 (2.7%) primiparas and 1 964 (3.8%) multiparas. According to a t-test, the mean of VAS of those lacking prepregnancy BMI did not significantly differ from the mean of VAS of complete data.
Patient and public involvement
In our register-based data patient and public involvement was not feasible. The data used in this study was collected retrospectively from the registers of Helsinki University Hospital and the Finnish Institute of Health and Welfare. The Institutional review board gave the permission (HUS/483/2020) to use the data and waived the requirement of the informed consent and a separate Ethical Committee review for the study since it was a purely register-based study. Therefore, the informed consents of registered patients were not required for this study.
Results
The inclusion criteria for this study are depicted in Fig. 1. We included all hospital childbirths of term (≥37 weeks) singleton pregnancy with live infant. Childbirth experience and labour induction being of interest, we excluded the childbirths of elective caesarean sections and those lacking VAS. The final data consisted of 95 051 parturients including 43 403 primiparas and 51 648 multiparas. The share of induced labours in primiparas was 27% and in multiparas 21%.
The characteristics of spontaneous and induced labour groups are presented in Table 1 in categories used in covariance analysis. Difference between distributions of induced and spontaneous groups was detected in all variables except the use of epidural anesthesia among primiparas and maternal age among multiparas. The maternal factors such as mean age (30.1 vs. 29.1 years for primiparas, p<0.001; 32.3 vs. 32.0 years for multiparas, p<0.001) and mean BMI before pregnancy (24.7 vs. 23.2 for primiparas, p<0.001; 26.0 vs. 23.9 for multiparas, p<0.001) were higher in the induced labour group compared to the spontaneous onset of labour group. Gestational age, being one of the common indications for labour induction, was higher in the induced labour group (40.2 vs. 39.7 for primiparas, p<0.001; 39.8 vs. 39.7 for multiparas, p<0.001). Prolonged labour was diagnosed more frequently with induction than with spontaneous labour (p<0.001). The average birth weight was higher for the labour induction group for both primiparas (3516g vs. 3465g, p<0.001) and multiparas (3661g vs. 3616g, p<0.001). In our data preeclampsia (ICD10 codes O11, O14, and O15.0) was diagnosed in 1000 (2.3%) of primiparous and in 431 (0.8%) of multiparous women. Gestational diabetes (ICD10 code O24.4) was diagnosed in 5926 (13.7%) primiparous and in 8415 (16.3%) multiparous women.
The Medical Birth Register does not include complete data about different techniques of induction used in hospitals. However, the used techniques of induction separately in primiparas and multiparas were artificial rupture of membranes (79% and 88%, of induced labours), prostaglandin (28% and 19%) and oxytocin (89% and 74%).
Effects of labour induction and mode of delivery on the childbirth experience
Main effects
The coefficients of different regression covariance analysis models for primiparas and multiparas are presented in Table 2. For both parity groups, the effect of labour induction was negative (βP=-0.34, p<0.001; βM=-0.25, p<0.001) on the childbirth experience when the actual mode of delivery was included in model 1. For primiparas, the coefficient of emergency caesarean section (β=-1.32, p<0.001) was strongest, followed by urgent caesarean section (β=-0.97, p<0.001) and instrumental delivery (β=-0.75, p<0.001) when compared to the vaginal delivery group.
The coefficients in the model of multiparas were -1.88 (p<0.001), -1.03 (p<0.001), and -0.91 (p<0.001), for emergency and urgent caesarean sections and instrumental delivery, respectively. When confounding variables were adjusted in model 2, the negative effect of labour induction faded slightly compared to the basic model being -0.28 for primiparas and -0.22 for multiparas (model 1).
Control variables
Six statistically significant variables – maternal age, partner support, use of epidural anesthesia, prolonged labour, fear of childbirth and birth weight – were detected in the model 2 of primiparas. The strongest negative effect had the fear of childbirth (β=-0.41, p<0.001), prolonged labour (β=-0.37, p<0.001) and use of epidural anesthesia (β=-0.35, p<0.001). Significant control variables in the model for multiparas were equal compared to primiparas, except for partner support, which lost its positive effect among multiparas. Prolonged labour had the strongest negative effect (β=-0.47, p<0.001) on the childbirth experience followed by fear of childbirth (β=-0.22, p<0.001) in model 2 for multiparas, while the effects of other significant control variables were smaller.
Interaction effects
Two significant interaction effects were observed in model 3 for primiparas. The induced labour resulting in instrumental delivery had negative interaction effect (β=-0.12, p=0.016) on the childbirth experience as well as the urgent caesarean section (β=-0.32, p<0.001) when adjusted for confounding variables. The negative effect of emergency caesarean section was statistically insignificant, even though its coefficient was close to the effect of instrumental delivery. This finding could be affected by the low number of emergency caesarean sections in both groups. In multiparas, both urgent (β=-0.34, p<0.001) and emergency caesarean sections (β=-0.51, p=0.004) had negative interaction effects with induction on the childbirth experience.
The adjusted means with 95% confidence intervals of the childbirth experience in each mode of delivery were calculated using model 3 for both parity groups (Fig. 2a and b). Following the coefficients shown in Table 2, the difference between spontaneous and induced labours was larger for instrumental delivery or urgent caesarean among primiparas (Fig. 2a). The overlapping confidence intervals of means revealed that VAS difference disappeared in the emergency caesarean section group.
The adjusted means of VAS with 95% confidence intervals for spontaneous and induced labours in each mode of delivery (corresponding data in a numerical Table 6 is available in a supplementary file)
Regarding multiparas, the mean differences between spontaneous and labour induction groups were considerably larger with urgent and emergency caesarean sections compared to both unassisted and instrumental vaginal delivery groups (Fig. 2b). The labour induction resulting to the unplanned caesarean section produced a lower childbirth experience than labour prolonged labour with spontaneous onset. These visual views coincided with the coefficients in Table 2.
Poor childbirth experience
Low VAS scores indicating poor childbirth experience (≤5) were presented for spontaneous and induced labour groups in each mode of delivery separately. The risk of low VAS was lowest for vaginal delivery with spontaneous onset of labour (5.3%) and highest for emergency caesarean section with induced onset of labour (26.5%) for primiparas and 2.4% and 35.3% for multiparas, respectively. Labour induction was associated with higher odds of perceiving a poor childbirth experience for each mode of delivery and both parity groups (Table 3). Comparing the risks of induced and spontaneous labours in mode of delivery groups for primiparas the OR varied from 1.54 to 1.70 except the estimate for emergency caesarean (OR=1.08 [0.69–1.68]). Corresponding estimates of multiparas varied from 1.43 to 1.77 in all modes of delivery except for emergency caesarean section (OR=1.70 [0.98–2.94]). These results imply that 10 poor experiences in spontaneous labour group equals at least 15 poor childbirth experiences in the induced labour group independent of the actual mode of delivery (excluding the emergency caesarean section).
Labour induction and risk to operative deliveries
The effect of mode of delivery on the childbirth experience was larger than the effect of labour induction. Labour induction was associated with increased risk for urgent (RR=2.51 with 95% CI [2.40, 2.62]) and emergency caesarean sections (RR=1.40 [1.16, 1.70]) while there was no association to the likelihood of instrumental delivery among primiparas (Table 4). Among multiparas, labour induction more than doubled the risk for both urgent (RR=2.08 [1.93, 2.25]) and emergency caesarean sections (RR=2.56 [2.00 3.29]), while the risk of instrumental delivery (RR=1.46 [1.34, 1.59]) was increased by nearly 50%. Correspondingly, labour induction was associated with a lower likelihood to achieve vaginal delivery, while the risk ratios are below one for both primiparas (RR=0.77 [0.76, 0.79]) and multiparas (RR=0.92 [0.91, 0.93]).
Discussion
Our study revealed three main findings: 1) The induction of labour in general impaired the childbirth experience, excluding primiparas who underwent an emergency caesarean section. Poor childbirth experience risk is higher in the induced labour group for both primiparas and multiparas. 2) Operational deliveries were perceived more negative if preceded by labour induction, as one fifth of induced primiparas and one seventh of induced multiparas valued their experience as poor. 3) We found a decreased likelihood to achieve vaginal delivery among women who had induced labour.
To compare previous studies assessing childbirth experience, we gathered their main results in Table 5. In our study, we show that induction of labour produces impaired childbirth experience, which is in line with a previous study [15]. The risk of achieving a poor experience was analysed in several studies [2, 7, 8, 24]. Inconsistencies in measurement of experience and definition of a poor or negative experience exist between the studies. However, the overall findings in the previous studies are in line with ours.
In previous studies, the role of the mode of delivery is mostly parallel to our findings. Two studies comparing average experience in mode of delivery groups [17, 18] confirm our finding that vaginal delivery produces the most positive and unplanned caesarean the most negative experience when elective caesarean is not considered. One study did not find association between the modes of delivery [25] and other findings were inconsistent with ours [19], which may be due to the sampling inadequacy (there were only 34 observations in CS group). The risk ratios of negative experience in previous studies indicate similar associations between the mode of delivery and childbirth experience regardless of the fact that we did not compute equivalent risk ratios for modes of delivery in our study.
In our study, we found that induced labour resulting in vaginal delivery was associated with a more positive childbirth experience on average than operational deliveries with spontaneous onset of labour. This leads to the conclusion that successful induction resulting in vaginal delivery does not ruin the positive childbirth experience. However, induction increases the risk for operational delivery which is also shown in previous studies [11, 12, 26, 27]. Operational delivery is likely to impair the childbirth experience, as supported by our findings that the childbirth is experienced more negatively if the labour induction results in caesarean section. It is possible that parturient feel frustration when failing to give vaginal birth together with discomfort and pain due to the unsuccessful labour induction. Our novel approach to evaluate the association of childbirth experience and induction in the mode of delivery should be explored more thoroughly to confirm the findings.
Our study is based on a large comprehensive data set of 95 051 childbirths and it covers 90% of eligible parturients in the study population. The data population covers nearly one third of all Finnish childbirths during the years 2012–2018. The VAS collection was an established routine practice of care, and its simplicity led to minimising the selection bias. The simplicity of the measure also attenuates the possible challenges due to the lack of shared language between the caregiver and the parturient. The national comprehensive Medical Birth Register in combination with the maternal childbirth experience provides reliable data to analyse the associations between the maternal childbirth experience and various factors behind it [28]. Despite the distinct levels of primiparas and multiparas, the resulting nearly identical patterns of childbirth experience confirm the reliability of our data.
Our study also has limitations. Our main outcome measure VAS does not incorporate the multidimensionality of the childbirth experience. However, VAS has been used to measure childbirth experience and satisfaction with childbirth in several previous studies [5,6,7,8, 19]. Furthermore, VAS is moderately correlated with the highly established and validated W-DEQ (Wijma Delivery Expectancy/Experience Questionnaire) scale for measuring childbirth experience [5, 29].
The maternal childbirth experience was collected before the patient was discharged from the post-partum care unit, usually less than 72 hours after the delivery. This could have had an effect on the results, since traumatic experience might take longer to process in the mind [30]. Maimburg and colleagues [31] found similar tendency that women told more negative experiences five years after delivery although women changing their mind had more often experienced operative delivery. In our study setting this would lead to even greater difference. However, there are results that indicate the consistency of childbirth experience from a few days postpartum to few months afterwards [6, 17]. We did not account potential effects of preeclampsia or gestational diabetes which may cause some bias to the results. It has been shown that although gestational diabetes seems to increase the risk of induction, it has no effect on childbirth experience [8]. In the absence of research focusing on the relation between preeclampsia and childbirth experience, the study comparing the mental health indicators after normotensive and hypertensive pregnancies suggests that preeclampsia rises the risk of traumatic childbirth [32].
While the trial of induction is mostly based on obstetrical arguments (suspected fetal macrosomia, post-term gestation, or fear of childbirth) the results of this study are complicated by these underlying factors. By using detailed register data, we attempted to control these effects on the childbirth experience.
Conclusion
Labour induction produces a more negative childbirth experience for both primiparas and multiparas. Women who had induced labour had also decreased likelihood to achieve vaginal delivery. Although the negative effect of labour induction is detected for all modes of delivery, the highest risk for a poor experience is when labour induction results in an operative delivery. Our findings can be used in decision-making related to parturients requesting labour induction without clear obstetrical indications. Furthermore, the parturients facing cumulative obstetrics interventions require special support and counselling from obstetric care during and after delivery.
Availability of data and materials
The data that support the findings of this study are available from Finnish Institution Health and Welfare and Helsinki University Hospital but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
Abbreviations
- VAS:
-
Visual Analogue Scale
- OR:
-
Odds ratio
- RR:
-
Risk ratio
- BMI:
-
Body mass index
- SVD:
-
Spontaneous vaginal delivery
- IVD:
-
Instrumental vaginal delivery
- OVD:
-
Operative delivery
- CS:
-
Caesarean section
- UCS:
-
Urgent caesarean section
- ECS:
-
Emergency caesarean section
- CEQ:
-
Childbirth Experience Questionnaire
- NRS:
-
Numeric rating scale
- W-DEQ:
-
Wijma Delivery Expectancy/Experience Questionnaire
References
Hodnett ED. Pain and women's satisfaction with the experience of childbirth: A systematic review. Am J Obstet Gynecol. 2002;186(5, Supplement):160–72. https://doi.org/10.1016/S0002-9378(02)70189-0.
Waldenström U, Hildingsson I, Rubertsson C, Rådestad I. A negative birth experience: Prevalence and risk factors in a national sample. Birth. 2004;31(1):17–27. https://doi.org/10.1111/j.0730-7659.2004.0270.x.
Gottvall K, Waldenström U. Does a traumatic birth experience have an impact on future reproduction? BJOG-Int J Obstet Gy. 2002;109(3):254–60.
Shorey S, Yang YY, Ang E. The impact of negative childbirth experience on future reproductive decisions: A quantitative systematic review. J Adv Nurs. 2018;74(6):1236–44.
Larsson C, Saltvedt S, Edman G, Wiklund I, Andolf E. Factors independently related to a negative birth experience in first-time mothers. Sex Reprod Healthc. 2011;2(2):83–9. https://doi.org/10.1016/j.srhc.2010.11.003.
Turkmen S, Tjernström M, Dahmoun M, Bolin M. Post-partum duration of satisfaction with childbirth. J Obstet Gynaecol Res. 2018;44(12):2166–73. https://doi.org/10.1111/jog.13775.
Falk M, Nelson M, Blomberg M. The impact of obstetric interventions and complications on women’s satisfaction with childbirth a population based cohort study including 16,000 women. BMC Pregnancy Childbirth. 2019;19(1):494. https://doi.org/10.1186/s12884-019-2633-8.
Adler K, Rahkonen L, Kruit H. Maternal childbirth experience in induced and spontaneous labour measured in a visual analog scale and the factors influencing it; a two-year cohort study. BMC Pregnancy Childbirth. 2020;20(1):415. https://doi.org/10.1186/s12884-020-03106-4.
Mishanina E, Rogozinska E, Thatthi T, Uddin-Khan R, Khan KS, Meads C. Use of labour induction and risk of cesarean delivery: A systematic review and meta-analysis. CMAJ. 186(9):665–73 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4049989/.
Middleton P, Shepherd E, Crowther CA. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev. 2018;5(5) https://pubmed.ncbi.nlm.nih.gov/29741208/.
Davey M, King J. Caesarean section following induction of labour in uncomplicated first births- a population-based cross-sectional analysis of 42,950 births. BMC Pregnancy Childbirth. 2016;16(92) https://pubmed.ncbi.nlm.nih.gov/27121614/.
Pyykönen A, Tapper A, Gissler M, Haukka J, Petäjä J, Lehtonen L. Propensity score method for analyzing the effect of labor induction in prolonged pregnancy. Acta Obstet Gynecol Scand. 2018;97(4):445–53 https://pubmed.ncbi.nlm.nih.gov/28832917/.
Keulen JK, Bruinsma A, Kortekaas JC, van Dillen J, van der Post JAM, de Miranda E. Timing induction of labour at 41 or 42 weeks? A closer look at time frames of comparison: A review. Midwifery. 2018;66:111–8.
Gülmezoglu AM, Crowther CA, Middleton P, Heatley E. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev. 2012;6(6) https://pubmed.ncbi.nlm.nih.gov/22696345/.
Schaal NK, Fehm T, Albert J, et al. Comparing birth experience and birth outcome of vaginal births between induced and spontaneous onset of labour: A prospective study. Arch Gynecol Obstet. 2019;300(1):41–7. https://doi.org/10.1007/s00404-019-05150-8.
Bossano CM, Townsend KM, Walton AC, Blomquist JL, Handa VL. The maternal childbirth experience more than a decade after delivery. Am J Obstet Gynecol. 2017;217(3):342.e1–8. https://doi.org/10.1016/j.ajog.2017.04.027.
Blomquist JL, Quiroz LH, MacMillan D, Mccullough A, Handa VL. Mothers’ satisfaction with planned vaginal and planned cesarean birth. Am J Perinatol. 2011;28(5):383.
Carquillat P, Boulvain M, Guittier M. How does delivery method influence factors that contribute to women's childbirth experiences? Midwifery. 2016;43:21–8.
Kempe P, Vikström-Bolin M. Women’s satisfaction with the birthing experience in relation to duration of labour, obstetric interventions and mode of birth. Eur J Obstet Gynecol Reprod Biol. 2020;246:156–9 https://www.ejog.org/article/S0301-2115(20)30050-6/abstract.
Ayers S, Pickering AD. Women's expectations and experience of birth. Psychol Health. 2005;20(1):79–92. https://doi.org/10.1080/0887044042000272912.
Rouhe H, Salmela-Aro K, Halmesmäki E, Saisto T. Fear of childbirth according to parity, gestational age, and obstetric history. BJOG-Int J Obstet Gy. 2009;116(1):67–73. https://doi.org/10.1111/j.1471-0528.2008.02002.x.
Joensuu J, Saarijärvi H, Rouhe H, Gissler M, Ulander VM, Heinonen S, Mikkola T. Maternal childbirth experience and time of delivery: A retrospective seven-year cohort study of 105,847 parturients in Finland. BMJ Open 2021 (accepted to publication)
Wu Y, Kataria Y, Wang Z, Ming W, Ellervik C. Factors associated with successful vaginal birth after a cesarean section: A systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019;19(1):1–12.
Hildingsson I, Karlström A, Nystedt A. Women’s experiences of induction of labour – findings from a swedish regional study. Aust N Z J Obstet Gynaecol. 2011;51(2):151–7. https://doi.org/10.1111/j.1479-828X.2010.01262.x.
Spaich S, Welzel G, Berlit S, et al. Mode of delivery and its influence on women's satisfaction with childbirth. Eur J Obstet Gynecol Reprod Biol. 2013;170(2):401–6. https://doi.org/10.1016/j.ejogrb.2013.07.040.
Henderson J, Redshaw M. Women's experience of induction of labor: A mixed methods study. Acta Obstet Gynecol Scand. 2013;92(10):1159–67. https://doi.org/10.1111/aogs.12211.
Jacquemyn Y, Michiels I, Martens G. Elective induction of labour increases caesarean section rate in low risk multiparous women. Obstet Gynaecol. 2012;32(3):257–9.
Langhoff-Roos J, Krebs L, Klungsøyr K, et al. The Nordic medical birth registers–a potential goldmine for clinical research. Acta Obstet Gynecol Scand. 2014;93(2):132–7.
Wijma K, Wijma B, Zar M. Psychometric aspects of the W-DEQ; a new questionnaire for the measurement of fear of childbirth. J Psychosom Obstet Gynaecol. 1998;19(2):84–97 https://pubmed.ncbi.nlm.nih.gov/9638601/.
Waldenström U. Why do some women change their opinion about childbirth over time? Birth. 2004;31(2):102–7. https://doi.org/10.1111/j.0730-7659.2004.00287.x.
Maimburg RD, Væth M, Dahlen H. Women's experience of childbirth – A five year follow-up of the randomised controlled trial “Ready for child trial”. Women Birth. 2016;29(5):450–4. https://doi.org/10.1016/j.wombi.2016.02.003.
Roberts L, Henry A, Harvey SB, et al. Depression, anxiety and posttraumatic stress disorder six months following preeclampsia and normotensive pregnancy: a P4 study. BMC Pregnancy Childbirth. 2022;22(1):108. https://doi.org/10.1186/s12884-022-04439-y.
Acknowledgements
Not applicable.
Funding
This study was supported by Helsinki University Hospital Research Grant. Open access funded by Helsinki University Library.
Author information
Authors and Affiliations
Contributions
JJ carried out the statistical analysis and wrote the first draft of the manuscript. The study was design by JJ, SH, TM, and HR. MG, V-MU, HS, PT, SH, TM and HR made contributions to the interpretation of data and significant revisions to the first draft. All authors revised successive versions of the article and approved the final article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional review board gave the permission (HUS/483/2020) to use the data and waived the requirement of the informed consent for the study since it was a register-based study. We confirm that the study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Joensuu, J.M., Saarijärvi, H., Rouhe, H. et al. Maternal childbirth experience and induction of labour in each mode of delivery: a retrospective seven-year cohort study of 95,051 parturients in Finland. BMC Pregnancy Childbirth 22, 508 (2022). https://doi.org/10.1186/s12884-022-04830-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04830-9