Abstract
Background
Obstetric anal sphincter injury (OASI) is a common and severe complication of vaginal delivery and may have short- and long-term consequences, including anal incontinence, sexual dysfunction and reduced quality of life. The rate of OASI varies substantially between studies and national birth statistics, and a recent meta-analysis concluded that there is a need to identify unrecognized risk factors. Our aim was therefore to explore both potential modifiable and non-modifiable risk factors for OASI.
Methods
We performed a case–control study in a single center maternity clinic in South-Eastern Norway. Data were extracted retrospectively from an institutional birth registry. The main outcome measure was the occurrence of the woman’s first-time 3rd or 4th degree perineal lesion (OASI) following singleton vaginal birth after 30 weeks’ gestation. For each woman with OASI the first subsequent vaginal singleton delivery matched for parity was elected as control. The study population included 421 women with OASI and 421 matched controls who gave birth during 1990–2002. Potential risk factors for OASI were assessed by conditional logistic regression analyses.
Results
The mean incidence of OASI was 3.4% of vaginal deliveries, but it increased from 1.9% to 5.8% during the study period. In the final multivariate regression model, higher maternal age and birthweight for primiparous women, and higher birthweight for the multiparous women, were the only non-modifiable variables associated with OASI. Amniotomy was the strongest modifiable risk factor for OASI in both primi- (odds ratio [OR] 4.84; 95% confidence interval [CI] 2.60–9.02) and multiparous (OR 3.76; 95% CI 1.45–9.76) women, followed by augmentation with oxytocin (primiparous: OR 1.63; 95% CI 1.08–2.46, multiparous: OR 3.70; 95% CI 1.79–7.67). Vacuum extraction and forceps delivery were only significant risk factors in primiparous women (vacuum: OR 1.91; 95% CI 1.03–3.57, forceps: OR 2.37; 95% CI 1.14–4.92), and episiotomy in multiparous women (OR 2.64; 95% CI 1.36–5.14).
Conclusions
Amniotomy may be an unrecognized independent modifiable risk factor for OASI and should be further investigated for its potential role in preventive strategies.
Similar content being viewed by others
Introduction
Most women experience perineal trauma of varying severity when giving vaginal birth [1]. Severe perineal lesions, referred to as obstetric anal sphincter injury (OASI), are diagnosed in as many as 11% of vaginal deliveries, but with significant variation between studies and national birth statistics [1,2,3,4,5]. The true incidence rate may be as high as 26% because the injuries can be overlooked at the delivery wards or be occult [4, 6]. Apart from the immediate perineal pain, OASI often has short- and long-term consequences including negative impact on sexual life and quality of life in general, including anal incontinence [7,8,9,10].
Adequate clinical examination following delivery is pivotal in the diagnosis of OASI [11, 12], and increased awareness and training of health care personnel have resulted in a doubling of detection rates [2, 12]. Alongside the focus on detection, prevention has gained increasing attention. Obstetric training programs for midwives with emphasis on potential preventive measures, such as attention to birth position and perineal massage during the second stage of labor, have been suggested as ways of decreasing the risk of OASI [13,14,15]. Implementation of a preventive program in five maternity clinics in Norway resulted in a decreased prevalence of OASI [16], as has similar programs in more recent studies in other European countries [17,18,19,20]. However, the evidence of persistent efficacy of preventive programs is weak, partly because the existing studies were assessed shortly after their introduction [21]. In a study involving the four large Nordic countries over seven years, a lasting reduction was only observed in Norway [22].
Established risk factors for OASI include primiparity, vaginal birth after caesarean delivery, advanced maternal age, high birthweight, fetal occiput posterior presentation, induction and augmentation of labor, instrumental delivery, increased duration of second stage of labor, episiotomy, and Asian ethnicity [1, 2, 23, 24]. A meta-analysis published in 2020 showed that the incidence of OASI remains high, and the need to search for hitherto unrecognized and potentially modifiable risk factors was highlighted [1]. We aimed at exploring both modifiable and non-modifiable risk factors in a large retrospective case–control study based on a regional cohort where detailed information related to maternal, pregnancy, delivery, and fetal characteristics had been collected prospectively.
Methods
Study design, setting and participants
At Innlandet Hospital Trust, Lillehammer, Norway, detailed information on maternal health, pregnancy, delivery, and the postpartum period until discharge is prospectively registered in a perinatal database. This hospital covers virtually all births in a region with a population of around 90,000 people at the time of the study; around 23,000 lived in the city Lillehammer and the others in rural areas with small towns. The women were registered in the perinatal database at 18–20 weeks’ gestation when they met for the routine ultrasound assessment. This study included all deliveries that occurred from January 1st,1990 through December 31st, 2002. From the database we identified singleton vaginal deliveries with gestational age (GA) > 30 weeks where women for the first time were diagnosed with perineal rupture. The data were quality assured and expanded by scrutinizing delivery protocols, charts, and patient records. Women with 3rd and 4th degree OASI were defined as cases, and we selected the next vaginal singleton delivery with the same parity and GA > 30 weeks without OASI as a matched control. Writing of the manuscript was done according to the STROBE checklist for the reporting of cohort, case–control and cross-sectional studies. The research project was approved by the Norwegian Social Science Data Services (project number: 2614) and The Norwegian Data Protection Authority (reference code: 95/2691–2 GSØ). The study was financed through Innlandet Hospital Trust research fund, grant number 150434.
Definitions and interventions
OASI was diagnosed according to the International Classification of Diseases (ICD) 9 definition 664.2 and 664.3 (similar to ICD 10 codes O70.2 and O70.3). The included cases were diagnosed at the time of the tear by the midwife or physician in charge of the delivery and subsequently confirmed by a specialist in obstetrics and gynecology. Consequently, women with potential delayed diagnosis of OASI are not included.
In addition to degree of perineal rupture, modifiable and non-modifiable variables regarding the infant, mother and birth process were registered. Non-modifiable variables included birth weight (gram), length (cm), head circumference (cm), gestational age (GA) (weeks), and maternal age (years), parity, duration of the first and second stage of labor (minutes), and fetal presentation (occiput posterior, occiput anterior, deep transverse, breech). Modifiable variables included the mother’s birth position (supine/sitting, side bearing, standing, kneeling, or on stool), induction of labor (yes/no), amniotomy (yes/no), episiotomy (mediolateral, yes/no), augmentation with oxytocin (yes/no), and instrumental delivery by vacuum extraction (yes/no) or forceps (yes/no).
Methods used for induction of labor were based on the Bishop scores and included membrane sweeping, transcervical Foley catheter, prostaglandin vaginal tablets, amniotomy or/and augmentation with oxytocin. Amniotomy was performed in births with a spontaneous onset when continuous surveillance of the fetus with a scalp-electrode or an examination of the amniotic fluid was considered necessary. Furthermore, amniotomy was employed before augmentation with oxytocin in cases of labor dystocia. Indications for performing an episiotomy included imminent fetal asphyxia, preterm birth. Instrumental vaginal delivery included vacuum extraction and the use of forceps at the physician’s discretion.
Birthweight was categorized into quartiles: < 3300, 3300–3659, 3660–4039, and ≥ 4040 g. Crown-heel length and head circumference were measured according to protocol. GA was estimated according to routine ultrasonography at 18–20 weeks of gestation at Lillehammer Hospital. Maternal age was categorized into the following three groups: < 25, 25–29, and ≥ 30 years. The cases and controls were stratified to primiparous (first birth) or multiparous (≥ second birth).
Statistical analyses
Missing data were treated by listwise deletion. Continuous variables were tested for distributions of normality and described by means and standard deviations. Categorical variables were described by frequencies and proportions. We performed separate analyses for the primi- and multiparous pregnancies. In addition, we performed subgroup regression analyses for cases and controls giving their 3rd birth or more. For the variables within each group, we analyzed differences between cases and controls with t-tests, Kruskal–Wallis or Chi2-tests. Significance level was set at 5%. Correlation matrices demonstrated covariation between weight, length, and head circumference of the infant, and only birthweight was used in logistic regression analyses. We used univariate conditional logistic regression analyses when assessing associations between exposure variables and OASI. Apart from birth length and head circumference, all registered modifiable and non-modifiable variables were tested in the univariate regression analyses. Subsequently, we built risk-factor models for OASI by using multivariate conditional logistic regression analyses progressing with a stepwise procedure. In this analysis we included variables that were significantly different between the cases and controls in the univariate analyses. We assessed multicollinearity by using variance inflation factor (VIF). We assessed interactions between amniotomy and the following variables: augmentation with oxytocin, episiotomy, and instrumental delivery by vacuum or forceps. STATA 16.1 software (STATA, College Station, TX, United States: StataCorp, 2020) was used for all the analyses.
Results
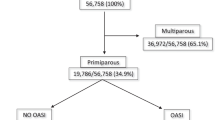
During this 13-year period, 12,883 women gave birth at the study hospital, and 11,374 of them had a vaginal delivery. The mean incidence of first time OASI after vaginal delivery was 3.4% (n = 421), but the rate increased gradually from 1.9% in 1990 to a maximum of 5.8% in 2002 (Fig. 1). Of the 421 women with OASI and their matched controls, 275 (65%) were primiparous and 146 (35%) multiparous (104 had their 2nd, 33 their 3rd, 5 their 4th, 3 their 5th, and one her 6th child). Both the primiparous and multiparous women with OASI differed similarly from their matched controls both on non-modifiable characteristics (larger size of the baby, higher GA, higher maternal age, and longer 1st and 2d stage of labor) and modifiable characteristics (higher rates of amniotomy, augmentation of labor with oxytocin, and instrumental delivery). The multiparous women with OASI also had a higher rate of episiotomy (Table 1).
In the final multivariate conditional logistic regression model, higher maternal age and birthweight for the primiparous women and birthweight for the multiparous women were the only non-modifiable variables associated with rates of OASI (Tables 2 and 3).
Of the modifiable variables, amniotomy was strongly associated with OASI, both in the primiparous (OR 4.84, 95% CI 2.60–9.02) and multiparous (OR 3.76, 95% CI 1.45–9.76) women, as was augmentation with oxytocin (OR 1.63, 95% CI 1.08–2.46 and 3.70, 95% CI 1.79–7.67, respectively, Tables 2 and 3). Instrumental delivery was associated with OASI in the primiparous women (Table 2) and episiotomy with OASI in the multiparous women (Table 3). The same trend, but not statistically significant, was found for the non-modifiable and modifiable variables when limiting the conditional regression analysis to the subgroup of women who gave birth to their 3rd or later child (n = 84). We found no significant interactions or multicollinearities.
Discussion
In this unselected population, OASI was associated with known non-modifiable factors like high maternal age, first pregnancy, and large babies. Of potentially modifiable factors, OASI was associated with induction of labor and instrumental vaginal delivery in primiparous women, and with amniotomy and augmentation with oxytocin in both primi- and multiparous women, procedures that are primarily initiated to accelerate delivery.
The major strengths of this study were the unselected population, the large number of participants, and completeness of data. We also consider the inclusion of only one obstetric hospital a strength since no major official changes in routines were introduced, although we cannot exclude gradual unrecognized changes during this 13-year period. The retrospective nature of the study may be a weakness since reasons for performing amniotomy and augmentation with oxytocin were not necessarily specified and since vigilance in classifying perineal rupture may have been less accurate than in a planned prospective study. Furthermore, we have no data on OASI diagnosed after discharge from the hospital. The time lap between the collection and publication of data may make the results less valid of today’s practice since increased focus on reducing the incidence of OASI has been implemented since the data were collected [13, 16]. According to the Medical Birth Registry of Norway, there has been a reduction in the proportion of women experiencing OASI after vaginal birth since our study was conducted (1.6 in 2020 vs 4.6 in 2003) [25]. This decrease has occurred even though the proportions of labor inductions and augmentation with oxytocin have increased nationally in the same period [25]. We speculate that a more cautious use of amniotomy may have contributed to the decline since our results became widely known in Norway at the time when the data were collected.
To our knowledge, our study is the first to include amniotomy as a potential independent risk factor for OASI. A recent meta-analysis on risk factors for severe perineal trauma in child birth only identified one study that addressed the potential role of amniotomy [1]. However, the significance of amniotomy per se could not be assessed because it was combined with the use of oxytocin for augmentation of labor. In our study, amniotomy was the strongest independent modifiable risk factor regardless of parity and suggests that attention to indications and timing of amniotomy may be a hitherto unrecognized means of preventing OASI. The use of amniotomy varies between institutions both in Norway and other countries and ranges from 20 to 60% [26, 27]. However, in our experience the documentation of amniotomy in patient charts during labor is highly variable. Even though we have a national high-quality birth registry in Norway, the use of amniotomy in spontaneous labor has not reported since 1998 [25].
With the goal of reducing cesarean births through active management of labor, amniotomy has been widely and readily accepted to avoid labor for more than 12 h [28]. However, reducing length of labor might not be a benefit for all women, and a Cochrane review from 2013 concluded that there is no evidence to support routine amniotomy to shorten spontaneous labor or to avoid prolonged labor [29]. The mechanism behind the association between amniotomy and OASI is unclear, but we speculate that amniotomy may disrupt the normal physiologic process of gradual adaptation of the birth canal and thereby a higher risk of trauma. Thus, our findings indicate that untimely use of amniotomy may act in line with other established indicators of pathologic birth mechanics such as high birth weight, large head circumference, fetal occiput presentation, prolonged second stage of labor, augmentation with oxytocin, episiotomy, and instrumental delivery [1].
In the present study, we also found that augmentation with oxytocin was an independent risk factor for OASI for both primi- and multiparous women. This is in accordance with previous studies [1]. Augmentation with oxytocin is widely used when labor is delayed, and probably more than half of women in labor worldwide receive oxytocin augmentation [25, 27]. However, the use of augmentation varies widely between countries and within the same country. In our study, 60% of the primiparous and 47% of the multiparous women were augmented with oxytocin, which is in line with current rates in maternity wards in Norway [27]. Increased frequency and intensity of contractions are known potential adverse effect of augmentation of labor with oxytocin [30]. We suggest that the effects of augmentation with oxytocin are similar to that of amniotomy in that the birth progress may be more rapid than the natural adaptation of the birth canal.
Instrumental vaginal delivery is a well-established risk factor for OASI [1, 2, 24]. However, this was only an independent risk factor in primiparous women in our study. Instrumental delivery was also associated with OASI in multiparous women in the unadjusted analysis, and the reason for no significant association in the adjusted analysis may partly be that the study lacked power to detect a risk since instruments were rarely used in this group.
In conclusion, the study suggests that indications for and timing of amniotomy and augmentation of the birth process with oxytocin need to be readdressed in order to reduce the risk of severe perineal ruptures.
Availability of data and materials
The dataset generated and analysed during the current study are not publicly available due to restrictions in data-sharing of the institutional perinatal database but are available from the corresponding author on reasonable request, MNH-A, upon reasonable request.
Abbreviations
- CI:
-
Confidence interval
- OR:
-
Odds ratio
- OASI:
-
Obstetric anal sphincter
References
Pergialiotis V, Bellos I, Fanaki M, Vrachnis N, Doumouchtsis SK. Risk factors for severe perineal trauma during childbirth: an updated meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2020;247:94–100.
Ampt AJ, Ford JB, Roberts CL, Morris JM. Trends in obstetric anal sphincter injuries and associated risk factors for vaginal singleton term births in New South Wales 2001–2009. Aust N Z J Obstet Gynaecol. 2013;53(1):9–16.
Jha S, Parker V. Risk factors for recurrent obstetric anal sphincter injury (rOASI): a systematic review and meta-analysis. Int Urogynecol J. 2016;27(6):849–57.
Dudding TC, Vaizey CJ, Kamm MA. Obstetric anal sphincter injury: incidence, risk factors, and management. Ann Surg. 2008;247(2):224–37.
Laine K, Gissler M, Pirhonen J. Changing incidence of anal sphincter tears in four Nordic countries through the last decades. Eur J Obstet Gynecol Reprod Biol. 2009;146(1):71–5.
Oberwalder M, Connor J, Wexner SD. Meta-analysis to determine the incidence of obstetric anal sphincter damage. Br J Surg. 2003;90(11):1333–7.
Gommesen D, Nohr EA, Qvist N, Rasch V. Obstetric perineal ruptures-risk of anal incontinence among primiparous women 12 months postpartum: a prospective cohort study. Am J Obstet Gynecol. 2020;222(2):165 (e1- e11).
Leeman L, Rogers R, Borders N, Teaf D, Qualls C. The effect of perineal lacerations on pelvic floor function and anatomy at 6 months postpartum in a prospective cohort of nulliparous women. Birth. 2016;43(4):293–302.
Cornelisse S, Arendsen LP, van Kuijk SM, Kluivers KB, van Dillen J, Weemhoff M. Obstetric anal sphincter injury: a follow-up questionnaire study on longer-term outcomes. Int Urogynecol J. 2016;27(10):1591–6.
LaCross A, Groff M, Smaldone A. Obstetric anal sphincter injury and anal incontinence following vaginal birth: a systematic review and meta-analysis. J Midwifery Womens Health. 2015;60(1):37–47.
Groom KM, Paterson-Brown S. Can we improve on the diagnosis of third degree tears? Eur J Obstet Gynecol Reprod Biol. 2002;101(1):19–21.
Harvey MA, Pierce M, Alter JE, Chou Q, Diamond P, Epp A, et al. Obstetrical Anal Sphincter Injuries (OASIS): prevention, recognition, and repair. J Obstet Gynaecol Can. 2015;37(12):1131–48.
Laine K, Skjeldestad FE, Sandvik L, Staff AC. Incidence of obstetric anal sphincter injuries after training to protect the perineum: cohort study. BMJ Open. 2012;2(5):e001649.
Naidu M, Sultan AH, Thakar R. Reducing obstetric anal sphincter injuries using perineal support: our preliminary experience. Int Urogynecol J. 2017;28(3):381–9.
Tunestveit JW, Baghestan E, Natvig GK, Eide GE, Nilsen ABV. Factors associated with obstetric anal sphincter injuries in midwife-led birth: A cross sectional study. Midwifery. 2018;62:264–72.
Hals E, Oian P, Pirhonen T, Gissler M, Hjelle S, Nilsen EB, et al. A multicenter interventional program to reduce the incidence of anal sphincter tears. Obstet Gynecol. 2010;116(4):901–8.
De Meutter L, van Heesewijk AD, van der Woerdt-Eltink I, de Leeuw JW. Implementation of a perineal support programme for reduction of the incidence of obstetric anal sphincter injuries and the effect of non-compliance. Eur J Obstet Gynecol Reprod Biol. 2018;230:119–23.
Pirhonen J, Samuelsson E, Pirhonen T, Odeback A, Gissler M. Interventional program to reduce both the incidence of anal sphincter tears and rate of Caesarean sections. Eur J Obstet Gynecol Reprod Biol. 2018;223:56–9.
Jango H, Westergaard HB, Kjaerbye-Thygesen A, Langhoff-Roos J, Lauenborg J. Changing incidence of obstetric anal sphincter injuries-A result of formal prevention programs? Acta Obstet Gynecol Scand. 2019;98(11):1455–63.
Gurol-Urganci I, Bidwell P, Sevdalis N, Silverton L, Novis V, Freeman R, et al. Impact of a quality improvement project to reduce the rate of obstetric anal sphincter injury: a multicentre study with a stepped-wedge design. BJOG. 2021;128(3):584–92.
Poulsen MO, Madsen ML, Skriver-Moller AC, Overgaard C. Does the Finnish intervention prevent obstetric anal sphincter injuries? A systematic review of the literature. BMJ Open. 2015;5(9):e008346.
Laine K, Rotvold W, Staff AC. Are obstetric anal sphincter ruptures preventable?– large and consistent rupture rate variations between the Nordic countries and between delivery units in Norway. Acta Obstet Gynecol Scand. 2013;92(1):94–100.
Hehir MP, Fitzpatrick M, Cassidy M, Murphy M, O’Herlihy C. Are women having a vaginal birth after a previous caesarean delivery at increased risk of anal sphincter injury? BJOG. 2014;121(12):1515–20.
Ramm O, Woo VG, Hung YY, Chen HC, RittermanWeintraub ML. Risk factors for the development of obstetric anal sphincter injuries in modern obstetric practice. Obstet Gynecol. 2018;131(2):290–6.
Health TNIoP. 2021 [cited 2021 24.03.2021]. Available from: https://www.fhi.no/en/hn/health-registries/medical-birth-registry-of-norway/.
Seijmonsbergen-Schermers AE, Zondag DC, Nieuwenhuijze M, van den Akker T, Verhoeven CJ, Geerts CC, et al. Regional variations in childbirth interventions and their correlations with adverse outcomes, birthplace and care provider: a nationwide explorative study. PLoS One. 2020;15(3):e0229488.
Gaudernack LC, Froslie KF, Michelsen TM, Voldner N, Lukasse M. De-medicalization of birth by reducing the use of oxytocin for augmentation among first-time mothers - a prospective intervention study. BMC Pregnancy Childbirth. 2018;18(1):76.
O’Driscoll K, Meagher D, Boylan P. Active management of labour. 3rd ed. London: Mosby; 1993.
Smyth RM, Alldred SK, Markham C. Amniotomy for shortening spontaneous labour. Cochrane Database Syst Rev. 2013;1:CD006167.
Oscarsson ME, Amer-Wahlin I, Rydhstroem H, Kallen K. Outcome in obstetric care related to oxytocin use. A population-based study. Acta Obstet Gynecol Scand. 2006;85(9):1094–8.
Acknowledgements
None.
Funding
The study was financed through Innlandet Hospital Trust research fund, grant number 150434.
Author information
Authors and Affiliations
Contributions
As the principal investigator, RK contributed to the conceptualization, planning and carrying out of the study. RK also participated in the analyses of the data and writing of the manuscript. KSB contributed to the analyses of the data and the writing of the manuscript. TM contributed to the conceptualization, planning and implementation of the study and in the writing of the manuscript. TM also supervised the analyses of the data. MNH-A carried out the cleaning and analyses of the data and contributed to the writing of the manuscript. All the authors have read and approved the final manuscript and agree to its publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research project was approved by the Norwegian Social Science Data Services (project number: 2614) and The Norwegian Data Protection Authority (reference code: 95/2691–2 GSØ). Participation in the study was based on informed consent from all included women. All methods were carried out in accordance with relevant guidelines and regulations. STROBE guidelines for observational studies were followed in the preparation of the manuscript.
Consent for publication
Not applicable for the current study.
Competing interests
No competing interests for any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Klokk, R., Bakken, K.S., Markestad, T. et al. Modifiable and non-modifiable risk factors for obstetric anal sphincter injury in a Norwegian Region: a case–control study. BMC Pregnancy Childbirth 22, 277 (2022). https://doi.org/10.1186/s12884-022-04621-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04621-2




