Abstract
Background
It is believed that HPV infection can result in the death of placental trophoblasts and cause miscarriages or preterm birth. In clinical cases of placental villi positive for HPV DNA reported by other authors, contamination is suspected in the act of crossing the cervical canal. We analyzed placental samples of women who resorted to elective abortion obtained by hysterosuction of ovular material, bypassing any contact with the cervical canal and vagina.
Methods
We studied the chorionic villi of the placenta of 64 women who resorted to voluntary termination of pregnancy, in the first trimester. To avoid contamination of the villi by the cervical canal, we analyzed placental samples obtained by hysterosuction of ovular material, bypassing any contact with the cervical canal and vagina. All samples of chorionic villi were manually selected from the aborted material and subjected to research for HPV DNA.
Results
HPV DNA was detected in 10 out of 60 women (16.6%). The HPV DNA identified in the placenta belonged to genotypes 6, 16, 35, 53, and 90.
Conclusion
The study shows that papillomavirus DNA can infect the placenta and that placenta HPV infection can occur as early as the first trimester of pregnancy.
Similar content being viewed by others
Background
Human papillomavirus infection (HPV) is a sexually transmitted disease associated with cervical carcinogenesis whose prevalence of genotypes shows significant differences worldwide [1, 2]. In its single or multiple form [3] persistent high-risk human papilloma virus infection (hr HPV) is necessary [4] for progression of Cervical Intraepithelial Neoplasia (CIN) lesions. HPV infection is the most common sexually transmitted disease (STD) in the world, however, recent studies have shown that the infection can also be acquired by vertical transmission and through the placenta from mother to child [5, 6].
Recently, it was discovered that the HPV virus is capable of infecting trophoblast cells as well as squamous cells [7]. This discovery adding further support to the proposed association between HPV infection and miscarriage. In fact, trophoblast cells play a crucial role in the placentation process [8] and it is believed that HPV infection can result in the death of placental trophoblasts and cause miscarriages or preterm birth [9].
Evidence of HPV transmission through the placenta is not without controversy; in fact, HPV DNA was detected with a wide prevalence range of 4 to 75% in the placenta of women who miscarried and in 20–24% of women who underwent voluntary termination of pregnancy [10,11,12]. Eppel et al. [13] did not find HPV DNA in any of the 147 placental villi samples collected by transabdominal amniocentesis. In addition, in clinical cases of placental villi positive for HPV DNA reported by other studies, contamination is suspected in the act of crossing the vagina.
We investigated the presence of HPV in the placenta of women in the first trimester of pregnancy, who asked for termination of pregnancy (TOP), in order to verify the hypothesis that the placenta may be infected with HPV and that this manifests as early as the first trimester of pregnancy.
Methods
From May 2019 to June 2020 we studied the chorionic villi of the placenta of 64 women who asked for TOP. The gestational age of women was between the 7th and 12th week. The decision on whether or not to participate in the study was at the patient’s discretion and the patient was not disadvantaged in any other way for refusing to participate in the study. Subjects were excluded if they had evidence of immunosuppression (HIV infection, transplantation, malignant tumor) or had been vaccinated against HPV. The women were invited to participate regardless of whether they had a history of HPV genital infection. The viral status (cervical HPV DNA) of the mother was not reported deliberately, first, because the aim of the research is to demonstrate the presence of HPV DNA in the placenta, second, because some data are incomplete and the risk is to reduce the number of women of the study group, already small. The prospective observational study was approved by the local institutional review committee (n. 154/2019/PO) and written informed consent was obtained from all study participants. Participants responded to a questionnaire with demographic and clinical data in order to characterize the study group (supplementary file).
Since other studies on vertical HPV transmission were often hampered by the possible contamination of the placenta with vaginal cells from an infected birth canal, other authors used the transabdominal pathway, whereas we analyzed placental samples obtained by hysterosuction of ovular material, bypassing any contact with the cervical canal and vagina.
Women were administred prostaglandins (geneprost 1 mg) by vaginal pessaries to dilate the cervix to such an extent that a cannula (Karman’s cannula) could be introduced in the uterus, which was connected to an aspirator to aspirate ovular material. In order to avoid contamination of the ovular material with HPV coming from the maternal vagina, we resorted to a particular method. We inserted a 10 mm Karman cannula into the already dilated cervix. This cannula acts as a shirt, through which a 6 mm Karman cannula reaches the uterine cavity and aspirates the ovular material, without contaminating it. Furthermore, the cervical canal lined with cylindrical cells, is hardly contaminated by papillomavirus as it has a particular tropism for the squamous epithelial cells that line the vagina and the uterine portio; this is even more so in pregnant women whose cervix is characterized by a physiological eversion of the endocervical mucosa on the uterine portio. Moreover, the cervix represents not only an anatomical barrier but also an immunological barrier against ascending infection through mucus production, inflammatory cytokines and antimicrobial peptides. All samples of chorionic villi were manually selected from the aborted material and subjected to research for HPV DNA.
Samples and isolation of nucleic acid from chorionic villi
We have chosen to work on fresh, non-paraffinized placental tissue: in order to make the sample as homogeneous as possible. The placental tissue was processed in a sterile hood and, using a petri dish as a support, reduced to very small pieces using a scalpel from which 3 small sample sections from 3 different points were taken and placed into an Eppendorf type test tube. Following this, the treatment continued with cellular lysis by adding the lysis buffer (ATL buffer) and proteinase K with overnight incubation at 55 °C.
The day after the extraction continued using the commercial HIGH Pure PCR Template (ROCHE) kit which is based on the ability of DNA to bind to inert media or filters contained in columns; subsequently the nucleic acids bound to the filter were eluted through elution buffer and the eluate was stored at − 80 °C until the moment of use.
DNA amplification
For the amplification of HPV DNA the Ampliquality kit HPV-TYPE EXPRESS v 3.0 (AB ANALITICA srl, Padova, Italy) was used. The kit is based on a rapid system for the identification of human Papillomavirus by single step PCR: in the preparation of the PCR session, in addition to the samples, a positive amplification and typing control (HPV 61 DNA) as well as a negative control (sterile distilled water) were also used; in addition, the kit can evaluate the suitability of the DNA extracted by the amplification of the TST gene (thiosulfate sulfurtransferase rhodanese).
The PCR mix was divided into a sufficient number of test tubes for the analysis of samples and controls, as follows:
HPV-TYPE EXPRESS MIX 20ul.
Extracted DNA 5ul.
The test tubes were then transferred to a thermocycler with the previously programmed amplification profile.
DNA genotyping using reverse line blot
The subsequent genotyping of the amplified product was carried out by an allele-specific hybridization technique; it is a technique that includes a solid phase support in which specific probes (Reverse Line Blot) have been used and includes:
-
a-
Denaturing: the marked amplified product is denatured by chemical or thermal denaturation (incubation at 95 °C);
-
b-
Hybridization: the strip is incubated, under specific temperature conditions, agitation and phj with the solution containing the marked and denatured amplified product;
-
c-
Washes: to remove the excess marked amplified product and then to define the “astringency” of the hybridization;
-
d-
Detection: Displays the hybrid that was formed based on the type of marked probe (NBT/BCIP coloring solution).
The kit used for genotyping was Ampliquality HPV-TYPE EXPRESS, able to determine the presence of 40 types of Papillomavirus, in particular: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, 82, 26, 53, 66, 67, 6, 11, 40, 42, 43, 61, 69, 70, 44, 54, 55, 62, 64, 71, 72, 81, 83, 84, 87, 89, 90.
Statistical analysis
The statistical analysis of the data was carried out with the software package SPSS 15.0 (SPSS Inc.; Chicago, IL, USA). Descriptive statistics were expressed by frequency, arithmetic mean and percentages.
Results
Four women were excluded from the study for insufficient chorionic villi obtined
Consequently, HPV DNA sequences were studied in 60 samples. HPV DNA was detected in 10 out of 60 women (16.6%). The HPV DNA identified in the placenta belonged to genotypes 6, 16, 35, 53, and 90. The villi of five placentas (50%) had high carcinogenic HPV (HPV 16, 53, and 35) and two (16.7%, n = 2/10) had two different types of HPV DNA. HPV 16 was the most frequent genotype in this study. Genotype 6 was the second most frequent (Table 1).
Discussion
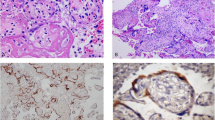
The aim of this study was to find evidence of HPV DNA in the placenta. Positive results from others anthors were affected by contamination of chorionic villi by a vaginal cells positive for papillomavirus [13]. To avoid contamination, authors such as Weyn [14] and Eppel used the transabdominal pathway to sample chorionic villi to be subjected to PCR. In our study, we analyzed the villi that come from the placentas of women who resorted to elective abortion and to avoid contamination of the villi by the vagina we used a procedure allowed us to aspirate ovular material through a cannula that was introduced through the already dilated cervical canal with the administration of local prostaglandins. Whereas the cervix represents not only an anatomical barrier but also an immunological barrier against ascending infection, this method allows the sampling of chorionic villi from the intrauterine cavity without coming into contact with the vagina, probably infected. We found 16.6% positive cases, therefore, our study undoubtedly demonstrates the presence of HPV in chorionic villi like the studies of Gomez [15] and of Weyn [14], which demonstrated the presence of HPV in placental samples obtained trans-abdominally, while the study of Eppel [13] reports the absence of HPV DNA in 147 placental samples obtained abdominally, probably due to the use of a less sensitive PCR. Furthermore, Chisanga et al. [16] demonstrated the presence of HPV in placental trophoblasts using both polymerase and immunohistochemistry chain reaction methods.
However, the path by which HPV infects the placenta is unknown. It is suspected to occur through the ascending vaginal pathway. In a healthy pregnancy, the growing uterus and fetus are protected from any upward infection by the cervix. The cervix plays a unique role in actively controlling and restricting microbial access through mucus production, inflammatory cytokines and antimicrobial peptides, and therefore represents not only an anatomical barrier but also an immunological barrier against ascending infection recognition receptors such as Toll like (TLR) in the cervical epithelium can detect the presence of microorganisms and elicit an innate immune response characterized by the production of cytokines and AMP [17].
Another possibility could be intrauterine transmission at the time of fertilization by latent HPV-carrying sperm; growing evidence indicates that HPV is found in the sperm of infertile males [18, 19].
The other way is hematogenic as HPV has been detected in the mononucleate cells of peripheral blood, suggesting a hematogenic diffusion path [20, 21]; however, no other data support the spread of the virus through blood. Studies on placental tissues have detected HPV genotypes in aborted tissues, including HPV 6, 11, 16, 18, 58, 66, 82, 83 while a clinical case of verruciform epidermodisplasia also reported the presence of HPV 3, 5, 8, 24, 36 [22]. In our study HPV 16 is the most frequent genotype, while genotype 6 was the second most frequent, in line with data in the literature showing that this genotype is related to vertical transmission. Genotypes 53 and 90 are very rare and little studied, it is thought that they are not related to any oncogenic activity although recently it has been shown that HPV 90 E6 is capable of completely degrading p53 with the same efficacy as HPV 16 E6 in an assay of single transfected cell [23].
The role of papillomavirus in the genesis of cervical cancer is now certain and one important factor is genotyping [24] since genotype 16, which is widespread, is responsible for 70% of cancer cases. During pregnancy, the mutated hormonal environment and immune response may promote the presence or persistence of HPV infection. Data on the prevalence of HPV infection in pregnancy are very discordant: Tenti et al. [25] reported 5.4%, while Cason et al. [26] reported 68.8%. The diversity of observed percentages is related to several factors that alone could influence the results, such as: sample characteristics, inclusion criteria and diagnostic techniques.
The human papillomavirus (HPV), was detected in the cervix in 15–25% of pregnant women [27, 28] and a cervical HPV infection during pregnancy was associated with an increased incidence of miscarriages [29], premature membrane rupture [30], spontaneous preterm birth, pre-eclampsia [31], and placental “villitis” not otherwise specified, however, HPV DNA was also discovered in the placenta of healthy pregnancies [32] and placenta samples obtained trans-abdominally. The relationship between HPV infection and pregnancy outcomes is unclear. Some studies have shown no association, while others have suggested that HPV infection, cervical disease and/or its treatment [33] are associated, in addition to changes in a woman’s sex life [34], with adverse outcomes of pregnancy, such as miscarriage, premature rupture of membranes or preterm birth. Hermonat, showed that HPV type 16 can replicate in trophoblasts [8] and You [5] on cultured 3A trophoblasts cells (chosen as the experimental cell type because they are well characterized and represent a near-normal trophoblast), showed that also other genotypes (11, 18, 31) are capable of reproducing in trophoblast cells. Oncogenic HPVs have pathologically important E6 / E7 bases and their oncogenicity is due in part to their ability to inactivate the cellular tumor suppressor genes, P53 and Rb, respectively. These two oncogenes have a vital functions in the development of HPV-associated cervical cancer. H. You [7] has shown that multiple physiological changes derive from the introduction of E6 and E7 in the trophoblasts 3. In fact, he for to evaluate the effects of E6 and E7, 3A trophoblast cells infected with recombinant adeno-associated viruses, while the AAV / NEO virus infection was used as a control. The investigation shows that there is a lack of recognition of highly defective endometrial cells and therefore a low adhesion of trophoblastic cells to the endometrium, the death of trophoblast cells for E7-induced apoptosis. Knowing the importance of good placentation for a physiological pregnancy, papillomavirus damage to the trophoblast strongly supports an HPV miscarriage link. In summary, the oncogenic component genes of HPV E6 and E7 have significant effects on the general cellular characteristics of trophoblasts, including cell survival, binding to endometrial cells, proliferation, differentiation, and immortalization. One could consider that any of these changes in trophoblasts it could be responsible for the alteration of the trophoblastic and placental physiology and could contribute to spontaneous abortions.
There is clearly a need for further research regarding the relationship between HPV infection and the abnormal course of early pregnancy leading to miscarriage or fetal defects.
While on the one hand our research has a limit represented by the small size of the sample studied, on the other it has a strong point represented by the particular method used to avoid contamination of the placenta with HPV coming from the maternal vagina.
Conclusion
Our study shows that papillomavirus DNA can infect the placenta and that placenta HPV infection can occur as early as the first trimester of pregnancy. The overall clinical implication of these results remains to be clarified.
Availability of data and materials
The dataset used and/or analyzed during the current study are available from the corresponding author on request.
Abbreviations
- STD:
-
Sexually transmitted disease
- CIN:
-
Cervical Intraepithelial Neoplasia
- HPV:
-
Human Papilloma Virus
- TOP:
-
Termination of Pregnancy
References
World Health Organization. World Cancer report 2014. International Agency for Research on Cancer; 2014:9 Accessed 12 Oct 2014.
Bruno MT, Ferrara M, Fava V, Cutello S, Sapia F, Panella MM. Prevalence genotypes and distribution of human papillomavirus infection in women with abnormal cervical cytology in Catania, Italy. Giornale Italiano di Ostetricia e Ginecologia. 2016;38(5–6):376–80.
Bruno MT, Scalia G, Cassaro N, Boemi S. Multiple HPV 16 infection with two strains: as possible marker of neoplastic progression. BMC Cancer. 2020;1:444.
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–9. https://doi.org/10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F.
Puranen MH, Yliskoski MH, Saarikoski SV, Syrjanen KJ, Syrjanen SM. Exposure of an infant to cervical human papillomavirus infection of the mother is common. Am J Obstet Gynecol. 1997;176:5,1039–45.
Hong Y, Li SQ, Hu YL, et al. Survey of human papillomavirus types and their vertical transmission in pregnant women. BMC Infect Dis. 2013;13:109. https://doi.org/10.1186/1471-2334-13-109.
You H, Liu Y, Agrawal N, Prasad CK, Edwards JL, Osborne AF, et al. Multiple human papillomavirus types replicate in 3A trophoblasts. Placenta. 2008;29(1):30–8. https://doi.org/10.1016/j.placenta.2007.08.005.
Liu Y, You H, Chiriva-Internati M, Korourian S, Lowery CL, Carey MJ, et al. Display of complete life cycle of human papillomavirus type 16 in cultured placental trophoblasts. Virology. 2001;290(1):99–105. https://doi.org/10.1006/viro.2001.1135.
You H, Liu Y, Carey MJ, Lowery CL, Hermonat PL. Defective 3A trophoblast-endometrial cell adhesion and altered 3A growth and survival by human papillomavirus type 16 oncogenes. Mol Cancer Res. 2002;1(1):25–31.
de Freitas LB, Pereira CC, Merçon-de-Vargas PR, Spano LC. Human papillomavirus in foetal and maternal tissues from miscarriage cases. J Obstet Gynaecol. 2018;38(8):1083–7. https://doi.org/10.1080/01443615.2018.1454408.
Ambühl LMM, Baandrup U, Dybkær K, Blaakær J, Uldbjerg N, Sørensen S. Human papillomavirus infection as a possible cause of spontaneous abortion and spontaneous preterm delivery. Infect Dis Obstet Gynecol. 2016;87:1181–8.
Hermonat PL, Han L, Wendel PJ, Quirk JG, Stern S, Lowery CL, et al. Human papillomavirus is more prevalent in first trimester spontaneously aborted products of conception compared to elective specimens. Virus Genes. 1997;14(1):13–7. https://doi.org/10.1023/a:1007975005433.
Eppel W, Worda C, Frigo P, Ulm U, Kucera E, Czerwenka K. Human papillomavirus in the cervix and placenta. Obstet Gynecol. 2000;96(3):337–41. https://doi.org/10.1016/s0029-7844(00)00953-4.
Weyn C, Thomas D, Jani J, Guizani M, Donner C, Rysselberge MV, et al. Evidence of human papillomavirus in the placenta. J Infect Dis. 2011;203(3):341–3. https://doi.org/10.1093/infdis/jiq056.
Gomez LM, Ma J, Ho C, McGrath CM, Nelson DB, Parry S. Placental infection with human papillomavirus is associated with spontaneous preterm delivery. Hum Reprod. 2008;23(3):709–15. https://doi.org/10.1093/humrep/dem404.
Chisanga C, Eggert A, Mitchell CD, Wood C, Angeletti PC. Evidence of placental HPV infection in HIV positive and negative women. Cancer Ther. 2015;6(15):1276–89. https://doi.org/10.4236/jct.2015.615140.
Hickey DK, Patel MV, Fahey JV, Wira CR. Innate and adaptive immunity at mucosal surfaces of the female reproductive tract: stratification and integration of immune protection against the transmission of sexually transmitted infections. J Reprod Immunol. 2011;88(2):185–94. https://doi.org/10.1016/j.jri.2011.01.005.
Foresta C, Garolla A, Zuccarello D, Pizzol D, Moretti A, Barzon L, et al. Human papillomavirus found in sperm head of young adult males affects the progressive motility. Fertil Steril. 2010;93(3):802–6. https://doi.org/10.1016/j.fertnstert.2008.10.050.
La Vignera S, Vicari E, Condorelli RA, Schillaci R, Calogero AE. Prevalence of human papilloma virus infection in patients with male accessory gland infection. Reprod BioMed Online. 2015;30(4):385–91. https://doi.org/10.1016/j.rbmo.2014.12.016.
Bodaghi S, Wood LV, Roby G, Ryder C, Steinberg SM, Zheng ZM. Could human papillomaviruses be spread through blood? J Clin Microbiol. 2005;43(11):5428–34. https://doi.org/10.1128/JCM.43.11.5428-5434.2005.
Pao CC, Lin SS, Lin CY, Maa JS, Lai CH, Hsieh TT. Identification of human papillomavirus DNA sequences in peripheral blood mononuclear cells. Am J Clin Pathol. 1991;95(4):540–6.
Favre M, Majewski S, De Jesus N, Malejczyk M, Orth G, Jablonska S. A possible vertical transmission of human papillomavirus genotypes associated with epidermodysplasia verruciformis. J Investig Dermatol. 1998;111(2):333–6. https://doi.org/10.1046/j.1523-1747.1998.00312.x.
Fu L, Van Doorslaer K, Chen Z, Ristriani T, Masson M, Trave G, et al. Degradation of p53 by human Alphapapillomavirus E6 proteins shows a stronger correlation with phylogeny than oncogenicity. PLoS One. 2010;5(9):e12816.
Bruno MT, Ferrara M, Fava V, Rapisarda A, Coco A. HPV genotype determination and E6/E7 mRNA detection for management of HPV positive women. Virol J. 2018;15(1):52. https://doi.org/10.1186/s12985-018-0957-z.
Tenti P, Zappatore R, Migliora P, Spinillo A, Maccarini U, De Benedittis M, et al. Latent human papillomavirus infection in pregnant women at term: a case-control study. J Infect Dis. 1997;176(1):277–80. https://doi.org/10.1086/517266.
Cason J, Kaye JN, Jewers RJ, Kambo PK, Bible JM, Kell B, et al. Perinatal infection and persistence of human papillomavirus types 16 and 18 in infants. J Med Virol. 1995;47(3):209–18. https://doi.org/10.1002/jmv.1890470305.
Koskimaa KM, Waterboer T, Pawlita M, et al. Human papillomavirus genotypes present in the oral mucosa of newborns and their concordance with maternal cervical human papillomavirus genotypes. J Pediatr. 2012;160(5):837–43. https://doi.org/10.1016/j.jpeds.2011.10.027.
Park H, Lee SW, Lee IH, et al. Rate of vertical transmission of human papillomavirus from mothers to infants: relationship between infection rate and mode of delivery. Virol J. 2012;9:80.
Hermonat PL, Han L, Wendel P, Quirk JG, Stern S, Lowery C, et al. Human papillomavirus DNA is more prevalent in first trimester spontaneously aborted products of conception compared to elective specimens. Virus Genes. 1997;14(1):13–7. https://doi.org/10.1023/a:1007975005433.
Cho G, Min KJ, Hong HR, et al. High-risk human papillomavirus infection is associated with premature rupture of membranes. BMC Pregnancy Childbirth. 2013;13:173.
McDonnold M, Dunn H, Hester A, et al. High-risk human papillomavirus at entry to prenatal care and risk of preeclampsia. Am J Obstet Gynecol. 2014;210:138.
Kim YH, Park JS, Norwitz ER, Park JW, Kim SM, Lee SM, et al. Genotypic prevalence of human papillomavirus infection during normal pregnancy: a cross-sectional study. J Obstet Gynaecol Res. 2014;40(1):200–7. https://doi.org/10.1111/jog.12155.
Bruno MT, Cassaro N, Garofalo S, Boemi S. HPV16 persistent infection and recurrent disease after LEEP. Virol J. 2019;16(1):148. https://doi.org/10.1186/s12985-019-1252-3.
Caruso S, Bruno MT, Cianci S, Minona P, Cianci A. Sexual behavior of women with diagnosed HPV. J Sex Marital Ther. 2019;45(7):569–73. https://doi.org/10.1080/0092623X.2019.1586019.
Acknowledgments
We wish to thank the Scientific Bureau of the University of Catania for language support.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Contributions
MTB designed the study; GA and SB collected the data; MTB and SC drafted the manuscript; FB compiled the statistical data. All authors were involved in editing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study were in accordance with the institutional ethical standards and the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was approved by the ethic Committee of Catania Policlinic (n. 154/2019/PO).
Consent for publication
This study does not contain any individual person’s data.
Competing interests
The authors declared that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bruno, M.T., Caruso, S., Bica, F. et al. Evidence for HPV DNA in the placenta of women who resorted to elective abortion. BMC Pregnancy Childbirth 21, 485 (2021). https://doi.org/10.1186/s12884-021-03937-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-021-03937-9