Abstract
Background
The burden of maternal and neonatal morbidity and mortality is a global health concern with the highest burden documented after childbirth in women and babies living in sub-Saharan Africa. To date, there is limited information on the quality of postnatal care and/or whether evidence-based interventions to improve postnatal care in a way that meets the specific health needs of each mother and her baby have been lacking. There is also limited data related to how quality of care (respectful or disrespectful) influences women's decision to access postnatal care.
Objective
To systematically review available qualitative evidence for how quality of care (respectful or disrespectful) influences perceptions and experiences of, and decisions to, access postnatal care for women living in sub-Saharan Africa.
Search strategy
CINAHL plus, Cochrane library, Global Health, Medline, PubMed, Web of Science were searched from 2009—2019. Grey literature was searched on Google Scholar.
Selection criteria
Qualitative literature in English describing women’s perceptions and experiences of the quality of care they received after childbirth and how this influenced their perceptions of and decisions to access postnatal care.
Data analysis
Thematic analysis was performed to extract subthemes and themes. Outcomes were themes from the qualitative data used to form a thematic synthesis.
Results
Fifteen studies were included with data from 985 women interviewed face-to-face across eight countries. Descriptions of respectful care included healthcare providers being kind, supportive and attentive to women’s needs. Women described preferring healthcare services where the healthcare providers communicated in a respectful and caring manner. Descriptions of disrespectful care included verbal and/or physical abuse and power imbalances between women and healthcare providers. Some women were denied postnatal care when attending a healthcare facility after giving birth at home. There is evidence to suggest that vulnerable women (adolescents; women with poor socioeconomic status; women who are HIV positive) are more likely to receive disrespectful care.
Conclusions
This systematic review describes how aspects of respectful and disrespectful maternity care influence women’s perceptions and experiences of, and decisions to access postnatal care services. There is a need for a renewed focus to prioritise respectful maternity care and to sustainably provide good quality postnatal care to all women and their babies in a way that meets their expectations and health needs.
Similar content being viewed by others
Tweetable abstract
Adolescent age, poor socioeconomic status, positive HIV status and power imbalances contribute to disrespectful maternity care and act as barriers for women to access postnatal care in sub-Saharan Africa.
Introduction
The current international aim is to ensure universal access to maternal and newborn health care so that every woman has an equal chance to ‘survive and thrive’ during and after pregnancy [1]. However, this is not the case for many women living in sub-Saharan Africa, where the rates of maternal and neonatal mortality are the highest in the world. An estimated 201, 000 women die every year in sub-Saharan Africa as a result of pregnancy and childbirth, accounting for 66% of the global maternal mortality [2]. Additionally, more than 1 million neonatal deaths occur in sub-Saharan Africa each year, with a baby born in sub-Saharan Africa ten times more likely to die in the first month than a baby born in a high-income country [3, 4].
The majority of maternal health intervention programmes across sub-Saharan Africa have focussed on improving coverage of skilled birth attendance and emergency obstetric and newborn care with the aim to reduce the global burden of maternal deaths, stillbirths and early neonatal deaths, ‘the triple return’ [1]. However, to date, there has been a lack of focus on interventions and programmes that seek to provide comprehensive and individualised care for women and their babies after childbirth. Over half of maternal deaths and the majority of neonatal deaths occur during the first week after childbirth, highlighting that early and good quality postnatal care is crucial to prevent maternal and neonatal mortality worldwide [5, 6]. Postnatal care involves several components of care which both assess the health of the mother and newborn as well as educate the new mother on caring for herself and her child. These evidence-based recommendations are outlined in Table 1.
It is estimated that for every maternal death, 20 to 30 women suffer an acute or chronic morbidity related to pregnancy and/or childbirth [7]. Early detection of ill-health after childbirth as part of routine postnatal care allows for prompt treatment in order to prevent long term maternal and newborn morbidity [8]. Furthermore, good quality postnatal care ensures that newborn vaccinations are completed [9, 10], that women have access to reliable contraception [11, 12], and that women who are HIV positive are supported with measures to prevent mother-to-child transmission of HIV [13].
WHO recommends that all mothers and newborns receive postnatal care within 24 h of childbirth regardless of where the birth takes place, and at least three further postnatal care contacts [14]. However, sub-Saharan Africa has the lowest coverage across all interventions in the reproductive, maternal, newborn and child health continuum of care, with the highest dropout rates reported between skilled birth attendance and postnatal care [14,15,16,17]. The increasing recognition of the importance of postnatal care highlights a need for increased coverage [18] but there is concern that the quality of postnatal care must be addressed and prioritised in policy before coverage is increased [19, 20].
The issue of disrespect and abuse during pregnancy and childbirth in sub-Saharan Africa is well documented [21,22,23], with recognition that disrespect and abuse negatively influence women’s perceptions and experiences of care and that this reduces the likelihood of women delivering at the same facility for future pregnancies [24]. In response to this, the Respectful Maternity Care Charter was published, which outlined the universal rights of childbearing women [25]. The Respectful Maternity Care Charter was updated in 2018 to clearly articulate the rights of the women and newborn during maternity care [26]. The updated charter reflects Agenda 2030 and is directly linked to Sustainable Development Goal 3: ‘Ensure healthy lives and promote well-being for all at all ages’ [27].
Understanding women’s perception of care and experiences of services is important, as perceived quality is an important determinant of service utilization [28]. Women play a central role in assessing and defining quality of care as they choose to access care based on their opinions, and previous experiences with maternal health services [29]. The use of services and outcomes are the result not only of the provision of care but also of women’s experience of that care [30].
There is a need to explore women’s perceptions and experiences to help understand why women stop accessing care soon after childbirth (including cultural and social aspects of care) [31]. Understanding what women consider respectful and disrespectful care to be after childbirth will help to inform patient centred interventions to improve the experience and uptake of postnatal care.
Objective
To systematically review of qualitative literature for how quality of care (respectful or disrespectful) influences perceptions and experiences of, and decisions to access postnatal care for women living in sub-Saharan Africa.
Materials and methods
Data sources and search strategy
Relevant studies published from 1990 to 2019 were identified using a structured search strategy in five electronic databases: CINAHL Plus, PubMed, Global Health, Medline and Cochrane Library. The inclusion of articles published from 1990 to present day was used as this is the same time as the childbirth activism movement began and when studies started to be published on disrespectful care and abuse and respectful maternity care in maternal health [32]. A search strategy was developed using thesaurus (including MeSH) and free-text terms for “respectful maternity care” “disrespect and abuse” and “postnatal care” with associated keywords were used as main search terms (Supplementary table 1). In addition, the search strategy was applied to Google Scholar to explore grey literature. Reference lists and bibliographies of key studies were searched using Web of Science and any additional studies that met the inclusion criteria were obtained.
Inclusion and exclusion criteria
Studies were included if they described quality of care (respectful or disrespectful) and perceptions and experiences of postnatal care for women living in sub-Saharan Africa. Studies were excluded if: (i) they were conducted in high income countries; (ii) they reported on healthcare providers’ or mens’ perceptions; (iii) examined women’s perceptions of antenatal or intrapartum care only; (iv) used a quantitative study design only. The review was limited to studies from sub-Saharan Africa as defined by the World Bank. Language was limited to English.
Selection and data extraction
Two researchers independently screened all titles and abstracts. Evaluation of full-text studies was done independently by two researchers with reasons for exclusion recorded and any discrepancies were discussed with a third researcher.
Information was extracted into a pre-designed summary table and included data on: location of study, study dates, study design, study population, study subject, study outcomes (Supplementary table 2). Throughout the reviewing and extraction processes, studies where uncertainty existed were discussed by all researchers to reach a consensus.
Quality assessment
The quality of evidence for each study was assessed using the Critical Analysis Skills Programme (CASP) tool (Supplementary table 3) [33]. Studies were reviewed by authors individually. On mutual consensus studies where more than 50% of all
questions on the CASP Tool were satisfied were automatically included for synthesis. Studies that had less than 50% of questions satisfied were discussed and agreement made between the authors regarding inclusion in the final review. In this qualitative systematic review, papers were not excluded based on their quality, with the acknowledgement that the value of papers is often not recognised until the analysis stage [34].
Data synthesis
The RETREAT framework was used as a guide to select a synthesis method based on the selected studies and a thematic synthesis methodology was chosen [35]. The qualitative results presented in selected studies were coded line by line. This was undertaken in hard copy with codes highlighted manually by the primary researcher (CL). Codes were reviewed by a second researcher (KL) to ensure consistency and allow for discussion of reflexivity. Data that was relevant to the review objectives was extracted. Codes were sorted into higher order codes, subthemes and themes which were reviewed and agreed upon with the second and third researchers (KL, HMC).
Results
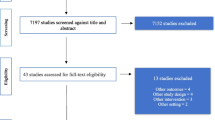
By combining the search terms, 5804 studies were identified and after screening for relevance, 129 were retrieved for full text review (Fig. 1). Upon applying the eligibility criteria, 15 studies met the inclusion criteria. The most common reasons for exclusion were there was no data related to quality of care in the study, antenatal or intrapartum data reported only and the study method was quantitative.
Characteristics of studies included
Geographical spread
Fifteen studies were from eight different countries across sub-Saharan Africa.
Uganda and Zambia had three studies conducted in each country (includes one study conducted in both Uganda and Zambia); Tanzania and Malawi had two studies conducted in each country; and Kenya, Zimbabwe and Ethiopia had one study conducted in each country.
Study design, source of data and data collection method
All 15 studies used face-to-face interviews or consultations to collect self-reported primary data from women. Semi-structured interviews, key informant in-depth interviews and focus group discussions were used for data collection. One study supplemented interviews with clinical observation [36]. Eight of the 15 studies assessed women after childbirth only and seven studies explored women’s views on postnatal care as part of the continuum of maternal care. Thematic analysis was used in all but two of the studies [37, 38] both of which used a thematic framework analysis. Although different methodologies, both analysis methods are descriptive in nature making the combining of results feasible.
Study population
985 women were interviewed across the 15 included studies. Seven of the 15 studies included the perceptions of healthcare providers and male participants in addition to women’s own perceptions and experiences. For these studies, only data from women who had given birth were extracted.
Setting and site of data collection
Two studies were conducted in urban settings [37, 39]; nine in rural settings [36, 38, 40,41,42,43,44,45,46]; and four studies were in both urban and rural settings [47,48,49,50]. Interviews were conducted with women in a variety of settings: their homes [40, 49], community centre [40], 'private locations' [41, 43, 47, 48, 50], rural healthcare centre [36], village based informant’s house [42], maternity unit at hospital [37], research site [49], at the bedside in the postnatal ward [49] and in some studies the interview site was unclear [38, 39, 41, 44, 46].
Qualitative results
The themes identified are summarised across two areas 1) respectful 2) disrespectful care and by sub-themes. The subthemes related to respectful care are; positive experiences of respectful care, women-centred care, respectful and kind healthcare providers providing care, care where women’s needs are prioritised, and informed choice. The subthemes identified regarding disrespectful care are: stigma and discrimination, non-dignified or disrespectful care, physical abuses and denial of care. Content quotes are provided in Tables 2 and 3.
Respectful care
In many studies women valued respectful care and expressed a desire to be treated with respect and kindness by healthcare providers [36, 37, 39, 42, 48, 49]. In several studies, being respectful was identified as the most important attribute for a healthcare provider to have [36, 42]. Women explained that they valued how they were treated by the healthcare providers more than the level of clinical experience that the healthcare providers had [37, 48].
Women described respectful care after childbirth as when healthcare providers displayed a positive attitude towards them [41, 45] and were attentive and sensitive to their needs [40, 45]. Women valued information and education as part of postnatal care [37, 44, 48, 49]. Women wanted to be able to make informed decisions about their care after childbirth [37] and they expected healthcare providers to give them all the necessary information to be able to do so [42, 45]. Women valued the healthcare providers’ opinion and trusted their judgement [42].
Disrespectful care
Across the included studies generally more examples of disrespectful care than respectful care was provided.
Verbal and/or physical abuse
Interactions with healthcare providers influenced women’s decisions to use postnatal care; with some women choosing not to access postnatal care due to fear of mistreatment from healthcare providers, including physical and verbal abuse [39, 43, 45,46,47]. Although some of these fears had originated from the accounts of other women, most women feared healthcare providers due to previous experiences they themselves had encountered throughout their antenatal or labour care [45, 47, 50]. Some women described that they were shouted at by the healthcare providers in front of other mothers at the clinic, which caused them to feel humiliated.
Healthcare providers’ negative attitudes
Women described experiences of disrespectful care with healthcare providers who had negative attitudes, describing them as unfriendly and in some cases threatening [36, 42, 43, 49]. Negative attitudes from healthcare providers resulted in women being too afraid to ask questions, finding healthcare providers ‘unapproachable’ and fearing their response [36, 39]. By avoiding asking questions some women did not have access to enough information to be able to properly consent to treatment [36].
Some women reported not understanding the importance of postnatal care due to a lack of information from healthcare providers [36, 42]. This meant that women were unsure of the postnatal care programme when questioned about it.
This lack of education about the importance of postnatal care was reflected in women’s knowledge of postnatal care, with women not understanding the need to attend postnatal care if both her and her child were well [38, 43, 45, 49]. Some of these women had been told by healthcare providers not to come back unless they had a medical problem after delivery.
The power imbalance between healthcare providers and women was highlighted in four studies [36,37,38, 45], with many women describing how the healthcare providers made decisions on their behalf and that women feared that they would not receive care if they did not allow the healthcare providers to make these decisions for them. Some women felt that they would be perceived as ‘insulting’ the authority of the healthcare providers if they asked questions [38].
Some women described experiencing an ‘uncomfortable environment’ during childbirth and this discouraged them from coming back to a healthcare facility for postnatal care services [36, 38]. Women described being encouraged to leave the facility straight after birth by healthcare providers which they perceived as being due to the lack of beds and adequate space for them to remain for at least the recommended minimum of 24 h after birth [38]. Some women accepted disrespectful care as ‘normal’ or justified it due to the stressful job of the midwife [36].
Stigma and discrimination
Examples of stigma and discrimination were reported by women in the majority (12/15) of studies. This included discrimination due to age, socio-economic status, positive HIV status.
Adolescent mothers described how healthcare providers would belittle them in front of other healthcare providers [49], and how they would not properly explain things in a way that would enable them to make informed choices [36]. This resulted in young women keeping their pregnancies and births secret and not accessing postnatal care for themselves or their babies [40]. Women reported stigma related to a woman’s nationality [50] and socioeconomic status, with women ensuring they appeared ‘well-groomed’ for postnatal clinic appointments to avoid stigma [36].
Women who were HIV positive reported discrimination from healthcare providers due to their HIV status describing verbal abuse [39, 50] and being humiliated in front of other mothers in the postnatal clinic [50]. Additionally, women living with HIV felt that they were treated differently by healthcare providers in a negative way during their postnatal appointments, compared to women who were not HIV positive [46]. Women who experienced this discrimination described not wanting to attend postnatal appointments due to the stigma they faced [39, 50]. In the included studies there were multiple examples of women explaining that they would access more care if they were treated better by the healthcare providers [36, 37, 39, 40, 42, 48, 49].
Denial of care
Women described being denied postnatal care either in the healthcare facilities or at home in five of the included 15 studies [38, 40, 42, 45, 47]. Women reported being told to leave the healthcare facility after birth by healthcare providers before the recommended 24 h, despite some women wanting to stay for longer [38, 42].
Women were also refused postnatal care after a home delivery, as a punishment for not delivering in the facility [40, 45]. Women described being chastised by healthcare providers for having had a planned home birth. Women reported that healthcare providers would not attend home visits for these women and when they attempted to access the facility for postnatal care they were turned away and denied medication, being told that they were a lower priority to women who had delivered in the facility [40, 43, 45, 47].
Women were also denied care unless they paid unofficial ‘under the table’ fees to healthcare providers [45, 47]. These unofficial payments were requested from women who had delivered at home; with women turned away due to their inability to pay for health cards or examinations which would normally be provided free of charge.
Discussion
Main findings
This systematic review explores the perceptions and experiences of 985 women living in sub-Saharan Africa and illustrates that women have a clear understanding of what respectful care looks like—describing this as healthcare providers being kind, attentive to women’s needs, and supportive. When women received respectful care, they had a positive perception and experience of postnatal care and reported being more likely to access care for subsequent health needs in settings where healthcare providers communicated in an empathic and caring manner.
Women reported power imbalances between themselves and the healthcare providers responsible for their care. Women described feeling afraid of healthcare providers due to previous experiences of physical and/or verbal abuse and described disrespectful care such as being denied postnatal care if they had delivered their baby at home. Some women felt that they had no choice but to follow the demands of healthcare providers or face denial of care. Studies document that vulnerable women (adolescents; women with poor socioeconomic status; women who are HIV positive) are more likely to report having received and experienced disrespectful care from healthcare providers.
Strengths and limitations
To the best of our knowledge, this is the one of the first systematic reviews to summarise the evidence that reports women’s perceptions and experiences of respectful and disrespectful maternity care after childbirth and how this influences women’s perceptions of and decision to access postnatal care across sub-Saharan African countries. By using a comprehensive search strategy, we captured descriptions of women’s perceptions of postnatal care within current literature. There were common themes and subthemes reported by women in many of the studies suggesting women’s experiences are similar across different contexts and countries. Few studies explored what respectful care looks like in the specific contexts especially with regard to cultural and societal expectations of women with newborn babies, highlighting the need to prioritise women’s needs and voices in future research. None of the studies included women who have suffered a stillbirth.
Interpretation
Data surrounding women’s perceptions and experiences of and decisions to access postnatal care to date are limited in sub-Saharan African countries, which confirm the need for a new approach and focus. A review of studies illustrates that women value respectful care as a priority when making decisions about accessing postnatal care. Similar findings have been described in studies exploring care during pregnancy and childbirth [28, 51, 52]. Being treated with respect, receiving support and good communication from healthcare providers are all valued by women during pregnancy and childbirth, and are predictors of women’s satisfaction with maternal health services [28, 51, 52].
Disrespectful care during childbirth has been well documented [53] and is a known barrier to women choosing to give birth in healthcare facilities [54]. However, there is less evidence about the significance of disrespect and abuse in the postnatal period. We found that women’s negative experiences during antenatal care and childbirth, or during postnatal care in previous pregnancies, prevented them from seeking postnatal care.
Stigma and discrimination were underlying issues across the themes. Stigma attached to women who chose to have a home birth may be due to the current international agenda recommending that all women give birth with a skilled birth attendant at healthcare facilities [27, 55]. Several African countries have made this mandatory and some healthcare facilities have introduced unofficial financial penalties if women do not access care at time of birth in a healthcare facility. Global health initiatives which focus on the quantity of facility deliveries, often associated with funding, put pressure on local health implementers and can create unhealthy incentives such as sanctioning women for delivering at home with fines [56]. This in turn can prevent women accessing postnatal care due to fear of healthcare providers and not being able to afford unofficial sanctions, unintentionally widening inequity and impacting the quality of care [57].
Denial of care is well documented as an abuse of women during childbirth, but there is limited literature on the denial of postnatal care across sub-Saharan African countries. In our systematic review, women were apprehensive about seeking postnatal care if they had delivered at home through fear of the negative reactions from healthcare providers and being denied care. This may play a significant role in women’s negative perceptions of postnatal care.
In our systematic review adolescent mothers describe that healthcare providers did not respond to their needs and that they felt judged. The treatment of pregnant adolescents in sub-Saharan Africa is recognised as an issue, with adolescents facing more challenges during their pregnancy due to community stigma and violence, meaning this group is less likely to seek care [58]. As a consequence, adolescent mothers have a higher risk for pregnancy complications [59]. It is recommended that healthcare services are adolescent friendly in order to provide equitable care for adolescents [60].
Women’s experience of discrimination due to their HIV status negatively influenced their perception of postnatal care and discouraged utilisation. Pregnant and postpartum women are a vulnerable group in relation to HIV stigma, as they are often the first in their families to be tested for HIV they can be seen as the person with whom the disease originates [61]. Additionally, with the integration of HIV and maternal health services, seeking care can be associated with unwanted disclosure and stigma [61]. The stigma and discrimination faced by women has been shown to have a negative impact on all stages of the ‘Prevention of Mother to Child Transmission of HIV’ cascade and has a significant effect on service uptake and adherence [61]. Further assessment of HIV related stigma during postnatal care is needed in order to inform ‘Prevention of Mother to Child Transmission of HIV’ programmes in sub-Saharan Africa.
Disrespectful care creates fear of healthcare providers and leads to power imbalances between women and healthcare providers. In our review, women felt that they had no choice but to follow the demands of healthcare providers or face denial of care. There have been many theoretical discussions about the driving forces behind disrespectful care and how power dynamics play their part in disrespect and abuse. These studies propose that if there is a background of organisational issues and disempowering environments, midwives attempt to exert power over women in an attempt to secure their own status in a hierarchical workplace [62,63,64].
Conclusion
Few studies to date have focussed on women’s perceptions and experiences of care after childbirth, and the results of this systematic review provide ample evidence and examples for the urgent need to address aspects of care that are disrespectful and that are likely to contribute significantly to the current low uptake of postnatal care across sub-Saharan Africa.
With a refocus from coverage to quality of care during pregnancy and childbirth, this review highlights the need for respectful care for women after childbirth also. We recommend that all postnatal care interventions implement respectful care principles from the design stage and comprehensive and routine auditing of respectful care standards during postnatal care is introduced to inform policy and program decisions and for resource allocation for postnatal care.
Availability of data and materials
All the sources of data are publicly available and referenced in the document. The datasets analysed during the current study are available in the CINAHL Plus [https://www.ebsco.com/products/research-databases/cinahl-plus], PubMed [https://pubmed.ncbi.nlm.nih.gov/], Global Health [https://www.ebsco.com/products/research-databases/global-health], Medline [https://www.nlm.nih.gov/medline/index.html] and Cochrane Library [https://www.cochranelibrary.com/] repository.
Abbreviations
- CASP:
-
Critical Analysis Skills Programme
- GRADE:
-
Grading of Recommendations, Assessment, Development and Evaluation
- LMIC:
-
Low- and middle-income countries
- MeSH:
-
Medical Subject Headings
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RETREAT:
-
Review question, Epistemology, Time/Timescale, Resources, Expertise, Audience and purpose, Type of Data
- WHO:
-
World Health Organization
References
United Nations. The global strategy for women’s, children’s and adolescents’ health (2016–2030). 2015.
Trends in maternal mortality: 1990 to 2015 report: The World Bank Group. https://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2015/en/. Accessed Sept 2020.
UN Inter-agency Group for Child Mortality Estimation. Levels & trends in child mortality report 2020. 2020.
World Health Organization. Newborns: improving survival and well-being 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality. Accessed Sept 2020.
World Health Organization. Newborns: reducing mortality 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality. Accessed Sept 2020.
The Partnership for Maternal Newborn and Child Health. Opportunities for Africa’s newborns: practical data, policy and programmatic support for newborn care in Africa. 2006.
Firoz T, Chou D, von Dadelszen P, Agrawal P, Vanderkruik R, Tunçalp O, et al. Measuring maternal health: focus on maternal morbidity. Bull World Health Organ. 2013;91(10):794–6.
Zainur RZ, Loh KY. Postpartum morbidity–what we can do. Med J Malaysia. 2006;61(5):651–6.
Asfaw AG, Koye DN, Demssie AF, Zeleke EG, Gelaw YA. Determinants of default to fully completion of immunization among children aged 12 to 23 months in south Ethiopia: unmatched case-control study. Pan Afr Med J. 2016;23:100.
Canavan ME, Sipsma HL, Kassie GM, Bradley EH. Correlates of complete childhood vaccination in East African countries. 2014.
Abraha TH, Teferra AS, Gelagay AA. Postpartum modern contraceptive use in northern Ethiopia: prevalence and associated factors. Epidemiol Health. 2017;39:e2017012.
Ajayi AI, Adeniyi OV, Akpan W. Maternal health care visits as predictors of contraceptive use among childbearing women in a medically underserved state in Nigeria. J Health Popul Nutr. 2018;37(1):19.
UNAIDS. Start free stay free AIDS free - 2017 progress report. Start free stay free AIDS free - 2017 progress report. Geneva: UNAIDS; 2018. p. 81.
World Health Organization. WHO recommendations on Postnatal care of the mother and newborn. 2013.
Abel Ntambue ML, Francoise Malonga K, Dramaix-Wilmet M, Donnen P. Determinants of maternal health services utilization in urban settings of the Democratic Republic of Congo–a case study of Lubumbashi City. BMC Pregnancy Childbirth. 2012;12:66.
Akinyemi JO, Afolabi RF, Awolude OA. Patterns and determinants of dropout from maternity care continuum in Nigeria. BMC Pregnancy Childbirth. 2016;16(1):282.
Creanga AA, Odhiambo GA, Odera B, Odhiambo FO, Desai M, Goodwin M, et al. Pregnant women’s intentions and subsequent behaviors regarding maternal and neonatal service utilization: results from a cohort study in Nyanza province, Kenya. PLoSONE. 2016.
Kikuchi K, Yasuoka J, Nanishi K, Ahmed A, Nohara Y, Nishikitani M, et al. Postnatal care could be the key to improving the continuum of care in maternal and child health in Ratanakiri, Cambodia. PLoS One. 2018;13(6):e0198829.
Fogel N. The inadequacies in postnatal health care. Curr Med Res Pract. 2017;7(1):16.
Sacks E, Langlois ÉV. Postnatal care: increasing coverage, equity, and quality. Lancet Glob Health. 2016;7:e442.
Abuya T, Warren CE, Miller N, Njuki R, Ndwiga C, Maranga A, et al. Exploring the prevalence of disrespect and abuse during childbirth in Kenya. PLoS One. 2015;10(4):e0123606.
Zemenu Yohannes K, Siraj H. Disrespectful and abusive behavior during childbirth and maternity care in Ethiopia: a systematic review and meta-analysis. BMC Res Notes. 2019;1:1.
Bradley S, McCourt C, Rayment J, Parmar D. Disrespectful intrapartum care during facility-based delivery in sub-Saharan Africa: a qualitative systematic review and thematic synthesis of women’s perceptions and experiences. 2016. p. 157–70.
Kujawski S, Mbaruku G, Freedman L, Ramsey K, Moyo W, Kruk M. Association between disrespect and abuse during childbirth and women’s confidence in health facilities in Tanzania. Matern Child Health J. 2015;19(10):2243–50.
The White Ribbon Alliance. Respectful maternity care: the universal rights of childbearing women. 2011.
The White Ribbon Alliance. Respectful maternity care: the universal rights of women and newborns. 2018.
United Nations Development Programme. Sustainable development goals 2019. Available from: http://www.undp.org/content/undp/en/home/sustainable-development-goals.html.
Srivastava A, Avan BI, Rajbangshi P, Bhattacharyya S. Determinants of women’s satisfaction with maternal health care: a review of literature from developing countries. 2015.
Gamedze-Mshayisa DI, Kuo SC, Liu CY, Lu YY. Factors associated with women’s perception of and satisfaction with quality of intrapartum care practices in Swaziland. Midwifery. 2018;57:32–8.
Larson E, Hermosilla S, Kimweri A, Mbaruku GM, Kruk ME. Determinants of perceived quality of obstetric care in rural Tanzania: a cross-sectional study. BMC Health Serv Res. 2014;14:483–483.
Fekadu GA, Kassa GM, Berhe AK, Muche AA, Katiso NA. The effect of antenatal care on use of institutional delivery service and postnatal care in Ethiopia: a systematic review and meta-analysis. BMC Health Serv Res. 2018;18(1):577.
Morton CH, Simkin P. Can respectful maternity care save and improve lives? Birth (Berkeley, Calif.). 2019. https://doi.org/10.1111/birt.12444.
Critical Appraisal Skills Programme. CASP checklist 2018. Available from: https://casp-uk.net/casp-tools-checklists/. Accessed Sept 2020.
Hannes K. Chapter 4: Critical appraisal of qualitative research. In: Noyes J, Booth A, Hannes K, Harden A, Harris J, Lewin S, Lockwood C (editors), Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. Version 1 (updated August 2011). Cochrane Collaboration Qualitative Methods Group, 2011. Available from URL http://cqrmg.cochrane.org/supplemental-handbook-guidance. Accessed Sept 2020.
Booth A, Noyes J, Flemming K, Gerhardus A, Wahlster P, van der Wilt GJ, et al. Structured methodology review identified seven (RETREAT) criteria for selecting qualitative evidence synthesis approaches. J Clin Epidemiol. 2018;99:41–52.
Kanengoni B, Andajani-Sutjahjo S, Holroyd E. Women’s experiences of disrespectful and abusive maternal health care in a low resource rural setting in eastern Zimbabwe. Midwifery. 2019;76:125–31.
Jolly Y, Aminu M, Mgawadere F, van den Broek N. “We are the ones who should make the decision” - knowledge and understanding of the rights-based approach to maternity care among women and healthcare providers. BMC Pregnancy Childbirth. 2019;19(1):42.
McMahon SA, Mohan D, LeFevre AE, Mosha I, Mpembeni R, Chase RP, et al. “You should go so that others can come”; the role of facilities in determining an early departure after childbirth in Morogoro region, Tanzania. BMC Pregnancy Childbirth. 2015;15:1–9.
Clouse K, Motlhatlhedi M, Bonnet K, Schlundt D, Aronoff DM, Chakkalakal R, et al. “I just wish that everything is in one place”: facilitators and barriers to continuity of care among HIV-positive, postpartum women with a non-communicable disease in South Africa. AIDS Care. 2018;30(sup2):5–10.
Amare Y, Scheelbeek P, Schellenberg J, Berhanu D, Hill Z. Early postnatal home visits: a qualitative study of barriers and facilitators to achieving high coverage. BMC Public Health. 2018;18(1):1074.
Sacks E, Moss WJ, Winch PJ, Thuma P, van Dijk JH, Mullany LC. Postnatal care utilization and local understandings of contagion among HIV-infected and uninfected women in rural, southern Zambia. AIDS Care. 2016;28(8):1052–7.
Mrisho M, Obrist B, Schellenberg JA, Haws RA, Mushi AK, Mshinda H, et al. The use of antenatal and postnatal care: perspectives and experiences of women and health care providers in rural southern Tanzania. BMC Pregnancy Childbirth. 2009;9:10.
Nabukera SK, Witte K, Muchunguzi C, Bajunirwe F, Batwala VK, Mulogo EM, et al. Use of postpartum health services in rural Uganda: knowledge, attitudes and barriers. J Community Health. 2006;31(2):84–93.
Zamawe CF, Masache GC, Dube AN. The role of the parents’ perception of the postpartum period and knowledge of maternal mortality in uptake of postnatal care: a qualitative exploration in Malawi. Int J Womens Health. 2015;7:587–94.
Sacks E, Masvawure TB, Atuyambe LM, Neema S, Macwan’gi M, Simbaya J, et al. Postnatal care experiences and barriers to care utilization for home- and facility-delivered newborns in Uganda and Zambia. Matern Child Health J. 2017;21(3):599–606.
Ashaba S, Kaida A, Coleman JN, Burns BF, Dunkley E, O’Neil K, et al. Psychosocial challenges facing women living with HIV during the perinatal period in rural Uganda. PLoS One. 2017;12(5):e0176256.
Sialubanje C, Massar K, Hamer DH, Ruiter RAC. Understanding the psychosocial and environmental factors and barriers affecting utilization of maternal healthcare services in Kalomo, Zambia: a qualitative study. Health Educ Res. 2014;29(3):521–32.
Colombini M, Mutemwa R, Kivunaga J, Stackpool Moore L, Mayhew SH. Experiences of stigma among women living with HIV attending sexual and reproductive health services in Kenya: a qualitative study. BMC Health Serv Res. 2014;14:412.
Duggan R, Adejumo O. Adolescent clients’ perceptions of maternity care in KwaZulu-Natal, South Africa. Women Birth. 2012;25(4):e62–7.
Clouse K, Schwartz S, Van Rie A, Bassett J, Yende N, Pettifor A. “What they wanted was to give birth; nothing else”: barriers to retention in option B+ HIV care among postpartum women in South Africa. J Acquir Immune Defic Syndr (1999). 2014;67(1):e12–8.
Mukamurigo JU, Berg M, Ntaganira J, Nyirazinyoye L, Dencker A. Associations between perceptions of care and women’s childbirth experience: a population-based cross-sectional study in Rwanda. BMC Pregnancy Childbirth. 2017;17(9 June):181.
Kabakian-Khasholian T, Campbell O, Shediac-Rizkallah M, Ghorayeb F. Women’s experiences of maternity care: satisfaction or passivity? Soc Sci Med. 2000;51(1):103–13.
Bohren MA, Hunter EC, Munthe-Kaas HM, Souza JP, Vogel JP, Guelmezoglu AM. Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis. 2014.
Idris SH, Sambo MN, Ibrahim MS. Barriers to utilisation of maternal health services in a semi-urban community in northern Nigeria: the clients’ perspective. Niger Med J. 2013;54(1):27–32.
United Nations. The millennium development goals report. 2015.
Greeson D, Sacks E, Masvawure TB, Austin-Evelyn K, Kruk ME, Macwan’gi M, et al. Local adaptations to a global health initiative: penalties for home births in Zambia. Health Policy Plan. 2016;31(9):1262–9.
World Health Organization. WHO | What is quality of care and why is it important? World Health Organization; 2017 [updated 2017–02–16] 11:24:31. Available from: https://www.who.int/maternal_child_adolescent/topics/quality-of-care/definition/en/.
Atuyambe L, Mirembe F, Tumwesigye NM, Annika J, Kirumira EK, Faxelid E. Adolescent and adult first time mothers’ health seeking practices during pregnancy and early motherhood in Wakiso district, central Uganda. Reprod Health. 2008;5:13.
World Health Organization. Adolescent pregnancy. 2019.
World Health Organization. Making health services adolescent friendly: developing national quality standards for adolescent friendly health services. 2012.
Turan JM, Nyblade L. HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: a review of the evidence. 2013. p. 2528–39.
Jewkes R, Abrahams N, Mvo Z. Why do nurses abuse patients? Reflections from South African obstetric services. Soc Sci Med. 1998;47(11):1781–95.
Bradley S, McCourt C, Rayment J, Parmar D. Midwives’ perspectives on (dis)respectful intrapartum care during facility-based delivery in sub-Saharan Africa: a qualitative systematic review and meta-synthesis. Reprod Health. 2019;1:1.
Bohren MA, Vogel JP, Tunçalp O, Fawole B, Titiloye MA, Olutayo AO, et al. “By slapping their laps, the patient will know that you truly care for her”: a qualitative study on social norms and acceptability of the mistreatment of women during childbirth in Abuja, Nigeria. SSM Popul Health. 2016;2:640–55.
Acknowledgements
Thank you to Isa Osage for assisting with initial screening of titles and abstracts.
Funding
This study was self-funded by Caitlin Lythgoe, as part of her dissertation of the Master’s in International Public Health programme at the Liverpool School of Tropical Medicine. MMc did not receive any funding for this work. Co-authors (KL and HMc) were funded by a grant from the Global Fund (20168770). The funders played no role in the writing of the manuscript or the decision to submit it for publication.
Author information
Authors and Affiliations
Contributions
CL, KL, HMc were responsible for the study inception and design and data interpretation. CL performed data extraction and wrote the manuscript. CL and KL performed the data analysis. MMc helped to interpret the data and wrote the manuscript. HMc supervised all research activities. All authors have read, critiqued and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This systematic review did not involve contact with any human participants, and therefore no ethical approval was needed. This study was conducted in compliance with the established ethical guidelines of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
MEsH terms. Supplementary Table 2. Summary of included studies. Supplementary Table 3. Critical Skills Appraisal Programme (2015) summary table.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lythgoe, C., Lowe, K., McCauley, M. et al. How women's experiences and perceptions of care influence uptake of postnatal care across sub-Saharan Africa: a qualitative systematic review. BMC Pregnancy Childbirth 21, 506 (2021). https://doi.org/10.1186/s12884-021-03910-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-021-03910-6