Abstract
Background
To better understand previous associations reported regarding nausea and vomiting in pregnancy (NVP) and pelvic girdle pain (PGP), an investigation into timing of symptom onset for NVP and PGP in pregnancy, as well as the association of NVP with PGP 4-6 months post-partum was performed. We hypothesised that women with NVP symptoms would be most susceptible to experiencing persistence of PGP post-partum.
Methods
Fifty two thousand six hundred seventy-eight pregnancies from the Norwegian Mother and Child Cohort Study were analysed regarding nausea, vomiting, pelvic girdle pain, and health outcome data collected from questionnaires answered between gestation weeks 15, 20, 30, and 6 months post-partum. Logistic regression was used.
Results
Women experiencing NVP and PGP together (6.9%) were heaviest in the sample, youngest at menarche and had highest proportion with education ≤12 years. The primiparous women in this group had the lowest timespan from menarche to pregnancy. Women with nausea alone (NP) and NVP had higher odds of PGP 4-6 months post-partum (adjusted odds ratio, aOR = 2.14, 95% CI 1.70–2.71, and aOR = 2.83, 95% CI 2.25–3.57, respectively), compared to symptom-free women. NP/NVP symptoms appeared early in the first trimester, while PGP symptoms appeared later in pregnancy. Women with longer durations of nausea and/or vomiting had a higher proportion of PGP compared to shorter duration women.
Conclusions
Women with NP and NVP had increased odds of PGP 4-6 months post-partum, and women with a long duration of nausea and/or vomiting had a higher proportion of PGP than women with shorter duration, both during pregnancy and 4-6 months post-partum. This finding suggests a synergistic relationship between NP/NVP and PGP.
Similar content being viewed by others
Background
Nausea alone (NP) or nausea and vomiting in pregnancy (NVP) affect approximately 80% of pregnancies [1,2,3]. Symptoms usually emerge early in the first trimester, around gestational weeks 5-6, peaking around week 9, and subsiding by approximately gestational week 12 or later [1, 4]. Women with a young age, previous deliveries, those overweight or obese, with an early menarche, with premenstrual symptoms, and non-smokers have been associated with symptoms of NP or NVP [5,6,7,8,9]. In addition, women who experienced symptoms in previous pregnancies seem more susceptible to NP or NVP in following pregnancies [10].
Pelvic girdle pain (PGP) is a pregnancy-related complication in which women have pain located between the posterior iliac crest and the gluteal fold, particularly close to the sacroiliac joints and the pubic symphysis [11]. The prevalence is estimated at 20% [11], however some researchers have reported higher prevalence values [12, 13]. The onset of symptoms occur from approximately week 6 of the pregnancy, and reach peak pain intensity between the 24th and 36th week of pregnancy [14, 15]. In previous studies, approximately 10% of women with PGP during pregnancy continued to experience pain up to 18 months after delivery [16, 17]. Known risk factors for PGP are smoking during pregnancy, a high BMI, young maternal age, previous pregnancies, and early menarche [18,19,20,21,22,23].
We recently reported that women with NP and NVP had increased odds for experiencing PGP compared with symptom-free (SF) women [24]. The NP/NVP and PGP conditions share similar risk factors, occur in the first trimester (particularly NP/NVP), and have unknown aetiologies. The current literature suggests that pregnancy hormones are one of the most likely causes of NVP, with human chorionic gonadotropin (hCG) as the main candidate, although estrogen, progesterone and relaxin have also been discussed [25]. Likewise, PGP aetiology has been linked previously to ovarian hormone levels, since these hormones may influence ligament laxity of the pelvic joints and lead to pain [11, 26]. As so little is understood about NP, NVP and PGP, an investigation of women with both of these conditions may reveal common traits that will provide a better understanding of their nature.
As we have already reported upon the association between NP/NVP and PGP during pregnancy, the aim of the present study was to focus upon women experiencing both NP/NVP and PGP during pregnancy, paying particular attention to the timing of onset for either condition, as well as to investigate PGP prevalence 4-6 months post-partum.
Methods
The Norwegian Mother and Child Cohort Study (MoBa)
MoBa is a prospective population-based pregnancy cohort study conducted by the Norwegian Institute of Public Health [27]. Participants were recruited from all over Norway from 1999 to 2008 and 40.6% of all women that were invited consented to participate. The cohort now includes 114,500 children, 95,200 mothers, and 75,200 fathers. Three questionnaires were answered during pregnancy, with follow-up questionnaires answered post-partum at regular intervals. Pregnancy and birth records from the Medical Birth Registry of Norway (MBRN) were linked to the MoBa cohort [28]. The quality-assured data files entitled ‘version 8’ were used. Response rates for the MoBa version 8 questionnaires can be found elsewhere [29, 30].
Questionnaires and variables
The data were primarily collected from four self-administered questionnaires (Q). The first one was answered in gestational week 15 (Q1), and the subsequent questionnaires were administered around week 20 (Q2), week 30 (Q3), and 6 months post-partum (Q4).
Q1 probed into details regarding maternal health and lifestyle, demographics, previous pregnancies, and early first trimester reports of NP, NVP, and PGP.
From Q1 we used maternal height (cm) and weight (kg) at the start of pregnancy to calculate body mass index (BMI, kg/m2), education (seven categories collapsed into: ≤12 years, 13–16 years, or ≥ 17 years), smoking during pregnancy (no, sometimes, or daily), age at menarche (years), incidences of irritability before menses (five categories collapsed into ‘yes/no’), number of previous pregnancies, previous experiences of NVP (yes or no), and experiences of NP, NVP, and PGP in the first 15 weeks of pregnancy (separated into 4 week intervals; yes or no). The incidences of irritability before menses were defined as having reported an alleviation of such symptoms after menses. Years from menarche to pregnancy were calculated by subtracting age at menarche (from Q1) from maternal age at time of birth (from MBRN). Due to obvious erroneous reporting, only values ≥5 years and < 35 years from menarche to current pregnancy were used. Likewise, ages at menarche < 7 years and > 25 years of age were considered to be erroneously reported.
Q2 included a food frequency questionnaire and was answered in mid-pregnancy. Version two of Q2 included detailed questions regarding nausea and vomiting, therefore only women answering this version were included in the sample. While the questions regarding NVP and PGP in Q1 were structured simply as ‘yes/no’ for the corresponding 4 week intervals in early first trimester, the NVP questions in Q2 probed experiences of nausea or vomiting during pregnancy (yes or no), the gestational week of onset and cessation, and whether women were still experiencing nausea and/or vomiting at the time of answering the questionnaire (around gestational week 20). These NP and NVP answers were cross-checked with answers provided in Q1 to avoid inconsistent responses, as detailed in the ‘Study Sample’ section below. Prior to calculating the duration of either nausea or vomiting from variables stating the gestational week of onset and the week of cessation of these conditions, recoding for some variables was required, as described in detail previously [5].
Data from Q3 (gestational week 30) enabled us to differentiate NVP women from women diagnosed with hyperemesis gravidarum (HG), defined as prolonged nausea and vomiting during pregnancy requiring hospitalisation before week 25 of gestation [31]. Q3 also provided comprehensive information regarding pain distribution and pain intensity (none/mild/severe) in the pelvic girdle during pregnancy. We defined PGP as self-reported pain in both the pubic symphysis in the anterior pelvis and bilaterally in the sacroiliac joints in the posterior pelvis (yes or no). Severe PGP (sPGP) was defined as having reported severe pain in all the above pain locations [21]. These conditions are referred to as PGP and sPGP, respectively. We also obtained responses regarding experiences of NP, NVP, and PGP from week 15 to week 29 or more of pregnancy (separated into 4 week intervals; yes or no). All ‘yes/no’ responses for NP, NVP, and PGP from Q1 and Q3 were cross-checked with identified cases based upon the more comprehensive definitions of NP, NVP, and PGP defined above.
We based the reporting of PGP or sPGP during the last part of pregnancy and/or 4-6 months post-partum upon questions in Q4 (six months post-partum) regarding pain in the anterior and bilateral posterior pelvis [32]. Women reporting PGP or sPGP during the last part of pregnancy were added to those women reporting PGP or sPGP in Q3, producing the total number of women reporting PGP or sPGP during pregnancy.
Data concerning maternal age at time of birth (year), parity (primiparous, multiparous), and gestational length (weeks) were obtained from the MBRN. Questions allowing only for an answer of ‘yes’ had non-answers recoded to ‘no’ or ‘none’ from MoBa and MBRN [24].
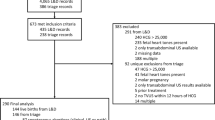
Study sample
The entire MoBa cohort includes 114,275 children and 95,200 mothers. The present sample comprises those women deemed eligible for inclusion, having satisfied criteria such as answering relevant questions related to the study in Q1 and version 2 of Q2, being registered in the MBRN with a singleton live birth, with complete weight and height data recorded, with a gestational length between 28 to 42 weeks, and with consistent reports regarding symptoms of NP and NVP throughout the first trimester. Furthermore, as some women participated in MoBa multiple times due to multiple pregnancies, only those women with one participation were included, or else only the first pregnancy if more than one was registered. Women with NP or NVP symptoms were only included if their condition did not develop into HG. A total of 52,678 women fulfilled all these criteria and were included in the study sample. These criteria were identical to those used in our previous studies [5, 24, 33].
Statistical analyses
The study sample was divided into three groups: symptom-free (SF), nausea alone (NP), and both nausea and vomiting (NVP). Furthermore, we categorised the women according to whether they were with or without all forms of PGP during pregnancy. Two variables were dichotomised according to the median value: nausea duration (< 8 or ≥ 8 weeks) and vomiting duration (< 7 or ≥ 7 weeks). Only women reporting either NP, NVP, or PGP both in the simple ‘yes/no’ questions as well as the more detailed definitions used for these conditions were included in the analyses regarding the reported week of onset.
Descriptive results are presented as means (standard deviations; SDs) or frequencies (%). Comparisons between women with or without PGP, stratified by condition (SF, NP and NVP), were performed by two sample t-test and chi-squared test. PGP and sPGP at 4-6 months post-partum were explored using logistic regression analysis. We present crude and adjusted odds ratios (cOR and aOR, respectively), with 95% confidence intervals (CI). We adjusted for maternal age, BMI, smoking during pregnancy, parity, education, age at menarche, and incidences of irritability before menses after reviewing previous literature regarding NP, NVP, and PGP. Additional adjustment for length of gestation, years from menarche to pregnancy, and use of hormonal contraceptives prior to pregnancy did not change the results, therefore these results are not reported.
A significance level of 0.05 was used except when we studied statistical interaction effects, where 0.01 was used to allow for multiple testing. All analyses were performed using SPSS 22.0 (IBM Corp, Armonk, NY, USA). We followed the guidelines in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (http://www.strobe-statement.org).
Results
Maternal and gestational history
Women with PGP tended to be heavier and with a higher pre-pregnancy BMI compared to those without PGP (Table 1), and the highest means were for NVP women with PGP. Age at menarche and the number of years from menarche to pregnancy were slightly lower for SF, NP, and NVP women with PGP as compared to women without PGP. SF, NP, and NVP women with PGP had the highest proportion with an education ≤12 years, the highest proportion of irritability before menses amongst those primiparous, and the highest proportion with previous experiences of NVP amongst those multiparous, compared to women without PGP.
When the total study sample was compared with women excluded from the sample, similar estimates were seen in regards to age, weight, BMI, and age at menarche, but among the excluded women a lower proportion were primiparous (48.4% vs 52.7%, found in supporting information Additional file 1), had ≤12 years of education (29.2% vs 30.5%), and a higher proportion were daily smokers (5.7 vs 5.1%).
Time of NP, NVP, and PGP symptom initiation
When we studied the timing of onset of total NP and NVP during the specific periods in pregnancy, we observed a sharp increase in early first trimester, with NP peaking in weeks 5-8 (31.9%) and NVP in weeks 9-12 (28.0%, Fig. 1). Thereafter, both conditions decreased steadily. By contrast, among the SF, NP and NVP women, the proportions of PGP increased gradually from 0.3, 1.2 and 1.5%, in weeks 0-4, respectively, to 8.5, 21.5 and 18.2%, respectively, in week 29 or over.
Duration of nausea and vomiting in relation to PGP
When comparing the occurrences of PGP and sPGP during pregnancy and 4-6 months post-partum with shorter or longer periods of nausea or vomiting, we observed consistently higher proportions of PGP and sPGP for women with longer durations of either nausea or vomiting (Fig. 2).
Association between NVP and PGP
Analysis of women with PGP and sPGP 4-6 months post-partum showed the NVP group having the highest proportion as compared to the NP and SF groups (Table 2).
Compared to SF women, NP and NVP women had significantly higher odds of PGP 4-6 months post-partum (aOR = 2.14, 95% CI 1.70-2.71, and aOR = 2.83, 95% CI 2.25–3.57, respectively). NVP women also had significantly higher odds of sPGP 4-6 months post-partum (aOR = 3.35, 95% CI 1.78-6.32) while non-significantly increased odds were found among NP women (aOR = 1.87, 95% CI 0.96-3.64).
Discussion
We found that women with both NVP and PGP were the heaviest, and had the highest proportion with an education ≤12 years. PGP with either NP or NVP appeared later in pregnancy compared to symptoms of NP or NVP only. Women with a longer duration of nausea or vomiting reported PGP and sPGP more frequently compared to women with a shorter duration. In multivariate analyses, women with NP and NVP had higher odds than SF women of experiencing PGP and sPGP at 4-6 months post-partum.
Women excluded from the study had similar age at delivery, weight, BMI, and ages at menarche. Furthermore, there was a lower proportion of primiparous women (4.3%) amongst the excluded, which is consistent with non-compliance reported elsewhere [34]. The higher proportions of daily smokers in the excluded group (0.6%) may be a result of the high number of missing values (23%). Furthermore, it has been presented elsewhere that although prevalence estimates such as smoking are under-represented in the MoBa cohort when compared with the general Norwegian population, the exposure-outcome associations are valid [35]. The deviation (1.3%) regarding maternal education may also be a reflection of the high number of missing cases in the excluded group (22%).
Gestational week 9-16 is the crossover period in which the proportions of NP and NVP decreased and the proportions of PGP increased amongst the women. As our data indicate that NP and NVP symptoms are more prevalent before PGP symptoms appear, and the proportion of women with PGP is higher for those having the longer duration of NP or NVP, it seems plausible to speculate that the presence of NP or NVP may exacerbate the occurrence of PGP.
NVP and PGP appear to have many risk factors in common. In this study we report that a prior pregnancy, high BMI, lower number of years from menarche to pregnancy, and incidences of irritability before menses, were all more present for the women experiencing NP and NVP with PGP.
Many of these risk factors may be attributable to hormonal mechanisms. A higher BMI has previously been shown to have a strong inverse association with the sex hormone-binding globulin and the total estrogen levels in the large prospective Nurses’ Health Study [36]. Additionally, numerous studies have suggested a hormonal aetiology in relation to NVP symptoms, yet no consensus has been achieved. Progesterone and estrogen/estradiol in high or low concentrations have been proposed previously [37,38,39], although others could not reproduce these findings [40, 41]. This situation is also the case for NVP’s most hypothesised causative hormone, hCG [38, 41,42,43].
It has previously been hypothesised that abnormal serum levels of relaxin during pregnancy increase the risk of PGP, although findings are inconsistent [44, 45]. Relaxin affects collagen synthesis during pregnancy, and together with progesterone, has been suggested to influence joint laxity in pregnant women [46]. In addition to relaxin, significantly higher levels of progesterone in early pregnancy have been suggested to play a role in the development of PGP [26]. The relationship between NVP and PGP identified in this study may be based on a synergistic effect of pregnancy hormones such as progesterone, estrogen and relaxin, although it remains speculative without access to early pregnancy biomarkers. Relaxin has apparently never been investigated clinically in relation to NVP symptoms, which is remarkable when one considers that both hCG and relaxin tend to peak in concentration at approximately the same time during early pregnancy [47, 48].
Our new results regarding PGP and sPGP 4-6 months post-partum strengthen our previous findings suggesting NP and NVP women have increased odds for pregnancy-related PGP [24]. One study of women experiencing PGP post-partum reported that pain was exacerbated by the onset of menstruation and/or ovulation [49], which further implies a hormonal contribution in PGP.
Strengths and limitations
The strengths of this study are the large sample from a population-based cohort and the linkage to the MBRN, providing detailed access to maternal health during pregnancy. The MoBa cohort specifically addressed NVP-related issues, providing the opportunity to differentiate between NP and NVP women [5, 24, 33]. Likewise, the detailed questions regarding PGP formed a basis for the robust definition of PGP used [21]. As this is a large cohort, numerous significant associations tend to appear, yet the merit of these in the clinical setting are not always relevant. Furthermore, the responses in the MoBa questionnaires do not allow for an easy assessment of the severity of NVP symptoms. Retrospective evaluation of NVP symptoms has previously been reported as a possible source of bias [50]. We attempted to address this by excluding cases with inconsistencies in NVP symptoms reported between questionnaires (n = 15,791) to have as much confidence as possible in the remaining study sample. When we performed sensitivity analyses with the excluded cases included in the sample, the results were mostly unaffected. Women excluded from the present study had similar ages at delivery, BMI and energy intake, while there tended to be more women with a lower education (29.2% vs 30.5%) as well as a higher parity (48.4% vs 52.7%), findings consistent with non-compliance present in other studies [34, 51, 52]. The slightly higher number of daily smokers in the excluded group (5.7% vs 5.1%) is most likely a product of the high number of missing values for this variable. Other weaknesses include the reliance on self-reports of PGP, nausea, and vomiting. The diagnosis of PGP in our study would have benefited from a clinical assessment, as has been suggested elsewhere [13], in order to support the women’s self-reports. However, this is not feasible in a large cohort study. Categorising the difference between retching and actual vomiting (defining NP and NVP) may also have led to misclassifications and affected the results. Another weakness is the lack of information on biomarkers (e.g. hormones).
Conclusions
We found that women with NP or NVP had higher odds of experiencing PGP or sPGP 4-6 months post-partum, compared to SF women. To our knowledge this is the first study examining elements of nausea and vomiting in relation to PGP post-partum. NP and NVP appeared earlier in pregnancy than PGP, and women with a longer duration of nausea and/or vomiting had a higher proportion of PGP compared to those women with a shorter duration of symptoms, suggesting a synergistic relationship between NP/NVP and PGP.
Our findings showing NP or NVP women with PGP representing a high proportion with irritability before menses and a lower number of years from menarche to first birth compared to those groups without PGP tend to support the hypothesis of a hormonal involvement in the underlying mechanisms of these disorders.
Abbreviations
- aOR:
-
Adjusted odds ratio
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- cOR:
-
Crude odds ratio
- hCG:
-
human chorionic gonadotropin
- HG:
-
Hyperemesis gravidarum
- MBRN:
-
Medical birth registry of Norway
- MoBa:
-
The Norwegian Mother and Child Cohort Study
- NP:
-
Nausea alone
- NVP:
-
Nausea and vomiting in pregnancy
- PGP:
-
Pelvic girdle pain
- Q1-4:
-
Questionnaire number
- SD:
-
Standard deviations
- SF:
-
Symptom-free
- sPGP:
-
severe pelvic girdle pain
References
Gadsby R, Barnie-Adshead AM, Jagger C. A prospective study of nausea and vomiting during pregnancy. Br J Gen Pract. 1993;43:245–8.
Sherman PW, Flaxman SM. Nausea and vomiting of pregnancy in an evolutionary perspective. Am J Obstet Gynecol. 2002;186(Suppl 5):S190–7.
Kallen B, Lundberg G, Aberg A. Relationship between vitamin use, smoking, and nausea and vomiting of pregnancy. Acta Obstet Gynecol Scand. 2003;82:916–20.
Lacroix R, Eason E, Melzack R. Nausea and vomiting during pregnancy: a prospective study of its frequency, intensity, and patterns of change. Am J Obstet Gynecol. 2000;182:931–7.
Chortatos A, Haugen M, Iversen PO, Vikanes A, Magnus P, Veierod MB. Nausea and vomiting in pregnancy: associations with maternal gestational diet and lifestyle factors in the Norwegian mother and child cohort study. BJOG. 2013;120:1642–53.
Chan RL, Olshan AF, Savitz DA, Herring AH, Daniels JL, Peterson HB, Martin SL. Maternal influences on nausea and vomiting in early pregnancy. Matern Child Health J. 2011;15:122–7.
Whitehead S, Andrews P, Chamberlain G. Characterisation of nausea and vomiting in early pregnancy: a survey of 1000 women. J Obstet Gynecol. 1992;12:364–9.
Han Y, Ha E, Park H, Kim Y, Lee S. Relationships between pregnancy outcomes, biochemical markers and pre-pregnancy body mass index. Int J Obes. 2011;35:570–7.
Temming L, Franco A, Istwan N, Rhea D, Desch C, Stanziano G, Joy S. Adverse pregnancy outcomes in women with nausea and vomiting of pregnancy. J Matern Fetal Neonatal Med. 2014;27:84–8.
Goodwin TM. Nausea and vomiting of pregnancy: an obstetric syndrome. Am J Obstet Gynecol. 2002;186(Suppl 5):S184–9.
Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J. 2008;17:794–819.
Mogren IM, Pohjanen AI. Low back pain and pelvic pain during pregnancy: prevalence and risk factors. Spine. 2005;30:983–91.
Robinson HS, Vøllestad NK, Veierød MB. Clinical course of pelvic girdle pain postpartum–impact of clinical findings in late pregnancy. Man Ther. 2014;19:190–6.
Wu WH, Meijer OG, Uegaki K, Mens JMA, van Dieen JH, Wuisman PIJM, Ostgaard HC. Pregnancy-related pelvic girdle pain (PPP), I: terminology, clinical presentation, and prevalence. Eur Spine J. 2004;13:575–89.
Kristiansson P, Svardsudd K, von Schoultz B. Back pain during pregnancy: a prospective study. Spine. 1996;21:702–9.
Röst CC, Jacqueline J, Kaiser A, Verhagen AP, Koes BW. Prognosis of women with pelvic pain during pregnancy: a long-term follow-up study. Acta Obstet Gynecol Scand. 2006;85:771–7.
Albert H, Godskesen M, Westergaard J. Prognosis in four syndromes of pregnancy-related pelvic pain. Acta Obstet Gynecol Scand. 2001;80:505–10.
Kovacs FM, Garcia E, Royuela A, Gonzalez L, Abraira V, Spanish Back Pain Research N, Seco Calvo J, Zamora Delmas L, Serra Calafat C, Montoliu E et al: Prevalence and factors associated with low back pain and pelvic girdle pain during pregnancy: a multicenter study conducted in the Spanish National Health Service. Spine 2012, 37:1516-1533.
Kirkeby MJ, Biering K, Olsen J, Juhl M, Nohr EA. Age at menarche and pregnancy-related pelvic pain. J Obstet Gynaecol Res. 2013;39:1037–44.
Bjelland EK, Eberhard-Gran M, Nielsen CS, Eskild A. Age at menarche and pelvic girdle syndrome in pregnancy: a population study of 74 973 women. BJOG. 2011;118:1646–52.
Bjelland EK, Eskild A, Johansen R, Eberhard-Gran M. Pelvic girdle pain in pregnancy: the impact of parity. Am J Obstet Gynecol. 2010;203:146.e141–6.
Biering K, Aagaard Nohr E, Olsen J, Hjollund N, Nybo Andersen AM, Juhl M. Smoking and pregnancy-related pelvic pain. BJOG. 2010;117:1019–26.
Juhl M, Andersen PK, Olsen J, Andersen A-MN. Psychosocial and physical work environment, and risk of pelvic pain in pregnancy. A study within the Danish national birth cohort. J Epidemiol Community Health. 2005;59:580–5.
Chortatos A, Haugen M, Iversen PO, Vikanes A, Eberhard-Gran M, Bjelland EK, Magnus P, Veierod MB. Pregnancy complications and birth outcomes among women experiencing nausea only or nausea and vomiting during pregnancy in the Norwegian mother and child cohort study. BMC Pregnancy Childbirth. 2015;15:167–77.
Koch KL, Frissora CL. Nausea and vomiting during pregnancy. Gastroenterol Clin N Am. 2003;32:201–34.
Kristiansson P, Svardsudd K, von Schoultz B. Reproductive hormones and aminoterminal propeptide of type III procollagen in serum as early markers of pelvic pain during late pregnancy. Am J Obstet Gynecol. 1999;180:128–34.
Magnus P, Birke C, Vejrup K, Haugan A, Alsaker E, Daltveit AK, Handal M, Haugen M, Høiseth G, Knudsen GP. Cohort profile update: the Norwegian mother and child cohort study (MoBa). Int J Epidemiol. 2016;45:382–8.
Irgens LM, et al. Acta Obstet Gynecol Scand. 2000;79:435–9.
Bjelland EK, Owe KM, Pingel R, Kristiansson P, Vangen S, Eberhard-Gran M. Pelvic pain after childbirth: a longitudinal population study. Pain. 2016;157:710–6.
Norwegian Institute of Public Health. MoBa research data files. [https://www.fhi.no/en/op/data-access-from-health-registries-health-studies-and-biobanks/data-from-moba/moba-research-data-files/]. Accessed 9 Oct 2017.
Haugen M, Vikanes A, Brantsaeter AL, Meltzer HM, Grjibovski AM, Magnus P. Diet before pregnancy and the risk of hyperemesis gravidarum. Brit J Nutr. 2011;106:596–602.
Bjelland E, Stuge B, Engdahl B, Eberhard-Gran M. The effect of emotional distress on persistent pelvic girdle pain after delivery: a longitudinal population study. BJOG. 2013;120:32–40.
Chortatos A, Haugen M, Iversen PO, Veierød MB. Dietary changes during first trimester pregnancy for women with nausea and vomiting in the Norwegian mother and child cohort study. Norw J Epidemiol. 2014;24:147–53.
Stacey T, Thompson J, Mitchell EA, Ekeroma AJ, Zuccollo JM, McCowan LM. The Auckland stillbirth study, a case–control study exploring modifiable risk factors for third trimester stillbirth: methods and rationale. Aust N Z J Obstet Gynaecol. 2011;51:3–8.
Nilsen RM, Vollset SE, Gjessing HK, Skjærven R, Melve KK, Schreuder P, Alsaker ER, Haug K, Daltveit AK, Magnus P. Self-selection and bias in a large prospective pregnancy cohort in Norway. Paediatr Perinat Epidemiol. 2009;23:597–608.
Tworoger SS, Eliassen AH, Missmer SA, Baer H, Rich-Edwards J, Michels KB, Barbieri RL, Dowsett M, Hankinson SE. Birthweight and body size throughout life in relation to sex hormones and prolactin concentrations in premenopausal women. Cancer Epidemiol Biomark Prev. 2006;15:2494–501.
Jarnfelt-Samsioe A, Bremme K, Eneroth P. Steroid-hormones in emetic and non-emetic pregnancy. Eur J Obstet Gyn R B. 1986;21:87–99.
Depue RH, Bernstein L, Ross RK, Judd HL, Henderson BE. Hyperemesis gravidarum in relation to estradiol levels, pregnancy outcome, and other maternal factors - a seroepidemiologic study. Am J Obstet Gynecol. 1987;156:1137–41.
Walsh JW, Hasler WL, Nugent CE, Owyang C. Progesterone and estrogen are potential mediators of gastric slow-wave dysrhythmias in nausea of pregnancy. Am J Physiol-Gastr L. 1996;270:G506–14.
Lagiou P, Tamimi R, Mucci LA, Trichopoulos D, Adami HO, Hsieh CC. Nausea and vomiting in pregnancy in relation to prolactin, estrogens, and progesterone: a prospective study. Obstet Gynecol. 2003;101:639–44.
Masson GM, Anthony F, Chau E. Serum chorionic gonadotrophin (hCG), schwangerschaftsprotein 1 (SP1), progesterone and oestradiol levels in patients with nausea and vomiting in early pregnancy. BJOG. 1985;92:211–5.
Soules MR, Hughes CL, Garcia JA, Livengood CH, Prystowsky MR, Alexander E. Nausea and vomiting of pregnancy - role of human chorionic-gonadotropin and 17-Hydroxyprogesterone. Obstet Gynecol. 1980;55:696–700.
Fairweather D, Loraine J. Urinary excretion of human chorionic gonadotrophin in patients with hyperemesis gravidarum. BMJ. 1962;1:666.
Kristiansson P, Svardsudd K, von Schoultz B. Serum relaxin, symphyseal pain, and back pain during pregnancy. Am J Obstet Gynecol. 1996;175:1342–7.
Aldabe D, Ribeiro DC, Milosavljevic S, Dawn Bussey M. Pregnancy-related pelvic girdle pain and its relationship with relaxin levels during pregnancy: a systematic review. Eur Spine J. 2012;21:1769–76.
Ireland ML, Ott SM. The effects of pregnancy on the musculoskeletal system. Clin Orthop Relat Res. 2000;372:169–79.
Bathgate RAD, Halls ML, van der Westhuizen ET, Callander GE, Kocan M, Summers RJ. Relaxin family peptides and their receptors. Physiol Rev. 2013;93:405–80.
Seki K, Uesato T, Tabei T, Kato K. The secretory patterns of relaxin and human chorionic gonadotropin in human pregnancy. Endocrinol Jpn. 1985;32:741–4.
Nielsen LL. Clinical findings, pain descriptions and physical complaints reported by women with post-natal pregnancy-related pelvic girdle pain. Acta Obstet Gynecol Scand. 2010;89:1187–91.
Koren G, Maltepe C, Navioz Y, Wolpin J. Recall bias of the symptoms of nausea and vomiting of pregnancy. Am J Obstet Gynecol. 2004;190:485–8.
Tough SC, Siever JE, Benzies K, Leew S, Johnston DW. Maternal well-being and its association to risk of developmental problems in children at school entry. BMC Pediatr. 2010;10:19.
Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17:643–53.
Acknowledgements
We are grateful to all the participating families in Norway who took part in this cohort study.
Funding
The Norwegian Mother and Child Cohort Study is supported by the Norwegian Ministry of Health and the Ministry of Education and Research, NIH/NIEHS (contract number N01-ES-75558), NIH/NINDS (grant number 1 UO1 NS 047537-01 and grant number 2 UO1 NS 047537-06A1).
Availability of data and materials
The authors are pleased to share the anonymized dataset upon receiving a reasonable request. Interested parties may contact the corresponding author.
Author information
Authors and Affiliations
Contributions
AC, POI, MH, MEG, EKB, and MBV designed the project; AC performed statistical analyses, drafted the manuscript and was responsible for the manuscript revisions; MH and MBV contributed to the statistical analyses; MH, POI, MEG, EKB, and MBV contributed to the interpretation of the data, results, and writing of the manuscript. All authors critically revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Regional Committee for Medical and Health Research Ethics in South-Eastern Norway Committee A (REC South East A, reference numbers S-97045 and S-95113) and the Norwegian Data Protection Authority. Written informed consent was obtained from all MoBa participants.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Selected maternal characteristics for women included and excluded from the study. (DOCX 19 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chortatos, A., Iversen, P.O., Haugen, M. et al. Nausea and vomiting in pregnancy – association with pelvic girdle pain during pregnancy and 4-6 months post-partum. BMC Pregnancy Childbirth 18, 137 (2018). https://doi.org/10.1186/s12884-018-1764-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-018-1764-7