Abstract
Background
Excessive gestational weight gain (GWG) is associated with adverse pregnancy outcomes. In non-pregnant populations, low leptin levels stimulate positive energy balance. In pregnancy, both the placenta and adipose tissue contribute to circulating leptin levels. We tested whether maternal leptin levels are associated with subsequent GWG and whether this association varies depending on stage of pregnancy and on maternal body mass index (BMI).
Methods
This prospective cohort study included 675 pregnant women followed from 1st trimester until delivery. We collected anthropometric measurements, blood samples at 1st and 2nd trimester, and clinical data until delivery. Maternal leptin was measured by ELISA (Luminex technology). We classified women by BMI measured at 1st trimester: BMI < 25 kg/m2 = normal weight; 25 ≤ BMI < 30 kg/m2 = overweight; and BMI ≥ 30 kg/m2 = obese.
Results
Women gained a mean of 6.7 ± 3.0 kg between 1st and 2nd trimester (mid pregnancy GWG) and 5.6 ± 2.5 kg between 2nd and the end of 3rd trimester (late pregnancy GWG). Higher 1st trimester leptin levels were associated with lower mid pregnancy GWG, but the association was no longer significant after adjusting for % body fat (%BF; β = 0.38 kg per log-leptin; SE = 0.52; P = 0.46). Higher 2nd trimester leptin levels were associated with greater late pregnancy GWG and this association remained significant after adjustment for BMI (β = 2.35; SE = 0.41; P < 0.0001) or %BF (β = 2.01; SE = 0.42; P < 0.0001). In BMI stratified analyses, higher 2nd trimester leptin levels were associated with greater late pregnancy GWG in normal weight women (β = 1.33; SE = 0.42; P = 0.002), and this association was stronger in overweight women (β = 2.85; SE = 0.94; P = 0.003 – P for interaction = 0.05).
Conclusions
Our results suggest that leptin may regulate weight gain differentially at 1st versus 2nd trimester of pregnancy: at 2nd trimester, higher leptin levels were associated with greater subsequent weight gain – the opposite of its physiologic regulation in non-pregnancy – and this association was stronger in overweight women. We suspect the existence of a feed-forward signal from leptin in second half of pregnancy, stimulating a positive energy balance and leading to greater weight gain.
Similar content being viewed by others
Background
Excessive gestational weight gain (GWG) and pre-pregnancy obesity are associated with higher risk of adverse pregnancy outcomes, such as macrosomia, gestational diabetes mellitus (GDM), preeclampsia, and caesarean delivery [1]. Several factors influence GWG, including quality of diet, physical activity levels, pre-pregnancy body mass index (BMI), maternal age and parity [2, 3]. The physiologic regulation of GWG is highly variable from one woman to another [4]; a few pregnancy-related hormones such as progesterone have been suggested to participate in GWG regulation [5] but most endogenous regulators are still unknown.
Leptin is an adipokine secreted mainly from adipocytes that circulates in proportion to white adipose tissue mass in non-pregnant individuals [6], reflecting energy stores in adipose tissue. Leptin is known for its role in energy homeostasis: monogenic leptin deficiency is associated with hyperphagia and morbid obesity in both animals and humans [7–9]. However, leptin resistance also appears to exist in obese individuals since higher endogenic leptin levels or exogenic leptin administration does not reduce weight in humans [10, 11]. In a physiologic framework, lower leptin levels are associated with increased weight gain in normal-weight young adults [12] and with greater weight regain after weight loss in obese individuals [13].
In pregnancy, the placenta is a substantial source of circulating leptin and levels increase throughout pregnancy [14, 15]. This seems counter-intuitive to leptin’s classic physiological role, as pregnancy should be a state where the energy signalling pathways favour a positive balance by increasing food intake. While we know that adiposity accumulation leads to higher leptin levels [15–19], how leptin may conversely act as regulator of subsequent weight gain in pregnancy is less understood. Current literature on this topic is sparse and inconclusive because of inconsistencies in study design – leptin levels measured before, during or after weight gain assessment – and incomplete adjustment for potential confounders [19–21]. Thus, we present here our prospective study designed to assess the associations between baseline leptin levels and subsequent GWG in a large population-based cohort of pregnant women, taking into account maternal adiposity status and period of the pregnancy.
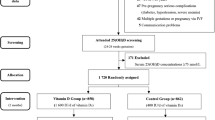
Methods
We recruited pregnant women at 1st trimester (5–16 weeks) of pregnancy and followed them until delivery in the prospective cohort study Glycemic regulation in Gestation and Growth (Gen3G). Pregnant women arriving for their 1st trimester blood sample visit between January 2010 and July 2013 were invited to participate in our study if they expected to deliver at the Centre Hospitalier Universitaire de Sherbrooke (CHUS). We excluded women who had any of the following criteria: age <18 years old, multiple pregnancy, pregestational diabetes (type 1 or 2) or diabetes discovered at 1st trimester (criteria based on 2008 Canadian Diabetes Association guidelines [22]), drugs and/or alcohol abuse, uncontrolled endocrine disease, or other major medical conditions (for attrition and further details, see [23]). The CHUS human-research ethics committee approved the project and all women gave written informed consent before they were included in the study, in accordance with the Declaration of Helsinki.
During their 1st visit, we collected demographics and baseline characteristics of participants, including maternal age, ethnic background, gestational age (confirmed by echography), parity, and personal and familial medical history. In order to collect data on lifestyle, we used validated questionnaires concerning nutrition and physical activity adapted from the Canadian Community Health Survey [24]. Anthropometric measurements including weight (kg; by a calibrated electronic scale, bare feet, in light clothing), height (m), BMI (kg/m2), % body fat (%BF; estimated by electrical bioimpedance using a standing foot-to-foot scale) and systolic and diastolic blood pressures were performed according to standardized procedures as described previously [25]. The majority of women (97%) also performed a 50g glucose challenge test with glucose levels measured 1-h after glucose ingestion, for early screening of GDM. We collected random non-fasting blood samples in the remaining participants.
At 2nd trimester (23–30 weeks), all women performed a 75g oral glucose tolerance test (OGTT) under fasting state for routine GDM diagnosis based on International Association of Diabetes and Pregnancy Study Groups criteria [26]. We collected extra fasting blood samples and at 1-h and 2-h during the OGTT for further analyses. Measures of glucose and insulin over the course of the OGTT allowed determination of dynamic indices of insulin sensitivity and secretion, respectively; Matsuda index (validated in pregnancy [27]), 10,000/[square root (fasting glucose × fasting insulin) × (mean glucose × mean insulin)] [28]; and total area under the curve (AUC)insulin/glucose was calculated using the trapezoidal rule applied to the insulin and glucose curves during the OGTT. We collected data concerning any medical updates since the last visit and repeated the nutrition and physical activity questionnaires. Once again, we measured anthropometry, according to the same standardized procedures. We calculated maternal GWG (kg) between 1st and 2nd trimester (mid pregnancy GWG) by subtracting 1st trimester from 2nd trimester maternal measured weights.
At the end of the 3rd trimester, we collected maternal weight (kg) based on the last prenatal visit (34–42 weeks of gestation) available in our electronic medical records (EMR). From the EMR, we additionally collected medical events from 2nd trimester to delivery for any additional major complications (premature deliveries, GDM, and pre-eclampsia) and placental and birth weights recorded by clinical staff at delivery. Women lost to follow-up did not differ from the ones followed until delivery [23]. We calculated maternal weight gain between 2nd and 3rd trimester (late pregnancy GWG) by subtracting 2nd trimester from 3rd trimester maternal weights.
Laboratory measurements
All blood samples collected at 1st and 2nd trimester were maintained at 4°C and centrifuged. Plasma was distributed in aliquots and stored at −80°C until measurements. Plasma leptin and insulin levels were measured by enzyme-linked immunosorbent assay (ELISA Luminex technology; Millipore Corp, Billerica, MA, USA). Plasma glucose levels were measured by glucose hexokinase (Roche Diagnostics, Indianapolis, IN, USA). Intra- and inter-assays coefficients of variation for leptin levels were respectively of 3 and 4%.
Statistical analyses
From all women followed until delivery, we excluded pregnancies with major complications (prematurity <37 weeks, pre-eclampsia) and missing data for weight or leptin levels at any of the time points. Participants excluded for complications, missing data or lost to follow-up (n = 288) were similar to women remaining in our dataset (n = 736) in terms of maternal age, ethnicity and pre-pregnancy BMI (all P > 0.05). We further excluded women diagnosed with GDM (n = 61) for this analysis because diagnosis and treatment of GDM greatly influence GWG. This report included 675 normoglycemic pregnant women who had a complete dataset from 1st trimester to delivery, including all necessary maternal weight and leptin levels.
Characteristics of participants are presented as means ± standard deviations if normally distributed or as median and interquartile ranges otherwise; categorical variables are presented as percentage. Continuous variables not normally distributed were log-transformed and we used log-transformed variables for correlations and linear regression models when appropriate; leptin levels were normally distributed after log-transformation. We performed correlation analyses (Pearson and Spearman as appropriate) to assess variables associated cross-sectionally with leptin levels and to evaluate potential confounders. We conducted linear regression analyses to assess associations between leptin levels (per one log increase) and subsequent GWG (using kg/week to standardize for different follow-up time), taking into account potential confounding factors. We first adjusted for gestational weeks and BMI (model 2a) measured cross-sectionally with leptin levels of interest at each time period assessed: for example the model testing the association between leptin at 1st trimester and subsequent GWG was adjusted for gestational age and BMI measured at 1st trimester. We then adjusted for %BF instead of BMI to account for adiposity per se (model 3a). We additionally adjusted for systolic and diastolic blood pressures, physical activity, quantity of fruits and vegetables consumed per day and frequency of restaurant meals per week to account for potential confounders including lifestyle (models 2b and 3b) using characteristics measured cross-sectionally with leptin levels for each respective model. We also performed linear regression analyses according to initial 1st trimester BMI categories as internationally defined (BMI <25 kg/m2 = normal weight; 25 ≤ BMI <30 kg/m2 = overweight; or BMI ≥30 kg/m2 = obese) to assess associations between leptin levels (per one log increase) and subsequent GWG (kg/week) per clinically defined BMI status. In addition to linear regression analyses assessing GWG per week (in tables), we performed subsidiary linear regression analyses with weight gain expressed as GWG between 1st and 2nd trimester (mid pregnancy GWG) and GWG between 2nd and 3rd trimester (late pregnancy GWG) for easier interpretation. We also conducted sensitivity analyses: 1- excluding underweight women defined as 1st trimester BMI <18.5 kg/m2 (n = 17); 2- excluding morbidly obese women defined as 1st trimester BMI >40 kg/m2 (n = 9); and by adding an additional variable in adjusted models, namely: 3- placental weight (available in 529 deliveries); 4- Matsuda index (insulin sensitivity index); or 5- AUCinsulin/glucose (insulin secretion index). P < 0.05 was considered statistically significant. All the analyses were performed using version 18 of Statistical Package for the Social Sciences (SPSS) for Windows.
Results
Characteristics of the 675 pregnant women included in the present study are presented in Table 1. Participants were 28.2 ± 4.3 years old and 97.2% were of European descent, similar to the general population of pregnant women receiving care at our institution [23].
Adiposity and weight gain
At 1st trimester, participants had a median BMI of 23.9[21.5–27.3] kg/m2 and a mean %BF equal to 31.3 ± 8.0 % (see Table 1). At 2nd trimester, median BMI was 26.6[24.1–29.8] kg/m2 and mean %BF was 35.4 ± 6.4 %. Women gained a mean of 6.7 ± 3.0 kg between 1st and 2nd trimester (weekly GWG = 0.40 ± 0.18 kg/week), and a mean of 5.6 ± 2.5 kg between 2nd trimester and late 3rd trimester (weekly GWG = 0.54 ± 0.23 kg/week) for a global mean GWG of 12.2 ± 4.4 kg between the 1st and the end of the 3rd trimester. Maternal factors at 1st trimester associated with larger subsequent GWG were lower adiposity levels (lower BMI and %BF) and being assessed at an earlier point of the pregnancy (as represented by gestational weeks). Other factors measured at 1st or 2nd trimester were weakly or non-significantly associated with subsequent GWG (see Additional file 1: Table S1). At delivery, birth weight was 3.408 ± 0.461 kg and placental weight was 557.4 ± 133.4 g in average. Most maternal weight and adiposity variables at 1st and 2nd trimester were positively correlated with birth weight and placental weight; the strongest associations were observed between maternal weight or %BF and either birth outcomes (see Additional file 2: Table S2).
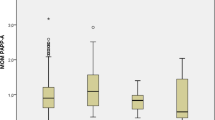
Leptin levels
Leptin levels increased from 1st (8.0[4.5–13.0] ng/ml) to 2nd trimester (10.3[6.1–16.0] ng/ml 1-h post OGTT; see Table 1), with a increase between 1st and 2nd trimester of 2.1[−0.5–5.3] ng/ml. Maternal factors positively associated cross–sectionally with leptin levels at 1st and 2nd trimester were adiposity levels (BMI and %BF) and blood pressures, while other factors were weakly or non-significantly associated with leptin levels (see Table 2 and Additional file 3: Table S3). Birth weight and placental weight were also weakly associated with maternal leptin levels at 1st and 2nd trimester (see Additional file 2: Table S2); these associations were substantially reduced and none of them remained significant after adjustments for maternal BMI.
Leptin levels and subsequent weight gain
Table 3 presents linear regression analyses testing the associations between leptin levels and subsequent GWG. In unadjusted analyses, higher 1st trimester leptin levels were associated with lower mid pregnancy GWG (β = −1.68, meaning a decrease of 1.68 kg per increase of one log-leptin at 1st trimester; standard error (SE) = 0.35; P < 0.0001). After adjusting for 1st trimester gestational weeks and BMI (model 2a), the direction of effect was reversed, meaning that higher leptin levels were associated with greater GWG (β = 1.32; SE = 0.49; P = 0.007). Replacing BMI by %BF at 1st trimester (model 3a) showed flattening of the association and leptin levels were no longer associated with mid pregnancy GWG (β = 0.38; SE = 0.52; P = 0.46). Further adjustments for blood pressure, physical activity, fruit and vegetable portions per day and restaurant meals per week did not modify associations in BMI of %BF adjusted models.
Higher 2nd trimester leptin levels were associated with greater late pregnancy GWG (β = 1.17; SE = 0.31; P = 0.0002 for 1-h post OGTT leptin levels). Associations were strengthened by adjustment for 2nd trimester gestational weeks and BMI with effect sizes almost doubling (β = 2.35; SE = 0.41; P < 0.0001 again for 1-h post OGTT leptin levels). Replacing BMI by %BF did not modify results in size or direction of effect. All associations remained statistically significant after further adjustment for blood pressure, physical activity, fruit and vegetable portions per day and restaurant meals per week, all measured at 2nd trimester (β = 2.15; SE = 0.42; P < 0.0001 for 1-h post OGTT leptin levels). Excluding underweight women (BMI <18.5 kg/m2) or morbidly obese women (BMI >40 kg/m2), or adding placental weight as an additional co-variable did not modify the results in sensitivity analyses. Our sensitivity analyses including insulin sensitivity or insulin secretion indices did not modify the associations. Linear regression analyses concerning late pregnancy GWG and 2nd trimester leptin levels measured fasting and 2-h post OGTT showed similar associations than those observed with 2nd trimester 1-h post OGTT leptin levels (see Additional file 4: Table S4).
Leptin levels and subsequent weight gain stratified by maternal weight status
In order to further investigate the role of initial adiposity in the association between leptin levels and subsequent GWG, we performed our analyses stratified by maternal weight status defined by BMI measured at 1st trimester (see Table 4). We found no association between 1st trimester leptin levels and mid pregnancy GWG in any BMI strata, neither in unadjusted nor in multivariate models (all P > 0.05).
Higher 2nd trimester leptin levels were associated with greater late pregnancy GWG in normal weight women (unadjusted β = 1.66, kg per log-leptin levels at 1h-OGTT; SE = 0.41; P < 0.0001). Associations between leptin levels and late GWG appeared stronger among overweight women with effect sizes almost twice the ones observed in normal weight women (unadjusted β = 3.60; SE = 0.88; P < 0.0001 – P = 0.05 for interaction between normal weight and overweight strata). Strength of associations was slightly reduced by adding potential confounders in fully adjusted models for normal weight and overweight women, mainly driven by presence of blood pressure and consumption of fruits/vegetables in the models. We observed no significant associations between 2nd trimester leptin levels and late pregnancy GWG in obese women (unadjusted β = 0.85; SE = 1.29; P = 0.51 for 1-h post OGTT leptin levels) in either unadjusted or adjusted analyses. After removing women with BMI >40 kg/m2 from the obese group, we observed that the effect size was slightly greater (unadjusted β = 1.66; SE = 1.38; P = 0.23 for 1-h post OGTT leptin levels; n = 101 women) but this remained non-significant. Our sensitivity analyses excluding underweight women (BMI <18.5 kg/m2) or including either placental weight, insulin sensitivity index or insulin secretion index as co-variables did not modify the results. Linear regression analyses using 2nd trimester leptin levels measured fasting and 2-h post OGTT showed similar associations than those observed with 1-h post OGTT leptin levels (see Additional file 5: Table S5).
Discussion
We demonstrated that higher 2nd trimester leptin levels were associated with greater subsequent GWG in pregnant women from a general population cohort, independent of maternal adiposity and other confounders. This positive association is the opposite of the expected physiologic regulation observed in non-pregnant individuals. Interestingly, this positive association was particularly observable and stronger in women classified as overweight at the beginning of pregnancy than in normal weight women.
Only a few studies have reported associations between baseline maternal leptin levels – measured at the beginning of the weight gain period – and subsequent GWG [19–21]. Our findings at 1st trimester are in line with previous findings from Walsh et al. and Kim et al., where 1st trimester leptin levels do not show a significant association with subsequent GWG after adjustments for %BF and other confounders [19, 21]. Thus, based on our results and those of others, lower 1st trimester leptin levels represent lower adiposity, signaling the need to increase positive energy balance and leading to greater weight gain early in pregnancy – similar to non-pregnant leptin’s role into central nervous system (CNS) signaling.
Our study adds to the current literature by investigating leptin levels measured at 24–28 weeks and subsequent GWG in a wide range of maternal BMI status. In contrast to our results, Kim et al. did not show associations between leptin levels measured at 24 weeks and any weight variables, including GWG. Difference in populations or limited power due to a smaller sample size (n = 75) may explain different findings from Kim et al. [21]. Walsh et al. measured leptin at 28 weeks, but assessed association with overall GWG throughout pregnancy – i.e. spanning a time period before and after our leptin measurement, and thus, we cannot compare their results to ours [19]. In line with our results in normal weight pregnant women, Stein et al. reported that higher leptin levels measured at 17 weeks of gestation were associated with a higher measured rate of weight gain between 20 and 36 gestational weeks in women with a pregravid BMI from 19.8 to 26.0 kg/m2 [20]. Our results expand current knowledge and suggest that this positive association is more prominent in overweight women. This is highly intriguing, as we know that clinically, overweight women are more likely to gain excessive GWG compared to normal weight and obese women.
The physiologic role of leptin during pregnancy is still obscure, but our results suggest that leptin promotes weight gain in a feed-forward mechanism during the second half of pregnancy. The placenta produces leptin in high quantity and contributes to maternal circulating levels throughout pregnancy, but why the placenta produces such a high quantity of leptin remains in question. Our results showing larger effect size in overweight women argue for the existence of this feed-forward regulation, as overweight women presented higher levels of leptin throughout pregnancy: if a pregnancy-specific CNS signal emerges as pregnancy advances, rising placental-derived leptin, in addition to high leptin from pre-pregnancy overweight status, might enhanced this positive feed-forward loop. Our findings of reduced associations in obese women could be explained by a state of central leptin resistance when levels reach the extreme upper range; but they could also reflect obese women self-regulating their energy balance based on clinical recommendations. It is also possible that leptin resistance occurring at the placenta level contributes to the absence of this feed-forward mechanism in obese women [29, 30]. However, the reduced effect sizes we observed in obese women should be interpreted with caution, given large confidence intervals and our smaller sample in this stratum.
Animal studies have supported the existence of a pregnancy-induced leptin resistance status [31–34]. For example, Ladyman et al. observed that intraperitoneal injections of leptin did not suppress food intake in pregnant mice compared to its observed effect of food intake reduction in non-pregnant mice [31]. The same report also demonstrated that the ventromedial hypothalamus and the paraventricular nucleus of pregnant mice showed a decrease in leptin sensitivity compared to non-pregnant mice [31]. Based on animal models, other potential mechanisms that could contribute to leptin resistance during pregnancy include an increase in circulating leptin binding protein, an impairment in leptin transport through the blood brain barrier, a decrease in Ob-Rb (isoform b of leptin’s receptor) mRNA (messenger ribonucleic acid) levels in the hypothalamus, and/or an impairment in the intracellular signalization induced by the binding of leptin to Ob-Rb [32–34]. In term human placenta tissue sections from obese pregnancies, it has also been shown that Ob-Rb is down regulated in comparison to lean pregnancies, raising the possibility of placental leptin resistance [29, 30]. Our results add to the current knowledge in suggesting that a state of leptin resistance also exists in human pregnancy, though the exact mechanisms leading to pregnancy-induced leptin resistance and a possible feed-forward loop in humans remain to be investigated. It did not seem that insulin resistance or insulin secretion influenced our observations, but other factors such as specific pregnancy hormones may be implicated and merit future investigations.
Strengths and limitations
A major strength of our study is the design, as participants were followed prospectively and represent the general population of pregnant women receiving care at our hospital [35]. Strengths of this study also include our large sample size, exclusion of diabetes at 1st and 2nd trimester, and use of standardized procedures with high reliability for all laboratory and clinical measures, including anthropometry.
The main limitation of our study is the observational study design; consequently, we cannot conclude about causality or any mechanistic pathways. Despite being validated in pregnancy [36], measurement of %BF by bioimpedance could be influenced differently at 2nd trimester by the presence of larger amount of body water, the placenta and the fetus. We used validated questionnaires for self-report of physical activity and nutrition, but direct measurements of energy intake and expenditure would have provided greater precision. Our population is mainly of European descent, so our results might not apply to other ethnicities.
Conclusions
In summary, our results suggest that body weight regulation by leptin during the second half of pregnancy does not follow the physiologic role as an adipostat with negative feedback to CNS that is classically attributed to leptin. We revealed a positive association between higher 2nd trimester leptin levels and greater subsequent GWG in normal weight women, and this association was stronger in overweight women. Our findings suggest a potential feed forward mechanism where higher leptin levels could signal the need to increase food intake and lead to greater weight gain. Feed forward loops are rare in human physiology, but are well known in the reproductive endocrine system – such as the menstrual cycle [37]. Mechanistic studies will be necessary to test this hypothesis and elucidate these mechanisms at the CNS and peripheral levels.
Ethics approval and consent to participate
The Centre Hospitalier Universitaire de Sherbrooke human-research ethics committee approved the project and all women gave a written informed consent before they were included in the study, in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Availability of data and materials
The dataset supporting the conclusions of this article is available upon request.
Abbreviations
- %BF:
-
percent body fat
- AUC:
-
area under the curve
- BMI:
-
body mass index
- CHUS:
-
Centre Hospitalier Universitaire de Sherbrooke
- CNS:
-
central nervous system
- ELISA:
-
enzyme-linked immunosorbent assay
- EMR:
-
electronic medical records
- GDM:
-
gestational diabetes mellitus
- GWG:
-
gestational weight gain
- mRNA:
-
messenger ribonucleic acid
- Ob-Rb:
-
isoform b of leptin’s receptor
- OGTT:
-
oral glucose tolerance test
- SD:
-
standard deviation
- SE:
-
standard error
- SPSS:
-
Statistical Package for the Social Sciences
References
Smith SA, Hulsey T, Goodnight W. Effects of obesity on pregnancy. J Obstet Gynecol Neonatal Nurs. 2008;37:176–84.
Wells CS, Schwalberg R, Noonan G, Gabor V. Factors influencing inadequate and excessive weight gain in pregnancy: Colorado, 2000-2002. Matern Child Health J. 2006;10:55–62.
Gardner B, Wardle J, Poston L, Croker H. Changing diet and physical activity to reduce gestational weight gain: a meta-analysis. Obes Rev. 2011;12:e602–20.
Dawes MG, Grudzinskas JG. Patterns of maternal weight gain in pregnancy. Br J Obstet Gynaecol. 1991;98:195–201.
Wuu J, Hellerstein S, Lipworth L, Wide L, Xu B, Yu GP, Kuper H, Lagiou P, Hankinson SE, Ekbom A, Carlstrom K, Trichopoulos D, Adami HO, Hsieh CC. Correlates of pregnancy oestrogen, progesterone and sex hormone-binding globulin in the USA and China. Eur J Cancer Prev. 2002;11:283–93.
Considine RV, Sinha MK, Heiman ML, Kriauciunas A, Stephens TW, Nyce MR, Ohannesian JP, Marco CC, McKee LJ, Bauer TL. Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N Engl J Med. 1996;334:292–5.
Hwa JJ, Ghibaudi L, Compton D, Fawzi AB, Strader CD. Intracerebroventricular injection of leptin increases thermogenesis and mobilizes fat metabolism in ob/ob mice. Horm Metab Res. 1996;28:659–63.
Farooqi IS, Matarese G, Lord GM, Keogh JM, Lawrence E, Agwu C, Sanna V, Jebb SA, Perna F, Fontana S, Lechler RI, DePaoli AM, O’Rahilly S. Beneficial effects of leptin on obesity, T cell hyporesponsiveness, and neuroendocrine/metabolic dysfunction of human congenital leptin deficiency. J Clin Invest. 2002;110:1093–103.
Gibson WT, Farooqi IS, Moreau M, DePaoli AM, Lawrence E, O’Rahilly S, Trussell RA. Congenital leptin deficiency due to homozygosity for the Delta133G mutation: report of another case and evaluation of response to four years of leptin therapy. J Clin Endocrinol Metab. 2004;89:4821–6.
Hukshorn CJ, Saris WH, Westerterp-Plantenga MS, Farid AR, Smith FJ, Campfield LA. Weekly subcutaneous pegylated recombinant native human leptin (PEG-OB) administration in obese men. J Clin Endocrinol Metab. 2000;85:4003–9.
Zelissen PM, Stenlof K, Lean ME, Fogteloo J, Keulen ET, Wilding J, Finer N, Rossner S, Lawrence E, Fletcher C, McCamish M, Group A. Effect of three treatment schedules of recombinant methionyl human leptin on body weight in obese adults: a randomized, placebo-controlled trial. Diabetes Obes Metab. 2005;7:755–61.
Allard C, Doyon M, Brown C, Carpentier AC, Langlois MF, Hivert MF. Lower leptin levels are associated with higher risk of weight gain over 2 years in healthy young adults. Appl Physiol Nutr Metab. 2013;38:280–5.
Holm JC, Gamborg M, Ward L, Ibsen KK, Gammeltoft S, Sorensen TI, Heitmann BL. Longitudinal analysis of leptin variation during weight regain after weight loss in obese children. Obes Facts. 2009;2:243–8.
Masuzaki H, Ogawa Y, Sagawa N, Hosoda K, Matsumoto T, Mise H, Nishimura H, Yoshimasa Y, Tanaka I, Mori T, Nakao K. Nonadipose tissue production of leptin: leptin as a novel placenta-derived hormone in humans. Nat Med. 1997;3:1029–33.
Misra VK, Trudeau S. The influence of overweight and obesity on longitudinal trends in maternal serum leptin levels during pregnancy. Obesity (Silver Spring). 2011;19:416–21.
Wolff S, Legarth J, Vangsgaard K, Toubro S, Astrup A. A randomized trial of the effects of dietary counseling on gestational weight gain and glucose metabolism in obese pregnant women. Int J Obes (Lond). 2008;32:495–501.
Ferraro ZM, Qiu Q, Gruslin A, Adamo KB. Excessive gestational weight gain and obesity contribute to altered expression of maternal insulin-like growth factor binding protein-3. Int J Womens Health. 2013;5:657–65.
Castellano Filho DS, do Amaral Correa JO, Dos Santos Ramos P, de Oliveira Montessi M, Aarestrup BJ, Aarestrup FM. Body weight gain and serum leptin levels of non-overweight and overweight/obese pregnant women. Med Sci Monit. 2013;19:1043–9.
Walsh JM, McGowan CA, Mahony RM, Foley ME, McAuliffe FM. Obstetric and metabolic implications of excessive gestational weight gain in pregnancy. Obesity (Silver Spring). 2014;22:1594–600.
Stein TP, Scholl TO, Schluter MD, Schroeder CM. Plasma leptin influences gestational weight gain and postpartum weight retention. Am J Clin Nutr. 1998;68:1236–40.
Kim KH, Kim YJ, Lee S, Oh SW, Lee K, Park Y, Kim HJ, Kwak H. Evaluation of plasma leptin levels & BMI as predictor of postpartum weight retention. Indian J Med Res. 2008;128:595–600.
Canadian Journal of Diabetes. [http://archive.diabetes.ca/files/cpg2008/cpg-2008.pdf]. Accessed 8 March 2016.
Guillemette L, Allard C, Lacroix M, Patenaude J, Battista M-C, Doyon M, Moreau J, Ménard J, Bouchard L, Ardilouze J-L, Perron P, Hivert M-F. Cohort profile: Genetics of Glucose regulation in Gestation and Growth (Gen3G) – a prospective pre-birth cohort of mother-child pairs in Sherbrooke, Canada. BMJ Open. 2016;6(2):e010031. doi:10.1136/bmjopen-2015-010031.
Canadian Community Health Survey, Cycle 2.2, Nutrition (2004)A Guide to Accessing and Interpreting the Data. [http://www.hc-sc.gc.ca/fn-an/alt_formats/hpfb-dgpsa/pdf/surveill/cchs-guide-escc-eng.pdf]. Accessed 8 March 2016.
Lacroix M, Battista MC, Doyon M, Menard J, Ardilouze JL, Perron P, Hivert MF. Lower adiponectin levels at first trimester of pregnancy are associated with increased insulin resistance and higher risk of developing gestational diabetes mellitus. Diabetes Care. 2013;36:1577–83.
Panel IA of D and PSGC, Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P, Dyer AR, Leiva A, Hod M, Kitzmiler JL, Lowe LP, McIntyre HD, Oats JJ, Omori Y, Schmidt MI. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–82.
Kirwan JP, Huston-Presley L, Kalhan SC, Catalano PM. Clinically useful estimates of insulin sensitivity during pregnancy: validation studies in women with normal glucose tolerance and gestational diabetes mellitus. Diabetes Care. 2001;24:1602–7.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–70.
Farley DM, Choi J, Dudley DJ, Li C, Jenkins SL, Myatt L, Nathanielsz PW. Placental amino acid transport and placental leptin resistance in pregnancies complicated by maternal obesity. Placenta. 2010;31:718–24.
Tessier DR, Ferraro ZM, Gruslin A. Role of leptin in pregnancy: consequences of maternal obesity. Placenta. 2013;34:205–11.
Ladyman SR, Fieldwick DM, Grattan DR. Suppression of leptin-induced hypothalamic JAK/STAT signalling and feeding response during pregnancy in the mouse. Reproduction. 2012;144:83–90.
Ladyman SR, Grattan DR. Suppression of leptin receptor messenger ribonucleic acid and leptin responsiveness in the ventromedial nucleus of the hypothalamus during pregnancy in the rat. Endocrinology. 2005;146:3868–74.
Ladyman SR, Grattan DR. Region-specific reduction in leptin-induced phosphorylation of signal transducer and activator of transcription-3 (STAT3) in the rat hypothalamus is associated with leptin resistance during pregnancy. Endocrinology. 2004;145:3704–11.
Trujillo ML, Spuch C, Carro E, Senaris R. Hyperphagia and central mechanisms for leptin resistance during pregnancy. Endocrinology. 2011;152:1355–65.
Hivert MF, Allard C, Menard J, Ouellet A, Ardilouze JL. Impact of the creation of a specialized clinic for prenatal blood sampling and follow-up care in pregnant women. J Obstet Gynaecol Can. 2012;34:236–42.
McCarthy EA, Strauss BJ, Walker SP, Permezel M. Determination of maternal body composition in pregnancy and its relevance to perinatal outcomes. Obstet Gynecol Surv. 2004;59:731–6.
Gardner DG, Shoback D. Greenspan’s Basic & Clinical Endocrinology. 2007. p. 508.
Acknowledgements
The authors wish to acknowledge the Blood Sampling in Pregnancy clinic at the Research Center of the Centre Hospitalier Universitaire de Sherbrooke (CR-CHUS; a Fonds de Recherche du Québec - Santé (FRQ-S) supported research center); the assistance of clinical research nurses (Maude Gérard, Marie-Josée Gosselin, Suzan Hayes, Georgette Proulx) and research assistants (Pascal Brassard, Caroline Rousseau) for recruitment and obtainment of consent from participants (all staff were employees of the CR-CHUS or the University of Sherbrooke); and the CHUS Biochemistry laboratory for performing blood glucose measurements.
Funding
The study was supported by a Fonds de Recherche du Québec - Santé (FRQ-S) Operating Grant (MF Hivert), Diabète Québec (P Perron) and a Canadian Diabetes Association Operating Grant (JL Ardilouze). MF Hivert was a FRQ-S research scholar and the recipient of a Clinical Scientist Award from the Canadian Diabetes Association (CDA) and the Maud Menten Award from the Institute of Genetics (IG) - Canadian Institute of Health Research (CIHR); MF Hivert is now the recipient of an ADA Accelerator Award #1-15-ACE-26. JL Ardilouze is a FRQ-S Junior 2 scholar. M Lacroix was supported by the FRQ-S, Diabète Québec, the Centre de recherche Mère-Enfant of Sherbrooke’s University, and the Foundation of Stars.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
ML performed data collection, data analysis/interpretation, and wrote the manuscript. MFH conceived the study design, provided assistance with the statistical analysis, and actively participated in data interpretation and the writing of the manuscript. MCB, MD, JMoreau and JMénard participated in recruitment and data collection. JP and LG participated in data collection. PP and JLA participated in study design conception. All authors revised the manuscript critically and gave their final approval of the submitted and published versions.
Additional files
Additional file 1: Table S1.
Correlations between women’s characteristics and subsequent GWG (expressed per week) in mid and late pregnancy. (DOCX 27 kb)
Additional file 2: Table S2.
Birth and placenta weights correlations with maternal weight-related variables and maternal leptin levels during pregnancy. (DOCX 27 kb)
Additional file 3: Table S3.
Correlations between women’s characteristics and leptin levels measured at 2nd trimester. (DOCX 27 kb)
Additional file 4: Table S4.
Correlations between 2nd trimester leptin levels and subsequent GWG (expressed per week)*. (DOCX 27 kb)
Additional file 5: Table S5.
Correlations between 2nd trimester leptin levels and subsequent GWG* stratified by 1st trimester BMI. (DOCX 27 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lacroix, M., Battista, MC., Doyon, M. et al. Higher maternal leptin levels at second trimester are associated with subsequent greater gestational weight gain in late pregnancy. BMC Pregnancy Childbirth 16, 62 (2016). https://doi.org/10.1186/s12884-016-0842-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-016-0842-y