Abstract
Background
The increasing number of operative deliveries is a topic of major concern in modern obstetrics. Maternal thyroid function is of known influence on many obstetric parameters. Our objective was to investigate a possible relation between maternal thyroid function, and operative deliveries. Secondary aim was to explore whether thyroid function was related to specific reasons for operative deliveries.
Methods
In this prospective cohort study, low-risk Caucasian women, pregnant of a single cephalic fetus were included. Women with known auto-immune disease, a pre-labour Caesarean section, induction of labour, breech presentation or preterm delivery were excluded. In all trimesters of pregnancy the thyroid function was assessed. Differences in mean TSH and FT4 were assessed using t-test. Mean TSH and FT4 levels for operative deliveries were determined by one way ANOVA. Repeated measurement analyses were performed (ANOVA), adjusting for BMI, partiy, maternal age and gestational age at delivery.
Results
In total 872 women were included, of which 699 (80.2 %) had a spontaneous delivery. At 36 weeks gestation women who had an operative delivery had a significantly higher mean TSH (1.63mIU/L versus 1.46mIU/L, p = 0.025) and lower mean FT4 (12.9pmol/L versus 13.3pmol/L, p = 0.007)) compared to women who had a spontaneous delivery. Mean TSH was significantly higher (p = 0.026) and mean FT4 significantly lower (p = 0.030) throughout pregnancy for women with an operative delivery due to failure to progress in second stage of labour, compared to women with a spontaneous delivery or operative delivery for other reasons.
Conclusions
Increased TSH and decreased FT4 seem to be associated with more operative vaginal deliveries and Caesarean sections. After adjusting for several confounders the association remained for operative deliveries due to failure to progress in second stage of labour, possibly to be explained by less efficient uterine action.
Similar content being viewed by others

Background
Increasing rates of Caesarean Sections (CS) is a topic of major concern in obstetrics. Both the incidences of planned and emergency CS are rising, without necessarily better neonatal outcomes [1, 2]. Operative vaginal deliveries (OVD) have a slowly decreasing trend, but OVD are still common, especially in nulliparous women [1]. Maternal morbidity and mortality rates are higher for women with a CS or OVD [2, 3]. Many studies have been performed to determine risk factors associated with operative deliveries. The main risk factors for CS and OVD are nulliparity, induction of labour, increasing maternal age, abnormal position of the fetus, high maternal body mass index (BMI) and previous CS [4–6]. Most CS and OVD are performed due to failure to progress, especially in nulliparous women [6]. The main reason is inefficient uterine action and to a lesser extent cephalopelvic disproportion. In fact, efficient uterine action is more and more considered as the key to normal delivery [7, 8].
In previous studies it has been demonstrated that suboptimal maternal thyroid function (high maternal thyrotrophine stimulating hormone (TSH) and low free thyroxine (FT4)) is associated with adverse pregnancy outcomes [9–12]. Women with suboptimal thyroid function, mainly those with TPO-antibodies (thyroid-peroxidase-antibody), are at risk for miscarriage and preterm birth [9, 10]. Furthermore, there is evidence that high maternal TSH might interfere with normal obstetric outcome at term, with higher incidences of small for gestational age neonates [11], gestational diabetes [10] and meconium stained amniotic fluid [12]. Low FT4 has been associated with poor fetal neurodevelopment and psychomotor development in early childhood [13].
Little research is done into the relation between maternal thyroid function and uterine contractions. However, there is some evidence that suboptimal maternal thyroid function might be associated with more breech presentations, possibly due to increased stiffness of the myometrium [14]. This increased stiffness in patients with suboptimal thyroid function has been demonstrated in previous research in vascular smooth muscle cells as well [15, 16].
In the current study we evaluated a possible relationship between suboptimal maternal thyroid function and inefficient uterine action at term. Primary objective was to investigate a possible relation between maternal thyroid function and incidence of CS and OVD. Secondary objective was to explore whether thyroid function was related to specific reasons for operative deliveries: due to fetal distress or failure to progress. In order to create a representative low-risk group we excluded the women at high risk for operative deliveries (previous CS, inductions, breech presentations, multiple pregnancies).
Methods
Design and participants
Between January 1997 and April 1998, 1702 women who booked for antenatal visits at 12 weeks gestation were followed in five community midwife practices in the vicinity of Eindhoven (the Netherlands). Only Dutch Caucasian women were eligible to avoid language problems and confounding factors of ethnicity. General patient characteristics including BMI, education level, smoking status, maternal age and parity were collected. Information of possible previous pregnancies was collected. A cohort of women at low-risk for obstetric complications was defined, with the exclusion of preterm deliveries, breech presentations, multiple pregnancies and induction of labour. Women on thyroid medication, with type I diabetes and with a new diagnosis of overt hyper- or hypothyroidism at first screening were excluded. Delivery was considered an OVD when there was a ventouse or forceps delivery. In cases without CS or OVD, delivery was defined as spontaneous. The reasons for OVD and CS were classified as fetal distress, failure to progress in first stage of labour (prolonged dilatation) or failure to progress in second stage of labour (prolonged expulsion). Fetal distress was defined as a non-reassuring fetal heart rate with cardiotocography, as assessed by the responsible obstetrician using the FIGO classification.
The selection process is shown in Fig. 1 and the characteristics are shown in Table 1. This study was approved by the Medical Ethical Committee of Máxima Medical Centre in Eindhoven/Veldhoven. (METC project number: 0116) and written informed consent was obtained from all participants.
Analysis
TSH was measured in serum at 12, 24 and 36 weeks using a solid-phase, two site chemiluminescent enzyme immunometric assay (IMMULITE Third generation TSH, Diagnostic Products Corporation, Los Angeles USA). The inter-assay coefficients of variation were 5.0 % and 4.4 % at concentrations 0.22 mIU/L and 2.9mIU/L, respectively. The non-pregnant reference range of TSH is 0.45 - 4.5 mIU/L. FT4 concentration was measured in serum at 12, 24 and 36 weeks with a solid-phase immunometric assay (IMMULITE Free T4). The inter-assay coefficients of variation for this technique were 6.7 % and 4.4 % at concentrations of 11.6 pmol/L and 31.5 pmol/L, respectively. TPO-Antibodies were determined in serum at 12, 24 and 36 weeks by means of the IMMULITE Anti-TPO-Ab kit. The inter-assay coefficients of variation for this analysis were 9 % and 9.5 % for concentrations of 40 kU/ml and 526 kU/ml, respectively. The anti-TPO assay is standardized in terms of the International Reference Preparation for anti-TPO MRC 66/387. Women were defined as TPO-Ab-negative when the titer was below 35 kU/ml at 12 weeks gestation. The highest TSH level found in our sample was 6.1 mIU/L. All measurements were performed in one laboratory.
Statistical analysis
Statistical analysis was performed using the Statistical Package of Social Science (SPSS, 19.0). There were missing data in 37 cases, which were excluded from further analysis. The data from women who gave informed consent did not differ from the non-responders regarding maternal age, educational level and parity.
TSH and FT4 concentrations were not normally distributed. However, because the cohort size of all subgroups was substantial (n > 30) we were able to calculate differences in means (SD) of thyroid hormones concentration levels using Welch T-test (two-tailed). Differences in prevalence were calculated by chi-square. Subsequently, repeated measures ANOVA was performed to determine whether the changes of TSH and FT4 during pregnancy were associated with the mode of delivery and the different reasons for OVD or CS. We compared the changes of mean FT4 and TSH throughout pregnancy in women with and without a spontaneous delivery using repeated measurement analyses, adjusting for various selected confounders such as parity, gestational age, BMI and maternal age, as these are all of known influence on the risk of an operative delivery.
Results
Table 1 shows that women who undergo an operative delivery have a higher pre-pregnancy BMI (26.3 kg/m2 versus 25.0 kg/m2) (p = 0.002) and have a longer gestational age (40.3 versus 39.8 weeks gestation) (p < 0.001). There were no statistically significant differences between a history of thyroid dysfunction in the family or the prevalence of positive TPO-antibodies. However, at 36 weeks gestation (third trimester) women who had an OVD or CS had a significantly higher mean TSH and lower mean FT4 compared to women who had a spontaneous delivery (TSH 1.63 mIU/L versus 1.46 mIU/L (p = 0.025) and FT4 12.9 pmol/L versus 13.4 pmol/L (p = 0.007) respectively). The 75 women with elevated TPO-Ab titres had significantly (T-test, two tailed, P < 0.001) higher mean TSH at 12, 24 and 36 weeks gestation compared to the remaining TPO-Ab negative women: 1.80 (SD: 1.21) versus 1.14 (0.68), 1.69 (SD0.98) versus 1.29 (0.60), 1.73 (SD:1.01) versus 1.46 (SD: 0.70), respectively. In the 797 TPO-Ab negative women at 12 weeks, we calculated the 2.5 and 97.5 percentile of TSH to define the normal reference range of TSH, this was 0.13 2.8 mIU/l. Subsequently we were able to assess the number of women with hypothyroxinemia at 12 weeks gestation: FT4 < 10th percentile (< 13.4 pmol/l) with normal TSH values: 79 (9.1 %).
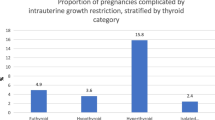
The different modes of delivery and the reasons for OVD and CS are shown in Table 2. 80.2 % of the women had a spontaneous delivery and in 19.8 % of the women an OVD or CS was performed. In 5.8 % of the deliveries there was an OVD or CS due to failure to progress in first stage of labour, in 7.9 % of the deliveries there was failure to progress in second stage of labour and 6.1 % of all deliveries were terminated due to fetal distress. Mean FT4 and mean TSH were compared between these subgroups using one way ANOVA. As shown in Table 2, mean TSH was significantly higher at 12 weeks of gestation (p = 0.010) and at showed a trend at 24 (p = 0.093) and 36 weeks gestation (p = 0.066) for women with an operative delivery due to failure to progress in second stage of labour. Mean FT4 was lower at a 90 % significance level at the first and third trimester of pregnancy for women with failure to progress in second stage of labour (p = 0.07, p = 0.16, p = 0.08 respectively).
As shown in Fig. 2, women who had an OVD or CS for failure to progress in the second stage of labour (delayed expulsion) had higher mean TSH levels (p = 0.026) at all trimester adjusted for age, parity, BMI and gestational age, compared to women who had a spontaneous delivery or an OVD or CS for other reasons. TSH was also significantly associated with parity. In Fig. 3 it is shown that women with an OVD or CS for failure to progress in second stage of labour, had a significant lower mean FT4 in all trimesters (p = .0.030), adjusted for age (p < 0.001), parity (p = 0.26), BMI (p < 0.001) and gestational age (0.44), compared to women with a spontaneous delivery or OVD or CS for other reasons (see Table 3). There were no differences in maternal thyroid function between women who had a spontaneous delivery compared to women who underwent an OVD or CS for fetal distress or failure to progress in the first stage of labour (delayed dilatation). When we repeated the analyses excluding women with hypothyroxinemia, similar results were found (data not shown).
The relation between mean TSH at all trimesters and the mode of delivery in 872 term women in whom labour started spontaneously: women who had an operative vaginal delivery or Caesarean section because of prolonged expulsion had significantly higher mean TSH throughout gestation (repeated measures ANOVA, F = 3.1, p = 0.026.), adjusted for age, parity, gestational age and BMI
The relation between mean FT4 at three trimesters and the mode of delivery in 872 term women in whom labour started spontaneously: women who had an operative vaginal delivery or Caesarean section because of prolonged expulsion had significantly lower mean FT4 throughout gestation (repeated measures ANOVA, F = 3.0, p = 0.030), adjusted for age, parity, gestational age and BMI
Discussion
In this study we found a significant association between high normal maternal TSH and low normal FT4 and the risk of operative delivery for women in spontaneous labour at term, not accounted for confounders. Our cohort consisted of 872 Caucasian women with a low-risk pregnancy. Planned Caesarean sections, inductions of labour, preterm deliveries and breech presentations were excluded. Our cohort was representative in terms of thyroid function and obstetric outcome. We did find a higher incidence of TPO-Ab in our study (8.6 %) compared to another large cohort study in the Netherlands (5.6 %) [17], but this can be explained by 40 % black women in their population, in whom TPO-Ab are less frequently found [18], while our sample included only white Caucasian women. Mean TSH and FT4 levels of the current study are comparable to their sample. Obstetric outcome was proportionate to a large cohort study carried out in the Netherlands to analyse trends in obstetric interventions[1]. They found a CS rate of 7.5 % for nulliparous women in spontaneous labour and an OVD rate of around 10 % between 1993 and 2002, with an increase in CS rates over the years [1]. Our total operative delivery rate was 20 %, for OVD and CS combined.
The current study showed that women who undergo a CS or OVD had a higher pre-pregnancy BMI and delivered at a later gestational age. This finding is consistent with previous reports [8, 19–21]. We also found that women with an operative delivery for failure to progress in second stage of labour had higher mean TSH levels and lower mean FT4 levels throughout pregnancy, compared to women who delivered spontaneously or had an operative delivery for another reason. This finding was adjusted for maternal age, pre-pregnancy BMI, parity and gestational age at time of delivery.
Strength and limitations
One of the main strengths of this study is the fact that maternal thyroid function was assessed prospectively throughout pregnancy at fixed time-intervals. Repeated measurement analysis was performed to assess changes in thyroid function within and between subjects. Furthermore, we corrected for important confounders, including BMI, which is one of the known risk factors for operative deliveries [8, 19, 20]. We have not used cut off values for suboptimal maternal thyroid function. We believe that this is a major strength of this study, as there is considerable discussion about the proper cut off values and the definition of, for example, subclinical hypothyroidism in pregnancy [22, 23].
A limitation of the study is the fact that this was an observational study and therefore no conclusions on causality of the associations can be drawn. Furthermore, no strict definitions of fetal distress were used. Diagnosis of fetal distress was made on the basis of a non-reassuring fetal heart pattern. As only healthy Dutch Caucasian women were analysed in this study, extrapolation of the results to women with other ethnicities or to high risk pregnant women with for example hypertension or diabetes must be taken with caution. Furthermore, we did not consider iodine status in our cohort. However, it is known that in this region iodine intake is generally sufficient [24].
Interpretation
Higher TSH and lower FT4 in this euthyroid sample were associated with higher operative delivery rates. However, TSH and FT4 were still in the normal ranges for all groups. In a large retrospective cohort study from Männistö et al. increased odds for CS (both prelabour and during labour) were found in women with primary hypothyroidism [25]. From that study however, it was not clear for what reasons the CS were performed.
The main difference in the current study, according to maternal TSH and FT4, is found in OVD and CS due to failure to progress in second stage of labour. It is known that the most important factor in the expulsion of the fetus is the thickness of the myometrium and thus the strength of the contractions, despite the pushing efforts of the mother [26]. It has not been well established whether the spontaneous contractions are stronger during the second stage of labour than during the first stage of labour, but it is known that during Valsalva the power of the contractions is significantly higher in the second stage of labour [27]. With Valsalva it is not only smooth muscle cell contractions, but contractions of the skeleton muscles of the abdominal wall as well, that determine the expulsive power. It is well known that thyroid hormones are of influence on the contractile phenotype of skeletal muscles [28]. The most effective uterine action is needed in the second stage of labour and factors that are of influence on the strength of the contractions will therefore become most apparent during this stage.
Calcium influx is necessary for excitation of the smooth muscle cells and therefore for the myometrial contractility required during labour. Parija et al. have demonstrated that hypothyroidism reduces calcium channel function in uterine tissue of the pregnant rat [29]. A study from Corriveau et al. has found that the amplitude and time course of contractions is enhanced in patients treated with thyroid hormone compared to controls [30]. This suggests that thyroid function is of direct influence on myometrial contractility. Besides the absolute strength of the contractions, it has also been found in vascular research that hypothyroidism leads to impaired smooth muscle cell relaxation, leading to increased artertial stiffness [15, 16]. Moreover, women with failed external cephalic version had higher TSH values, probably because of impaired uterine relaxation which is essential for the breech baby to turn [31]. The combination of the strength of the contractions and the impaired relaxation of the myometrium might lead to less efficient uterine action in women with suboptimal thyroid function in this study. Future research should confirm this finding in a larger population and determine whether treatment of suboptimal maternal thyroid function leads to less failure to progress. In our cohort the mean TSH and FT4 were all in the normal reference ranges for the pregnant population.
Conclusions
Increased TSH and decreased FT4 seem to be associated with more operative vaginal deliveries and Caesarean sections. After adjusting for several confounders the association remained for operative deliveries due to failure to progress in second stage of labour, possibly to be explained by less efficient uterine action. The conclusions of this study are very relevant, as the increasing incidence of CS is one of the major concerns in modern obstetrics. Future research should confirm our findings and focus on determining the direct effect of maternal thyroid hormones on uterine contractions in vivo.
Abbreviations
- BMI:
-
Body mass index
- CS:
-
Caesarean section
- FT4:
-
Free thyroxine
- OVD:
-
Operative vaginal delivery
- TPO-Ab:
-
Thyroid peroxidase antibodies
- TSH:
-
Thyrotropine stimulating hormone
References
Kwee A, Elferink-Stinkens P, Reuwer P, Bruinse H. Trends in obstetric interventions in the Dutch obstetrical care system in the period 1993–2002. Eur J Obstet Gynecol Reprod Biol. 2007;132(1):70–5.
Khunpradit S, Tavender E, Lumbiganon P, Laopaiboon M, Wasiak J, Gruen R. Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database Syst Rev. 2011;15:6.
Burrows L, Meyn L, Weber A. Maternal morbidity associated with vaginal versus Cesarean delivery. Obstet Gynecol. 2004;103(5):907–12.
Vayssière C, Beucher G, Dupuis O, Feraud O, Simon-Toulza C, Sentilhes L, et al. Instrumental delivery: clinical practice guidelines from the French College of Gynaecologists and Obstetricians. Eur J Obstet Gynecol Reprod Biol. 2011;159(1):43–8.
Schuit E, Kwee A, Westerhuis M, van Dessel H, Graziosi G, van Lith J, et al. A clinical prediction model to assess the risk of operative delivery. BJOG. 2012;119:915–23.
Sheiner E, Levy A, Feinstein U, Hallaki M, Mazori M. Risk factors and outcome of failure to progress during the first stage of labor: a population-based study. Acta Obstet et Gynecol Scand. 2002;81:3.
O'Driscoll K, Stronge J, Minogue M. Active management of labour. BMJ. 1973;3:135–7.
Kenyon S, Tokumasu H, Dowswell T, Pledge D, Mori R. High-dose versus low-dose oxytocin for augmentation of delayed labour. Cochrane Database Syst Rev. 2013;13:7.
Thangaratinam S, Tan A, Knox E, Kilby M, Franklyn J, Coomarasamy A. Association between thyroid autoantibodies and miscarriage and preterm birth: meta-analysis of evidence. BMJ. 2011;9(342):1–8.
Karakosta P, Alegakis D, Georgiou V, Roumeliotaki T, Fthenou E, Vassilaki M, et al. Thyroid dysfuntion and autoantibodies in early pregnancy are associated with increased risk of gestational diabetes and adverse birth outcomes. J Clin Endocrinol Metab. 2012;97(12):4464–72.
Monen L, Kuppens S, Hasaart T, Oosterbaan H, Oei S, Wijnen H, et al. Maternal thyrothropin is independently related to small for gestational age neonates at term. Clin Endocrinol. 2015;82(2):254–9.
Monen L, Kuppens S, Hasaart T, Wijnen H, Pop V. Maternal thyrotrophin in euthyroid women is related to meconium stained amniotic fluid in women who deliver at or over 41 weeks of gestation. Early Hum Dev. 2014;90(7):329–32.
Pop V, Kuijpens J, van Baar A, Verkerk G, van Son M, de Vijlder J, et al. Low maternal free thyroxine concentrations during early pregnancy are associated with impaired psychomotordevelopment in infancy. Clin Endocrinol (Oxf). 1999;50(2):149–55.
Kuppens S, Kooistra L, Wijnen H, Crawford S, Vader H, Hasaart T, et al. Maternal thyroid function during gestation is related to breech presentation at term. Clin Endocrinol. 2010;72(6):820–4.
Owen P, Rajiv C, Vinereanu D, Mathew T, Fraser A, Lazarus J. Subclinical hypothyroidism, arterial stiffness and myocardial reserve. J Clin Endocrinol Metab. 2006;91(6):2126–32.
Ojamaa K, Klemperer J, Klein I. Acute effects of thyroid hormone on vascular smooth muscle. vascular smooth muscle. Thyroid. 1996;6(5):505–12.
Medici M, Timmermans S, Visser W, de Muinck K-SS, Jaddoe V, Hofman A, et al. Maternal thyroid hormone parameters during early pregnancy and birth weight: the generation R study. J Clin Endocrinol Metab. 2013;98(1):59–66.
La'ulu SL, Roberts WL. Second-Trimester Reference Intervals for Thyroid Tests: The Role of Ethnicity. Clin Chem. 2007;53(9):1658–64.
Roman H, Goffinet F, Hulsey T, Newman R, Robillard P, Hulsey T. Maternal body mass index at delivery and risk of caesarean section due to dystocia in low risk pregnancies. Acta Obstet Gynecol Scand. 2008;87(2):163–70.
Zhang J, Bricker L, Wray S, Quenby S. Poor uterine contractility in obese women. BJOG. 2007;114(3):343–8.
Caughey A, Stotland N, Washington A, Escobar G. Maternal and obstetric complications of pregnancy are associated with increasing gestational age at term. Am J Obstet Gynecol. 2007;196(2):155.
Pop V, Broeren M, Wiersinga W. The attitude towards hypothyroidism during early gestation: time for a change of mind? Thyroid. 2014;24(10):1541–6.
Teng W, Shan Z, Patil-Sisodia K, Cooper D. Hypothyroidism in pregnancy. Lancet Diabetes endocrinol. 2013;1(3):228–37.
Wiersinga WM, Podoba J, Srbecky M, v Vessem M, v Beeren HC, Platvoet-Ter Schiphorst MC. A survey of iodine intake and thyroid volume in dutch schoolchildren: reference values in an iodine-sufficient area and the effect of puberty. Eur J Endocrinolog. 2001;144(6):595–603.
Männistö T, Mendola P, Grewal J, Xie Y, Chen Z, Laughon K. Thyroid disease and adverse pregnancy outcomes in a contemporary US cohort. J Clin Endocrinol Metab. 2013;98(7):2725–33.
Buhimschi C, Buhimschi I, Malinow A, Kopelman J, Weiner C. Pushing in labor: performance and not endurance. Am J Obstet Gynecol. 2002;186(6):1339–44.
Buhimschi C, Buhimschi I, Malinow A, Weiner C. Uterine contractility in women whose fetus is delivered in the occipitoposterior position. Am J Obstet Gynecol. 2003;188(3):734–9.
Simonides W, van Hardeveld C. Thyroid hormone as a determinant of metabolic and contractile phenotype of skeletal muscle. Thyroid. 2008;18(2):205–16.
Parija S, Mishra A, Raviprakash V. Hypothyroid state reduces calcium channel function in 18-day pregnant rat uterus. Indian J Exp Biol. 2006;44(1):19–27.
Corriveau S, Pasquier J, Blouin S, Bellabarba D, Rousseau E. Chronic levothyroxine and acute T3 treatments enhance the amplitude and time course of uterine contractions in human. Am J Physiol Endocrinol Metab. 2013;304(5):E478–85.
Kuppens S, Kooistra L, Hasaart T, van der Donk R, Vader H, Oei G, et al. Maternal thyroid function and the outcome of external cephalic version: a prospective cohort study. BMC Pregnancy Childbirth. 2011;11(10).
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LM participated in the design, performed the statistical analysis and drafted the manuscript. VP has performed the statistical analysis and helped to draft the manuscript. TH has helped to draft the manuscript. HW has collected all the data and helped to perform the statistical analyses. SO has participated in the design of the study and helped to draft the manuscript. SK has participated in the design of the study and drafted the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Monen, L., Pop, V., Hasaart, T. et al. Increased maternal TSH and decreased maternal FT4 are associated with a higher operative delivery rate in low-risk pregnancies: A prospective cohort study. BMC Pregnancy Childbirth 15, 267 (2015). https://doi.org/10.1186/s12884-015-0702-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-015-0702-1