Abstract
Background
Stroke-associated pneumonia (SAP) considerably burden healthcare systems. This study aimed to identify predictors of developing SAP in acute ischemic stroke patients admitted to the Stroke Unit at Manial Specialized Hospital factors with microbiological causality and impact on 30-day mortality.
Methods
This was a retrospective cohort study. All patients with acute ischemic stroke admitted to the Stroke Unit at Manial Specialized Hospital (from February 2021 to August 2023) were divided into the SAP and non-SAP groups. Detailed clinical characteristics and microbiological results were recorded.
Results
Five hundred twenty-two patients diagnosed with acute ischemic stroke (mean age of 55 ± 10) were included. One hundred sixty-nine (32.4%) of stroke patients developed SAP; Klebsiella pneumoniae was the most commonly detected pathogen (40.2%), followed by Pseudomonas aeruginosa (20.7%). Bacteremia was identified in nine cases (5.3%). The number of deaths was 11, all of whom were diagnosed with SAP, whereas none from the non-SAP group died (P < 0.001). The binary logistic regression model identified three independent predictors of the occurrence of SAP: previous history of TIA/stroke (OR = 3.014, 95%CI = 1.281–7.092), mechanical ventilation (OR = 4.883, 95%CI = 1.544–15.436), and bulbar dysfunction (OR = 200.460, 95%CI = 80.831-497.143).
Conclusions
Stroke-associated pneumonia was reported in one-third of patients with acute ischemic stroke, adversely affecting mortality outcomes. Findings showed that the main predictors of SAP were bulbar dysfunction, the use of mechanical ventilation and previous history of TIA/stroke. More attention to these vulnerable patients is necessary to reduce mortality.
Similar content being viewed by others
Introduction
Stroke-associated pneumonia (SAP) is defined as pneumonia that occurs within seven days of the stroke onset. It is associated with prolonged hospital stays, poor outcomes, and high economic burden [1, 2]. However, Morbidity and mortality rates of SAP vary among hospital-based studies. Bulbar dysfunction is a well-known risk factor implicated in developing SAP. However, stroke itself induces an immunosuppressive state, increasing infection susceptibility [3, 4].
Based on epidemiological reports of SAP, Streptococcus pneumoniae (S. pneumoniae) Methicillin-resistant Staphylococcus aureus (MRSA), Klebsiella pneumonia (K. pneumoniae), Pseudomonas aeruginosa (P. aeruginosa), and Escherichia coli (E. coli), and Haemophilus influenza (H. influenzae) are the main pathogens linked to SAP [5,6,7]. Antibiotic-resistant organisms are also a critical concern [8].
Each region should share its experience with SAP from the perspective of the prevalence of SAP, identifying risk factors, commonly detected pathogens and its impact on mortality outcomes. This will contribute to developing appropriate management and prevention strategies to reduce the risks and improve patient outcomes.
Hence, we conducted this observational retrospective study to identify factors associated with the increased occurrence of SAP with underlying microbiological analysis among acute ischemic stroke patients and their impact on 30-day mortality.
Methods
Study design and participants
This retrospective cohort study targeted patients admitted to the Stroke Unit at Manial Specialized Hospital in Cairo, Egypt, from February 2021 to August 2023. Only adult patients (age > 18) admitted with acute ischemic stroke during the study period were included. Exclusion criteria included stroke of hemorrhagic type, stroke patients presented with infections other than bacterial pulmonary infections, and pediatric group (age < 18). The ethical approval was granted by the ethical committee at Kasr Alainy Faculty of Medicine-Cairo University (N-135-2023).
The included patients were divided into the stroke-associated pneumonia (SAP) and non-SAP groups. The diagnosis of SAP was established by clinicians during the hospital stay based on modified Centers for Disease Control and Prevention (CDC) criteria [9]; symptoms and signs suggestive of acute lower respiratory tract infection, chest imaging, and supported by microbiological results.
Data collection
The following data were collected from the medical records of all enrolled patients: age, sex, medical comorbidities, smoking status, and drug abuse. Besides, stroke characteristics include the site of brain infarction and etiological classification according to the Org 10,172 trial in the acute stroke treatment (TOAST) categories [10]. The severity of neurological deficits at stroke onset was also assessed using the National Institutes of Health Stroke Scale (NIHSS), based on the following evaluations: a score of 1–4 = minor stroke, 5–15 = moderate stroke, 16–20 = moderate to severe, and a score ≥ 21 denotes severe stroke [11]. The initial level of consciousness was assessed, using the Glasgow coma scale (GCS) [12]. The 3-ounce water swallow test was used for screening for bulbar dysfunction [13]. Patients who fail dysphagia screening were further evaluated by Videofluoroscopic swallowing evaluation (VFSE) to directly visualize the swallowing process. Also, the need for mechanical ventilation, nasogastric tube, and duration of hospital stay were recorded.
Microbiological analysis
Results of the positive cultures of respiratory specimens (sputum, endotracheal aspirate, and bronchoalveolar lavage) and blood specimens were obtained from the medical records of the SAP patients and further analyzed for the frequency of Gram-negative and Gram-positive bacteria distribution.
Study outcome
The main study outcome is either 30-day mortality or survival.
Sampling
The sample size was calculated based on a previous study in which the incidence of SAP was 21% [14]. Accordingly, the minimal sample size was 162 patients to achieve 80% power and 5% significance using the Open Epi online sample size calculator.
Statistical analysis
All the collected data were revised for completeness and logical consistency. The data was entered into the Microsoft Office Excel Software Program 2019, then transferred into the Statistical Package of Social Science Software program, version 26 (SPSS) for statistical analysis.
Median and IQR were used to summarize quantitative variables, and the Mann-Whitney U test was used for comparison, where the significance at P-value ≤ 0.05. Frequency and percentage were used to summarize qualitative variables, and the Chi-square test was used for comparison, where a significance at a P-value ≤ 0.05.
A binary logistic regression model was used to determine the effect of independent factors (previous history of TIA/stroke, diabetes mellitus, NIHSS, disturbed conscious level, bulbar dysfunction, and mechanical ventilation) on the occurrence of SAP (dependent variable).
Results
Data for 522 patients diagnosed with acute ischemic stroke were evaluated [363 males (69.5%) and 159 females (30.5%)], with a mean age of 55 ± 10. The median NIHSS at stroke onset was 11, with IQR 8–12. Their median hospital stay was 5, with IQR 4–10 days.
Microbiological analysis
One hundred sixty-nine (32.4%) of stroke patients developed SAP, in which pathogens were isolated from sputum samplings in 130 patients (76.9%), endotracheal tube aspirate in 38 (22.5%), and bronchoalveolar lavage in only one case (0.6%).
Most of the patients were infected by Gram-negative aerobic bacilli (n = 138), of whom seven patients had double Gram-negative aerobic bacilli infections (Klebsiella species and E. coli), while thirty-one were infected by Gram-positive aerobic cocci (Fig. 1).
Bacteremia -evident by blood cultures- was identified in nine cases (5.3%) (5 were infected by MERSA, two were infected by Actinobacter, and the other two were infected by Klebsiella). Candida albicans was detected in seven cases.
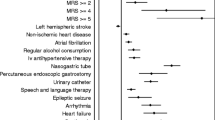
Comparison of patients with SAP and non-SAP groups
the percent of History of previous stroke/TIAs as well as the presence of diabetics, was significantly higher in patients with SAP than those without SAP. However, other vascular risk factors did not significantly differ between the two groups (Table 1).
Regarding stroke characteristics, the percent of bulbar dysfunction was significantly higher in patients with SAP (80.9%) than those without SAP (19.1%). Moreover, the percent of non-disturbed consciousness was significantly higher in non-SAP (71.6%) than in SAP (28.4%) groups (Table 2). Categorical severity of NIHSS was also significantly different between SAP and non-SAP groups, as the SAP group had significantly more severe NIHSS grading than the non-SAP group (Table 2).
Also, mechanical ventilation and nasogastric tube use were significantly higher in patients who had SAP (78.3%, 84.2%) than those without SAP (21.7%, 15.8%), respectively (Table 3). Patients with SAP had a significantly higher length of hospital stay than the group without SAP (Table 3).
Predictors of occurrence of SAP
The binary logistic regression model identified three independent predictors of the occurrence of SAP. Previous history of TIA/stroke, mechanical ventilation, and bulbar dysfunction increased the odds of developing SAP by 3, 5, and 200 times (Table 4).
Mortality outcome
Five hundred-eleven patients survived (97.9%), whereas 11 (2.1%) died (P < 0.001, Table 5). All deaths had SAP, nine of whom had bacteremia.
Discussion
The current study provides thorough information on the incidence and predictors of SAP with detailed microbiological analysis and its impact on 30-day mortality outcomes among 522 patients with acute ischemic stroke admitted to the Stroke Unit at Manial Specialized Hospital, one of the tertiary stroke centres in Cairo. These findings would be of interest to healthcare specialists who aim to improve stroke care services and reduce the financial burden on medical care.
Our analysis showed that the incidence of SAP among acute ischemic stroke patients was 32.4%, which is comparable to the reports issued by another centre in Egypt “Alexandria Main University Hospital” (37.1%) [15], and some other developing countries such as Northwest Ethiopia (36%) [16], Zambia (30%) [17]. However, the incidence rate of SAP was much lower in stroke centres in developed countries, including the United Kingdom (13.2%) [18], France (8.6%) [19], and Austria (5.2%) [20]. The wide variability in the reported incidence across studies might be attributed to differences in study designs, eligibility criteria, criteria used to define pneumonia, and duration of follow-up.
Gram-negative bacteria were identified in 81.7% of pneumonia cases, while Gram-positive bacteria were detected in 18.3%, with a predominance of K. pneumoniae (40.2%) followed by P. aeruginosa (20.7%), staphylococcus aureus (14.2%) then Acinetobacter spp (10.7%). The frequency of causative pathogens reported here aligns with a systemic review evaluating 7968 patients with SAP in which K. pneumonia was also the most commonly isolated organism (12.8%), followed by E. coli (9%), S. aureus (10.1%), then P. aeruginosa (6%) [7]. It is worth noting that the results of isolated organisms in SAP cases were more similar to the results of positive cultures of hospital-acquired pneumonia (HAP) than those of community-acquired pneumonia (CAP) [21].
Bulbar dysfunction and mechanical ventilation have already been reported in previous studies to be associated with an increased risk of SAP [3, 4, 22], which aligns with current findings. In bulbar dysfunction, fluid entry into the bronchi and alveolar spaces provokes an infectious process mediated by proinflammatory cytokines release [23]. On the other hand, the endotracheal tube may impair the mucociliary clearance, increasing the susceptibility to SAP. Moreover, mechanical ventilation may prolong hospital stays, increasing patients’ exposure to the bacterial environment [24, 25].
Previous studies have not unanimously agreed upon the finding in our study that previous history of TIA/stroke could predict SAP; some have confirmed [26, 27], while others have opposed it [22, 28]. However, previous TIA/stroke was incorporated in the integer-based pneumonia risk (ISAN), a scale established by CJ Smith et. [29].
Our findings confirm previous studies that SAP was associated with higher mortality than stroke patients without SAP. Yet, the overall rate of 30-day mortality in this study (6.5%) is less than the rates reported by other registries among acute ischemic stroke patients with SAP; 19.0% in the UK [30] and 39.5% in Canada [31].
In light of the current findings, we look forward to conducting a study aimed at external validation of widely used predictive scores of SAP such as ISAN, A2DS2, and acute ischemic stroke-associated pneumonia score (AIS-APS), as has been done in different countries [32,33,34].
Future research directions should implement and evaluate the effectiveness of a standard care service for the prevention and early treatment of SAP that ultimately reduces mortality. Indeed, a Chinese hospital adopted an infection control project, including screening for dysphagia, feeding adjustment, care of the oral cavity, airway management, and nursing qualifications. The results were impressive as the rate of SAP declined to 14.0% after a baseline rate of 37.2% [35], an encouraging experience that seems worth replicating at our centre.
Although this study showed the experience of a single center with a high volume of patients with a detailed description of the main pathogens related to SAP, the generalizability of the findings would be limited. Also, it is a retrospective analysis of patient records, and thus, the data were largely dependent on precise documentation. Other limitations include the short follow-up period and the small number of patients regarding certain variables such as history of combined previous stroke/TIA. The effect of SAP on long-term functional outcomes waited to be answered by future studies.
Conclusion
In our centre, 32.4% of patients with acute ischemic stroke developed SAP, adversely affecting mortality outcomes. Bulbar dysfunction, mechanical ventilation use, and previous history of TIA/stroke could predict the occurrence of SAP. A better understanding of predictors of the occurrence of SAP helps improve the prevention and control of SAP and reduce the mortality rate of patients with acute ischemic stroke.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Chen Y, Yang H, Wei H, Chen Y, Lan M. Stroke-associated pneumonia: a bibliometric analysis of worldwide trends from 2003 to 2020. 2021;100 38:e27321; https://doi.org/10.1097/md.0000000000027321.
Teh WH, Smith CJ, Barlas RS, Wood AD, Bettencourt-Silva JH, Clark AB, et al. Impact of stroke-associated pneumonia on mortality, length of hospitalization, and functional outcome. Acta Neurol Scand. 2018;138 4:293–300. https://doi.org/10.1111/ane.12956.
Hoffmann S, Harms H, Ulm L, Nabavi D, Mackert B-M, Schmehl I, et al. Stroke-induced immunodepression and dysphagia independently predict stroke-associated pneumonia – the PREDICT study. J Cereb Blood Flow Metabolism. 2016;37:0271678X16671964. https://doi.org/10.1177/0271678X16671964.
Li Y-m, Zhao L, Liu Y-g, Lu Y, Yao J-z, Li C-j, et al. Novel predictors of Stroke-Associated Pneumonia: a single Center Analysis. Front Neurol. 2022;13. https://doi.org/10.3389/fneur.2022.857420.
Zhao J, Li LQ, Zhen NX, Du LL, Shan H, Yu Y, et al. Microbiology and outcomes of Institutionalized patients with Stroke-Associated Pneumonia: an Observational Cohort Study. Front Microbiol. 2021;12:720051. https://doi.org/10.3389/fmicb.2021.720051.
Grossmann I, Rodriguez K, Soni M, Joshi PK, Patel SC, Shreya D, et al. Stroke and pneumonia: mechanisms, risk factors, management, and Prevention. Cureus. 2021;13 11:e19912. https://doi.org/10.7759/cureus.19912.
Kishore AK, Vail A, Jeans AR, Chamorro A, Di Napoli M, Kalra L, et al. Microbiological etiologies of Pneumonia complicating stroke: a systematic review. Stroke. 2018;49 7:1602–9. https://doi.org/10.1161/strokeaha.117.020250.
Hakansson AP, Orihuela CJ, Bogaert D. Bacterial-host interactions: physiology and pathophysiology of respiratory infection. Physiol Rev. 2018;98 2:781–811. https://doi.org/10.1152/physrev.00040.2016.
Smith CJ, Kishore AK, Vail A, Chamorro A, Garau J, Hopkins SJ, et al. Diagnosis of Stroke-Associated Pneumonia. Stroke. 2015;46 8:2335–40. https://doi.org/10.1161/STROKEAHA.115.009617.
Adams HP Jr., Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41. https://doi.org/10.1161/01.str.24.1.35.
Hussein HM, Abdel Moneim A, Emara T, Abd-Elhamid YA, Salem HH, Abd-Allah F, et al. Arabic cross cultural adaptation and validation of the National Institutes of Health Stroke Scale. J Neurol Sci. 2015;357(1–2):152–6. https://doi.org/10.1016/j.jns.2015.07.022.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet (London England). 1974;2 7872:81–4. https://doi.org/10.1016/s0140-6736(74)91639-0.
DePippo KL, Holas MA, Reding MJ. Validation of the 3-oz water swallow test for aspiration following stroke. Arch Neurol. 1992;49 12:1259–61. https://doi.org/10.1001/archneur.1992.00530360057018.
Elhasin H, Szolics M, Hassan A, Soliman N, Kaasch A. Risk scores for predicting stroke associated pneumonia: validity of A2DS2 and ISAN scores. J Neurol Sci. 2019;405:41–2. https://doi.org/10.1016/j.jns.2019.10.501.
Helmy TA, Abd-Elhady MA, Abdou M. Prediction of ischemic stroke-Associated Pneumonia: a comparison between 3 scores. J Stroke Cerebrovasc Diseases: Official J Natl Stroke Association. 2016;25 11:2756–61. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.07.030.
Assefa M, Tadesse A, Adane A, Yimer M, Tadesse M. Factors associated with stroke associated pneumonia among adult stroke patients admitted to university of Gondar hospital, Northwest Ethiopia. Sci Rep. 2022;12(1:12724). https://doi.org/10.1038/s41598-022-14656-2.
Prust ML, Nutakki A. Aspiration pneumonia in adults hospitalized with stroke at a large Academic Hospital in Zambia. 2021;11 6:e840–7; https://doi.org/10.1212/cpj.0000000000001111.
Ali AN, Howe J, Majid A, Redgrave J, Pownall S, Abdelhafiz AH. The economic cost of stroke-associated pneumonia in a UK setting. Top Stroke Rehabil. 2018;25 3:214–23. https://doi.org/10.1080/10749357.2017.1398482.
Cugy E, Sibon I. Stroke-Associated Pneumonia Risk score: validity in a French stroke unit. J Stroke Cerebrovasc Diseases: Official J Natl Stroke Association. 2017;26 1:225–9. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.09.015.
Matz K, Seyfang L, Dachenhausen A, Teuschl Y, Tuomilehto J, Brainin M. Post-stroke pneumonia at the stroke unit - a registry based analysis of contributing and protective factors. BMC Neurol. 2016;16:107. https://doi.org/10.1186/s12883-016-0627-y.
Feng DY, Zhou YQ, Zou XL, Zhou M, Zhu JX, Wang YH, et al. Differences in microbial etiology between hospital-acquired pneumonia and ventilator-associated pneumonia: a single-center retrospective study in Guang Zhou. Infect drug Resist. 2019;12:993–1000. https://doi.org/10.2147/idr.s204671.
Chaves MAL, Gittins M, Bray B, Vail A, Smith CJ. Variation of stroke-associated pneumonia in stroke units across England and Wales: a registry-based cohort study. Int J Stroke. 2021;17(2):155–62. https://doi.org/10.1177/17474930211006297.
Dai Y, Qiao J. Exploring the influence of Dysphagia and Tracheostomy on Pneumonia in patients with stroke: a retrospective cohort study. 2022;12 12; https://doi.org/10.3390/brainsci12121664.
Coppadoro A, Bittner E, Berra L. Novel preventive strategies for ventilator-associated pneumonia. Crit Care. 2012;16 2:210. https://doi.org/10.1186/cc11225.
Wu D, Wu C, Zhang S, Zhong Y. Risk factors of Ventilator-Associated Pneumonia in critically III patients. Front Pharmacol. 2019;10:482. https://doi.org/10.3389/fphar.2019.00482.
Wästfelt M, Cao Y, Ström JO. Predictors of post-stroke fever and infections: a systematic review and meta-analysis. BMC Neurol. 2018;18(1:49). https://doi.org/10.1186/s12883-018-1046-z.
Zhang R, Ji R, Pan Y, Jiang Y, Liu G, Wang Y, et al. J stroke Cerebrovasc diseases: official J Natl Stroke Association. 2017;26 5:938–43. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.10.043. External Validation of the Prestroke Independence, Sex, Age, National Institutes of Health Stroke Scale Score for Predicting Pneumonia After Stroke Using Data From the China National Stroke Registry.
Huang GQ, Lin YT, Wu YM. Individualized prediction of Stroke-Associated Pneumonia for patients with Acute ischemic stroke. 2019;14:1951–62; https://doi.org/10.2147/cia.s225039.
Smith CJ, Bray BD, Hoffman A, Meisel A, Heuschmann PU, Wolfe CD, et al. Can a novel clinical risk score improve pneumonia prediction in acute stroke care? A UK multicenter cohort study. J Am Heart Association. 2015;4(1):e001307. https://doi.org/10.1161/jaha.114.001307.
Tinker RJ, Smith CJ, Heal C, Bettencourt-Silva JH, Metcalf AK, Potter JF, et al. Predictors of mortality and disability in stroke-associated pneumonia. Acta Neurol Belgica. 2021;121(2):379–85. https://doi.org/10.1007/s13760-019-01148-w.
Finlayson O, Kapral M, Hall R, Asllani E, Selchen D, Saposnik G. Risk factors, inpatient care, and outcomes of pneumonia after ischemic stroke. Neurology. 2011;77 14:1338–45. https://doi.org/10.1212/WNL.0b013e31823152b1.
Zapata-Arriaza E, Moniche F, Blanca PG, Bustamante A, Escudero-Martínez I, Uclés O, et al. External validation of the ISAN, A2DS2, and AIS-APS scores for Predicting Stroke-Associated Pneumonia. J Stroke Cerebrovasc Diseases: Official J Natl Stroke Association. 2018;27 3:673–6. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.09.059.
Papavasileiou V, Milionis H, Smith CJ, Makaritsis K, Bray BD, Michel P, et al. External validation of the Prestroke Independence, Sex, Age, National Institutes of Health Stroke Scale (ISAN) score for Predicting Stroke-Associated Pneumonia in the Athens Stroke Registry. J Stroke Cerebrovasc Diseases: Official J Natl Stroke Association. 2015;24 11:2619–24. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.07.017.
Kishore AK, Vail A, Bray BD, Chamorro A, Napoli MD, Kalra L, et al. Clinical risk scores for predicting stroke-associated pneumonia: a systematic review. Eur Stroke J. 2016;1 2:76–84. https://doi.org/10.1177/2396987316651759.
Liu Z-Y, Wei L, Ye R-C, Chen J, Nie D, Zhang G, et al. Reducing the incidence of stroke-associated pneumonia: an evidence-based practice. BMC Neurol. 2022;22(1:297). https://doi.org/10.1186/s12883-022-02826-8.
Acknowledgements
Not applicable.
Funding
The authors extend their appreciation to the Deanship of Research and Graduate Studies at King Khalid University for funding this work through Large Research Project under grant number RGP2/391/45.
Author information
Authors and Affiliations
Contributions
Alshaimaa M. Aboulfotooh contributed to conceptualization, methodology, data collection and interpretation and helped in writing the manuscript draft; Heba Sherif Abdel Aziz contributed to conceptualization, methodology, data collection and interpretation and helped in writing the manuscript draft; Marwa M. Zein contributed to methodology, data analysis and interpretation and helped in writing the manuscript draft; Mohamed Sayed contributed to methodology, data collection and interpretation and helped in writing the manuscript draft; Ahmed R. N. Ibrahim contributed to data collection and interpretation. Lamiaa N Abdelaty contributed to data collection and interpretation. Rehab Magdy contributed to conceptualization, methodology, data collection and interpretation and helped in writing the manuscript draft. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethical approval was granted by the ethical committee at Kasr Alainy Faculty of Medicine-Cairo University (N-135-2023) following the Helsinki Declaration with a waiver of informed consent from all subjects due to the retrospective nature of the study.
Consent to participate
Waiver of informed consent, which was waived to the Ethical Committee of Kasr El Aini Faculty of Medicine - Cairo University, was obtained from all subjects and/or their legal guardian.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Aboulfotooh, A.M., Aziz, H.S.A., Zein, M.M. et al. Bacterial stroke-associated pneumonia: microbiological analysis and mortality outcome. BMC Neurol 24, 265 (2024). https://doi.org/10.1186/s12883-024-03755-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-024-03755-4