Abstract
Objective
The optimal blood pressure (BP) targets for acute ischemic stroke are unclear. We aimed to assess the relationship between Mean BP and clinical outcomes during hospitalization.
Materials and methods
We included 649 patients with Acute ischemic stroke (AIS) from December 2020 to July 2021. BP was measured daily, and mean blood pressure was calculated. Clinical events recorded within 90 days of randomization were: recurrent ischemic stroke, symptomatic intracranial hemorrhage, and death. The modified Rankin Scale (mRS) was used to measure primary outcomes 3 months after AIS. Logistic multiple regression analysis was performed by statistical software R.
Result
There is a nonlinear U-shaped relationship between SBP and poor outcomes. This means higher SBP and lower SBP will increase the incidence of poor outcomes. The optimal mean SBP during hospitalization was 135-150 mmHg, and patients with SBP < 135mmhg OR 2.4 [95% Cl, (1.16 ~ 4.97)], P = 0.018; and > 150mmhg OR 2.04 [95% Cl, 1.02 ~ 4.08], p = 0.045 had a higher probability of poor outcomes.
Conclusion
Our study shows that the optimal SBP of patients with AIS during hospitalization was 135-150 mmHg. The findings suggest that the relationship between mean SBP and 3-month functional outcome after AIS was U-shaped. Both higher SBP and lower SBP lead to poor prognosis in AIS patients.
Similar content being viewed by others
Introduction
Elevated blood pressure is common in the acute phase of stroke [1, 2], possibly as a compensatory mechanism to increase blood flow to the ischemic area [3]. BP control in the acute phase is an important factor affecting AIS patients’ clinical outcomes. However, it is generally believed that BP should not be excessively controlled in the acute stage of AIS as low BP may lead to ischemic tissue hypoperfusion [4, 5]. Poststroke hypotension is associated with different factors depending on stroke subtypes, such as cardioembolic stroke, which may be attributable to related heart failure [6], lacunar events attributable to coronary heart disease [6], and partial anterior circulation infarction attributable to previous myocardial infarction [7]. In addition, the stroke itself may cause damage to important vasomotor control centers (such as the hypothalamus and cortical vasomotor centers), particularly the right insular cortex, resulting in dysrhythmias, all potentially contributing to low BP [8]. Current guidelines about the management of poststroke hypotension provide no objective clarification on appropriate management, which is a reflection of the paucity of evidence in this field, and an indicator of the practical difficulties of carrying out research in the setting of acute stroke [9]. Therefore, some studies also support pressor therapy in response to acute hypotension [9]. However, increased BP during acute ischemic stroke may improve cerebral perfusion of ischemic tissue or may aggravate edema and hemorrhagic transformation of ischemic tissue [10]. Thus, it is important to raise blood pressure in an appropriate range. Both high and low blood pressure are independent predictors of poor outcomes. These associations appear to be partly mediated by higher rates of early recurrence and death in patients with high blood pressure and higher coronary heart disease events rates in those with low blood pressure [1].
At present, the blood pressure (BP) level that should be maintained in patients with AIS to ensure the best outcome is not known [11]. Therefore, ideal management in these situations should be individualized. Different subgroups of patients may need to have their BP lowered (e.g., before or after thrombolysis), left alone, or elevated [12].
Various studies have observed a U-shaped relationship between BP and clinical outcomes in many patients with ischemic stroke [1, 13,14,15]. Both extremes of BP were associated with poorer outcomes, although the reported optimal SBP varied widely from 120 to 130 mmHg [13, 14] to 156 to 220 mmHg in additional studies [16]. A J-shaped relationship between SBP and adverse outcomes has also been reported, whereas low SBP was not associated with functional outcomes [1, 17]. Because of these uncertainties, BP management during the acute stage of ischemic stroke remains an unresolved and controversial issue. The optimal blood pressure level to maintain in patients with AIS is unknown [11, 18]. Few studies have reported taking the mean blood pressure of AIS patients during hospitalization as the research object and comparing other BP values. The mean BP summarizes the overall level of BP of AIS patients during admission, which is an objective and stable value. We aimed to assess the relationship between mean BP and admission BP and clinical outcomes in patients with acute ischemic stroke.
Methods
We used data from the stroke center of Jiangsu Province Hospital of Chinese medicine from December 2020 to July 2021. An observational cohort study of 649 patients with ischemic stroke was conducted. Patients were enrolled if they (1) had AIS and were seen within 72 h of symptom onset; (2) had acute ischemic lesions on the brain imaging; (3) had BP measurements q4 hours in the first 24 hours and then q8 hours after that. Patients with terminal malignant tumors or other underlying diseases like severe renal disease and liver disease, who failed to follow up at 90 days after the onset of symptoms, who had an mRS score ≥ 3 before onset, or who were treated with reperfusion, got excluded.
Potential risk factors for stroke, including hypertension (BP ≥ 140/90 mmHg, or previously used antihypertensive drugs), diabetes mellitus (previously used hypoglycemic drugs or glycated hemoglobin > 6.5% at admission), dyslipidemia (previously used lipid-lowering drugs or LDL ≥ 4.1 mmol/L, triglyceride ≥2.3 mmol/lL), coronary artery disease, smoking history, etc., were assessed.
Measurement and management of BP
BP measurements were q4 h in the first 24 h and q8 h after that. Therefore, the mean value was calculated. BP was managed according to the Japanese Guidelines for Stroke Management [19, 20]. The mean blood pressure during the first 4 days of admission and from the fourth day of admission to discharge were evaluated. Data from BP measurements≥5 days were used to calculate the mean value in groups. After excluding patients hospitalized for less than 5 days, 649 patients were analyzed (Fig. 1).
Clinical assessment and outcome measurements
The severity of neurological deficit was assessed during admission using the National Institutes of Health Stroke Scale (NIHSS) score [21]. The primary outcome was measured using the modified Rankin Scale (mRS) 3 months after the onset of symptoms. Clinical information of the results after discharge was obtained through follow-up 3 months after the qualifying event. An mRS score of 0-2 was defined as a favorable outcome (functional independence). Scores≥3 were considered poor outcomes. Moreover, clinical events were recorded, such as recurrent ischemic stroke, symptomatic intracranial hemorrhage, and death [1, 22, 23].
Brain imaging examination (CT/MRI) was performed during admission. According to the Trial of Org 10,172 in Acute Stroke Treatment classification, clinical and neuroimaging findings were used to classify patients into five-stroke subtypes: (1) large-artery atherosclerosis, (2) small-vessel occlusion, (3) cardioembolism, (4) stroke of other determined etiology, and (5) stroke of undetermined etiology [24].
Statistical analysis
This study included 649 patients with AIS. BP was measured and entered into the database for all patients in the trial. Data are expressed as mean ± SD, IQR. Logistic regression analysis was used to determine the relationship between BP parameters (mean ± SD, IQR of SBP or DBP) and poor functional outcome.
The relationship between baseline BP and the functional prognosis was best fitted by smooth curve fitting, and reverse stepwise logistic regression analysis was used to evaluate the odds ratios (OR) and corresponding 95% confidence intervals (CIs) of the main results. BP was considered a continuous variable, and the optimal BP was determined by the dichotomous method based on threshold estimations for the main analysis. In addition, logistic regression analysis was performed to assess the optimal BP range [18]. All the analyses were performed using the statistical software R (http://www.R-project.org, The R Foundation) and Free Statistics software version 1.4 [25].
The primary outcome was the modified Rankin Scale (mRS) score at 90 days [26]. The mRS measures functional outcomes after stroke, ranging from 0 (no symptoms) to 6 (death). Scores ≥3 were defined as poor outcomes.
According to their clinical significance and the results of previous studies, the following variables were adjusted: age, sex, dyslipidemia, hypertension, diabetes mellitus, antihypertensive drugs, coronary heart disease, atrial fibrillation, and smoking. P-value < 0.05 was determined as the level of significance.
Result
Study population
Among 649 AIS patients during the study period, the median age was 69 (IQR 60-77) years, and 427 (65.8%) were male. In addition, 92 (14.18%) patients had poor outcomes, and 557 (85.82%) patients had good outcomes. mRS on admission was 2.0 (interquartile range, 1.0-3.0). Patients with poor outcomes were older than those with good outcomes. For patients with poor outcomes, more males than females, and more frequently have a medical history of diabetes or hypertension or use antihypertensive medication (Table 1).
BP grouping and clinical results
AIS patients with admission SBP and mean SBP and functional prognosis followed a ‘U-curve pattern’. Both extremes of BP were associated with poor outcomes. Although the correlation between SBP and the functional prognosis was significantly better than DBP, the correlation between DBP and prognosis was not statistically significant. The optimal range of mean blood pressure during hospitalization was between 135 mmHg and 150 mmHg.
Patients with mean SBP above 150 mmHg and below 135 mmHg had a higher median mRS score and more deaths at 90 days compared to patients with mean SBP between 135 and 150 mmHg (Fig. 2).
To elucidate whether mean BP during the acute stage days 1–4 after onset and days>4 was associated with functional outcome, Patients were divided into two groups according to daily BP. In the adjusted model, the nonlinear relationship between BP and functional results presented a symmetric U-shaped diagram (Figs. 3, 4, 5, 6). Day-by-day SBP during the acute 1-4 days and >4 days after onset was independently associated with a poor functional outcome, but DBP>4 days was not associated with a functional outcome. We evaluated according to the cut-points (135 mmHg) in the fitted curves (Fig. 3 and Table 2). Threshold effect analysis using piecewise linear regression (Table 2) showed that when BP was < 138 mmHg, the odds of outcomes negatively correlated with BP [OR 0.936 (0.882 ~ 0.992) p = 0.0258]. However, when the BP was > 135 mmHg, the incidence of poor outcomes increased with increasing SBP [OR 1.036 (1.008 ~ 1.066) p = 0.0125].
Sensitivity analysis
Both higher SBP and lower SBP lead to poor prognosis in AIS patients. In the following analysis, restricted cubic spline smoothing curve fitting was used to assess the relationship between BP and functional outcome, showing that SBP and functional results have a ‘U-curve pattern (Fig. 7).
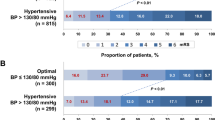
We used piecewise linear regression analysis according to the best range of fitting results (Table 3). Further confirm the range of mean systolic blood pressure. The piecewise linear regression showed that 135-150 mmHg is the best blood pressure range that can be determined in this study during hospitalization. Lower and higher blood pressures were significantly associated with functional outcomes. BP < 135 mmHg(OR 1.93 [95%Cl, OR 1.11-3.36], P = 0.021; After adjustment, OR 2.4 [95%Cl, 1.16-4.97], P = 0.018). And BP > 150 mmHg(OR 1.95 [95%Cl,1.12-3.37], P = 0.017; Adjusted OR 2.04 [95%CL, 1.02-4.08], P = 0.045) (Table 3).
Because there was significant discussion about antihypertensive therapy in the guidelines for post stroke therapy. We adjusted variable with and without antihypertensive therapy. we used logistic regression analysis to evaluate the blood pressure data at 10 mmHg interval with 135-145 mmHg as reference. The adjusted values showed the relationship between different blood pressure values and functional outcomes (Fig. 8), a significant increase in the probability of a poor functional outcome in patients with SBP < 135 mmHg or > 145 mmHg (vs. > 135 to ≤145 mmHg). The results indicate that either with or without antihypertensive treatment our conclusions are stable, lower and higher blood pressure are significantly associated with functional outcomes, which further confirmed our U-shaped curve.
Association of different mean systolic blood pressure levels with a 3-month functional outcome in all patients. A multiple logistic regression test was used to analyze odds ratios. CI, confidence interval. Adjusted variables: TOAST, antihypertensive drugs, atrial fibrillation, coronary heart disease, hypertension, diabetes, hyperlipidemia, age and gender
Discussion
This Retrospective study demonstrates that SBP is significantly correlated with the functional outcome of AIS. There was a nonlinear U-shaped relationship between the SBP level during hospitalization and the mRS scores at 3 months after AIS in these patients. Furthermore, comparing admission SBP, mean SBP during hospitalization correlated more with the functional outcome at 3 months after AIS in patients. Moreover, maintaining a mean SBP of 135-150 mmHg during hospitalization is associated with higher odds of a favorable outcome 3 months after AIS.
Some observational studies show an association between worse outcomes and lower BP, whereas others have not [1, 11, 14, 16]. Although in other reports, most studies targeted BP at admission or the mean BP measured within 24 or 72 h after the onset of symptoms [14,15,16], studies of overall mean BP during hospitalization are rare. Due to the patient’s personal reasons or other influencing factors, SBP at admission is difficult to control. Whether to take antihypertensive measures after admission also needs to consider various factors. We assume that the overall mean value of daily BP at a fixed time is more reliable as a long-term index than a random or a single BP value at a specific time point because it is less affected by various factors.
Taking the mean BP during hospitalization as the main research object is more stable and objective. Moreover, our study demonstrates that mean BP is more stable during hospitalization, and both low BP levels and high BP levels were associated with poor outcomes. Furthermore, SBP maintained between 135 and 150 may be optimal for AIS patients during hospitalization.
In the subgroups of this study, the mean BP in the acute (1-4 days after onset) and subacute (>4 days) stages were equally stable, and both were related to the functional outcome, but the difference was not significant.
In another study, BP during the subacute phase was significantly associated with functional outcomes after ischemic stroke, but there was no association between BP during the acute stage and functional outcome [27]. The results in the present study may be related to the widespread use of antihypertensive drugs in China. According to the latest guidelines, patients with AIS need emergency BP reduction to prevent serious complications [11]. However, excessive lowering of BP can sometimes aggravate cerebral ischemia [28]. Therefore, ideal BP management should be personalized. In this study, antihypertensive drugs were not classified but were adjusted in statistical analysis. The impact of antihypertensive drug use on outcomes has been reflected in the adjusted model.
The change in BP is affected by many factors, including increased sympathetic drive, reduced arterial and cardiopulmonary reflexes, impaired arterial compliance, humoral factors, blood viscosity, and emotional factors [29, 30]. Sykora et al. [31] hypothesized that autonomic dysfunction in AIS patients might have unfavorable effects on outcomes through secondary brain injury caused by cerebral hypoperfusion, impaired brain autoregulation, and cardiovascular complications. These conditions may exacerbate cerebral ischemia or hinder recovery, leading to poor functional outcomes after AIS [27]. Further studies are needed to elucidate the association mechanism between blood pressure changes and post-stroke functional outcomes.
A potential limitation of this study is a single-center study with a small number of samples, which may lead to an underestimation of the true association. Furthermore, the study is retrospective, and the recorded data may be incomplete. Patients with short hospital stays and fewer blood pressure measurements were excluded, resulting in potential selection bias. Furthermore, unidentified confounders may not be adjusted, and the data must be interpreted cautiously. Further studies are required to elucidate the mechanism and clinical significance of the relationship between mean blood pressure and functional outcome in patients with acute ischemic stroke during hospitalization.
Conclusion
The result of the present study indicates that maintenance of mean BP between 135 mmHg and 150 mmHg in AIS patients during hospitalization is associated with promising short- or long-term clinical outcomes. These findings have significant potential implications for managing BP in acute stroke, as they support the need to initiate treatment for high BP early rather than conservatively delaying therapy to a certain point after symptom onset. The overall BP stability has a more objective value than the fixed time.
Availability of data and materials
All data are available from the corresponding author upon reasonable request.
References
Leonardi-Bee J, Bath PM, Phillips SJ, Sandercock PA. Blood pressure and clinical outcomes in the international stroke trial. Stroke. 2002;33:1315–20. https://doi.org/10.1161/01.str.0000014509.11540.66.
Qureshi AI, et al. Prevalence of elevated blood pressure in 563,704 adult patients with stroke presenting to the ED in the United States. Am J Emerg Med. 2007;25:32–8. https://doi.org/10.1016/j.ajem.2006.07.008.
Regenhardt RW, et al. Blood pressure and penumbral sustenance in stroke from large vessel occlusion. Front Neurol. 2017;8:317. https://doi.org/10.3389/fneur.2017.00317.
Qureshi AI. Acute hypertensive response in patients with stroke: pathophysiology and management. Circulation. 2008;118:176–87. https://doi.org/10.1161/circulationaha.107.723874.
Alqadri SL, Sreenivasan V, Qureshi AI. Acute hypertensive response management in patients with acute stroke. Curr Cardiol Rep. 2013;15:426. https://doi.org/10.1007/s11886-013-0426-7.
Vemmos KN, et al. Factors influencing acute blood pressure values in stroke subtypes. J Hum Hypertens. 2004;18:253–9. https://doi.org/10.1038/sj.jhh.1001662.
Aslanyan S, Fazekas F, Weir CJ, Horner S, Lees KR. Effect of blood pressure during the acute period of ischemic stroke on stroke outcome: a tertiary analysis of the GAIN international trial. Stroke. 2003;34:2420–5. https://doi.org/10.1161/01.Str.0000091233.04524.0c.
Colivicchi F, Bassi A, Santini M, Caltagirone C. Prognostic implications of right-sided insular damage, cardiac autonomic derangement, and arrhythmias after acute ischemic stroke. Stroke. 2005;36:1710–5. https://doi.org/10.1161/01.STR.0000173400.19346.bd.
Mistri AK, Robinson TG, Potter JF. Pressor therapy in acute ischemic stroke: systematic review. Stroke. 2006;37:1565–71. https://doi.org/10.1161/01.Str.0000222002.57530.05.
Weiss A, Beloosesky Y, Kenett RS, Grossman E. Systolic blood pressure during acute stroke is associated with functional status and long-term mortality in the elderly. Stroke. 2013;44:2434–40. https://doi.org/10.1161/strokeaha.113.001894.
Powers WJ, et al. Guidelines for the early Management of Patients with Acute Ischemic Stroke: 2019 update to the 2018 guidelines for the early Management of Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:e344–418. https://doi.org/10.1161/str.0000000000000211.
Gąsecki D, Kwarciany M, Kowalczyk K, Narkiewicz K, Karaszewski B. Blood pressure Management in Acute Ischemic Stroke. Curr Hypertens Rep. 2020;23:3. https://doi.org/10.1007/s11906-020-01120-7.
Mulder M, et al. Baseline blood pressure effect on the benefit and safety of intra-arterial treatment in MR CLEAN (multicenter randomized clinical trial of endovascular treatment of acute ischemic stroke in the Netherlands). Stroke. 2017;48:1869–76. https://doi.org/10.1161/strokeaha.116.016225.
Vemmos KN, et al. U-shaped relationship between mortality and admission blood pressure in patients with acute stroke. J Intern Med. 2004;255:257–65. https://doi.org/10.1046/j.1365-2796.2003.01291.x.
Bangalore S, et al. Blood pressure and in-hospital outcomes in patients presenting with ischaemic stroke. Eur Heart J. 2017;38:2827–35. https://doi.org/10.1093/eurheartj/ehx330.
Stead LG, Gilmore RM, Decker WW, Weaver AL, Brown RD Jr. Initial emergency department blood pressure as predictor of survival after acute ischemic stroke. Neurology. 2005;65:1179–83. https://doi.org/10.1212/01.wnl.0000180939.24845.22.
Maïer B, et al. Mortality and disability according to baseline blood pressure in acute ischemic stroke patients treated by Thrombectomy: a collaborative pooled analysis. J Am Heart Assoc. 2017;6 https://doi.org/10.1161/jaha.117.006484.
Vitt JR, Trillanes M, Hemphill JC 3rd. Management of blood pressure during and after recanalization therapy for acute ischemic stroke. Front Neurol. 2019;10:138. https://doi.org/10.3389/fneur.2019.00138.
Shinohara Y, et al. II. Cerebral infarction/transient ischemic attack (TIA). J Stroke Cerebrovasc Dis. 2011;20:S31–73. https://doi.org/10.1016/j.jstrokecerebrovasdis.2011.05.004.
Shinohara Y, Yamaguchi T. Outline of the Japanese guidelines for the Management of Stroke 2004 and subsequent revision. Int J Stroke. 2008;3:55–62. https://doi.org/10.1111/j.1747-4949.2008.00178.x.
Brott T, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20:864–70. https://doi.org/10.1161/01.str.20.7.864.
Bonita R, Beaglehole R. Recovery of motor function after stroke. Stroke. 1988;19:1497–500. https://doi.org/10.1161/01.str.19.12.1497.
Angelini F, et al. Comparison of antithrombotic strategies in patients with cryptogenic stroke and patent foramen ovale: an updated meta-analysis. Cardiovasc Drugs Ther. 2021;35:987–93. https://doi.org/10.1007/s10557-020-07068-9.
Adams HP Jr, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of org 10172 in acute stroke treatment. Stroke. 1993;24:35–41. https://doi.org/10.1161/01.str.24.1.35.
Yang Q, et al. Association between preadmission metformin use and outcomes in intensive care unit patients with Sepsis and type 2 diabetes: a cohort study. Front Med. 2021;8:640785. https://doi.org/10.3389/fmed.2021.640785.
Bamford JM, Sandercock PA, Warlow CP, Slattery J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1989;20:828. https://doi.org/10.1161/01.str.20.6.828.
Fukuda K, et al. Day-by-day blood pressure variability and functional outcome after acute ischemic stroke: Fukuoka stroke registry. Stroke. 2015;46:1832–9. https://doi.org/10.1161/strokeaha.115.009076.
Stead LG, et al. Impact of acute blood pressure variability on ischemic stroke outcome. Neurology. 2006;66:1878–81. https://doi.org/10.1212/01.wnl.0000219628.78513.b5.
Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 2013;10:143–55. https://doi.org/10.1038/nrcardio.2013.1.
Stergiou GS, et al. Blood pressure variability assessed by home measurements: a systematic review. Hypertens Res. 2014;37:565–72. https://doi.org/10.1038/hr.2014.2.
Sykora M, Diedler J, Turcani P, Hacke W, Steiner T. Baroreflex: a new therapeutic target in human stroke? Stroke. 2009;40:e678–82. https://doi.org/10.1161/strokeaha.109.565838.
Acknowledgments
We acknowledge Prof. Minghua Wu, Dr. Yuan Zhu and Dr. Zhaoyao Chen for their advice. We appreciate Yangjingyi Xia MD, Tianrui Zhang MD, and Qinghua Feng MD for their help in the collection of raw data.
Funding
This work was supported by National Administration of Traditional Chinese Medicine: Evidence-Based Capacity Building Project (2019XZZX-NB007), National Natural Science Foundation of China (Grant No. 82274428 , 81973794), National Natural Science Foundation of China (Grant No. 81973794), Jiangsu Province Administration of Chinese Medicine (ZT202102). The Youth Fund of Jiangsu Natural Science Foundation (BK20201095).
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit it to the current journal; gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All experiments were performed in accordance with the Declaration of Helsinki guidelines and regulations. The study was approved by the Institutional Review Board of Aftiliated Hospital of Nanjing University of Chinese Medicine (Jiangsu Province Hospital of Chinese Medicine).
Approval number: [2017NL-012-01].
This is a retrospective study and does not require written informed consent. The need for written informed consent was waived by the Institutional review board of [Aftiliated Hospital of Nanjing University of Chinese Medicine(Jiangsu Province Hospital of Chinese Medicine)].
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare. The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Relationship Between >4d SBP and functional outcome. Table S2. Relationship Between mean SBP and functional outcome. Table S3. Relationship Between admission SBP and functional outcome. Table S4. Relationship between admission SBP and functional outcome indifferent models. Fig. S1. Relationship between mean DBP and functional outcome according to smooth fitting curve. Adjusting variables: TOAST, antihypertensive drugs, atrial fibrillation, coronary heart disease, hypertension, diabetes, hyperlipidemia, age, and gender. Fig. S2. Relationship between Admission SBP and functional outcome according to smooth fitting curve. Adjusting variables: TOAST, antihypertensive drugs, atrial fibrillation, coronary heart disease, hypertension, diabetes, hyperlipidemia, age, and gender.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hu, M., Zhu, Y., Chen, Z. et al. Relationship between mean blood pressure during hospitalization and clinical outcome after acute ischemic stroke. BMC Neurol 23, 156 (2023). https://doi.org/10.1186/s12883-023-03209-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-023-03209-3