Abstract
Background
Currently, there are several studies showing that wearable inertial sensors are highly sensitive in the detection of gait disturbances in people with multiple sclerosis (PwMS), showing excellent reliability within one or 7–14 days. However, it is not known how stable these gait parameters remain over a longer period of time. This is surprising, because many treatments last longer than two weeks. Thus, the purpose of the current study was to examine gait parameters obtained by means of wearable inertial sensors during a 6-min walk and to reassess these parameters after a period of one year.
Methods
Fifty PwMS (without a relapse or a recent change in the Expanded Disability Status Scale (EDSS) or treatment) and 20 healthy participants were examined at two assessment points (interval between assessments: 14.4 ± 6.6 months). At each assessment point, all participants had to complete a 6-min walking test, an observer-rater test (Berg Balance Scale, BBS) and a Timed-up and Go Test (TUG). To measure mean gait parameters (i.e. walking speed, stride length, stride time, the duration of the stance and swing phase and minimum toe-to-floor distance), as well as the intraindividual standard deviation of each mean gait parameter, wearable inertial sensors were utilized.
Results
We found that even after one year all mean gait parameters showed excellent Intraclass Correlation Coefficients (ICC between 0.75 and 0.95) in PwMS. Looking at MS subgroups, the ICCs were slightly higher in MS subgroup 2 (EDSS 2.0–5.0) than those in MS subgroup 1 (EDSS 0.0–1.5) and healthy controls. Compared to the mean gait parameters, parameters of gait variability showed only good-to-fair ICC values in PwMS. Concerning BBS and TUG, the ICC values after one year were close to the ICC values of the measured mean gait parameters.
Conclusions
Due to the excellent stability of mean gait parameters after one year, these sensor-based gait parameters can be identified as clinically relevant markers to evaluate treatment effects over a longer (several months) period of time in MS.
Similar content being viewed by others
Background
Multiple sclerosis (MS) is a progressive chronic inflammatory disease with a variety of clinical symptoms that results in multiple neurological deficits with a major effect on balance control and walking ability (e.g., [1,2,3,4,5,6,7,8,9]). Moreover, around 40% of people with MS (PwMS) report walking problems that unfavorably affect their quality of life [10]. In order to improve PwMS's quality of life, early detection of gait deficits is crucial.
Currently, a few studies explored the potential value of wearable inertial sensors in the detection of gait deficits in PwMS (e.g., [8, 9, 11, 12]). This is striking, as the sensors could potentially be utilized to conduct automatic and standardized assessments to objectively identify walking deficits and monitor walking performance in PwMS [13]. However, there are several studies showing that wearable inertial sensors are highly sensitive in the detection of gait disturbances in MS, even in early MS, where global scales such as the Expanded Disability Status Scale (EDSS) do not provide specific clinical information about deviations in gait behavior (e.g., [8, 9, 11, 12]). Even though the EDSS remains the most common measure of functional disability in MS, it only provides relatively superficial information on walking capacity. For example, on its scale from 1.0 to 10, a value of 4.0 implies that walking of at least 500 m without support or rest is possible, which then decreases with higher EDSS values [14].
Additionally, wearable inertial sensors show good reliability within one or 7–14 days during short (e.g. 25-foot walk, 10-m test) and prolonged distances (e.g. 2-min and 6-min walk test). For example, Flachenecker et al. [12] investigated the correlation coefficient between consecutive 25-foot walking tests (two times at a self-selected speed, followed by two times at a speed as fast as possible) in 102 PwMS and 22 healthy controls and found high reliability (r = 0.9) for the mean gait parameters for both self-selected and fast walking speeds. In another study, 57 PwMS and 24 healthy controls were asked to walk back and forth a 10-m distance for six minutes at their comfortable speed [11]. The authors repeated the assessment on a second visit, which was held 7–14 days after the first one and found that the higher the EDSS score, the more the reliability was increased. These results obtained by means of wearable inertial sensors are comparable to previously reported test–retest analyses of a 6-min walk using a stop-watch [3] or an electronic walkway [15].
The studies mentioned above show excellent reliability within one or 7–14 days. However, it is not known how stable these objective sensor-based gait parameters remain over a longer period of time. We hypothesized that gait analysis after a longer period of time would reveal changes in gait parameters, especially in more disabled PwMS. Thus, the purpose of the current study was to examine gait parameters obtained by means of wearable inertial sensors during a 6-min walk and to reassess these parameters after a period of one year in PwMS.
Methods
Participants
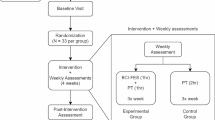
Fifty PwMS and 20 healthy participants were recruited sequentially in the outpatient clinic of the Department of Neurology, Klinikum Bayreuth GmbH, Medical Campus Upper Frankonia, Germany (Table 1). PwMS were eligible to participate in case of a verified MS diagnosis [16], stable symptoms between both assessment points performed one year apart (i.e. no relapse and no treatment or EDSS change), an age between 18–65 years and the ability to walk without a walking aid for six minutes. PwMS were not included in case of a relapse or a treatment or EDSS change between both assessment points. All participants provided written informed consent. The study was approved by the ethical review board of the Friedrich Schiller University Jena, Germany (2018–1221-BO) and was in accordance with the Declaration of Helsinki.
Measurements
Participants were examined at two assessment points during routine clinical appointments in the Klinikum Bayreuth GmbH, Department of Neurology (interval between assessments: 14.4 ± 6.6 months). Out of the 50 PwMS, six experienced a relapse between assessments. Since a relapse potentially affects gait, and since six participants are too less to be analyzed as a subgroup, the datasets of these participants were excluded from the further analysis focusing on stability. EDSS values in PwMS remained identical across the two assessments.
At each assessment point, both PwMS and healthy participants had to complete a walking test that required them to cover a distance of 25 feet repeatedly throughout a period of six minutes as enduring and fast as possible (6-min walk). A cone was placed three feet away from each endpoint of the 25-foot distance and participants circled the cones to make their turn back toward the 25-foot distance [6, 8, 9]. To measure gait parameters (i.e. walking speed, stride length, stride duration, the duration of the stance and swing phase as well as the minimum toe-to-floor distance), wearable inertial sensors were utilized (MTw2, Xsens Technologies B.V.; sampling rate: 100 Hz). The sensors were attached to the forefoot of the participants’ dominant leg (i.e., the foot they would take to kick a ball; [9]). In addition to the walking test and gait parameter measures, an observer-rater test (Berg Balance Scale, BBS, [17]) and Timed-up and Go Test (TUG, [18]) were administered.
Data processing
To exclude effects of acceleration and deceleration the first and the last 25 feet distances, as well as the first and the last 2.5 m of each distance between the cones were excluded from the following analysis [8, 9]. We used a validated algorithm [19] to calculate mean gait parameters (i.e. walking speed, stride length, stride time, the duration of the stance, swing phase and minimum toe-to-floor distance), as well as the intraindividual standard deviation of each mean gait parameter as gait variability measures. Heel strikes and toe-off events were identified based on local minima of the angular velocity of the foot in the sagittal plane [20].
Statistical analysis
Statistical analyses were performed with SPSS 20 (Chicago, IL, USA). To test normality of distributions, Kolmogorov–Smirnov tests were implemented for all gait parameters (mean, standard deviation (SD)). Participant characteristics were compared using Pearson’s Chi-square for gender and independent t-Tests for age, height, weight and EDSS scores, separately for healthy controls, PwMS and both MS subgroups. MS subgroups (subgroup 1: EDSS 0.0–1.5, subgroup 2: EDSS 2.0–5.0) were established using a median split based on EDSS scores (e.g., [5]). Differences in mean gait parameters and gait variability (SD) between PwMS and healthy participants were assessed by a one-way between-subjects analysis of variance (factor GROUP with four levels: healthy controls, PwMS, MS subgroup 1, and MS sub-group 2) with Bonferroni post-hoc analysis. Stability was assessed using the calculation of Intraclass Correlation Coefficients (ICCs) with an ICC(2,1) model and 95% confidence intervals [21]. ICC values were interpreted as follows: > 0.75 was excellent, 0.60–0.74 was good, 0.40–0.59 was fair, < 0.40 was poor [22]. Furthermore, Bland–Altman analysis/ plots with 95% Limits of Agreement (LoA) for each measure were performed/ produced to assess the agreement of gait measures obtained in the two visits [23]. An alpha level of 0.05 was used for all statistical tests.
Results
Stability of mean gait parameters
Table 2 summarizes the ICC values with 95% CI and the bias with 95% LoA of the mean gait parameters for healthy controls and PwMS as well as for both MS subgroups. For healthy controls, five out of six gait parameters showed excellent and only one (minimum toe-to-floor distance) fair ICC values (Table 2). For PwMS, all six gait parameters showed excellent ICC values (Table 2). In MS subgroups, the ICCs were good-to-excellent in MS subgroup 1 and excellent in MS subgroup 2. On average, MS subgroup 2 had higher ICC values than MS subgroup 1. Bland–Altman plots (Fig. 1) revealed no systematic bias for all mean gait parameters.
Bland–Altman plots for mean gait parameters show the difference versus the mean of both measurements for all single measurements (assessment 1, assessment 2). The solid line indicates the bias and the dashed lines the Limits of Agreement (95% confidence interval of the bias) for healthy controls (grey) and PwMS (black). MTC: minimum toe-to-floor distance
Stability of gait variability parameters
The ICC values with 95% CI and the bias with 95% LoA of gait variability parameters for healthy controls and PwMS as well as for both MS subgroups were summarized in Table S1. For healthy controls, two out of six gait variability parameters showed good, one fair and three poor ICC values (Table S1). For PwMS, two out of six gait variability parameters showed good and four fair ICC values. In MS subgroups, the ICCs were poor-to-fair in MS subgroup 1 and fair-to-excellent in MS subgroup 2. On average, MS subgroup 2 had higher ICC values than MS subgroup 1. Bland–Altman plots (Figure S1) revealed no systematic bias for all gait variability parameters.
Stability of observer rater and Timed-up and Go Test
Concerning observer-rater test (BBS) and TUG, the ICC of the TUG was good for healthy controls and MS subgroup 2 and excellent for PwMS and MS subgroup 1 (Table 3). The ICC of the BBS was excellent for PwMS and both MS subgroups (Table 3). For healthy controls, the ICC was not calculated due to zero variance. Bland–Altman plots (Fig. 2) and analysis (Table 3) showed a bias between 0.079 (MS subgroup 2) and 0.4 (healthy controls) for TUG and a bias between 0.065 (MS subgroup 1) and 0.238 (MS subgroup 2) for BBS.
Bland–Altman plots for observer-rater test (Berg Balance Scale, BBS) and Timed-up and Go Test (TUG) show the difference versus the mean of both measurements for all single measurements (assessment 1, assessment 2). The solid line indicates the bias and the dashed lines the Limits of Agreement (95% confidence interval of the bias) for healthy controls (grey) and PwMS (black)
Discussion
Stability of sensor-based gait parameters reassessed after one year
The primary aim of the current study was to determine the stability of several gait parameters obtained by means of wearable inertial sensors (i.e. walking speed, stride length, stride time, the duration of the stance and swing phase as well as the minimum toe-to-floor distance) during a 6-min walk after one year in PwMS. We found that even after 12 months all mean gait parameters were stable in PwMS (ICC between 0.75 and 0.95; Table 2) and that the ICC values were close to the previously reported ICC values within one or 7–14 days measured by a stop-watch [3], an electronic walkway [15] or wearable inertial sensor [11, 12]. It is noteworthy that the interval between assessements in the current work was considerable longer than in the studies mentioned above. One may suggest that such a long time period of 12 months involves increasing unsystematic variance in the measures obtained. For example, it is conceivable that some PwMS might engage in health behavior, such as sports or physical therapy, in order to maintain their walking capacity, while other might neglect such options. Despite the fact that throughout the long period in the current work, such effects may yield considerable unsystematic variance, ICCs obtained were relatively similar to those of studies with short intervals. This is generally supportive of the methods implemented in the current work and suggests that intertial sensors provide reliable information even throughout longer time periods. Therefore, these sensor-based gait parameters can be identified as clinically relevant markers to evaluate treatment effects over a longer period of time (e.g. the effect of mindfulness training [24] or a six-month Tai Chi training on balance and coordination in PwMS; [2]). Looking at the MS subgroups, the ICCs were slightly higher in MS subgroup 2 (EDSS 2.0–5.0) than those in MS subgroup 1 (EDSS 0.0–1.5) and healthy controls. This is compatible with a previous study that showed that the higher the EDSS score, the more the reliability was increased [11].
It has been known that wearable inertial sensors are highly sensitive in the detection of gait disturbances, even in PwMS with lower or even no obvious gait impairment (e.g., [9, 12, 25, 26]). For example, during a 6-min walk mean gait parameters (mainly walking speed and stride length) consistently revealed significant differences between healthy participants and PwMS from as early as an EDSS value of 1.5 onwards (Table 2; [9]). Due to the good sensitivity of several mean gait parameters (i.e. walking speed and stride length) they can be identified as clinically relevant markers to assess gait impairment in PwMS.
Compared to the mean gait parameters, the parameters of gait variability (SD of gait parameters) showed only good-to-fair ICC values in PwMS (Table S1). However, looking at the MS subgroups the ICCs were slightly higher in MS subgroup 2 (EDSS 2.0–5.0) than those in MS subgroup 1 (EDSS 0.0–1.5). In addition, gait variability seems to be less sensitive in the detection of gait disturbances in early MS (e.g., [4, 27]. For example, Kalron [4] observed no significant differences in gait variability between PwMS classified in the lower disability level categories (EDSS 0 to 3.5) and a significant increase in gait variability when PwMS reached the moderate disability level, represented by EDSS scores of 4 and 5. Thus, parameters of gait variability seem to be less suitable for the detection of gait disturbances in early MS.
Concerning observer-rater test (BBS) and TUG, the ICC values after a period of one year were close to the ICC values of the measured mean gait parameters (Table 3) and in line with previous studies [28, 29]. However, both TUG and BBS showed a bias between 0.079 (MS subgroup 2) and 0.4 (healthy controls) and between 0.065 (MS subgroup 1) and 0.238 (MS subgroup 2), respectively. The time to complete the TUG (from signal to start to the moment the participant returns to the seat) was measured by a stop-watch. Thus, the bias in TUG can be caused by the subject who measures the time. Compared to that, automatically applicable gait assessments (as provided by wearable inertial sensors) provide more objective results. Nevertheless, while the TUG seems to be sensitive in the detection of gait disturbances in early MS (even depending on the subject who measures the time), the BBS seems not to be efficient in discrimination groups in early MS (as expected).
Limitations of the study
Some limitations of the present study require consideration. First, no people with Primary Progressive MS (PPMS) participated in our study. Compared to the included PwMS, it is to be expected that gait parameters in PPMS will deteriorate over a longer period of time and thus, reveal a systematic bias for gait parameters. Second, the mean age for MS subgroup 2 was almost 10 years higher than the other groups (Table 1). Since gait parameters (e.g. walking speed or stride length) change with age [30], some of the differences between MS subgroup 2 and healthy controls can be explained by age-related effects. However, there is no effect of age on the ICC analysis. Third, differences between PwMS and healthy controls (Table 2) are not as noticeable as shown in previous studies (e.g., [9]). This effect can be attributed to the comparatively lower number of participants.
Conclusion
The purpose of the current study was to examine multiple gait parameters (obtained by means of wearable inertial sensors) during a 6-min walk and to determine their stability after one year in PwMS. We found that even after one year all mean gait parameters showed excellent ICC values in PwMS. Due to the excellent stability of mean gait parameters after one year, these sensor-based gait parameters can be identified as clinically relevant markers to evaluate treatment effects over a longer period of time.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Burschka JM, Keune PM, Menge U, Oy UHV, Oschmann P, Hoos O. An exploration of impaired walking dynamics and fatigue in multiple sclerosis. BMC Neurol. 2012;12(1):1–8.
Burschka JM, Keune PM, Oy UHV, Oschmann P, Kuhn P. Mindfulness-based interventions in multiple sclerosis: beneficial effects of Tai Chi on balance, coordination, fatigue and depression. BMC neurology. 2014;14(1):1-9.
Goldman MD, Marrie RA, Cohen JA. Evaluation of the six-minute walk in multiple sclerosis subjects and healthy controls. Mult Scler J. 2008;14(3):383–90.
Kalron A. Gait variability across the disability spectrum in people with multiple sclerosis. J Neurol Sci. 2016;361:1–6.
Keune PM, Young WR, Paraskevopoulos IT, Hansen S, Muenssinger J, Oschmann P, Müller R. Measuring standing balance in multiple sclerosis: further progress towards an automatic and reliable method in clinical practice. J Neurol Sci. 2017;379:157–62.
Keune PM, Cocks AJ, Young WR, Burschka JM, Hansen S, Hofstadt-van Oy U, Muenssinger J. Dynamic walking features and improved walking performance in multiple sclerosis patients treated with fampridine (4-aminopyridine). BMC neurology. 2015;15(1):1–8.
Martin CL, Phillips BA, Kilpatrick TJ, Butzkueven H, Tubridy N, McDonald E, Galea MP. Gait and balance impairment in early multiple sclerosis in the absence of clinical disability. Mult Scler J. 2006;12(5):620–8.
Müller R, Schreff L, Koch LE, Oschmann P, Hamacher D. Measuring Gait Stability in People with Multiple Sclerosis Using Different Sensor Locations and Time Scales. Sensors. 2021;21(12):4001.
Müller R, Hamacher D, Hansen S, Oschmann P, Keune PM. Wearable inertial sensors are highly sensitive in the detection of gait disturbances and fatigue at early stages of multiple sclerosis. BMC Neurol. 2021;21(1):1–8.
LaRocca NG. Impact of walking impairment in multiple sclerosis. The Patient: Patient-Centered Outcomes Research. 2011;4(3):189–201.
Angelini L, Hodgkinson W, Smith C, Dodd JM, Sharrack B, Mazzà C, Paling D. Wearable sensors can reliably quantify gait alterations associated with disability in people with progressive multiple sclerosis in a clinical setting. J Neurol. 2020;267(10):2897–909.
Flachenecker F, Gaßner H, Hannik J, Lee DH, Flachenecker P, Winkler J, Klucken J. Objective sensor-based gait measures reflect motor impairment in multiple sclerosis patients: reliability and clinical validation of a wearable sensor device. Multiple sclerosis and related disorders. 2020;39.
Zahn AM, Koch V, Schreff L, Oschmann P, Winkler J, Gaßner H, Müller R. Validity of an inertial sensor-based system for the assessment of spatio-temporal parameters in people with multiple sclerosis. Frontiers in Neurology. 2023;14:620. https://doi.org/10.3389/fneur.2023.1164001.
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33(11):1444–1444.
Hadouiri N, Monnet E, Gouelle A, Decavel P, Sagawa Y. Evaluation of prolonged walking in persons with multiple sclerosis: reliability of the spatio-temporal walking variables during the 6-minute walk test. Sensors. 2021;21(9):3075.
McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, Wolinsky JS. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001;50(1):121–7.
Berg K, Wood-Dauphinee S, Williams JI. The Balance Scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995;27(1):27–36.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8.
Hamacher D, Hamacher D, Müller R, Schega L, Zech A. The effect of a cognitive dual task on the control of minimum toe clearance while walking. Mot Control. 2019;23(3):344–53.
Hamacher D, Hamacher D, Müller R, Schega L, Zech A. Exploring phase dependent functional gait variability. Hum Mov Sci. 2017;52:191–6.
Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Measur. 1973;33(3):613–9.
Craig JJ, Bruetsch AP, Lynch SG, Horak FB, Huisinga JM. Instrumented balance and walking assessments in persons with multiple sclerosis show strong test-retest reliability. J Neuroeng Rehabil. 2017;14(1):1–9.
Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–60.
Sauder T, Hansen S, Bauswein C, Müller R, Jaruszowic S, Keune J, Keune PM. Mindfulness training during brief periods of hospitalization in multiple sclerosis (MS): beneficial alterations in fatigue and the mediating role of depression. BMC Neurol. 2021;21(1):1–15.
Pau M, Caggiari S, Mura A, Corona F, Leban B, Coghe G, Cocco E. Clinical assessment of gait in individuals with multiple sclerosis using wearable inertial sensors: Comparison with patient-based measure. Multiple Scleros Relat Disord. 2016;10:187–91.
Psarakis M, Greene DA, Cole MH, Lord SR, Hoang P, Brodie M. Wearable technology reveals gait compensations, unstable walking patterns and fatigue in people with multiple sclerosis. Physiol Meas. 2018;39(7): 075004.
Moon Y, Wajda DA, Motl RW, Sosnoff JJ. Stride-time variability and fall risk in persons with multiple sclerosis. Mult Scler Int. 2015;2015:964790. https://doi.org/10.1155/2015/964790.
Cattaneo D, Jonsdottir J, Repetti S. Reliability of four scales on balance disorders in persons with multiple sclerosis. Disabil Rehabil. 2007;29(24):1920–5.
Learmonth YC, Paul L, McFadyen AK, Mattison P, Miller L. Reliability and clinical significance of mobility and balance assessments in multiple sclerosis. Int J Rehabil Res. 2012;35(1):69–74.
Himann JE, Cunningham DA, Rechnitzer PA, Paterson DH. Age-related changes in speed of walking. Med Sci Sports Exerc. 1988;20(2):161–6.
Acknowledgements
The authors thank all participants for their efforts taking part in the study.
Funding
The current work was supported by Sanofi-Aventis GmbH, Germany.
Author information
Authors and Affiliations
Contributions
RM conceived of the study, participated in its design, coordination and data acquisition and drafted the manuscript. DH participated in the design of the study, calculated the gait parameter, reviewed the statistical analysis and revised the manuscript. PMK and PO participated in the design of the study and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethical review board of the Friedrich Schiller University Jena, Germany (2018–1221-BO) and was in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects involved in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Variability (SD) values of the 6-min walk. Figure S1. Bland-Altman plots for gait parameters variability show the differenceversus the mean of both measurements for all single measurements (assessment 1,assessment 2). The solid line indicates the bias and the dashed lines theLimits of Agreement (95% confidence interval of the bias) for healthy controls (grey)and PwMS (black). MTC: minimum toe-to-floor distance.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Müller, R., Hamacher, D., Keune, P.M. et al. Stability of sensor-based gait parameters reassessed after a period of one year in people with multiple sclerosis. BMC Neurol 23, 120 (2023). https://doi.org/10.1186/s12883-023-03168-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-023-03168-9