Abstract
Background
Cerebral resuscitation determines the prognosis for patients who have experienced sudden death, and brain protection is the focus of clinical treatment. Cerebral resuscitation depends on the timing and quality of cardiopulmonary resuscitation (CPR). At present, cerebral oxygen monitoring is used mainly to monitor the quality of external cardiac compression and provide a prognosis for the nervous system. However, after the return of autonomous circulation, it is necessary to conduct continuous monitoring to ensure measures are taken timeously since hemodynamic instability, brain edema, and other factors may cause occult brain injury, and invasive arterial pressure cannot represent cerebral perfusion.
Case presentation
By using continuous cerebral oxygen monitoring after CPR and the return of spontaneous circulation, a patient who was witnessed to have experienced sudden death in the hospital was found to have insufficient cerebral perfusion; he underwent timely intra-aortic balloon counterpulsation to improve his hemodynamics and cerebral perfusion. The patient went on to achieve a good neurological prognosis.
Conclusion
Cerebral oxygen monitoring should be conducted throughout the treatment period; physicians should understand cerebral perfusion in real time and implement timely intervention measures to reduce occult brain injury and improve the neurological prognosis of patients.
Similar content being viewed by others
Background
After successful cardiopulmonary resuscitation (CPR), the overall prognosis of patients who have experienced sudden death is poor. The success rate of CPR for out-of-hospital sudden death is 7.6% in Europe, 6.8% in North America, 3.0% in Asia, and 9.7% in Australia [1]. The main reasons for this low success rate are that CPR for out-of-hospital sudden death is not conducted timeously, and the quality of the CPR is not of a high standard. However, the success rate of CPR for in-hospital sudden death is also low, with some large studies reporting a success rate of approximately 20% [2]. The reasons are as follows: After successful CPR, occult cerebral hypoperfusion persists as a result of factors such as cardiogenic sudden death, myocardial infarction complications, and circulatory instability. Often, this hypoperfusion is not identified, and timely measures are not implemented to correct it. At present, most monitoring methods have a limited effect and cannot reflect cerebral perfusion accurately in real time. In current studies, cerebral oxygen monitoring is mainly used to guide CPR [3]. The present case study revealed that routine cerebral oxygen monitoring after successful CPR may help identify problems, guide treatment, and further improve patients’ neurological prognoses.
Case presentation
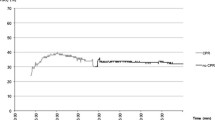
Herein, we report a case in which cerebral oximetry was used to optimize brain perfusion in a patient with a return of spontaneous circulation (ROSC) after cardiac arrest (CA). A 67-year-old man (height = 172 cm, weight = 55 kg) suffered a CA secondary to acute myocardial infarction. His past medical history included hypertension, diabetes mellitus, and chronic renal failure (stage 5). The patient had a 15-min history of chest distress and sweating, and CA occurred as the ambulance arrived at the emergency department. Mechanical CPR was started using the LUCAS 2 Chest Compression System (Medtronic, Minneapolis, USA), an intravenous infusion of various drugs was administered, and monitoring of frontal oxygenation using near-infrared spectrophotometry (INVOS™ 5100 C Cerebral/Somatic Oximeter, Medtronic) was started. An ROSC occurred 8 min later, and an electrocardiogram indicated extensive ST-segment elevation in leads V2–V5. The regional cerebral oxygen saturation (rSO2) levels were 70–80%. Cardiologists performed a coronary artery balloon dilation and administered 300-mg aspirin, 180-mg ticagrelor, and 5,500-IU heparin within 3 h of admission. However, the patient’s pupils became dilated, and they reacted slowly to light. His consciousness deteriorated. The rSO2 showed a continuous decline from 80 to 21%, with little change in the arterial blood gas analysis, but the heart rate, blood pressure, and ejection fraction (EF) measured by ultrasound cardiogram decreased from 130 to 90 bpm, 180/90 to 99/58 mmHg, and 46–33%, respectively. A left ventricular aneurysm was observed. An intra-aortic balloon pump (IABP) was fitted to maintain the patient’s blood pressure at 130–140/70–90 mmHg.
The next day, the patient felt mild–moderate pain, their EF was 55%, and their rSO2 increased gradually from 21 to 50%. Five days after PCI passed away, the IABP was removed successfully, the patient’s vital signs were stable, most indicators were improving, and the patient’s neurological prognosis was good (cerebral performance category = 2).
Discussion
At present, the static value of brain oxygenation as an indicator of neurological prognosis is an important research topic [4].
In the past, cerebral resuscitation treatment has primarily consisted of providing treatment and observing the outcome without conducting any monitoring. At present, brain oxygen monitoring is not implemented routinely. A mean arterial pressure of > 65 mmHg does not represent good cerebral perfusion [5]. In this case, through the continuous monitoring of brain oxygen levels (in which changes in values were monitored to identify and explain problems that had occurred), a possible brain function injury caused by a hemodynamic disorder was revealed; timely measures were implemented to avoid further brain injury, and a good neurological outcome was achieved. This type of monitoring can further improve a patient’s overall neurological prognosis. Therefore, routine cerebral oxygen monitoring is recommended. However, further studies should be conducted on patients who experience sudden death to compare the neurological prognoses between those who receive cerebral oxygen monitoring and those who do not.
Currently, brain damage is the most important cause of morbidity and mortality in survivors of CA, and an rSO2 level of < 25% increases the likelihood of death and poor neurological outcome [6,7,8]. Despite adequate resuscitation, occult cerebral ischemia can still occur. Therefore, it is necessary to conduct cerebral oxygen monitoring in real time. Several studies have shown that the use of near-infrared spectrophotometry (cerebral oximetry) is feasible since it reliably reflects perfusion [9] and offers real-time noninvasive monitoring [10]. Recent evidence suggests that the use of cerebral oximetry could illustrate the quality of resuscitation during CA [11]. In this case study, it was used for the timeous identification of occult cerebral ischemia and hypoxia.
Some studies have shown that increased extracorporeal membrane oxygenation (ECMO) blood flow and sweep gas flow are effective at correcting low rSO2 [12]. However, the use of ECMO can cause complications and result in an economic burden. Conversely, IABP is easy to manage, is relatively cheap, has a wide range of indications (e.g., complications associated with acute myocardial infarction and pump failure), can reduce the load on the heart, and can increase organ perfusion[13]. In this case study, IABP was shown to be efficient.
Therefore, we recommend that the rSO2 of patients who are in a coma should be monitored routinely and continuously. An IABP may be an effective means of ensuring adequate brain oxygenation in patients who have experienced CA [14].
Further studies are needed to explore the application of cerebral oxygen monitoring.
Conclusion
In this case study, cerebral oxygen monitoring, which was conducted throughout the treatment period after resuscitation, helped the doctors understand the patient’s cerebral perfusion in real time. This facilitated timely interventions, resulting in reduced occult brain injury and a good prognosis. The approach creates possible routes for treatment after resuscitation in patients who have experienced sudden death. Furthermore, hemodynamics should be optimized based on rSO2 levels to improve patients’ neurological prognoses. The limitation of this study is that it lacks sufficient data to reveal the characteristics and influencing factors of dynamic changes in cerebral oxygenation.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ROSC:
-
Return of spontaneous circulation
- CA:
-
Cardiac arrest
- IABP:
-
Intra-Aortic Balloon Pump
- rSO2:
-
Regional cerebral oxygen saturation
- PTCA:
-
Coronary Artery Balloon Dilation
- EF:
-
Ejection fraction
- CPC:
-
Cerebral performance categories
References
Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–87.
Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33(2):237–45.
Takegawa R, Taniuchi S, Ohnishi M, Muroya T, Hayakawa K, Tachino J, et al. Effectiveness of near-infrared spectroscopy-guided continuous chest compression resuscitation without rhythm check in patients with out-of-hospital cardiac arrest: The prospective multicenter TripleCPR 16 study. Resuscitation. 2021;169:146–53.
Genbrugge C, Dens J, Meex I, Boer W, Jans F, De Deyne C. Cerebral saturation monitoring during cardiopulmonary resuscitation should be used as dynamic, rather than static, information. Resuscitation. 2013;84(9):e111-2.
Kishihara Y, Yasuda H, Kashiura M, Harada N, Moriya T. Can Cerebral Regional Oxygen Saturation (rSO(2)) Be Used as an Indicator of the Quality of Chest Compressions in Patients With Cardiopulmonary Arrest? A Study Evaluating the Association Between rSO(2) and Mean Arterial Pressure: The PRESS Study. Front Med. 2022;9:810449.
Parnia S, Yang J, Nguyen R, Ahn A, Zhu J, Inigo-Santiago L, et al. Cerebral Oximetry During Cardiac Arrest: A Multicenter Study of Neurologic Outcomes and Survival. Crit Care Med. 2016;44(9):1663–74.
Liu Y, Jing K, Liu H, Mu Y, Jiang Z, Nie Y, et al. Association between cerebral oximetry and return of spontaneous circulation following cardiac arrest: A systematic review and meta-analysis. PLoS ONE. 2020;15(8):e0234979.
Sanfilippo F, Murabito P, Messina A, Dezio V, Busalacchi D, Ristagno G, et al. Cerebral regional oxygen saturation during cardiopulmonary resuscitation and return of spontaneous circulation: A systematic review and meta-analysis. Resuscitation. 2021;159:19–27.
Kalkan A, Bilir O, Ersunan G, Ozel D, Tas M, Memetoglu ME. Abdominal oxygen saturation for monitoring return of spontaneous circulation in out-of-hospital cardiac arrest using near infrared spectrophometry. Am J Emerg Med. 2015;33(3):344–8.
Reagan EM, Nguyen RT, Ravishankar ST, Chabra V, Fuentes B, Spiegel R, et al. Monitoring the Relationship Between Changes in Cerebral Oxygenation and Electroencephalography Patterns During Cardiopulmonary Resuscitation: A Feasibility Study. Critical care medicine. 2018.
Takegawa R, Shiozaki T, Ogawa Y, Hirose T, Mori N, Ohnishi M, et al. Usefulness of cerebral rSO 2 monitoring during CPR to predict the probability of return of spontaneous circulation. Resuscitation. 2019;139.
Taccone FS, Fagnoul D, Rondelet B, Vincent JL, de Backer D. Cerebral oximetry during extracorporeal cardiopulmonary resuscitation. Crit Care (London England). 2013;17(1):409.
Nussbaum ES, Heros RC, Solien EE, Madison MT, Sebring LA, Latchaw RE. Intra-aortic balloon counterpulsation augments cerebral blood flow in a canine model of subarachnoid hemorrhage-induced cerebral vasospasm. Neurosurgery. 1995;36(4):879–84. discussion 84 – 6.
Bellapart J, Geng S, Dunster K, Timms D, Barnett AG, Boots R, et al. Intraaortic Balloon Pump Counterpulsation and Cerebral Autoregulation: an observational study. BMC Anesthesiol. 2010;10:3.
Acknowledgements
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
No external funding received to conduct this study.
Author information
Authors and Affiliations
Contributions
ZH and LC conceived the idea and conceptualised the study. LJ collected the data and analysed the data. WX drafted the manuscript, then ZH reviewed the manuscript. All authors read and approved the final draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
I confirm that I have read the Editorial Policy pages. This study was conducted with approval from the Ethics Committee of Aerospace Center Hospital. This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from the participant.
Consent for publication
Written informed consent was obtained from the case patient for publication of this report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, H., Lin, C., Liu, J. et al. Continuous monitoring of brain perfusion by cerebral oximetry after spontaneous return of circulation in cardiac arrest: a case report. BMC Neurol 22, 365 (2022). https://doi.org/10.1186/s12883-022-02880-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-022-02880-2