Abstract
Background
Posterior Reversible Encephalopathy Syndrome (PRES) is a neurotoxic state characterized by seizures, headache, vision change, paresis, and altered mental status. PRES has an important place in medicine due to the wide variety of causative diseases, infections, and medications that precipitate its mysterious onset. Although exposure to medications, particularly immunosuppressants, cancer chemotherapy, and biologic drugs, is a common occurrence in patients who develop PRES, Mepolizumab has never before been associated.
Case presentation
This report of a 67-year-old male patient outlines the first reported case of Mepolizumab-induced PRES in the literature.
Conclusions
Treatment of severe asthma, asthma-exacerbations, and diseases such as eosinophilic granulomatosis with polyangiitis (formerly Churg-Strauss) with Mepolizumab is rapidly gaining popularity ever since the drug’s recent FDA-approval. This report aims to raise awareness of this potentially life-threatening and previously unreported side effect of Mepolizumab since early identification of the causative agent is the key to preventing the severe neurologic disability and possible death that may occur from the delayed treatment of PRES.
Similar content being viewed by others
Background
Mepolizumab (NUCALA) is a humanized monoclonal antibody antagonist to IL-5, recently approved by the FDA in 2015. It has gained popularity in the treatment of severe eosinophilic asthma and eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome). This report is the first in the literature to identify the IL-5 directed antibody, Mepolizumab, as a potential causative agent of Posterior Reversible Encephalopathy Syndrome (PRES) also known as Reversible Posterior Leukoencephalopathy [1,2,3]. PRES is a clinico-radiologic syndrome of heterogeneous etiologies that is diagnosed upon both identification of specific clinical manifestations indicative of a neurotoxic state as well as pathognomonic radiologic criteria such as subcortical brain edema.
Case presentation
A 67-year-old male presented to the emergency department with an acute event of altered awareness. The patient was watching TV with his family when he suddenly had an unusual sensation of sand in his eyes. His family noticed that he was verbally unresponsive for 15 min with a blank stare. There were no abnormal movements of the body or limbs. He scratched his head and stood up during the episode but did not remember this. The patient maintained postural tone and there was no loss of bowel or bladder control. When he regained speech, it was slurred and incoherent. He presented to our emergency department by ambulance and was back to baseline when he was evaluated with no apparent recollection of the event.
He endorsed 4 weeks of new-onset worsening bifrontal headaches and new-onset episodes of pins and needles in his extremities. Prior to that, he reported a normal state of health. He denied fevers, chills, night sweats, stiff neck, or weight change. The patient has a medical history of chronic asthmatic bronchitis, obstructive sleep apnea, hypertension, and well-controlled type II diabetes on daily metformin. His asthma was well controlled on Omalizumab, but two months prior, he changed to Mepolizumab due to personal preference for a lower dosing frequency. The patient had been newly prescribed 100 mg/mL of Mepolizumab on a dosing frequency of every 4 weeks and it had been taken twice prior to his hospital admission (last dose two weeks prior). His eosinophil counts (absolute) were 170, 60, 70, and 310 / uL at his prior outpatient visits over the previous 18 months.
On examination by neurology, the patient was fully alert, attentive, and oriented. He provided a coherent history with no difficulty answering questions or following commands. Speech was slow and mildly dysarthric, but the patient and his wife state that this was his baseline. Language was fluent without paraphasic errors. Naming and repetition were intact. No extinction or neglect was elicited. His left pupil was irregular and larger than the right (noted to have prior cataract surgery in that eye). Both were briskly reactive. Visual fields were intact. His extraocular movements showed saccadic breakdown of pursuit, and he had multiple beats of bidirectional end-gaze nystagmus with intermittent rotary qualities. His facial sensation was symmetrically intact. He had unilateral flattening of the nasolabial fold which corrected with a smile (patient stated this was normal). Shoulder shrug was strong bilaterally. Tongue protrusion was midline with full rapid lateral motion. No asterixis, tremors or other abnormal movements were observed. He had a normal muscular tone throughout and 5/5 bilateral upper and lower extremities without pronator drift. Biceps and brachioradialis reflexes were 1 + and symmetric. Patellar and ankle jerk reflexes were 2 + and symmetric. Hoffman’s and Babinski’s signs were not noted and clonus was absent. His sensation to light touch and pinprick was intact throughout. He reported decreased vibratory sensation at left medial malleolus compared to right, although both were near normal. Dysmetria was present on both bilateral finger-nose-finger and heel-shin testing. Rapid alternating movements were intact. He took a few steps with a normal and stable, casual gait.
The patient was admitted to the hospital for observation and workup of his isolated episode of altered mental status as well as his new headaches and paresthesias. He was started on Keppra (levetiracetam) for possible complex-partial seizure. The initial differential included hypetensive encephalopathy, cerebral venous thrombosis, acute demyelinating encephalomyelitis, malignancy (primary or metastatic) or paraneoplastic encephalitis, infectious encephalitis, and various toxidromes (such as lead, carbon monoxide, inhalants, amphetamines, opiates, and/or benzodiazepines). Head CT revealed bilateral areas of confluent subcortical white matter hypoattenuation (Fig. 1). The differential was narrowed to include leukoencephalopathy, vasculitis, or infiltrating neoplasm such as lymphoma among other etiologies.
CT without contrast, initial scan on presentation. This head CT revealed confluent areas of white matter hypoattenuation bilaterally, slightly worse on the left, involving the subcortical white matter. No significant mass effect midline shift, or hemorrhage. The differential was thought to include leukoencephalopathy, vasculitis, or infiltrating neoplasm such as lymphoma among other etiologies
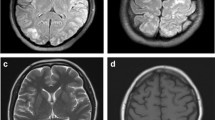
He had an EEG which showed left frontal sharps and spikes with focal slowing and mild generalized slowing. MRI was conducted 35 h after initial CT scan with findings characteristic for PRES (Fig. 2). Labs, including lumbar puncture (glucose 69, protein 78, RBC 4, WBC 0) were unremarkable. His blood pressure had been stable in the 130–160/70–90 mmHg range over the previous 12 months and the patient had no recent changes to his regimen (candesartan). The patient’s blood pressure values during two unrelated hospital visits within the two months prior to hospitalization were 137/76 mmHg (MAP 96) and 129/71 mmHg (MAP 90). During the hospitalization, the patient’s blood pressure ranged between 137/68 mmHg (MAP 91) and 148/78 mmHg (MAP 102) with a mean MAP of 94 across the hospitalization. His other vitals were also unremarkable.
PRES was ultimately identified due to the suspicious temporal relationship between Mepolizumab initiation and the onset of symptoms in conjunction with pathognomonic imaging findings. Though other IL-modulating drugs such as tocilizumab and ustekinumab have been implicated in PRES, there are no previous reports of Mepolizumab-associated PRES; this suspicion was relayed to the patient’s pulmonology team, however, due to lack of evidence and worsening control of the patient’s respiratory symptoms, Mepolizumab was re-ordered. The patient ultimately declined re-starting the drug due to the recommendations from neurology. Symptoms and imaging showed improvement at both 1-month and 6-month follow up appointments (Figs. 2 and 3). Due to the absence of seizures or any new episode of altered awareness, the patient was titrated off his levetiracetam dose and has not reported any more issues or concerns. He has transitioned back to omalizumab and has regained good control of his asthma.
MRI sequences related to patient’s PRES. Top row Diffusion, Middle and Bottom Row FLAIR (A) Initial Presentation (B) 1-month after stopping Mepolizumab (C) 6-months after stopping Mepolizumab. Underlying white matter edema. There is also an unusual pattern of associated susceptibility artifact, which might imply a process that is hemorrhagic. In all sequences assessed, this patient’s scan is notably improved
Discussion
PRES was first described in a case series in 1996 by Hinchey et. al. in the New England Journal of Medicine where four syndromes (Reversible Posterior Cerebral Edema Syndrome, Posterior Leukoencephalopathy Syndrome, Hyperperfusion Encephalopathy, Brain Capillary Leak Syndrome) were codified under a single name [4]. Unfortunately, none of these names are satisfactory as the syndrome is, confusingly, not always reversible and it is not always confined to the white matter nor the posterior regions of the brain [5]. However, it is postulated that the posterior brain is more commonly involved due to the slightly lower concentrations of autoregulatory adrenergic nerves around the pial and intracerebral vessels posteriorly compared to anterior circulation [6]. PRES affects women more than men and is seen most often in age 40–50 [4].
The pathophysiology of PRES is unclear, although two primary theories have been postulated [7]. The hyperperfusion theory proposes that hypertension, or even simply a rapid increase from the patient’s baseline blood pressure disrupts basement membrane integrity in the blood–brain barrier (BBB), causing extravasation of fluid and subsequent vasogenic edema (VE). Consistent with this theory, patients with chronic hypertension are at increased risk of developing PRES, and acute increases in blood pressure are present in 60–80% of PRES patients [7]. Conversely, the hypoperfusion theory proposes that cell cytotoxicity through mechanisms such as autoimmune disease, immunosuppression, and cancer chemotherapy can cause similar BBB disruption resulting in VE. PRES has been described extensively in the use of immunosuppressant drugs such as gemcitabine, tacrolimus, and sirolimus. Commonly used biologics such as Adalimumab (Humira), Infliximab (Remicade), Rituximab (Rituxan), and Etanercept (Enbrel) have all been implicated in numerous PRES cases as well. The high percentage of patients with PRES who have autoimmune disorders may further support the theory that PRES is in part caused by endothelial dysfunction, a process in which the host autoimmune response is essential; endothelial cells become activated and damaged by an inflammatory cytokine response stemming from monocytes and lymphocytes, which can lead to leakage of fluid and protein into the interstitium [8,9,10,11].
The symptoms of PRES evolve rapidly over hours to days and include seizures, headaches, altered consciousness, and visual disturbances often in the context of elevated BP as discussed above. Seizures are often the presenting symptom with only a small minority of patients with mild disease being seizure-free. Though noncontrast head CTs are often the first neuroimaging study performed in the emergency department, follow-up neuroimaging with noncontrast brain MRI is essential to an accurate diagnosis. Elimination of other differential diagnoses such as hypertensive encephalopathy and reversible cerebral vasoconstriction syndrome is critical as PRES can mimic many other disease processes. It is necessary to treat PRES promptly to prevent permanent neurological damage or even death. Treatment typically consists of antiseizure medications and removal of the offending agent along with strict blood pressure control.
Conclusions
Reversible posterior leukoencephalopathy syndrome (PRES) is an increasingly recognized neurological disorder with an ever-increasing number of documented etiologies. It most often presents with clinical seizures, headache, and visual symptoms, all three of which were seen in this case report. Seizures have been noted to appear slightly later in onset relative to headaches, consistent with the 4-weeks of new-onset headaches leading up to our patient’s episode of altered mental status and subsequent 911 call. The relationship between PRES and mepolizumab remains unknown however this case report is the first of its kind. It hopes to highlight the importance for prescribers of mepolizumab such as pulmonologists, rheumatologists, and immunologists as well as physicians who care for patients on mepolizumab to identify signs and symptoms so that early discontinuation of the drug can prevent the permanent damage and even death that may occur from delayed treatment of PRES.
Availability of data and materials
All the data supporting our findings is contained within the manuscript. Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- PRES:
-
Posterior Reversible Encephalopathy Syndrome
- BBB:
-
Blood–Brain Barrier
- VE:
-
Vasogenic Edema
References
Ortega HG, Liu MC, Pavord ID, Brusselle GG, FitzGerald JM, Chetta A, Chanez P. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014;371(13):1198–207 PMID: 25199059.
FitzGerald JM, Bleecker ER, Nair P, Korn S, Ohta K, Lommatzsch M, Gilmartin G. Benralizumab, an anti-interleukin-5 receptor α monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. The Lancet. 2016;388(10056):2128–41 PMID: 27609406.
Bernstein JA, Virchow JC, Murphy K, Maspero JF, Jacobs J, Adir Y, Hickey L. Effect of fixed-dose subcutaneous reslizumab on asthma exacerbations in patients with severe uncontrolled asthma and corticosteroid sparing in patients with oral corticosteroid-dependent asthma: results from two phase 3, randomised, double-blind, placebo-controlled trials. Lancet Respir Med. 2020;8(5):461–74 PMID: 32066536.
Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, Caplan LR. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334(8):494–500 PMID: 8559202.
Stott VL, Hurrell MA, Anderson TJ. Reversible posterior leukoencephalopathy syndrome: a misnomer reviewed. Intern Med J. 2005;35(2):83–90 PMID: 15705136.
Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. The Lancet Neurology. 2015;14(9):914–25 PMID: 26184985.
Feske SK. Posterior reversible encephalopathy syndrome: a review. Semin Neurol. 2011;31(02):202–15 Thieme Medical Publishers PMID: 28054130.
Boukari F, Dugourd PM, Chassang M, Mondot L, Passeron T, Lacour JP, Montaudie H. Posterior reversible encephalopathy syndrome due to combination of vemurafenib and cobimetinib for metastatic melanoma. Pigment Cell Melanoma Res. 2017;30(2):262–4. https://doi.org/10.1111/pcmr.12562 Epub 2017 Mar 6 PMID: 27885826.
Hosoi M, Yamamoto G, Imai Y, Kurokawa M. Reversible posterior leukoencephalopathy syndrome following R-CHOP therapy for diffuse large B-cell lymphoma. Ann Hematol. 2010;89(2):207–8. https://doi.org/10.1007/s00277-009-0783-x Epub 2009 Jul 7 PMID: 19582454.
Maur M, Tomasello C, Frassoldati A, Dieci MV, Barbieri E, Conte P. Posterior reversible encephalopathy syndrome during ipilimumab therapy for malignant melanoma. J Clin Oncol. 2012;30(6):e76–8. https://doi.org/10.1200/JCO.2011.38.7886 Epub 2011 Dec 27 PMID: 22203769.
Pritikanta Paul, Koffman Boyd. Neurological Complications of Monocloncal Antibodies. Presentation presented at: American Academy of Neurology Annual Meeting. Los Angeles: indexed P1.147 and as part of published meeting catalogue in supplement 15; 2018.
Acknowledgements
Michal Kucewicz thankfully acknowledged for contributions to this work.
Funding
Funding for publication supported by the University of Minnesota Department of Neurology. This funding body has had no role in the design of the study, data collection, analysis, interpretation of the data nor in the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
BB, MG, GM & KB responsible for the clinical management of the patient and manuscript. VP, AS, KM, DG and KN were responsible for drafting the manuscript. All authors: critical revision of the manuscript for important intellectual content, read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics committee approval was not applicable as the information was analyzed in a retrospective manner and had no effect on treatment.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. No identifying patient information was used.
Competing interests
IDUB Aurum grant from the Gdansk University of Technology to support international research team building.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Puram, V.V., Ghazaleh, D., Salari, A. et al. Mepolizumab-Induced Posterior Reversible Encephalopathy Syndrome (PRES), a new patient report. BMC Neurol 22, 318 (2022). https://doi.org/10.1186/s12883-022-02849-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-022-02849-1