Abstract
Background
Eptinezumab is an anti-calcitonin gene-related peptide humanized monoclonal antibody approved for the preventive treatment of migraine in adults. The PREVAIL study demonstrated a favorable safety profile with sustained reductions in overall migraine-related burden in patients with chronic migraine (CM). This post hoc analysis aimed to examine item-level changes in the Migraine Disability Assessment (MIDAS) questionnaire over 2 years in participants with CM on eptinezumab treatment.
Methods
PREVAIL was an open-label, phase 3 trial that included 96 weeks of treatment where 128 adults received intravenous eptinezumab administered over 30 min every 12 weeks (wks) for up to 8 doses of 300 mg. MIDAS was administered at baseline, Wk12, and every 12wks thereafter. Two supplementary MIDAS items not included in the total score calculation assessed number of headache days in the past 3 months (MIDAS headache) and average headache pain severity (from 0 [none] to 10 [worst]). MIDAS total scores were summed from 5 items, each quantifying the number of days in the past 3 months with migraine-related disability. Items 1, 3, and 5 assessed absenteeism, namely how many days the patient missed work/school (Q1), household work (Q3), or family/social/leisure activities (Q5). Items 2 and 4 were measures of presenteeism, namely how many days the patient had reduced productivity in work/school (Q2) or household work (Q4).
Results
Mean MIDAS headache days decreased from 47.4 (baseline) to 17.1 (Wk12) and 16.3 (Wk104). The average headache pain severity score (0‒10) decreased from a mean of 7.3 (baseline) to 5.5 (Wk12) to 4.5 (Wk104). Mean MIDAS scores measuring absenteeism (Q1, 3, 5) changed from 9.7 days at baseline to 3.2 days (Wk12) and to 3.9 days (Wk104). Mean MIDAS scores measuring presenteeism (Q2, 4) at Wk12 decreased from 14.2 days at baseline to 5.2 days (Wk12, 104). Patients categorized with very severe MIDAS disability had a mean total MIDAS score of 84.8, with an average reduction of 56.7 days (Wk12), which was maintained at 32 days at Wk104.
Conclusions
Long-term treatment with eptinezumab in patients with CM suggested sustained reductions in MIDAS-quantified disability, consistent with the sustained reductions in headache frequency and pain severity.
Trial registration
ClinicalTrials.gov identifier: NCT02985398.
Similar content being viewed by others
Introduction
Chronic migraine (CM) is a disease that results in long-term disability and high disease burden. Migraine is one of the top five leading causes of disability among people aged 10‒49 years [1, 2]. The majority of patients with migraine rely on acute medication to control symptoms, where approximately 38% of patients would benefit from the use of preventive therapies and only 3‒13% actually receive them [3]. Among the patients using preventive migraine treatment, e.g., topiramate and onabotulinumtoxinA, patients with CM discontinue preventive treatment primarily due to side effects and lack of efficacy [3, 4], with a sharp drop in persistence in commonly prescribed oral preventive medication at 30 days and over the ensuing 12 months [5]. Given the enduring effects of migraine, understanding the effects of long-term treatment, particularly on patient-reported outcomes (PROs), is important.
A humanized immunoglobulin G1 monoclonal antibody that binds quickly and durably to calcitonin gene-related peptide, which is integral in migraine pathophysiology [6,7,8], eptinezumab is approved for the preventive treatment of episodic and chronic migraine in adults [9]. The two pivotal phase 3 trials, PROMISE-1 in patients with episodic migraine and PROMISE-2 in patients with CM, determined that intravenous (IV) infusion of 100 mg and 300 mg achieved the primary efficacy endpoint by significantly decreasing mean monthly migraine days over Weeks 1‒12 [10, 11].
The PREVAIL study evaluated the long-term safety, immunogenicity, and impact on PROs of repeated doses of eptinezumab in patients with CM, demonstrated a favorable safety profile, and provided early and sustained reductions in overall migraine-related burden [12]. The favorable safety profile of eptinezumab demonstrated in this long-term trial is consistent with previously published results [13, 14]. The objective of this post hoc analysis was to evaluate item-level changes in the Migraine Disability Assessment (MIDAS) questionnaire over 2 years in patients with CM on eptinezumab treatment. Additional objectives of this analysis included examining correlations between MIDAS total score and migraine days and between MIDAS scores and other PROs (6-item Headache Impact Test [HIT-6], Patient Global Impression of Change [PGIC]) in order to further support the clinical relevance of MIDAS in patients with CM.
Methods
Data source
The detailed methodology for PREVAIL has been reported [12]. In brief, PREVAIL was a phase 3, open-label study conducted at 20 study sites in the United States from 12 December 2016 to 11 April 2018 that evaluated the long-term safety, immunogenicity, and impact on PROs of repeated doses of 300 mg IV eptinezumab administered over 30 min in 128 adults [12]. In addition, PREVAIL included 2 treatment phases: the primary treatment phase included 4 infusions of eptinezumab 12 weeks apart (Day 0, and Weeks 12, 24, and 36); the secondary treatment phase included up to 4 additional eptinezumab infusions 12 weeks apart (Weeks 48, 60, 72, and 84). Further, patients were followed for 20 additional weeks until Week 104, for a total study duration of 106 weeks, including the screening period.
Patients were between the ages of 18‒65 and had a diagnosis of migraine at \(\le\) 50 years of age with history of CM \(\ge\) 1 year (International Classification of Headache Disorders, 3rd edition, beta [ICHD-3β] criteria) [15]. In addition, patients had been prescribed or recommended by a healthcare professional to use prescription or over-the-counter medication for acute and/or prophylactic treatment of migraine, and any prophylactic use of medications for headaches was stable for ≥ 3 months prior to screening. All clinical work was in compliance with current Good Clinical Practices as outlined in the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use, local regulatory requirements, and the principles of the Declaration of Helsinki. All participants provided written informed consent prior to participation.
Outcomes and assessments
PRO measures included the MIDAS questionnaire [12], which measured the headache effect on patient daily functioning. The MIDAS questionnaire was administered on Day 0, at Week 12, and every 12 weeks thereafter until Week 104. Specifically, MIDAS is composed of five questions that assessed the patient’s performance over the past 3 months (i.e., 12-week recall), where the response to each question was provided in number of days, which were then totaled to determine the level of disability: 0‒5, MIDAS grade I (little or no disability); 6‒10, MIDAS grade II (mild disability); 11‒20, MIDAS grade III (moderate disability); and 21‒40, MIDAS grade IV (severe disability) [16]. Due to the high number of patients included within the severe disability category, this category was further subdivided into a fifth category, 41‒270, MIDAS grade V (very severe disability) [17]. Within the MIDAS questionnaire, items 1, 3, and 5 assess absenteeism, or how many days the patient missed work/school (Question 1), household work (Question 3), or family/social/leisure activities (Question 5), whereas items 2 and 4 measure presenteeism, or how many days the patient had reduced productivity in work/school (Question 2) or household work (Question 4) [18]. Two supplementary items assessed the number of headache days, i.e., MIDAS headache days in the past 3 months (if a headache lasted more than 1 day, each day was counted), and average headache pain severity (from 0 [no pain at all] to 10 [pain as bad as it can be]). A meaningful threshold for change in MIDAS total score is a reduction of \(\ge\) 5 points (days) in total score when a baseline score is 11‒20 days and \(\ge\) 30% with a baseline score of > 20 days [19].
In addition, the PGIC was administered at Weeks 4, 8, 12, and every 12 weeks thereafter until Week 104. The PGIC includes a single question concerning the patient’s impression of change in their disease status since the start of the study, with seven potential answers: very much improved, much improved, minimally improved, no change, minimally worse, much worse, and very much worse [12]. The HIT-6 was administered at screening, on Day 0, at Weeks 4 and 12, and every 12 weeks thereafter until Week 104 [12]. Specifically, HIT-6 measures the impact of migraine on daily life, comprising six items: severe pain, social limitations, role limitations, cognitive functioning (4-week recall), psychological distress (4-week recall), and vitality (4-week recall) using a Likert scale of frequency: never (6), rarely (8), sometimes (10), very often (11), and always (13). The total scores range from 36‒78, where a 6-point decrease is considered clinically meaningful in patients with chronic migraine [20].
Statistical analysis
The safety population included all patients receiving \(\ge\) 1 dose of eptinezumab [12]. MIDAS, HIT-6, and PGIC scores were summarized using descriptive statistics by timepoint with no imputation for missing values. To examine the relationships among MIDAS, HIT-6, and PGIC scores, Spearman correlations were calculated at Week 12. All analyses were conducted using SAS software (SAS Institute, Cary, North Carolina) Version 9.2 or higher.
Results
Study population
All 128 patients enrolled in the study received \(\ge\) 1 dose of 300 mg eptinezumab, where 125 patients (97.7%) remained in the study until Week 12, 118 patients (92.2%) attended the Week 48 visit, and 100 patients (78.1%) attended the Week 104 visit. The majority of patients (67.2%) received all 8 doses of eptinezumab and 87.5% received \(\ge\) 4 doses [12]. Patients were predominately female (85.2%), white (95.3%), and an ethnicity other than Hispanic or Latino (79.7%); baseline demographic information is reported in Table 1. In the 3 months prior to screening, the mean number of migraine and headache days per 28 days among patients was 14.1 and 20.3, respectively [12]. In addition, at baseline, 38.3% of patients had a diagnosis of medication-overuse headache (ICHD-3β criteria) [12, 15].
MIDAS headache days and migraine pain severity
Eptinezumab reduced mean headache days, as assessed by MIDAS, over a 3-month period from 47.4 at baseline to 17.1 at Week 12, which was sustained to Week 104 (mean 16.3 days) (Fig. 1). Further, the average MIDAS headache pain severity (graded on a 0‒10 scale) was reduced from a mean of 7.3 at baseline to 5.5 at Week 12 and to 4.5 at Week 104 (Fig. 2).
MIDAS item scores over 2 years
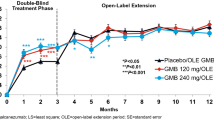
At baseline, the greatest MIDAS disability was noted in Question 4 (mean 16.4 days) and Question 3 (mean 15.6 days), which was reduced to means of 5.5 and 4.7 days, respectively, at Week 12. Mean scores for Questions 1, 2, and 5 were reduced from 5.4, 12.0, and 8.0 days at baseline to 2.2, 4.8, and 2.8 at Week 12, respectively. Reductions at Week 12 were generally sustained through Week 104 (Table 2, Supplemental Fig. 1). The mean MIDAS scores measuring absenteeism (Questions 1, 3, 5) changed from 9.7 days at baseline to 3.2 days (Week 12, n = 123) to 3.9 days (Week 104, n = 95). Mean MIDAS scores measuring presenteeism (Questions 2, 4) decreased from 14.2 days at baseline to 5.2 days at Week 12 (n = 123) and was sustained at 5.2 days at Week 104 (n = 95) (Fig. 3).
Change from baseline in MIDAS item scores measuring absenteeism* and presenteeism† over 2 years. MIDAS, Migraine Disability Assessment. *Absenteeism comprises the average of Items 1, 3, and 5. Item 1: missed work/school; Item 3: no household work; Item 5: missed family/social/leisure activities. The average at baseline was 9.7 †Presenteeism comprises the average of Items 2 and 4. Item 2: work/school productivity ≤ half; Item 4: household productivity ≤ half. The average at baseline was 14.2
MIDAS total score from baseline to week 104
Patients who were categorized with very severe MIDAS disability (scores ≥ 41) had a mean total MIDAS score of 84.8, with an average reduction of 56.7 days at Week 12, which was sustained at 32 days at Week 104 (Fig. 4A). At baseline, patients who were < 50%, 50‒74%, and ≥ 75% monthly headache responders had a mean total MIDAS score of 46.0, 49.0, and 62.2 days, respectively, that changed to 46.5, 17.2, and 10.1 by Week 12, and by 23.4, 36.2, and 18.2 by Week 104 (Fig. 4B).
MIDAS total score ± standard error at baseline, Week 12, Week 84, and Week 104: A total safety population and subgroup with very severe MIDAS disability*, and B patients with < 50%, 50‒74%, or ≥ 75% HRR at Week 12. HRR, headache responder rate assessed by MIDAS; MIDAS, Migraine Disability Assessment. *Level of disability based on MIDAS total score: little or no disability (0–5), mild disability (6–10), moderate disability (11–20), severe disability (21–40), very severe disability (41–270)
Correlations among patient-reported outcomes
The percentage of patients reporting “very much improved” or “much improved” PGIC increased from 61.1% at Week 4 to 81.0% at Week 48 and was maintained throughout the remainder of the study [12]. The mean (standard deviation) HIT-6 scores were 65.2 (4.76) at baseline, 57.1 (8.15) at Week 4, 56.9 (8.69) at Week 48, and 56.1 (9.07) at Week 104 [12]. At Week 12, MIDAS headache days were moderately correlated with MIDAS total score (r = 0.5937) and PGIC (r = 0.4679) and weakly correlated with HIT-6 total score (r = 0.3995).
Discussion
In this post hoc analysis, repeated doses of eptinezumab led to clinically meaningful improvement in total MIDAS score and in MIDAS-measured headache pain severity and mean number of headache days, an effect that was observed at the first post-baseline assessment (at 12 weeks) and sustained after each additional dose. This early efficacy finding is consistent with a previous post hoc analysis of data from PROMISE-2, where more patients treated with eptinezumab than those receiving placebo responded as early as month 1 following infusion [21]. Additionally, eptinezumab has been associated with rapid improvements of health-related quality of life, even when administered during a migraine attack, with eptinezumab significantly improving PROs after 4 weeks compared with placebo [22]. The results reported here support and are consistent with previously published results from the double-blind, placebo-controlled PROMISE-2 trial demonstrating that the preventive treatment effect of eptinezumab significantly reduces monthly migraine days from baseline relative to placebo (100 mg, ‒7.7 days, 300 mg, ‒8.2 days; placebo, ‒5.6 days), is sustained over a full 24 weeks, and has an acceptable safety profile in patients with chronic migraine [11, 23].
In PREVAIL, eptinezumab reduced mean monthly headache frequency as quantified by MIDAS from 15.8 monthly headache days at baseline (47.4 headache days over previous 3 months) to 5.7 monthly headache days at Week 12 (17.1 headache days over previous 3 months), which was sustained to Week 104 (5.4 monthly headache days; 16.3 headache days over previous 3 months). These reductions in monthly headache days throughout the study mirrored the reduction in average MIDAS headache pain severity from baseline to Week 104.
Further, the MIDAS scores assessing absenteeism (Questions 1, 3, and 5) or how many days the patient missed work/school/family activities, decreased ~ 6 days from baseline to Week 104, whereas the scores measuring presenteeism (Questions 2 and 4) or how many days the patient had reduced productivity in work or school, decreased ~ 9 days from baseline to Week 104; the slightly lower efficacy seen at Week 104 is likely due to the time from last eptinezumab dose (20 weeks). Overall, these data suggest that eptinezumab treatment may increase patient productivity and engagement in everyday life. In addition, these reductions in MIDAS total score were most pronounced in patients categorized as “very severe” at baseline, suggesting additional benefits for patients most affected by CM [17].
MIDAS, HIT-6, and PGIC are all PRO measures that are recognized by the International Headache Society as valid instruments to quantify patient satisfaction and headache-related healthcare outcomes [24], and all demonstrated improvements in health-related quality of life (HRQoL) that were sustained throughout the course of the study. In addition, the number of headache days assessed by supplemental questions on MIDAS were moderately correlated to MIDAS total scores and PGIC scores and weakly correlated to HIT-6 scores, providing modest validation of the use of the MIDAS questionnaire to assess headache severity in patients.
Overall, these findings demonstrating sustained reductions in headache pain severity in patients treated with eptinezumab are important due to the high frequency of disability, higher healthcare costs, and reduced HRQoL attributed to migraine overall, particularly in patients with CM [17, 25,26,27,28,29]. Further, given that many patients with CM discontinue preventive migraine treatment [5], this study indicates that long-term treatment with eptinezumab provides sustained reduction of headache frequency and severity and, relatedly, high treatment persistency, with 78.9% of patients receiving eptinezumab treatment through Week 84.
Limitations
Because this was a post hoc analysis, additional prospectively designed trials are required to confirm these findings. In addition, PREVAIL was not a placebo-controlled study, which limits the interpretation regarding the clinical relevance and internal validation [12]. Further, individuals were excluded from PREVAIL if they had a history or diagnosis of a headache or migraine disorder that did not meet the ICHD-3β criteria for CM, required botulinum toxin injections for any medical/cosmetic reasons within 4 months prior to screening, or had pre-existing significant cardiovascular disease [12], which limits the ability to generalize these results to all adults with CM. Finally, the number of headache days as quantified by MIDAS was based on patient recall rather than real-time recording of headache days using an electronic headache diary.
Conclusion
Long-term treatment with eptinezumab in patients with CM provided profound and sustained reductions in migraine-related disability as assessed by MIDAS, consistent with the sustained reduction of headache day frequency and pain severity in response to treatment.
Availability of data and materials
In accordance with EFPIA’s and PhRMA’s “Principles for Responsible Clinical Trial Data Sharing” guidelines, Lundbeck is committed to responsible sharing of clinical trial data in a manner that is consistent with safeguarding the privacy of patients, respecting the integrity of national regulatory systems, and protecting the intellectual property of the sponsor. The protection of intellectual property ensures continued research and innovation in the pharmaceutical industry. Deidentified data are available to those whose request has been reviewed and approved through an application submitted to https://www.lundbeck.com/global/our-science/clinical-data-sharing.
Abbreviations
- CM:
-
Chronic migraine
- ICHD-3β:
-
International Classification of Headache Disorders, 3rd edition, beta
- IV:
-
Intravenous
- HIT-6:
-
6-Item Headache Impact Test
- HRQoL:
-
Health-related quality of life
- MIDAS:
-
Migraine Disability Assessment
- PGIC:
-
Patient Global Impression of Change
- PRO:
-
Patient-reported outcome
References
GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neur. 2019;18:459–80. https://doi.org/10.1016/S1474-4422(18)30403-4.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22. https://doi.org/10.1016/S0140-6736(20)30925-9.
Ford JH, Jackson J, Milligan G, et al. A real-world analysis of migraine: a cross-sectional study of disease burden and treatment patterns. Headache. 2017;57:1532–44. https://doi.org/10.1111/head.13202.
Blumenfeld AM, Bloudek LM, Becker WJ, et al. Patterns of use and reasons for discontinuation of prophylactic medications for episodic migraine and chronic migraine: results from the second international burden of migraine study (IBMS-II). Headache. 2013;53:644–55. https://doi.org/10.1111/head.12055.
Hepp Z, Dodick DW, Varon SF, et al. Persistence and switching patterns of oral migraine prophylactic medications among patients with chronic migraine: A retrospective claims analysis. Cephalalgia. 2017;37:470–85. https://doi.org/10.1177/0333102416678382.
Garcia-Martinez LF, Raport CJ, Ojala EW, et al. Pharmacologic characterization of ALD403, a potent neutralizing humanized monoclonal antibody against the calcitonin gene-related peptide. J Pharmacol Exp Ther [Internet]. 2020;374:93–103. https://doi.org/10.1124/jpet.119.264671.
Ho TW, Edvinsson L, Goadsby PJ. CGRP and its receptors provide new insights into migraine pathophysiology. Nat Rev Neurol. 2010 6:10 6:573–82. https://doi.org/10.1038/nrneurol.2010.127.
Edvinsson L, Haanes KA, Warfvinge K, Krause DiN. CGRP as the target of new migraine therapies — successful translation from bench to clinic. Nat Rev Neurol. 2018;14:338–50. https://doi.org/10.1038/s41582-018-0003-1.
VYEPTI [package insert] [Internet]. Bothell, WA; 2022. Available from: Lundbeck Seattle BioPharmaceuticals, Inc.
Ashina M, Saper J, Cady R, et al. Eptinezumab in episodic migraine: A randomized, double-blind, placebo-controlled study (PROMISE-1). Cephalalgia. 2020;40:241–54. https://doi.org/10.1177/0333102420905132.
Lipton RB, Goadsby PJ, Smith J, et al. Efficacy and safety of eptinezumab in patients with chronic migraine. Neurology. 2020;94:e1365–77. https://doi.org/10.1212/WNL.0000000000009169.
Kudrow D, Cady RK, Allan B, et al. Long-term safety and tolerability of eptinezumab in patients with chronic migraine: a 2-year, open-label, phase 3 trial. BMC Neurol. 2021;21:1–12. https://doi.org/10.1186/s12883-021-02123-w.
Smith TR, Spierings ELH, Cady R, et al. Cardiovascular outcomes in adults with migraine treated with eptinezumab for migraine prevention: pooled data from four randomized, double-blind, placebo-controlled studies. J Headache Pain. 2021;22(16):1–11. https://doi.org/10.1186/s10194-021-01360-1.
Smith TR, Spierings ELH, Cady R, et al. Safety and tolerability of eptinezumab in patients with migraine: a pooled analysis of 5 clinical trials. J Headache Pain. 2021;22:1–11. https://doi.org/10.1186/s10194-021-01227-5.
The International Classification of Headache Disorders - ICHD-3 [Internet]. [cited 2022 Jan 3]. Available from: https://ichd-3.org/.
Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology. 2001;56:S20–8. https://doi.org/10.1212/WNL.56.SUPPL_1.S20.
Blumenfeld AM, Varon SF, Wilcox TK, et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: Results from the International Burden of Migraine Study (IBMS). Cephalalgia. 2011;31:301–15. https://doi.org/10.1177/0333102410381145.
Stewart WF, Lipton RB, Whyte J, et al. An international study to assess reliability of the Migraine Disability Assessment (MIDAS) score. Neurology. 1999;53:988–988. https://doi.org/10.1212/WNL.53.5.988.
Ailani J, Burch RC, Robbins MS. The American Headache Society Consensus Statement: Update on integrating new migraine treatments into clinical practice. Headache. 2021;61:1021–39. https://doi.org/10.1111/head.14153.
Houts CR, Wirth RJ, McGinley JS, et al. Determining thresholds for meaningful change for the headache impact test (HIT-6) total and item-specific scores in chronic migraine. Headache. 2020;60:2003–13. https://doi.org/10.1111/head.13946.
Buse DC, Winner PK, Charleston L, et al. Early response to eptinezumab indicates high likelihood of continued response in patients with chronic migraine. J Headache Pain. 2022;23:1–12. https://doi.org/10.1186/s10194-022-01387-y.
McAllister P, Winner PK, Ailani J, et al. Eptinezumab treatment initiated during a migraine attack is associated with meaningful improvement in patient-reported outcome measures: secondary results from the randomized controlled RELIEF study. J Headache Pain. 2022;23:22. https://doi.org/10.1186/s10194-021-01376-7.
Silberstein S, Diamond M, Hindiyeh NA, et al. Eptinezumab for the prevention of chronic migraine: Efficacy and safety through 24 weeks of treatment in the phase 3 PROMISE-2 (Prevention of migraine via intravenous ALD403 safety and efficacy-2) study. J Headache Pain. 2020;21:1–12. https://doi.org/10.1186/s10194-020-01186-3.
Tassorelli C, Diener HC, Dodick DW, et al. Guidelines of the International Headache Society for controlled trials of preventive treatment of chronic migraine in adults. Cephalalgia. 2018;38:815–32. https://doi.org/10.1177/0333102418758283.
Vo P, Paris N, Bilitou A, et al. Burden of Migraine in Europe Using Self-Reported Digital Diary Data from the Migraine Buddy© Application. Neurol Ther. 2018;7:321. https://doi.org/10.1007/S40120-018-0113-0.
Adams AM, Serrano D, Buse DC, et al. The impact of chronic migraine: The Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia. 2015;35:563–78. https://doi.org/10.1177/0333102414552532.
Stokes M, Becker WJ, Lipton RB, et al. Cost of Health Care Among Patients With Chronic and Episodic Migraine in Canada and the USA: Results From the International Burden of Migraine Study (IBMS). Headache. 2011;51:1058–77. https://doi.org/10.1111/j.1526-4610.2011.01945.x.
Feigin VL, Nichols E, Alam T, et al. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:459–80. https://doi.org/10.1016/S1474-4422(18)30499-X.
Buse DC, Rupnow MFT, Lipton RB. Assessing and managing all aspects of migraine: migraine attacks, migraine-related functional impairment, common comorbidities, and quality of life. Mayo Clin Proc. 2009;84:422. https://doi.org/10.1016/S0025-6196(11)60561-2.
Acknowledgements
The authors thank Beth Reichard, PhD, and Nicole Coolbaugh, CMPP, of The Medicine Group, LLC (New Hope, PA, United States) for providing medical writing support, which was funded by H. Lundbeck A/S (Copenhagen, Denmark) in accordance with Good Publication Practice guidelines.
Funding
Sponsored and funded by H. Lundbeck A/S. The sponsor participated in the design and conduct of the study; data collection, management, analysis, and interpretation; and preparation, review, and approval of the manuscript. All statistical analyses were performed by a contracted research organization and were directed or designed by Pacific Northwest Statistical Consulting under contractual agreement with Lundbeck Seattle BioPharmaceuticals, Inc. All authors and H. Lundbeck A/S and Lundbeck Seattle BioPharmaceuticals, Inc. prepared, reviewed, and approved the manuscript and made the decision to submit the manuscript for publication. Editorial support for the development of this manuscript was funded by H. Lundbeck A/S.
Author information
Authors and Affiliations
Contributions
Conception and design of the work: RC. Analysis (JH) and Interpretation (AB, AE, JH, BE, RC). Drafting of the work: AB, AE, JH, BE, RC. Revising it critically for important intellectual content: AB, AE, JH, BE, RC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the independent ethics committee or institutional review board for each of the 21 study sites: San Diego, California, United States, 92108; Santa Monica, California, United States, 90404; Colorado Springs, Colorado, United States, 80918; Bradenton, Florida, United States, 34201; DeLand, Florida, United States, 32720; Miami, Florida, United States, 33125; Tampa, Florida, United States, 33634; Winter Haven, Florida, United States, 33880; Prairie Village, Kansas, United States, 66206; Boston, Massachusetts, United States, 02131; North Attleboro, Massachusetts, United States, 02760 & 02481; Wellesley, Massachusetts, United States, 02481; Minneapolis, Minnesota, United States, 55402; Brooklyn, New York, United States, 11229; Rochester, New York, United States, 14609; Dayton, Ohio, United States, 45432; Mount Pleasant, South Carolina, United States, 29464; Chattanooga, Tennessee, United States, 37421; Fort Worth, Texas, United States, 76104; and Bellevue, Washington, United States, 98007. The PREVAIL study was conducted in accordance with standards of Good Clinical Practice as defined by the International Conference on Harmonisation and all applicable federal and local regulations. All study documentation was approved by the local review board at each site or by a central institutional review board or ethics committee. All patients provided written informed consent prior to their participation in the study.
Consent for publication
Not applicable.
Competing interests
AB has served on advisory boards for AbbVie, Aeon, Alder, Amgen, Biohaven, Eaglet, Eli Lilly, Impel, Lundbeck, Novartis, Promius, Revance, Supernus, and Teva; and has received funding for speaking from AbbVie, Amgen, Avanir, Biohaven, Depomed, Eli Lilly, Impel, Lundbeck, Pernix, Promius, Supernus, and Teva. AE and BE are employees of H. Lundbeck A/S. JH is an employee of Pacific Northwest Statistical Consulting, Inc., a contracted service provider of biostatistical resources for H. Lundbeck A/S. RC was an employee of Lundbeck at the time of manuscript development.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Blumenfeld, A., Ettrup, A., Hirman, J. et al. Long-term reductions in disease impact in patients with chronic migraine following preventive treatment with eptinezumab. BMC Neurol 22, 251 (2022). https://doi.org/10.1186/s12883-022-02774-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-022-02774-3