Abstract
Background
We aimed to investigate the risk factors of early neurological deterioration (END) after intravenous thrombolysis with recombinant tissue-type plasminogen activator (rt-PA) and the relationship between END and poor 3-month functional outcomes.
Methods
Patients who accepted intravenous recombinant rt-PA were enrolled continuously. END was defined as an increase in National Institute of Health Stroke (NIHSS) score ≥ 4 points or death within 24 hours after intravenous thrombolysis. The modified Rankin Scale (mRS) score was recorded to evaluate the functional outcome of stroke, and the poor 3-month prognosis was defined as an mRS score ≥ of 3. Univariate and multivariate analyses were used to analyze the risk factors of END. The relation between END and 3-month functional outcome was analyzed by multivariate logistic regression analysis.
Results
A total of 1107 patients (mean age, 63.42 ± 11.33 years; 673 males) were included in the final analysis, and 81(7.32%) patients had END. In multivariate analysis, the serum glucose level was significantly associated with END; the odds ratio was 1.10 (95% CI 1.03 to 1.18, p = 0.004). The multivariate logistic analysis showed END has a notable association with the poor 3-month functional recovery even after adjusting for confounding factors; the adjusted OR was 8.25 (95% CI 3.77 to 18.03, p < 0.0001).
Conclusions
The initial serum glucose level might be an independent risk factor of END, and END might predict a poor 3-month prognosis.
Similar content being viewed by others
Introduction
Stroke has become one of the leading causes of death and disability in humans, and there has been a high incidence of stroke in China [1, 2]. It has been confirmed that target-vessel revascularization is the most effective method to reduce the disability and mortality of patients. Meanwhile, intravenous thrombolysis with recombinant tissue-type plasminogen activator (rt-PA) has been the most economical and convenient treatment [3]. However, some studies have found that some patients still suffered severe neurological deterioration after receiving intravenous thrombolysis, which resulted in prolonged hospitalization and severe adverse prognosis [4]. This study explored the risk factors of early neurological deterioration (END) and the correlation between END and 3-month functional prognosis.
Methods
Study population
The data were obtained from the Thrombolysis Implementation and Monitor of Acute Ischemic Stroke in China (TIMS-CHINA) database - a multicenter prospective stroke registry program that enrolled patients who received intravenous tPA within 4.5 hours after symptom onset from May 2007 to July 2012 in China [5]. Some previous pieces of literature have reported the trial design and some results of the study [6, 7]. The ethics committee approved the study protocol of Beijing Tiantan Hospital with the Helsinki Declaration. The quality monitoring committee of TIMS-China and the Contract Research Organization independently have been regularly monitoring the registry. All participants had signed written consent.
Definition of END and clinical outcome measurement
END was defined as an increase of NIHSS (National Institute of Health Stroke) score ≥ 4 points or death within 24 hours after intravenous thrombolysis [8]. The primary outcome was poor 3-month functional recovery, expressed as a modified Rankin Scale (mRS) score ≥ 3. The secondary outcomes were sICH (symptomatic intracranial hemorrhage) [9] and mortality at 7 days and 90 days. We used the definitions of sICH in the following three studies: Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST) [8], National Institute of Neurological Disorders and Stroke (NINDS) [10], and European Cooperative Acute Stroke Study II (ECASS II) [11].
Statistical analysis
Continuous variables were described by means (standard deviations [SDs]) or medians (interquartile ranges [IQRs]). Categorical variables were presented as frequencies and percentages. The baseline characteristics of patients between the END group and the non-END group were compared by Wilcoxon rank-sum tests for continuous variables and X2 test for categorical variables. Univariate and multivariate logistic regression was used to estimate the odds ratios (ORs), the corresponding 95% confidence intervals (CIs), and the adjusted ORs with their 95% CI. The multiple ordinal regression was used to test the distribution of mRS at 3-month of patients. SAS software performed all statistical analyses, version 9.4 (SAS Institute Inc., Cary, NC, USA). All P values were two-sided, with P < 0.05 considered statistically significant.
Results
Baseline characteristics
A total of 1107 consecutive patients (mean age, 63.42 ± 11.33 years; 673 males) were included in the final analysis, among which 81(7.32%) patients occurred END (Fig. 1). Between the END group and the non-END group, there were statistical differences in the history of prior stroke/TIA (2.47% vs.9.75%, p = 0.029), initial serum glucose level (9.00 ± 4.35 mmol/L vs.7.58 ± 2.87 mmol/L, p = 0.001), fibrinogen (3.47 ± 1.24 g/L vs. 3.23 ± 1.23 g/L, p = 0.040), low-density lipoprotein (3.20 ± 0.90 mmol/L vs. 2.92 ± 0.96 mmol/L, p = 0.003), cholesterol (5.08 ± 1.16 mmol/L vs. 4.85 ± 1.20 mmol/L, p = 0.021), SBP (systolic blood pressure) on admission (152.30 ± 18.56 mmHg vs. 147.57 ± 21.09 mmHg, p = 0.039), DBP (diastolic blood pressure) on admission (88.35 ± 11.86 mmHg vs. 85.70 ± 12.68 mmHg, p = 0.038), taking aspirin within 7 days before thrombolysis (38.27% vs. 65.20, p < 0.0001), and taking clopidogrel within 7 days before thrombolysis (13.58% vs. 23.59%, p = 0.039). There was no significant statistical difference in the neurological deficit on admission between the two groups. Concerning TOAST types, although the proportion of CE (cardioembolism) in the END group was higher than in the non-END group (28.21% vs. 18.69%), there was no difference in the etiology distribution between the two groups. In multivariate analysis, END has a significant correlation with the initial serum glucose level (OR,1.10, 95% CI 1.03–1.18; p = 0.004), taking aspirin within 7 days before thrombolysis (OR, 0.25, 95% CI 0.14–0.44; p < 0.0001), and taking clopidogrel within 7 days before thrombolysis (OR,0.39, 95% CI 0.19–0.82; p = 0.013). The demographics and clinical characteristics at the baseline of subjects in this study were demonstrated in Table 1, and multivariate logistic regression analysis for risk factors of END was shown in Table 2.
Clinical outcomes
During the follow-up, 23 patients were excluded because of missing, and there were 1084 patients (97.92%) who had a 3-month mRS score. The proportion of poor function outcomes is 83.54% in the END group and 37.41% in the non-END group (crude OR 8.49; 95%CI 4.62 to 15.60; P < 0.0001). After adjusting the baseline variables as the history of prior stroke/TIA, initial serum glucose level, fibrinogen, low-density lipoprotein, cholesterol, SBP on admission, DBP on admission, taking aspirin within 7 days before thrombolysis, taking clopidogrel within 7 days before thrombolysis, and TOAST types, END has a statistical correlation with poor 3-month functional outcomes, the adjusted OR was 8.25(95% CI 3.77–18.03; P < 0.0001; Table 3). There was a numerical difference in the distribution of 3-month mRS among patients in the two groups (crude p < 0.0001), and this difference was still significant after adjusting confound factors (adjusted OR 11.74, 95%CI 7.58 to 18.18; P < 0.0001; Fig. 2). Regarding the secondary outcomes, END has a prominent correlation with SICH.
And the adjusted OR (END with SICH defined by NINDS) was 12.53 (95% CI 5.15–30.49; P < 0.0001; Table 3). Meanwhile, END has a significant correlation with mortality at 7 days and mortality at 90 days, the adjusted OR was 20.92(95% CI 7.45–58.72; P < 0.0001; Table 3) and 8.06(95% CI 3.91–16.62; P < 0.0001; Table 3).
Discussion
Our study aimed to explore the risk factors of END and the relationship between END and poor 3-month functional outcomes. In some studies, the incidence of END was significantly different due to the lack of a unified definition of END, which was from 5.8 to 34.9% [12,13,14,15]. Most studies have defined END as an increasing NIHSS score ≥ 4 points or death within 24 hours after intravenous thrombolysis, which was our study’s exact definition of END [8, 16]. Our study enrolled 1107 patients accepting intravenous thrombolysis, and 81 (7.32%) patients occurred END. Simonsen et al. studied 569 patients who received reperfusion therapy and found the incidence of END was 5.8% [14].
Concerning the risk factors of END, although some experts generally believe that elderly patients are more prone to END, it has not been confirmed in some studies [10, 15]. Some studies also have demonstrated the predictors of END as follows: diabetes [17, 18], neurological functional deficits on admission [19], and systolic BP [20,21,22].
There was no statistical difference in age between the END and non- END groups. Still, there were statistical differences in the history of prior stroke/TIA, initial serum glucose level, fibrinogen, low-density lipoprotein, cholesterol, SBP on admission, and DBP on admission between the two groups. However, in the multivariate analysis, our study found the initial serum glucose level was an independent risk factor of END; the odds ratio was 1.10 (95%CI 1.03 to 1.18, p = 0.004).
Our study found that antiplatelet therapy before thrombolysis might be the protective factor for END. The incidence of END in patients taking aspirin could be 0.25 times lower than in patients without aspirin, similar to patients taking clopidogrel within 7 days. Due to the limitation of our research, we had no further study on this result, and it would be a meaningful research focus in the future.
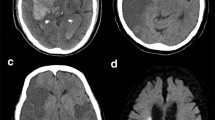
The series of pathophysiological reactions of the brain after intravenous thrombolysis, such as intracranial hemorrhage (ICH) [23, 24], malignant edema [25], early recurrent ischemic stroke [12], and early seizures [26], resulted in the aggravation of neurological deficit [20, 21]. Meanwhile, SICH had been the leading cause of END. Our study confirmed that the patients in the END group had a higher incidence of ICH than in the non-END group. The incidence of SICH (NINDS) in the END group patients could be 12.53 times higher than patients in the non-END group. Furthermore, END was significantly correlated with mortality at 7 days and mortality at 3 months. Compared the patients with non- END, the mortality at 7 days of patients with END could be 20.92 times higher, and the mortality at 3 months could be 8.06 times higher.
Our study still has some shortcomings. Firstly, our study did not analyze patients separately in anterior circulation stroke (ACS) and posterior circulation stroke (PCS) groups, which has been confirmed there was no significant difference in the incidence of END between ACS and PCS groups in a recent study [27]. Secondly, we also did not perform subgroup analysis based on the time of ICH, although we have realized that patients usually experience hemorrhagic transformation within 24 h after thrombolysis [28]. Thirdly, owing to the lack of records on other complications(i.e., hyperperfusion syndrome, early stroke recurrence) after intravenous thrombolysis, we were still unable to explain the pathological mechanism of END. Fourthly, confounding factors (i.e., mechanical ventilation, fluid resuscitation, decompressive craniectomy) were not eliminated in our study, which may lead to data bias. We look forward to furthering research in the future.
Conclusions
Early neurological deterioration has a high incidence after intravenous thrombolysis, and the initial serum glucose level might be an independent risk factor of END. END might predict a poor 3-month prognosis. It might be essential to understand the underlying mechanism of END.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
12 September 2022
A Correction to this paper has been published: https://doi.org/10.1186/s12883-022-02865-1
Abbreviations
- TIA:
-
Transient ischemic attack
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- WBC:
-
White blood cell
- PLT:
-
Platelet
- INR:
-
International normalized ratio
- PT:
-
Prothrombin time
- APTT:
-
Activated partial thromboplastin time
- FBG:
-
Fibrinogen
- NIHSS:
-
National Institute of Health Stroke
- LDL:
-
Low-density lipoprotein
- TC:
-
Cholesterol
- IQR:
-
Interquartile ranges
- TOAST:
-
Trial of Org 10,172 in Acute Stroke Treatment
- LAA:
-
Large-artery atherosclerosis
- Scale:
-
SAO, small-artery occlusion
- CE:
-
Cardioembolism
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- TIA:
-
Transient ischemic attack
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- FBG:
-
Fibrinogen
- LDL:
-
Low-density lipoprotein
- TC:
-
Cholesterol
- mRS:
-
modified Rankin Scale
- SICH:
-
Symptomatic intracranial hemorrhage
- SITS-MOST:
-
Safe implementation of treatments in stroke-monitoring
- ECASS II:
-
Second European–Australasian acute stroke study
- NINDS:
-
National Institute of Neurological Disorders and Stroke
References
GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1151–210.
Wu S, Wu B, Liu M, Chen Z, Wang W, Anderson CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18(4):394–405.
Marko M, Posekany A, Szabo S, Scharer S, Kiechl S, Knoflach M, et al. Trends of r-tPA (recombinant tissue-type plasminogen activator) treatment and treatment-influencing factors in acute ischemic stroke. STROKE. 2020;51(4):1240–7.
Thiebaut AM, Gauberti M, Ali C, Martinez De Lizarrondo S, Vivien D, Yepes M, et al. The role of plasminogen activators in stroke treatment: fibrinolysis and beyond. Lancet Neurol. 2018;17(12):1121–32.
Liao XL, Wang CX, Wang YL, Wang CJ, Zhao XQ, Zhang LQ, et al. Implementation and outcome of thrombolysis with alteplase 3 to 4.5 h after acute stroke in Chinese patients. CNS Neurosci Ther. 2013;19(1):43–7.
Liao X, Wang Y, Pan Y, Wang C, Zhao X, Wang DZ, et al. Standard-dose intravenous tissue-type plasminogen activator for stroke is better than low doses. STROKE. 2014;45(8):2354–8.
Wang C, Yang Y, Pan Y, Liao X, Huo X, Miao Z, et al. Validation of the simplified stroke-thrombolytic predictive instrument to predict functional outcomes in Chinese patients. STROKE. 2018;49(11):2773–6.
Wahlgren N, Ahmed N, Dávalos A, Ford GA, Grond M, Hacke W, et al. Thrombolysis with alteplase for acute ischaemic stroke in the safe implementation of thrombolysis in stroke-monitoring study (SITS-MOST): an observational study. LANCET. 2007;369(9558):275–82.
Zhou H, Chen W, Pan Y, Suo Y, Meng X, Li H, et al. Effect of sex differences on prognosis of intravenous thrombolysis: data from the thrombolysis implementation and monitor of acute ischemic stroke in China (TIMS-China). Stroke Vasc Neurol. 2021;6(1):10–5.
Mione G, Ducrocq X, Thilly N, Lacour JC, Vespignani H, Richard S. Outcome of intravenous recombinant tissue plasminogen activator for acute ischemic stroke in patients aged over 80 years. Geriatr Gerontol Int. 2016;16(7):843–9.
Larrue V, von Kummer RR, Müller A, Bluhmki E. Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian acute stroke study (ECASS II). STROKE. 2001;32(2):438–41.
Awadh M, MacDougall N, Santosh C, Teasdale E, Baird T, Muir KW. Early recurrent ischemic stroke complicating intravenous thrombolysis for stroke: incidence and association with atrial fibrillation. STROKE. 2010;41(9):1990–5.
Nanri Y, Yakushiji Y, Hara M, Eriguchi M, Okada R, Yukitake M, et al. Stroke scale items associated with neurologic deterioration within 24 hours after recombinant tissue plasminogen activator therapy. J Stroke Cerebrovasc Dis. 2013;22(7):1117–24.
Simonsen CZ, Schmitz ML, Madsen MH, Mikkelsen IK, Chandra RV, Leslie-Mazwi T, et al. Early neurological deterioration after thrombolysis: clinical and imaging predictors. Int J Stroke. 2016;11(7):776–82.
Huang ZX, Huang Y, Zeng J, Hao H, Petroski GF, Lu H, et al. Admission glucose levels may increase the risk for early neurological deterioration in females with acute ischemic stroke. Front Neurol. 2020;11:548892.
Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317–29.
Tanaka R, Ueno Y, Miyamoto N, Yamashiro K, Tanaka Y, Shimura H, et al. Impact of diabetes and prediabetes on the short-term prognosis in patients with acute ischemic stroke. J Neurol Sci. 2013;332(1–2):45–50.
Hong JM, Kim DS, Kim M. Hemorrhagic transformation after ischemic stroke: mechanisms and management. Front Neurol. 2021;12:703258.
Seners P, Turc G, Tisserand M, Legrand L, Labeyrie MA, Calvet D, et al. Unexplained early neurological deterioration after intravenous thrombolysis: incidence, predictors, and associated factors. STROKE. 2014;45(7):2004–9.
Chung JW, Kim N, Kang J, Park SH, Kim WJ, Ko Y, et al. Blood pressure variability and the development of early neurological deterioration following acute ischemic stroke. J Hypertens. 2015;33(10):2099–106.
Park TH, Lee JK, Park MS, Park SS, Hong KS, Ryu WS, et al. Neurologic deterioration in patients with acute ischemic stroke or transient ischemic attack. NEUROLOGY. 2020;95(16):e2178–91.
Gong P, Zhou J, Zhang Y. Letter by Gong et al regarding article, "predictors of unexplained early neurological deterioration after endovascular treatment for acute ischemic stroke". STROKE. 2021;52(1):e44–5.
Mori M, Naganuma M, Okada Y, Hasegawa Y, Shiokawa Y, Nakagawara J, et al. Early neurological deterioration within 24 hours after intravenous rt-PA therapy for stroke patients: the stroke acute management with urgent risk factor assessment and improvement rt-PA registry. Cerebrovasc Dis. 2012;34(2):140–6.
Wei XE, Zhao YW, Lu J, Li MH, Li WB, Zhou YJ, et al. Timing of recanalization and outcome in ischemic-stroke patients treated with recombinant tissue plasminogen activator. Acta Radiol. 2015;56(9):1119–26.
Battey TW, Karki M, Singhal AB, Wu O, Sadaghiani S, Campbell BC, et al. Brain edema predicts outcome after nonlacunar ischemic stroke. STROKE. 2014;45(12):3643–8.
Jung S, Schindler K, Findling O, Mono ML, Fischer U, Gralla J, et al. Adverse effect of early epileptic seizures in patients receiving endovascular therapy for acute stroke. STROKE. 2012;43(6):1584–90.
Cui Y, Meng WH, Chen HS. Early neurological deterioration after intravenous thrombolysis of anterior vs posterior circulation stroke: a secondary analysis of INTRECIS. Sci Rep. 2022;12(1):3163.
Jickling GC, Liu D, Stamova B, Ander BP, Zhan X, Lu A, et al. Hemorrhagic transformation after ischemic stroke in animals and humans. J Cereb Blood Flow Metab. 2014;34(2):185–99.
Acknowledgments
We gratefully appreciate all the participants and staff for their contributions.
Funding
The study was supported by grants from the Beijing Natural Science Foundation (Z200016).
Author information
Authors and Affiliations
Contributions
Concept and design: FC, XZ, XG, and YJ. Drafting of the manuscript: FC, YL, and XG. Critical revision of the manuscript for important intellectual content: HD, YD, and JJ. Provision of study material or patients: YL and YJ. Collection and assembly of data: FC, YL, JJ, AW, HD, YJ, YD, and XG. Check and approve of clinical definition: XG and XZ. Data analysis: FC and AW. Data interpretation: FC, AW, HD, JJ, YD, and XG. Administrative, technical, or material support: XZ and YJ. Supervision: XG and XZ. Final approval of manuscript: all authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The ethics committee of Beijing Tiantan Hospital approved this study. All study subjects had signed informed consent. We confirm that all methods in our study were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: an error was found in the affiliations 1 and 2.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Che, F., Wang, A., Ju, Y. et al. Early neurological deterioration in acute ischemic stroke patients after intravenous thrombolysis with alteplase predicts poor 3-month functional prognosis - data from the Thrombolysis Implementation and Monitor of Acute Ischemic Stroke in China (TIMS-China). BMC Neurol 22, 212 (2022). https://doi.org/10.1186/s12883-022-02737-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-022-02737-8