Abstract
Background
Few studies focused on the functional outcomes of patients at 3 months after receiving intravenous thrombolysis, anticoagulation, or antiplatelet therapy within 4.5 h of onset of the cardiogenic cerebral embolism (CCE) subtype.
Methods
The purpose of this retrospective study was to analyse the clinical data of patients with acute CCE and compare the 3-month functional prognoses of patients after administration of different antithrombotic therapies within 4.5 h of stroke onset. A total of 335 patients with CCE hospitalized in our institution were included in this study. The patients were stratified according to the hyperacute treatment received, and baseline clinical and laboratory data were analysed. A 3-month modified Rankin scale (mRS) score of 0–2 was defined as an excellent functional outcome.
Results
A total of 335 patients were divided into thrombolytic (n = 78), anticoagulant (n = 88), and antiplatelet therapy groups (n = 169). A total of 164 patients had a good prognosis at 3 months (mRS ≤ 2). After adjustments were made for age and National Institute of Health Stroke Scale (NIHSS) score, each group comprised 38 patients, and there were no significant differences in sex composition, complications, lesion characteristics, or Oxfordshire Community Stroke Project (OSCP) classification among the three groups. The plasma D-dimer level (µg/ml) in the thrombolytic group was significantly higher than those in the anticoagulant and antiplatelet groups [3.07 (1.50,5.62), 1.33 (0.95,1.89), 1.61 (0.76,2.96), P < 0.001]. After one week of treatment, the reduction in NIHSS in the thrombolytic group was significantly greater than those in the other two groups [3.00 (1.00, 8.00), 1.00 (0.00, 5.00), 1.00 (0.00, 2.00), P = 0.025]. A total of 47 patients (41.2 %) had an mRS score of ≤ 2 at 3 months, and 23 patients died (20.2 %). There was no significant difference in the proportion of patients with a good prognosis or the mortality rate among the three groups (P = 0.363, P = 0.683).
Conclusions
Thrombolytic therapy is effective at improving short-term and 3-month prognoses. Anticoagulant therapy may be a safe and effective treatment option for patients with the cardiac stroke subtype who fail to receive intravenous recombinant tissue plasminogen activator (r-tPA) thrombolysis within 4.5 h in addition to antiplatelet therapy, as recommended by the guidelines.
Similar content being viewed by others
Background
Approximately one-fourth of ischaemic strokes are caused by abnormal cardiac structure or function, namely, cardiogenic cerebral embolism (CCE) [1]. The most common cause of CCE is non-valvular atrial fibrillation (NVAF) [2]. Compared with those who have other ischaemic stroke subtypes, patients with CCE have more serious symptoms, poorer prognoses, higher mortality and a higher risk of recurrence or haemorrhagic conversion early after stroke onset [3, 4]. Hyperacute treatment strategies are crucial for improving patient prognosis. For patients whose onset times are within the treatment window, thrombolysis treatment, arterial embolectomy, and bridging therapy are recommended by the American Heart Association/American Stroke Association (AHA/ASA) and European Society of Cardiology (ESC) guidelines [5, 6], and antiplatelet therapy is suggested during the hyperacute stage of CCE [5, 6]; however, the effectiveness of hyperacute anticoagulation remains controversial.
To provide a corresponding clinical reference for CCE subtypes, we retrospectively analysed the clinical characteristics of patients with CCE and compared their 3-month clinical prognoses after receiving different antithrombotic drugs within 4.5 h of stroke onset using data from patients who did not receive either arterial embolectomy or bridging therapy but only drug treatment.
Methods
Patient recruitment and criteria
From December 2011 to December 2016, a total of 369 patients with CCE (within 4.5 h of onset) were hospitalized at the Department of Neurology, the Second Affiliated Hospital of Soochow University in Suzhou, China. The follow-up period was 3 months. The study protocol was approved by the Ethics Committee of the Second Affiliated Hospital of Soochow University. Consent to use patient data for clinical analysis was obtained verbally by telephone from the patient or his or her family, and then an informed consent form was signed by the investigators and the patient or his or her family face to face. Patients satisfying the following criteria were enrolled: (1) age > 18 years; (2) average time from onset to admission ≤ 4.5 h; (3) craniocerebral magnetic resonance imaging (MRI) or computed tomography (CT) performed to confirm a diagnosis of new cerebral infarction; (4) diagnostic criteria met for cardiogenic embolism according to Trial of Org 10,172 in the Acute Stroke Treatment (TOAST) classification [7]; and (5) heart disease defined as NVAF with a history of atrial fibrillation of more than 1 month without medication or cardioversion, failure to undergo drug or electrical cardioversion, sinus rhythm that could not be maintained for an extended time, definite dilated heart disease, or rheumatic valvular heart disease. Patients were excluded based on the following criteria: (1) allergy or obvious contraindications to therapeutic drugs, such as recombinant tissue plasminogen activator (r-tPA), warfarin, argatroban, aspirin, clopidogrel, cilostazol, and dabigatran etexilate capsules; (2) a pre-existing haematological disease or an obvious bleeding tendency; (3) severe liver and kidney dysfunction; (4) severe infection; (5) unwillingness to participate and undergo follow-up visits; (6) arterial embolectomy or bridging treatment; (7) gastrointestinal bleeding or gross haematuria; (8) head CT suggesting cerebral haemorrhage at admission; and (9) other stroke subtypes by intracranial and external vascular examinations, imaging or laboratory examinations.
Finally, 335 patients with CCE were stratified into thrombolytic (n = 78), anticoagulant (n = 88), or antiplatelet (n = 169) treatment groups according to the specific drug received within 4.5 h of stroke onset.
Treatment plan, medication, and monitoring
For thrombolytic therapy, the r-tPA dose was 0.9 mg/kg, with the total dose not exceeding 90 mg. Re-examination by head CT was performed 24 h after administration of thrombolytic treatment and if the patient’s condition changed or before discharge. The antithrombotic regimen at 24 h after thrombolysis was as follows: 1) anticoagulant therapy: (i) 1.25 mg or 1.875 mg warfarin daily with review every 3–5 d using a target international normalized ratio (INR) between 2.0 and 3.0 or (ii) 110 mg dabigatran twice daily, and 2) antiplatelet therapy: (i) 100 mg aspirin daily; (ii) 75 mg clopidogrel daily; (iii) 50 mg cilostazol twice daily; (iv) 100 mg aspirin and 75 mg clopidogrel daily; or (v) 50 mg cilostazol twice daily with 75 mg clopidogrel daily.
For the anticoagulant group, the anticoagulation schemes were as follows: (i) 10 mg argatroban every 4 h for 2 d followed by 10 mg twice daily for 5 d for a total of 7 d or 10 mg argatroban twice daily for 7 d, followed by selection of an individualized antithrombotic regimen; (ii) 1.25 mg or 1.875 mg warfarin daily with review every 3–5 d using a target INR between 2.0 and 3.0; or (iii) 110 mg dabigatran twice daily. Re-examination by head CT was performed if the patient’s condition changed or before discharge; re-examination occurred at least once during hospitalization.
For antiplatelet therapy, the regimens were (i) 100 mg aspirin daily; (ii) 75 mg clopidogrel daily; (iii) 50 mg cilostazol twice daily; (iv) 100 mg aspirin and 75 mg clopidogrel daily; and (v) 50 mg cilostazol twice daily with 75 mg clopidogrel daily. Re-examination head CT was performed if the patient’s condition changed or before discharge; re-examination was performed at least once during hospitalization.
Patient baseline and clinical characteristics
The following information was collected for each patient: (i) general demographic data (age and sex); (ii) clinical indicators, including aetiology of cerebral embolism (NVAF, rheumatic heart valvular disease, and dilated cardiomyopathy) and concomitant diseases (hypertension, diabetes, prior stroke history, and prior non-cerebrovascular events); (iii) Oxfordshire Community Stroke Project (OCSP) classification [8] with complete anterior circulation (TACI), partial anterior circulation (PACI), posterior circulation (POCI), and lacunar nature (LACI); (iv) laboratory indices, including INR, plasma D-dimer level, C-reactive protein (CRP) level, and serum creatinine (Scr) level; (v) severity, safety, and risk indicators, such as NIHSS at admission and after 1 week of treatment and CHADS2, CHADS2-VASc and HAS-BLED scores; and (vi) prognostic indicators, including the haemorrhagic transformation [9] rate during hospitalization and modified Rankin scale (mRS) score at the 3-month follow-up.
Statistical methods
All the statistical analyses were performed using SPSS Statistics for Windows version 17.0 (SPSS Inc., Chicago, IL, USA) and R version 4.0.2. Normal distributions are expressed as the mean ± standard deviation (SD). Student’s t-test was used to compare two groups, and one-way ANOVA was used for comparisons among the three groups. Skewed measurements are expressed as the median and interquartile range [M (IQR)]. The nonparametric rank-sum test was used for comparisons, post hoc analyses were performed, and pairwise comparisons were performed using the Wilcoxon test with the Bonferroni correction. Count data are expressed as percentages and were compared by means of two-tailed Student’s t-test or Fisher’s exact test. Statistically significant differences were defined as P-values < 0.05.
The age and NIHSS indices of the three groups were used as the benchmark to match each group so that the baseline data of the three groups were unified and comparable and bias was eliminated. Propensity score matching (PSM) was used to unify the baseline data of each group. The calliper value selected was 0.02 and matched according to the 1:1 nearest neighbour matching method.
Results
Comparison of baseline data and metrics among the CCE-treated subgroups
Our cohort of 335 patients with CCE was divided into three groups according to the therapy adopted within 4.5 h of stroke onset: the thrombolytic (n = 78), anticoagulant (n = 88), and antiplatelet (n = 169) groups. Baseline characteristics are shown in Table 1. The mean ages of the thrombolytic, anticoagulant, and antiplatelet groups were 72.81 ± 8.02, 71.28 ± 9.74, and 76.80 ± 8.41 years, respectively (P < 0.001). We found no sex differences among the cohorts, with 39 (50.0 %), 43 (48.9 %), and 77 (45.6 %) males in the thrombolytic, anticoagulant, and antiplatelet groups, respectively (P = 0.773).
There were 75 (96.2 %), 75 (85.2 %), and 161 (95.3 %) cases of NVAF in the thrombolytic, anticoagulant, and antiplatelet groups, respectively, according to the aetiology of the cerebral embolism (P = 0.005). Rheumatic valvular disease ranked second to NVAF. In addition, hypertension was the most common accompanying disease, with 69 (88.5 %), 62 (70.5 %), and 133 (78.7 %) cases in the thrombolytic, anticoagulant, and antiplatelet groups, respectively (P = 0.018). We also found no significant differences in OCSP classification among the three groups (TACI: P = 0.174; PACI: P = 0.949; POCI: P = 0.743; and LACI: P = 0.059). Regarding the biochemical indices, we found that plasma D-dimer levels were different among the three groups (P = 0.002), that the D-dimer polymer level was the highest in the thrombolytic group, and that there were no significant differences in CRP levels among the groups (P = 0.406).
Comparison of rating scales, complications, treatments, and patient prognoses
The median NIHSS scores at admission were 14.00 (10.00,19.00), 9.50 (3.00,13.00), and 8.00 (3.00,15.00) for the thrombolytic, anticoagulant, and antiplatelet groups, respectively (P < 0.001); however, we found no significant differences in the NIHSS scores after one week of treatment among the three groups (P = 0.059; Table 2). After one week of treatment, the reductions in the NIHSS scores [3.00 (1.00, 9.00), 1.00 (0.00, 3.00), 1.00 (0.00, 2.00), P < 0.001] were improved most significantly in the thrombolytic group. Current guidelines [10, 11] recommend using the risk stratification schema congestive heart failure, hypertension, age, diabetes, prior stroke (CHADS2) and congestive heart failure, hypertension, age, diabetes, prior stroke, vascular disease, sex (CHA2DS2-VASc) as secondary prevention for patients with atrial fibrillation. However, the threshold value for predicting the prognosis of CCE is unknown, so we evaluated the CHADS2 and CHA2DS2-VASc scores of the patients in the three groups. We found that the CHADS2 and CHA2DS2-VASc scores were significantly different among the three groups (P = 0.005, P < 0.001, respectively); similarly, the hypertension, abnormal renal and liver function, stroke, bleeding, labile international normalized ratio, elderly age, drugs or alcohol (HAS-BLED) scores of the three groups were all ≥ 3.
Next, we evaluated the haemorrhagic transformation rate of patients with CCE in the acute stage (during hospitalization) and found that it was high. There were 26 cases (7.8 %) of intracranial haemorrhagic transformation, with 13 cases in the thrombolytic group (16.7 %), 4 cases in the anticoagulation group (4.5 %), and 9 cases in the antiplatelet group (5.3 %) (P = 0.003); 2 patients in the thrombolytic group had symptomatic intracranial haemorrhage [11], and 1 of these two patients died. There were 4 cases of extracranial haemorrhage among the 335 patients (1.2 %, P = 0.316).
A total of 164 patients (49.0 %) in our cohort had a good prognosis at 3 months (mRS ≤ 2), namely, 30 patients (38.5 %) in the thrombolytic group, 53 patients (60.2 %) in the anticoagulant group, and 81 patients (47.9 %) in the antiplatelet group (P = 0.018; Table 2).
Comparison of baseline data and metrics among the CCE-treated subgroups after PSM
The age and NIHSS indices of the three groups were used as the benchmarks to match each group. After PSM, each group had 38 patients. The mean ages of the patients in the thrombolytic, anticoagulant, and antiplatelet groups were 73.53 ± 6.88, 72.05 ± 8.44, and 76.34 ± 9.30, respectively (P = 0.076), and the numbers of male patients were 18 (47.4 %), 18 (47.4 %), and 20 (52.6 %), respectively (P = 0.869). There were no significant differences in the proportion of NVAF or rheumatic valvular heart disease among the three groups, and there were no patients with dilated cardiomyopathy among the groups. There were no significant differences in the incidences of diabetes mellitus (P = 0.074), hypertension (P = 0.220), history of stroke (P = 0.390), or previous peripheral vascular and cardiovascular events (P = 0.365) among the three groups. Similarly, there was no significant difference in the lesion characteristics or OSCP classification among the three groups.
Regarding biochemical indices, the level of the plasma D-dimer polymer was significantly increased in the thrombolytic group, with values of 3.07 (1.50, 5.62), 1.33 (0.95, 1.89), and 1.61 (0.76, 2.96) for the thrombolytic, anticoagulant and antiplatelet groups, respectively (P < 0.001). There were no significant differences in the INR (P = 0.697) or the levels of Scr (P = 0.504), Hcy (P = 0.234), or CRP (P = 0.523) among the groups (Table 3).
Comparison of rating scales, complications, treatments, and patient prognoses after PSM
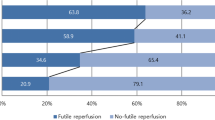
The CHASD2 scores of the three groups all indicated which patients had a high risk of embolism, and the CHASD2 score was highest in the antiplatelet group (P = 0.04); however, there were no significant differences in the CHASD2-VASc scores among the three groups (P = 0.142). The HAS-BLED scores indicated patients with a high bleeding risk, but there were no significant differences among the three groups (P = 0.073). After PSM, the NIHSS scores of the thrombolytic, anticoagulant, and antiplatelet groups were 11.00 (9.00, 13.75), 13.00 (9.00, 15.00), and 13.00 (5.25, 16.00) (P = 0.768), respectively, and the NIHSS reductions after 1 week were 3.00 (1.00, 8.00), 1.00 (0.00, 5.00), and 1.00 (0.00, 2.00), respectively (P = 0.025). Among the three groups, the improvement was greatest in the thrombolytic group (n = 38, each group). Eleven patients had intracranial haemorrhage conversion, namely, 6 patients in the thrombolytic group, 2 patients in the anticoagulant group, and 3 patients in the antiplatelet group (P = 0.281), yet all the patients were asymptomatic. At the same time, there were no extracranial bleeding events in the three groups. There were no significant differences in the proportion of patients with good prognoses at 3 months (mRS ≤ 2) or the number of deaths at 3 months among the three groups (P = 0.363; P = 0.683) (Table 4).
Discussion
CCE accounts for 14–30 % of all cases of ischaemic stroke [12]. The mortality and disability rate of patients with acute cardiogenic stroke can be as high as 50 % [13]. Currently, r-tPA thrombolysis and antiplatelet therapy are recommended for all types of acute ischaemic stroke (including CCE) [5, 6] within 4.5 h of stroke onset; however, anticoagulation therapy in the hyperacute stage of CCE remains a subject of considerable debate. No previous studies have explored the relationship between different anti-thrombolytic regimens and prognosis within 4.5 h of stroke onset in CCE patients. For the first time, we retrospectively observed the 3-month functional prognoses of 335 CCE patients who received thrombolytic, anticoagulant, or antiplatelet regimens within 4.5 h of stroke onset.
The results of this study showed that among the 335 cases, 38.5 % of patients in the thrombolytic group, 60.2 % of patients in the anticoagulant group, and 47.9 % of patients in the antiplatelet group had a good prognosis (mRS ≤ 2) at 3 months (P = 0.018). However, after adjustments for age and NIHSS score, there was no difference in the number of patients with an mRS score of ≤ 2 among the groups at 3 months (n = 38). Although the thrombolysis group showed no differences compared to the other two groups in terms of improving disability at 3 months, the reduction in the NIHSS score after 1 week in the thrombolytic group was greater than that in the other two groups (P < 0.001), indicating that thrombolysis can significantly improve the short-term prognosis of patients with CCE.
Symptomatic intracranial haemorrhage transformation (sICH) is an important factor affecting the prognosis of patients with CCE. Of the 335 patients, 13 (16.7 %) patients in the thrombolysis group experienced intracranial haemorrhagic transformation during hospitalization, only 2 (2.56 %) of whom had sICH, with 1 patient dying suddenly. There were no cases of sICH in the anticoagulant or antiplatelet groups. After PSM, although there was no significant difference in the conversion rate of intracranial haemorrhage among the three groups (P = 0.281), there was still a higher chance of intracranial haemorrhage conversion in the thrombolytic group and 1 patient with sICH in this group. This may also be the reason why the good prognosis of the thrombolytic group at 3 months was not different from that of the other two groups.
In recent years, clinicians have been exploring biological indices as prognostic predictive factors. D-dimer is a specific cross-linked fibrin degradation product, and it is a sensitive biomarker for indicating coagulation and fibrinolytic activation [14]. Studies have shown that D-dimer polymer levels in patients with AF are higher than those in normal controls [15,16,17] and that D-dimer levels remain an independent predictor of unfavourable functional outcomes and mortality [18]. Elevated plasma D-dimer levels on admission are significantly associated with a poor outcome of acute ischaemic stroke, and the best discriminating factor for poor outcome is a plasma D-dimer level ≥ 3.15 µg/ml [19]. In our study (n = 335), the D-dimer level of the thrombolytic group was significantly higher than that of the other two groups (P = 0.002). Specifically, after PSM, the D-dimer levels of the thrombolytic, anticoagulant, and antiplatelet groups were 3.07 µg/ml (1.50, 5.62), 1.33 (0.95, 1.89), and 1.61 (0.76, 2.96), respectively (P < 0.001). The mean value of the thrombolytic group was 3.07 µg/ml, which was close to the cut-off value for a poor prognosis reported in the previous literature [19].
The D-dimer polymer level of the thrombolytic group was significantly higher than that of the other two groups. This was thought to indicate that the thrombolytic group would have a worse outcome, but the prognosis of the thrombolytic group at 3 months was not inferior to that of the other two groups. This finding conversely indicated that thrombolysis can improve functional outcomes at 3 months, consistent with NINDS [13] and ECASS II [9], and that a higher D-dimer level in the thrombolytic group led to a worse outcome, negatively affecting the advantages of thrombolytic treatment.
Two studies, namely, the European Atrial Fibrillation Trial (EAFT) [20] and Studio Italiano Fibrillation Atriale (SIFA) [21], confirmed the safety of warfarin administration during the acute phase of CCE. Furthermore, four randomized control trials [22,23,24,25] showed that the bleeding risk of new non-vitamin K antagonist oral anticoagulants is lower than that of warfarin and that these drugs work quickly, exhibiting an anticoagulant effect that is either superior or comparable to that of warfarin. To date, there have been few small-sample exploratory and observational studies of the use of novel anticoagulants in patients with mild-to-medium acute ischaemic stroke related to NVAF [26,27,28,29]. In this retrospective study, the median score of the anticoagulant group was 9.5. We chose to initiate anticoagulation within 4.5 h, which is earlier than the EHRS “1–3–6–12 day” rule [30] and the ASA/AHA “4–14 day” recommendation [5]. Intracranial haemorrhage conversion secondary to ultra-early anticoagulation is the most concerning problem for clinicians; however, in our study, transformation of intracranial haemorrhage occurred in only 4 of 88 patients who received anticoagulant therapy within 4.5 h. After PSM, only 2 of 38 patients experienced transformation of intracranial haemorrhage, and all of these patients exhibited asymptomatic patchy bleeding, not intracranial parenchymal haematoma or non-major bleeding events; furthermore, there were no extracranial bleeding events. In this study, the functional prognosis of the anticoagulant group at 3 months was similar to that of the thrombolytic group. The treatment benefits were speculated to be derived from two aspects: the type of anticoagulant used and the time to anticoagulation initiation. Regarding the anticoagulant type, intravenous argatroban (a direct thrombin inhibitor) is the most common treatment approach, followed by dabigatran anticoagulants instead of controversial heparins, low-molecular-weight heparin and heparinoids. The safety and efficacy of argatroban have been demonstrated in a number of studies [31,32,33,34,35]. New anticoagulants act quickly to reduce the risk of bleeding, which consequently improves prognosis. Regarding the time to anticoagulation initiation, previous studies have reported that blood-brain barrier (BBB) destruction is an independent predictor of haemorrhagic transformation and malignant oedema in patients with acute ischaemic stroke [36, 37]. In this study, anticoagulation was initiated within 4.5 h, when BBB damage was minimal and reversible, so the rate of bleeding conversion was low, the reperfusion injury caused by early anticoagulation was mild, and anticoagulant therapy could reduce small and moving thrombi [38]. These may be important reasons why the good prognosis at 3 months in the anticoagulant group in this study was not inferior to that in the thrombolytic group or the antiplatelet group. Currently, the time between the acute phase and secondary prevention has gradually blurred. Given the above findings, we recommend that for some patients with CCE who fail to receive intravenous thrombolytic therapy within 4.5 h, clinicians may consider new novel anticoagulants an effective option. Our future research directions aim to observe the changes in the dynamic BBB and its relationship with prognosis in patients with CCE treated with novel anticoagulants at the hyperacute stage.
At present, the guidelines for the acute phase of CCE anticoagulation with respect to starting time are still inconclusive, and exploratory research is encouraged. This study found that the risk of anticoagulation bleeding in patients with CCE within 4.5 h is not high, which may remind us that in addition to the guideline-recommended anticoagulation time frame (1-3-6-12 days, 4–14 days), 4.5 h may be another time point to start anticoagulation. It must be mentioned that our study is a single-centre study with a small sample size, and more studies are needed to confirm the findings.
Antiplatelet therapy is an important treatment option for CCE patients in the acute phase. The results of randomized controlled studies, namely, IST [39], CAST [40], CHANCE [41], and POINT [42], established the role of aspirin in the treatment of ischaemic stroke during the acute phase. In our study, of 335 patients, 169 chose antiplatelet therapy within 4.5 h, and 9 underwent intracranial haemorrhage transformation (5.3 %); all were asymptomatic, and 2 experienced extracranial haemorrhage (1.2 %). After adjustments were made for age and NIHSS score, there was no significant difference in the incidences of intracranial or extracranial haemorrhage between the antiplatelet group and the other two groups. In this study, initiating antiplatelet therapy within 4.5 h did not lead to a better outcome in terms of safety than thrombolysis and anticoagulation. Although the incidence of bleeding is not high, the risk of bleeding due to antiplatelet therapy should not be ignored by clinicians or patients. According to the results of this study, there was no significant difference in 3-month functional outcomes between the antiplatelet therapy group and the other two groups.
The data in this study showed that the proportion of patients with anticoagulant prophylaxis for CCE was very low from 2011 to 2016, which is very frustrating and concerning. With the popularity of new anticoagulants and the development of anticoagulant prophylactic treatment, the proportion of CCE patients choosing anticoagulants for secondary prevention is gradually increasing.
Our study has a number of limitations. It is a single-centre, retrospective study with a modest sample size, but it is a study of real-world CCE. Future multicentre, prospective, randomized controlled trials with large patient cohorts are warranted.
Conclusions
Thrombolytic therapy should be the first-line therapy for CCE patients within 4.5 h of stroke onset. For patients who fail to receive intravenous r-tPA thrombolysis within this time window, hyperacute anticoagulant therapy may be an available option as well as antiplatelet therapy.
Availability of data and materials
All the summarized and analysed data during this study are included in this published article; the original data in this study are available from the corresponding author upon reasonable request.
Abbreviations
- CCE:
-
Cardiogenic cerebral embolism
- CHA2DS2-VASc:
-
Congestive heart failure, hypertension, age, diabetes, prior stroke, vascular disease, sex
- CHADS2:
-
Congestive heart failure, hypertension, age, diabetes, prior stroke
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- EAFT:
-
European Atrial Fibrillation Trial
- HAS-BLED:
-
Hypertension, abnormal renal and liver function, stroke, bleeding, labile international normalized ratio, elderly age, drugs or alcohol
- Hcy:
-
Homocysteine
- INR:
-
International normalized ratio
- IQR:
-
Interquartile range
- LACI:
-
Lacunar cerebral infarction
- M:
-
Median
- MRI:
-
Magnetic resonance imaging
- mRS:
-
Modified Rankin scale
- NIHSS:
-
National Institutes of Health Stroke Scale
- NVAF:
-
Non-valvular atrial fibrillation
- OCSP:
-
Oxfordshire Community Stroke Project
- PACI:
-
Partial anterior cerebral infarction
- POCI:
-
Posterior cerebral infarction
- r-tPA:
-
Recombinant tissue plasminogen activator
- Scr:
-
Serum creatinine
- SIFA:
-
Studio Italiano Fibrillation Atriale
- TACI:
-
Total anterior cerebral infarction
- TTR:
-
Time treatment range
References
Ferro JM. Cardioembolic stroke: an update[J]. Lancet Neurol. 2003;2(3):177–88. DOI:https://doi.org/10.1016/s1474-4422(03)00324-7.
Arboix A, Alió J. Acute cardioembolic stroke: an update[J]. Expert Rev Cardiovasc Ther. 2011;9(3):367–79. DOI:https://doi.org/10.1586/erc.10.192.
Hart RG, Coull BM, Hart D. Early recurrent embolism associated with nonvalvular atrial fibrillation: a retrospective study[J]. Stroke. 1983;14(5):688–93. DOI:https://doi.org/10.1161/01.str.14.5.688.
D’Amelio M, Terruso V, Famoso G, et al. Early and late mortality of spontaneous hemorrhagic transformation of ischemic stroke[J]. J Stroke Cerebrovasc Dis. 2014;23(4):649–54. DOI:https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.06.005.
Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association[J]. Stroke, 2019,50(12):e344–4e418. DOI:https://doi.org/10.1161/STR.0000000000000211.
Steffel J, Verhamme P, Potpara TS, et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation: executive summary[J]. Europace. 2018;20(8):1231–42. DOI:https://doi.org/10.1093/europace/euy054.
Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment[J]. Stroke. 1993;24(1):35–41. DOI:https://doi.org/10.1161/01.str.24.1.35.
Kim YD, Hong HJ, Cha MJ, et al. Determinants of infarction patterns in cardioembolic stroke[J]. Eur Neurol. 2011;66(3):145–50. DOI:https://doi.org/10.1159/000330563.
Hacke W, Kaste M, Fieschi C, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators[J]. Lancet. 1998;352(9136):1245–51. DOI:https://doi.org/10.1016/s0140-6736(98)08020-9.
Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventriculararrhythmias and the prevention of sudden cardiac death–executive summary: A report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death) Developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society[J]. Eur Heart J, 2006,27(17):2099–140. https://doi.org/10.1093/eurheartj/ehl199.
European Heart Rhythm Association, European Association for Cardio-Thoracic Surgery. Camm AJ, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC)[J]. Eur Heart J, 2010,31(19):2369–429. DOI:https://doi.org/10.1093/eurheartj/ehq278.
Arboix A, Alió J. Cardioembolic stroke: clinical features, specific cardiac disorders and prognosis[J]. CurrCardiol Rev. 2010;6(3):150–61. DOI:https://doi.org/10.2174/157340310791658730.
National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke[J]. N Engl J Med. 1995;333(24):1581–7. DOI:https://doi.org/10.1056/NEJM199512143332401.
Tripodi A. D-dimer testing in laboratory practice[J]. Clin Chem. 2011;57(9):1256–62. DOI:https://doi.org/10.1373/clinchem.2011.166249.
Weymann A, Sabashnikov A, Ali-Hasan-Al-Saegh S, et al. Predictive Role of Coagulation, Fibrinolytic, and Endothelial Markers in Patients with Atrial Fibrillation, Stroke, and Thromboembolism: A Meta-Analysis, Meta-Regression, and Systematic Review[J]. Med Sci Monit Basic Res. 2017;23:97–140. DOI:https://doi.org/10.12659/MSMBR.902558.
Sadanaga T, Mitamura H, Fukuda K, et al. D-dimer levels positively correlate with B-type natriuretic peptide levels in patients with atrial fibrillation[J]. Int J Cardiol. 2012;158(1):110–1. DOI:https://doi.org/10.1016/j.ijcard.2012.04.079.
Thulin Å, Lindbäck J, Granger CB, et al. Extracellular vesicles in atrial fibrillation and stroke[J]. Thromb Res. 2020;193:180–9. DOI:https://doi.org/10.1016/j.thromres.2020.07.029.
Yang XY, Gao S, Ding J, et al. Plasma D-dimer predicts short-term poor outcome after acute ischemic stroke[J]. PLoS One. 2014;9(2):e89756. DOI:https://doi.org/10.1371/journal.pone.0089756.
You LR, Tang M. The association of high D-dimer level with high risk of ischemic stroke in nonvalvular atrial fibrillation patients: A retrospective study[J]. Medicine. 2018;97(43):e12622. DOI:https://doi.org/10.1097/MD.0000000000012622.
Secondary prevention in. non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. EAFT (European Atrial Fibrillation Trial) Study Group[J]. Lancet. 1993;342(8882):1255–62.
Morocutti C, Amabile G, Fattapposta F, et al. Indobufen versus warfarin in the secondary prevention of major vascular events in nonrheumatic atrial fibrillation. SIFA (Studio ItalianoFibrillazioneAtriale) Investigators[J]. Stroke. 1997;28(5):1015–21. DOI:https://doi.org/10.1161/01.str.28.5.1015.
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation[J]. N Engl J Med. 2009;361(12):1139–51. DOI:https://doi.org/10.1056/NEJMoa0905561.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation[J]. N Engl J Med. 2011;365(10):883–91. DOI:https://doi.org/10.1056/NEJMoa1009638.
Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation[J]. N Engl J Med. 2011;365(11):981–92. DOI:https://doi.org/10.1056/NEJMoa1107039.
Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation[J]. N Engl J Med. 2013;369(22):2093–104. DOI:https://doi.org/10.1056/NEJMoa1310907.
Hong KS, Kwon SU, Lee SH, et al. Rivaroxaban vs Warfarin Sodium in the Ultra-Early Period After Atrial Fibrillation-Related Mild Ischemic Stroke: A Randomized Clinical Trial[J]. JAMA Neurol. 2017;74(10):1206–15. DOI:https://doi.org/10.1001/jamaneurol.2017.2161.
Macha K, Volbers B, Bobinger T, et al. Early Initiation of Anticoagulation with Direct Oral Anticoagulants in Patients after Transient Ischemic Attack or Ischemic Stroke[J]. J Stroke Cerebrovasc Dis. 2016;25(9):2317–21. DOI:https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.06.031.
Gioia LC, Kate M, Sivakumar L, et al. Early Rivaroxaban Use After Cardioembolic Stroke May Not Result in Hemorrhagic Transformation: A Prospective Magnetic Resonance Imaging Study[J]. Stroke. 2016;47(7):1917–9. DOI:https://doi.org/10.1161/STROKEAHA.116.013491.
Deguchi I, Tanahashi N, Takao M. Timing of Treatment Initiation With Oral Anticoagulants for Acute Ischemic Stroke in Patients With Nonvalvular Atrial Fibrillation[J]. Circ J. 2017;81(2):180–4. DOI:https://doi.org/10.1253/circj.CJ-16-0923.
Heidbuchel H, Verhamme P, Alings M, et al. EHRA practical guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation: executive summary[J]. Eur Heart J. 2013;34(27):2094–106. DOI:https://doi.org/10.1093/eurheartj/eht134.
Cossy J, Belotti D. A short synthesis of argatroban. a potent selective thrombin inhibitor[J]. Bioorg Med Chem Lett. 2001;11(15):1989–92. DOI:https://doi.org/10.1016/s0960-894x(01)00351-1.
Huang P, He XY, Xu M. Effect of Argatroban Injection on Clinical Efficacy in Patients with Acute Cerebral Infarction: Preliminary Findings[J]. Eur Neurol. 2021;84(1):38–42. DOI:https://doi.org/10.1159/000512813.
Berekashvili K, Soomro J, Shen L, et al. Safety and Feasibility of Argatroban, Recombinant Tissue Plasminogen Activator, and Intra-Arterial Therapy in Stroke (ARTSS-IA Study)[J]. J Stroke Cerebrovasc Dis. 2018;27(12):3647–51. DOI:https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.08.036.
Barreto AD, Ford GA, Shen L, et al Randomized. Multicenter Trial of ARTSS-2 (Argatroban With Recombinant Tissue Plasminogen Activator for Acute Stroke)[J]. Stroke. 2017;48(6):1608–16. DOI:https://doi.org/10.1161/STROKEAHA.117.016720.
Bath PM. The argatroban and tissue-type plasminogen activator stroke study: final results of a pilot safety study[J]. Stroke. 2012;43(3):623–4. DOI:https://doi.org/10.1161/STROKEAHA.111.640557.
Rosenberg GA, Yang Y. Vasogenic edema due to tight junction disruption by matrix metalloproteinases in cerebral ischemia[J]. Neurosurg Focus. 2007;22(5):E4. DOI:https://doi.org/10.3171/foc.2007.22.5.5.
Hom J, Dankbaar JW, Soares BP, et al. Blood-brain barrier permeability assessed by perfusion CT predicts symptomatic hemorrhagic transformation and malignant edema in acute ischemic stroke[J]. AJNR Am J Neuroradiol. 2011;32(1):41–8. DOI:https://doi.org/10.3174/ajnr.A2244.
Yasaka M, Yamaguchi T, Miyashita T, et al. Regression of intracardiac thrombus after embolic stroke[J]. Stroke. 1990;21(11):1540–4. DOI:https://doi.org/10.1161/01.str.21.11.1540.
The International Stroke Trial (IST). a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. International Stroke Trial Collaborative Group[J] Lancet. 1997;349(9065):1569–81.
CAST. randomised placebo-controlled trial of early aspirin use in 20,000 patients with acute ischaemic stroke. CAST (Chinese Acute Stroke Trial) Collaborative Group[J]. Lancet. 1997;349(9066):1641–9.
Wang Y, Johnston SC, Wang Y. Clopidogrel with aspirin in minor stroke or transient ischemic attack[J]. N Engl J Med. 2013;369(14):1376–7. DOI:https://doi.org/10.1056/NEJMc1309713.
Johnston SC, Easton JD, Farrant M, et al. Clopidogrel and Aspirin in Acute Ischemic Stroke and High-Risk TIA[J]. N Engl J Med. 2018;379(3):215–25. DOI:https://doi.org/10.1056/NEJMoa1800410.
Acknowledgements
We appreciate professor Chunfeng Liu for giving valuable advice to enhance the integrity of this article during revision.
Funding
This study was supported by the Discipline Construction Program of the Second Affiliated Hospital of Soochow University (Grant No: XKTJ-XK202001 and XKTJ-TD202004) and the Diagnosis and Treatment Technology for Key Clinical Diseases in Suzhou (Grant No: LCZX201806). The funding bodies did not play a role in the collection, analysis, and interpretation of the data. The funding bodies did not contribute to the writing of this manuscript.
Author information
Authors and Affiliations
Contributions
HL had full access to the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis; drafting of the manuscript; and statistical analysis. CYJ was involved in the study conception and design; administrative, technical, and material support; study supervision; and critical revision of the manuscript for important intellectual content. DGX and XY were involved in the acquisition, analysis, and interpretation of the data. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Soochow University, and all the participants provided informed verbal and written consent. We obtained verbal consent from the patient or his or her immediate family members by telephone and written consent in a face-to-face situation, and the Ethics Committee approved this procedure.
Consent for publication
Written informed consent for publication was obtained from all the participants. All the authors agreed to the publication of the article.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hu, L., Duan, G., Xu, Y. et al. Prognostic analysis of different therapeutic regimens in patients with acute cardiogenic cerebral embolism. BMC Neurol 21, 325 (2021). https://doi.org/10.1186/s12883-021-02348-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-021-02348-9