Abstract
Background
Functional biomarkers able to identify multiple sclerosis (MS) patients at high risk of fast disability progression are lacking. The aim of this study was to evaluate the ability of multimodal (upper and lower limbs motor, visual, lower limbs somatosensory) evoked potentials (EP) to monitor disease course and identify patients exposed to unfavourable evolution.
Methods
One hundred MS patients were assessed with visual, somatosensory and motor EP and rated on the Expanded Disability Status Scale (EDSS) at baseline (T0) and about 6 years later (T1). The Spearman correlation (rS) was used to evaluate the relationship between conventional EP scores and clinical findings. Multiple (logistic) regression analysis estimated the predictive value of baseline electrophysiological data for three clinical outcomes: EDSS, annual EDSS progression, and the risk of EDSS worsening.
Results
In contrast to longitudinal correlations, cross-sectional correlations between the different EP scores and EDSS were all significant (0.33 ≤ rS < 0.67, p < 0.001). Baseline global EP score and EDSS were highly significant predictors (p < 0.0001) of EDSS progression 6 years later. The baseline global EP score was found to be an independent predictor of the EDSS annual progression rate (p < 0.001), and of the risk of disability progression over time (p < 0.005). Based on a ROC curve determination, we defined a Global EP Score cut off point (17/30) to identify patients at high risk of disability progression illustrated by a positive predictive value of 70 %.
Conclusion
This study provides a proof of the concept that electrophysiology could be added to MRI and used as another complementary prognostic tool in MS patients.
Similar content being viewed by others
Background
Evoked potentials (EP) provide quantitative functional measures in well-defined pathways of the central nervous system (CNS). In multiple sclerosis (MS), the use of EP to diagnose the disease or assess its biological activity has been limited, mainly because of the high sensitivity of magnetic resonance imaging (MRI), especially at the brain level [1]. There are situations though where electrophysiological data can provide useful diagnostic information. For instance, visual EP can demonstrate lesional spatial dissemination [2, 3]. During the course of MS, EP can be used to confirm unclear relapses in patients expressing vague or transitory symptoms [4]. EP have also been used in some clinical trials targeted on relapse anti-inflammatory treatments [5], immunomodulatory disease modifying drugs [6–8] and symptomatic medications designed to facilitate the central nervous conductions [9, 10].
Overall, EP were more sensitive than clinical metrics to demonstrate drug efficacy [5, 6], anticipate clinical changes [6], and help predicting good response in specific situations [9, 10].
If conventional MRI (T1, T2 and T1 + Gadolinium) and clinical evaluation can be regarded as the standard approach for diagnosing MS and monitoring its biological activity, they usually demonstrate a weak association known as the functional-anatomical paradox [11–13]. By contrast, EP can evaluate long eloquent pathways well correlated to the functional involvement [14]. EP latency and amplitude abnormalities evaluate the pathological conduction characteristics. Latency prolongation is due to demyelination, while conduction block or axonal loss lead to reduced amplitude [15]. In previous studies, cross-sectional correlations with EDSS were generally good, ranging from 0.3 to 0.6 [11, 16–22]. By contrast, longitudinal correlations were weaker [11, 17, 20, 23], which may be attributed to lower EP reproducibility [4, 24], to a level-off effect of EP measures in patients with more advanced disease [14], but also to a lack of responsiveness of clinical scales [25, 26]. The weak longitudinal association is balanced by the potential ability of EP to anticipate a clinical deterioration, which could be useful for the prognosis of the disease course [7, 16, 17, 27], especially in the era of early treatment procedure for patients with a poor prognosis. Yet, the prognostic role of EP is not fully admitted and further studies are needed to address this issue [28]. Therefore, the present work aimed to evaluate the ability of multimodal EP, summarized by a conventional score, to monitor MS and identify patients exposed to an unfavourable progression.
Methods
Subjects
We performed a retrospective analysis of the local database of 100 MS patients followed in our academic clinical centre between 2001 and 2014. The selection was based on a convenience sampling procedure. The inclusion criteria were: (1) a definite diagnosis of MS based on the 2001 and 2005 McDonald criteria [29, 30]; (2) a clinical follow-up of at least 3 years, including a disability rating using the Expanded Disability Status Scale (EDSS) obtained at baseline (T0) and at the end of the follow-up period (T1) [31]; (3) a multimodal EP examination at T0, i.e. motor evoked potentials from lower and upper limbs (MEP), visual evoked potentials (VEP), and somatosensory evoked potentials from lower limbs (SEP); (4) a clinically stable phase at the time of each evaluation ensured by a 3-month period between the previous relapse and the evaluation.
For 76 of the 100 MS patients, a second electrophysiological examination was available at the end of the follow-up period (T1) enabling a longitudinal analysis of multimodal EP data. The study was approved by the Local Ethics Committee (University Hospital of Liege) and has been performed in accordance with the ICH (International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use) guidelines.
Evoked potentials
All electrophysiological examinations were performed by the same investigator (XG) using the same recording system (Keypoint, Alpine Biomed, France); clinical evaluations were conducted by a non-blinded investigator (DD).
Motor Evoked Potentials (MEP) were recorded bilaterally from the first dorsal interosseous (FDI) in the upper limbs and from the tibialis anterior (TA) in the lower limbs. Each measurement started by recording the compound muscle action potential (CMAP) elicited by a supramaximal electrical stimulation of the ulnar nerve at the wrist and common peroneal nerve at the knee. Then, three transcranial magnetic stimulations (TMS) were delivered to the hand and leg areas of the motor cortex, respectively on Cz and Fz, with a Magstim 200 device (The Magstim Company Ltd., Whitland, UK) using a circular coil (maximal output 2.2 T). For each limb, the shortest latency and highest amplitude event out of the 3 waves were selected for analysis. A peripheral magnetic stimulation was applied over the C8 and L5 nerve root for the upper limbs and lower limbs, respectively, to derive the central motor conduction time (CMCT). The CMCT was obtained by subtracting the peripheral conduction time obtained by magnetic stimulation of the cervical and lumbar spinal roots from the cortical MEP latency. The following MEP parameters were considered in the study: peripheral, radicular and cortical latencies; CMCT; absolute baseline-to-peak amplitude from the peripheral and cortical stimulations; amplitude ratio (AR) expressed as the MEPampl/CMAPampl ratio; duration of the cortical stimulation induced response measured from the onset of the initial negative deflection to the latest positive deflection.
Visual evoked potentials (VEP) were recorded using EEG cup electrode Ag-AgCl electrodes. The active electrode was placed at Oz and the reference at Fz, based on the 10–20 international EEG system. Monocular visual stimulation was performed with a pattern-reversal check board screen. The size of the squares was adjusted to subtend a 15-min visual arc with an individual square. The two parameters used for the analysis were latency of the P100 component and N75-P100 amplitude difference.
Somatosensory evoked potentials (SEP) of the lower extremities were obtained through posterior tibial nerve electrical stimulation at the ankle. The afferent volley was recorded at 3 levels by active electrodes located at the popliteal fossa, over the intervertebral space D12-L1 and 2 cm posterior to Cz. The reference electrodes were placed, respectively, on the lateral side of the thigh, over the intervertebral space L5-S1 and at Fz. The parameters studied were the latencies of the main peripheral (N9), spinal (N21) and cortical (P40) components along with P40-N21 difference (central sensitive conduction time) and P40 amplitude (baseline-to-peak).
Analysis and rating of EP data
We developed from EP data a conventional ordinal score (EP score) modified from Jung et al. [16]. Specifically, for the sensory EP, both latency and amplitude abnormalities were included in the score. For MEP, the duration of the cortex stimulation induced response was added to these parameters to account for the temporal dispersion of the corticospinal discharges. Absolute or body side difference values above 2 standard deviations (SD) from our local normative data were considered pathological.
For each modality and body side, the score was derived from a 6-point graded ordinal scale summarized in Table 1. A result in the normal range but with a pathological body side difference received a score of 1 (for latency) and 2 (for amplitude). This score was assigned to the worst body side. In case of absolute latency above the normal limit, we attributed a score of 2, 3 or 4, according to the delay. The worst and maximum score of the scale (5) was attributed to an evoked response either absent or with amplitude below the normal range. Hence, the EP score for each side and each modality (UL MEP, LL MEP, LL SEP, VEP) ranged from 0 to 5. To give equal weight to each modality in the global EP score (MEP + SEP + VEP), we divided the MEP score by 2 since it was derived from the 4 limbs (UL MEP + LL MEP). Thus, the overall worst score of the scale was 30.
Statistical analysis
Results were expressed as mean and SD for quantitative data and as frequencies (number and percent) for categorical findings. The associations between EP scores and clinical data were assessed by the Spearman correlation coefficient (rs). Mean values between groups (e.g. relapsing–remitting vs. progressive patients) were compared by analysis of variance (ANOVA) and proportions by the chi-square or Fisher exact test. Score changes between T0 and T1 were assessed by the paired Student t-test.
Multivariate methods were used to assess the 6-year predictive value of demographic (age, size, weight, sex, laterality), clinical (relapsing-remitting or progressive phenotype, disease duration, follow-up duration, disease-modifying therapy between T0 and T1) and baseline electrophysiological (global EP score) data for three main clinical outcomes: the EDSS score (model 1), the annual EDSS progression score (model 2), and the EDSS worsening (yes/no). EDSS worsening was defined as a 1-point increase from T0 to T1 given a baseline EDSS <5.5 or an increase of 0.5 point given a baseline EDSS ≥ 5.5 [17] (model 3). The EDSS progression score per year was obtained by the absolute EDSS progression score divided by the follow-up duration in years. Multiple regression was used for models 1 and 2 and logistic regression for model 3. The quality of the fit was measured by the coefficient of determination (R2) for models 1 and 2 and by the area under the curve (AUC) for model 3. Results were expressed in terms of regression coefficients with their standard error (SE). Odds Ratios (OR) and associated 95 % confidence intervals (95 % CI) were added for the logistic model. Observed and predicted probabilities of worsening were cross-classified to further enhance the prognostic ability of baseline EP data. Finally, the receiver operating characteristic (ROC) curve method was used to determine an optimal cut-off value on the total EP scale to discern patients with poor and favourable prognosis. Results were considered significant at the 5 % critical level (p < 0.05). All statistical calculations and graphs were performed with SAS (version 9.4 for Windows) and the R software (version 3.0.3).
Results
Clinical and electrophysiological data are summarized in Table 2. At baseline, 90 patients were in a relapsing-remitting (RR) course, 9 patients in a secondary progressive (SP) course and one patient in a primary progressive (PP) course. The mean age was 39 years (SD 10) and the disease duration 9.1 years (SD 8.0). EDSS averaged 3.0 (SD 1.2) and the mean global EP score was 12.1 (SD 7.6). When comparing RR and P phenotypes, significant differences were observed for all clinical and electrophysiological parameters (except VEP) even after adjustment for disease duration.
After a median follow-up period of 6.3 years, the deteriorations of EDSS (+0.6; SD 1.1) and of the global EP score (+2.7; SD 3.9) were highly significant (p < 0.0001), as were those of lower limbs MEP and SEP. By contrast, the visual functional system progression, although significant (p < 0.05), was less marked, while the sensory functional system did not evidence any change. In classifying clinical and EP data with respect to their relative progression over time, we found that the global and LL MEP scores presented a worsening nearly twice as high as clinical measures (Table 3).
As seen in Table 4, the cross-sectional correlations (T0 and T1) between the different EP scores and EDSS or their related functional systems were all significant. The best association concerned the aggregate scores: global EP score and EDSS (r s = 0.67, p < 0.001). Longitudinally (T0 → T1), the only significant correlation was attributed to the motor function for a follow-up period longer than 6.3 years (T0 → T1).
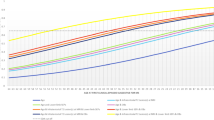
When predicting EDSS at T1 from baseline covariates by multiple regression analysis (model 1), only the global EP score and EDSS at baseline turned out to be significant after adjusting for follow-up time. None of the other parameters (e.g. demographic parameters, phenotype, disease duration, follow-up duration, disease-modifying therapy) were predictive of the outcome (Table 5). The strong correlation (R 2 = 0.72) between observed and predicted EDSS from model 1 at T1 evidenced the high performance of the disability prediction (Fig. 1). When discarding EDSS from the model 1, the global EP score still explained more than half (R 2 = 0.61) of the variance of EDSS at T1. Now, when considering the annual progression of EDSS (model 2), the global EP score at baseline was the only significant predictive parameter but the quality of the model was much lower (R 2 = 0,21) (Table 5).
Among the 100 MS patients at baseline, 38 evidenced an EDSS worsening during follow-up and 89 % received a disease-modifying therapy between T0 and T1. Logistic regression analysis (model 3) was applied to evaluate the probability of disability worsening based on the same demographic, clinical and electrophysiological factors (Table 6). When accounting for follow-up duration, only the baseline global EP score was found to be of significant prognostic value (OR = 1.2; 95 % CI 1.1–1.3; p = 0.0012). Interestingly, the baseline EDSS (p = 0,24) did not impact the prediction, as for the factor therapy (binary variable) between T0 and T1 (p = 0,05). The prognostic efficacy of model 3 was high (AUC = 0.84). When predicting EDSS worsening by the sole global EP score at baseline, the AUC was 0.77, only slightly less than for the full model. Further, a global EP score of 17 (over a scale of 30) was determined as the best cut-off point at baseline to identify patients at high risk of EDSS aggravation (Fig. 2). This cut-off yielded a sensitivity of 56.7 %, a specificity of 88.3 % with a corresponding positive predictive value (PPV) of 70.8 %.
ROC curve of baseline global EP score with respect to EDSS worsening. Area under the ROC curve (AUC = 0.77) and best cut-off point (Global EP score = 17/30) with a sensitivity of 56.7 % and a specificity of 88.3 %. EDSS worsening (Yes/No) was defined as a 1-point increase from T0 to T1 given a baseline EDSS <5.5 or an increase of 0.5 point given a baseline EDSS ≥5.5
Discussion
For the past 30 years, MS diagnosis, disease activity monitoring, and clinical trials have been essentially based on clinical and conventional MRI data. At the individual follow-up level, though, there is an apparent paradox between clinical metrics and MRI T2 lesion load [12]. This paradox is due to a subclinical activity before the first clinical symptoms in the early stage of the disease [32]. Up to 50–70 % of patients with a clinically isolated syndrome (CIS) exhibit clinically silent T2-weighted lesions [33]. After the relapsing-remitting phase, disability progresses without any MRI focal inflammatory activity due to axonal loss and diffuse inflammatory infiltration, which is not visible through conventional MRI [34–36].
Electrophysiology provides functional quantified data on multimodal afferent and efferent pathways through the brain and long spinal tracks. A standardized procedure was developed to study highly relevant functions (VEP, LL SEP and 4 limbs MEP). We advocate that our EP battery (VEP, UL and LL MEP and LL SEP), which takes 90–120 min depending on the patient’s compliance, constitutes the best trade-off between time efficiency and information relevance. As mentioned previously, to improve the EP prognostic yield, it seems more important adding EP modalities than repeating electrophysiological evaluations within a short period of time [37]. In our study, a post hoc analysis designed to investigate the individual contribution of EP modalities showed that restricting the test battery to VEP and UL MEP did not significantly lowered the predictive power of our models. This observation is in line with Schlaeger et al. who stated that, for the long term disability prediction, VEP and UL MEP were the most relevant variables [38]. However, in another study aimed to prognosticate the future disability in a sample of primary progressive patients, the same authors claimed that multimodal EP (VEP, UL and LL MEP, UL and LL SEP) could be simplified to a test battery containing only UL MEP and LL SEP without loss of information [19]. From these observations, it appears that the superiority of one EP modality over another in the prognostic field depends on the population characteristic in terms of phenotype, disability and disease duration at the time of the electrophysiological assessment.
Latency, conduction times, and amplitude parameters were taken into account to evaluate demyelination and axonal loss or conduction blocks. We constructed a composite neurophysiological score and retrospectively applied it to 100 MS patients followed for a median duration of about 6 years. Cross-sectional correlations with EDSS were good, in agreement with those reported in previous studies [11, 16–22, 27, 39]. The global EP score in the progressive form (19.8/30) was significantly higher than in the RR form (11.2/30) regardless of disease duration, and was closely related to clinical metrics (Table 2). This difference is mainly attributed to motor and somatosensory EP, suggesting a higher implication of spinal cord dysfunction in the progressive phenotype [40]. The lower correlation between VEP and EDSS also confirms that EDSS overweighs ambulation and spinal cord metrics and relatively underweighs more advanced measures of visual disability like change in low contrast vision, colour vision or visual field. We confirmed the markedly weaker longitudinal correlations already noticed by other authors [11, 17, 20, 23]. The relative longitudinal progression rate of clinical data illustrates the low EDSS sensitivity to change with a nearly twice higher deterioration of the global EP score and LL MEP score compared to EDSS and the functional systems (Table 3). The weaker correlation in the subgroup with the shorter follow-up is probably an additional argument for the lower EDSS sensitivity. The EDSS scale needs a sufficient amount of time to measure functional changes detected at an earlier stage by electrophysiology. On the other hand, high EP score level or progression, with long track dysfunction, is not necessarily associated with a clinical deterioration due to plasticity or adaptation but certainly indicates a depletion of functional reserve [41].
This ability of EP to anticipate a clinical deterioration constitutes the most salient result of our study. In the past, models with EP alone [37, 39] or integrated in multivariate approaches [19, 20, 38, 42] were used to forecast disability and disability progression for relatively homogenous samples [19, 22, 37, 43]. In this context, we performed a multivariate analysis to define a model able to predict the EDSS score at 6 years. Predicted and observed EDSS were highly correlated in agreement with published data obtained in smaller groups and in specific conditions [19, 37]. The statistical analysis showed that the initial global EP score and EDSS explain a significant part of the variance of the EDSS, 6 years later. Furthermore, the baseline global EP score was the unique significant factor able to predict the EDSS annual progression rate (p < 0.001) and the risk of EDSS worsening after a median follow up period of 6.3 years (p < 0.005). Our study also provides an EP score cut-off limit of 17, on a scale ranging from 0 to 30, which is potentially useful at the individual level as it suggests that a patient with a Global EP score higher than 17/30 exhibits a risk of clinical worsening of around 70 %. To some extent, this observation provides a proof of the concept that electrophysiology could be used as part of a prognostic armamentarium in MS.
The present study was limited by the retrospective design and by the heterogeneity of the follow-up duration between subjects. Nevertheless, the multivariate analysis showed that this variability didn’t impact outcome prediction. While the therapeutic factor did not significantly impact the prognosticating potential of our EP score, as previously argued by Schlaeger on a smaller sample size [42], it would be valuable, in the era of highly active therapies, to design a prospective study focused on the prognostic interplay between EP and immunomodulatory drugs. Further studies are however needed to implement spinal and cerebral MRI metrics as well as to confirm the validity of our models, based on the same EP procedure but with other datasets. It could be useful, and not redundant, to integrate clinical, neurophysiological functional data and anatomical information to define a multivariate prognostic index.
Furthermore, EP amplitude measures can indirectly reflect central axonopathy, which is highly correlated with irreversible disability. Motor triple stimulation technique can precise and quantify corticospinal conduction failure and should be more largely implemented in the electrophysiological evaluation [44].
Conclusion
In conclusion, multimodal EP, summarized in an ordinal score, seem to be well suited as a biomarker of the MS disease course given the high correlations observed with EDSS at any time point. Using a multivariate approach we proposed models for EDSS prediction and for the risk of clinical aggravation at a second follow-up time point. Based on ROC curve analysis we were able to define an EP score cut-off point which is associated with a high risk of disability progression. At the individual clinical level, this finding could be a relevant and independent argument for early highly active therapy. It could also support the process of patient selection in the scientific settings.
Abbreviations
ANOVA, analysis of variance; AR, amplitude ratio; AUC, area under the ROC curve; CDMS, clinically definite diagnosis of MS; CI, confidence interval; CMAP, compound muscle action potential; CMCT, central motor conduction time; DMT, disease-modifying therapy; EDSS, expanded disability status scale; EP, evoked potentials; F, female; FDI, first dorsal interosseous; LL, lower limb; M, male; Max, maximal theoretical value for each individual score; MEP, motor evoked potentials; mFS, pyramidal functional system; MRI, magnetic resonance imaging; MS, multiple sclerosis; NA, not applicable; OR, odds ratio; P, progressive; PP, primary progressive; R2, coefficient of determination; ROC, receiver operating characteristic; RR, relapsing–remitting; rs, Spearman correlation coefficient; SD, standard deviation; SE, standard error; SEP, somatosensory evoked potentials; sFS, sensory functional system; SP, secondary progressive; TA, tibialis anterior; TMS, transcranial magnetic stimulation; UL, upper limb; VEP, visual evoked potentials; vFS, visual functional system.
References
Hutchinson M. Evoked Potentials Are of Little Use in the Diagnosis or Monitoring of Ms: Commentary. Mult Scler. 2013;19(14):1824–5.
Beer S, Rosler KM, Hess CW. Diagnostic Value of Paraclinical Tests in Multiple Sclerosis: Relative Sensitivities and Specificities for Reclassification According to the Poser Committee Criteria. J Neurol Neurosurg Psychiatry. 1995;59(2):152–9.
Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, Fujihara K, Havrdova E, Hutchinson M, Kappos L, Lublin FD, Montalban X, O'Connor P, Sandberg-Wollheim M, Thompson AJ, Waubant E, Weinshenker B, Wolinsky JS. Diagnostic Criteria for Multiple Sclerosis: 2010 Revisions to the Mcdonald Criteria. Ann Neurol. 2011;69(2):292–302.
Comi G, Leocani L, Medaglini S, Locatelli T, Martinelli V, Santuccio G, Rossi P. Measuring Evoked Responses in Multiple Sclerosis. Mult Scler. 1999;5(4):263–7.
La Mantia L, Riti F, Milanese C, Salmaggi A, Eoli M, Ciano C, Avanzini G. Serial Evoked Potentials in Multiple Sclerosis Bouts. Relation to Steroid Treatment. Ital J Neurol Sci. 1994;15(7):333–40.
Nuwer MR, Packwood JW, Myers LW, Ellison GW. Evoked Potentials Predict the Clinical Changes in a Multiple Sclerosis Drug Study. Neurology. 1987;37(11):1754–61.
Feuillet L, Pelletier J, Suchet L, Rico A, Ali Cherif A, Pouget J, Attarian S. Prospective Clinical and Electrophysiological Follow-up on a Multiple Sclerosis Population Treated with Interferon Beta-1 A: A Pilot Study. Mult Scler. 2007;13(3):348–56.
Meuth SG, Bittner S, Seiler C, Gobel K, Wiendl H. Natalizumab Restores Evoked Potential Abnormalities in Patients with Relapsing-Remitting Multiple Sclerosis. Mult Scler. 2011;17(2):198–203.
Horton L, Conger A, Conger D, Remington G, Frohman T, Frohman E, E, Greenberg B. Effect of 4-Aminopyridine on Vision in Multiple Sclerosis Patients with Optic Neuropathy. Neurology. 2013;80(20):1862–6.
Zeller D, Reiners K, Brauninger S, Buttmann M. Central Motor Conduction Time May Predict Response to Fampridine in Patients with Multiple Sclerosis. J Neurol Neurosurg Psychiatry. 2014;85(6):707–9.
O’Connor P, Marchetti P, Lee L, Perera M. Evoked Potential Abnormality Scores Are a Useful Measure of Disease Burden in Relapsing-Remitting Multiple Sclerosis. Ann Neurol. 1998;44(3):404–7.
Zivadinov R, Leist TP. Clinical-Magnetic Resonance Imaging Correlations in Multiple Sclerosis. J Neuroimaging. 2005;15(4 Suppl):10S–21.
Kesselring J, Miller DH, MacManus DG, Johnson G, Milligan NM, Scolding N, Compston DA, McDonald WI. Quantitative Magnetic Resonance Imaging in Multiple Sclerosis: The Effect of High Dose Intravenous Methylprednisolone. J Neurol Neurosurg Psychiatry. 1989;52(1):14–7.
Leocani L, Comi G. Neurophysiological Markers. Neurol Sci. 2008;29 Suppl 2:S218–21.
Comi G, Locatelli T, Leocani L, Medaglini S, Rossi P, Martinelli V. Can Evoked Potentials Be Useful in Monitoring Multiple Sclerosis Evolution? Electroencephalogr Clin Neurophysiol Suppl. 1999;50:349–57.
Jung P, Beyerle A, Ziemann U. Multimodal Evoked Potentials Measure and Predict Disability Progression in Early Relapsing-Remitting Multiple Sclerosis. Mult Scler. 2008;14(4):553–6.
Leocani L, Rovaris M, Boneschi FM, Medaglini S, Rossi P, Martinelli V, Amadio S, Comi G. Multimodal Evoked Potentials to Assess the Evolution of Multiple Sclerosis: A Longitudinal Study. J Neurol Neurosurg Psychiatry. 2006;77(9):1030–5.
Fuhr P, Borggrefe-Chappuis A, Schindler C, Kappos L. Visual and Motor Evoked Potentials in the Course of Multiple Sclerosis. Brain. 2001;124(Pt 11):2162–8.
Schlaeger R, D’Souza M, Schindler C, Grize L, Kappos L, Fuhr P. Electrophysiological Markers and Predictors of the Disease Course in Primary Progressive Multiple Sclerosis. Mult Scler. 2014;20(1):51–6.
Margaritella N, Mendozzi L, Garegnani M, Colicino E, Gilardi E, Deleonardis L, Tronci F, Pugnetti L. Sensory Evoked Potentials to Predict Short-Term Progression of Disability in Multiple Sclerosis. Neurol Sci. 2012;33(4):887–92.
Ramanathan S, Lenton K, Burke T, Gomes L, Storchenegger K, Yiannikas C, Vucic S. The Utility of Multimodal Evoked Potentials in Multiple Sclerosis Prognostication. J Clin Neurosci. 2013;20(11):1576–81.
Margaritella N, Mendozzi L, Garegnani M, Nemni R, Colicino E, Gilardi E, Pugnetti L. Exploring the Predictive Value of the Evoked Potentials Score in Ms within an Appropriate Patient Population: A Hint for an Early Identification of Benign Ms? BMC Neurol. 2012;12:80.
Bednarik J, Kadanka Z. Multimodal Sensory and Motor Evoked Potentials in a Two-Year Follow-up Study of Ms Patients with Relapsing Course. Acta Neurol Scand. 1992;86(1):15–8.
Aminoff MJ, Davis SL, Panitch HS. Serial Evoked Potentials Studies in Patients with Definite Multiple Sclerosis. Arch Neurol. 1984;44:1232–6.
Sharrack B, Hughes RA. Clinical Scales for Multiple Sclerosis. J Neurol Sci. 1996;135(1):1–9.
Sharrack B, Hughes RA, Soudain S, Dunn G. The Psychometric Properties of Clinical Rating Scales Used in Multiple Sclerosis. Brain. 1999;122(Pt 1):141–59.
Kallmann BA, Fackelmann S, Toyka KV, Rieckmann P, Reiners K. Early Abnormalities of Evoked Potentials and Future Disability in Patients with Multiple Sclerosis. Mult Scler. 2006;12(1):58–65.
McGuigan C. Evoked Potentials Are of Little Use in the Diagnosis or Monitoring of Ms: Yes. Mult Scler. 2013;19(14):1820–1.
McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, McFarland HF, Paty DW, Polman CH, Reingold SC, Sandberg-Wollheim M, Sibley W, Thompson A, van den Noort S, Weinshenker BY, Wolinsky JS. Recommended Diagnostic Criteria for Multiple Sclerosis: Guidelines from the International Panel on the Diagnosis of Multiple Sclerosis. Ann Neurol. 2001;50(1):121–7.
Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP, Kappos L, Lublin FD, Metz LM, McFarland HF, O'Connor PW, Sandberg-Wollheim M, Thompson AJ, Weinshenker BG, Wolinsky JS. Diagnostic Criteria for Multiple Sclerosis: 2005 Revisions to the “Mcdonald Criteria”. Ann Neurol. 2005;58(6):840–6.
Kurtzke JF. Rating Neurologic Impairment in Multiple Sclerosis: An Expanded Disability Status Scale (Edss). Neurology. 1983;33(11):1444–52.
O’Riordan JI, Thompson AJ, Kingsley DP, MacManus DG, Kendall BE, Rudge P, McDonald WI, Miller DH. The Prognostic Value of Brain Mri in Clinically Isolated Syndromes of the Cns. A 10-Year Follow-Up. Brain. 1998;121(Pt 3):495–503.
Fisniku LK, Brex PA, Altmann DR, Miszkiel KA, Benton CE, Lanyon R, Thompson AJ, Miller DH. Disability and T2 Mri Lesions: A 20-Year Follow-up of Patients with Relapse Onset of Multiple Sclerosis. Brain. 2008;131(Pt 3):808–17.
Li DK, Held U, Petkau J, Daumer M, Barkhof F, Fazekas F, Frank JA, Kappos L, Miller DH, Simon JH, Wolinsky JS, Filippi M, Sylvia Lawry Centre for MSR. Mri T2 Lesion Burden in Multiple Sclerosis: A Plateauing Relationship with Clinical Disability. Neurology. 2006;66(9):1384–9.
Neema M, Stankiewicz J, Arora A, Dandamudi VS, Batt CE, Guss ZD, Al-Sabbagh A, Bakshi R. T1- and T2-Based Mri Measures of Diffuse Gray Matter and White Matter Damage in Patients with Multiple Sclerosis. J Neuroimaging. 2007;17 Suppl 1:16S–21.
Miller DH, Thompson AJ, Filippi M. Magnetic Resonance Studies of Abnormalities in the Normal Appearing White Matter and Grey Matter in Multiple Sclerosis. J Neurol. 2003;250(12):1407–19.
Schlaeger R, D’Souza M, Schindler C, Grize L, Kappos L, Fuhr P. Combined Evoked Potentials as Markers and Predictors of Disability in Early Multiple Sclerosis. Clin Neurophysiol. 2012;123(2):406–10.
Schlaeger R, Schindler C, Grize L, Dellas S, Radue EW, Kappos L, Fuhr P. Combined Visual and Motor Evoked Potentials Predict Multiple Sclerosis Disability after 20 Years. Mult Scler. 2014;20(10):1348–54.
Invernizzi P, Bertolasi L, Bianchi MR, Turatti M, Gajofatto A, Benedetti MD. Prognostic Value of Multimodal Evoked Potentials in Multiple Sclerosis: The Ep Score. J Neurol. 2011;258(11):1933–9.
Filippi M, Campi A, Mammi S, Martinelli V, Locatelli T, Scotti G, Amadio S, Canal N, Comi G. Brain Magnetic Resonance Imaging and Multimodal Evoked Potentials in Benign and Secondary Progressive Multiple Sclerosis. J Neurol Neurosurg Psychiatry. 1995;58(1):31–7.
Comi G, Leocani L, Medaglini S, Locatelli T, Martinelli V, Santuccio G, Rossi P. Evoked Potentials in Diagnosis and Monitoring of Multiple Sclerosis. Electroencephalogr Clin Neurophysiol Suppl. 1999;49:13–8.
Schlaeger R, D’Souza M, Schindler C, Grize L, Dellas S, Radue EW, Kappos L, Fuhr P. Prediction of Long-Term Disability in Multiple Sclerosis. Mult Scler. 2012;18(1):31–8.
Margaritella N, Mendozzi L, Tronci F, Colicino E, Garegnani M, Nemni R, Gilardi E, Pugnetti L. The Evoked Potentials Score Improves the Identification of Benign Ms without Cognitive Impairment. Eur J Neurol. 2013;20(10):1423–5.
Humm AM, Magistris MR, Truffert A, Hess CW, Rosler KM. Central Motor Conduction Differs between Acute Relapsing-Remitting and Chronic Progressive Multiple Sclerosis. Clin Neurophysiol. 2003;114(11):2196–203.
Acknowledgement
The authors would like to thank Christine Ernon for proofreading the manuscript.
Funding
We state that no funding was obtained for this study.
Availability of data and materials
The datasets supporting the conclusions of this article are included in Additional file 1.
Authors’ contributions
All authors read and approved the final manuscript. Author contribution: XG: Study design, patient collection and electrophysiological evaluations, data collection and analysis, manuscript preparation and manuscript writing; DD: Study design, patient collection and clinical assessments, manuscript preparation and review; AA: Statistical and data analysis, manuscript review; NM: Statistical and data analysis; PM and JMC: manuscript review.
Competing interests
The authors declare that they have no conflict of interest.
Consent for publication
Not applicable.
Ethical approval
The study was approved by the Local Ethics Committee (University Hospital of Liege, Ref: B707201318670) and has been performed in accordance with the ICH (International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use) guidelines.
Consent to participate
Not applicable (retrospective study).
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Raw demographical, clinical and electrophysiological data of the 100 MS patients obtained at T0 and T1. (XLSX 362 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Giffroy, X., Maes, N., Albert, A. et al. Multimodal evoked potentials for functional quantification and prognosis in multiple sclerosis. BMC Neurol 16, 83 (2016). https://doi.org/10.1186/s12883-016-0608-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-016-0608-1