Abstract
Background
We aimed to determine the association of clinical and routine cerebrospinal fluid biochemical markers (total protein, IgG index and oligoclonal bands) with disability in multiple sclerosis and whether these biomarkers assessed at diagnosis add prognostic value.
Methods
We followed a cohort of patients included in the Multiple Sclerosis Lorraine Register (eastern France) who had a diagnosis of multiple sclerosis for at least 5 years, as well as biological markers values and MRI findings (Barkhof’s criteria). In a Cox regression model, endpoint was time to score of 4 on the Expanded Disability Status Scale (EDSS) (i.e., limited time walking without aid or rest for more than 500 m).
Results
For 407 patients included, the median time from multiple sclerosis onset to EDSS score 4 was 4.5 years [2.2–7.2]. Cerebrospinal fluid total protein factor < 500 mg/L was associated with EDSS score 4 on bivariate analysis (hazard ratio 0.66, 95% confidence interval 0.46–0.95, p = 0.02). On multivariate analysis, older age at disease onset (≥50 years) and initial primary progressive course of MS but not biological markers predicted worse prognosis.
Conclusion
Routine cerebrospinal fluid biological markers at diagnosis were not prognostic factors of multiple sclerosis progression.
Similar content being viewed by others
Background
Analysis of cerebrospinal fluid (CSF) has gained renewed interest in diagnosis of multiple sclerosis (MS) [1,2], but any prognostic value for disease progression is debated. Among CSF markers, oligoclonal IgG bands (OCGBs) are present in more than 95% of patients with MS [3,4] and may have utility and prognostic value for MS diagnosis [5]. Another prognostic CSF marker may be IgG index [6]. Some studies [7,8] have indicated a correlation between index of IgG synthesis or number of OCGBs in CSF and progression rate, but others have not [5,9-12]. Low number or absence of OCGBs in CSF at diagnosis may predict better prognosis, particularly in terms of disability [5,9,10,13-20]. However, the prognostic value has not been established [21].
Among the various prognostic factors of disability in MS, both primary progressive (PP) and remittent relapsing (RR) MS, the number of relapses in the first years and MRI-determined lesional changes seemed to be the most reliable [22-27]. However, most authors agree that the clinical course cannot be predicted by initial symptoms alone [22]. A short interval between the 2 first relapses [26], a rapid early course [27], a primary progressive course without remission [25-27] or onset at older age [26-28] have all been associated with worse long-term prognosis [29]. Sex may influence disease progression (female [23,25]; male [27]). CSF markers with prognostic value at diagnosis would provide the physician with useful information early in the disease course to adjust treatment, without waiting for further clinical manifestations.
We used a population-based MS cohort to determine at MS diagnosis the role of routine CSF biochemical variables, particularly IgG index and presence of OCGBs, on disability (i.e., whether these biomarkers assessed at diagnosis have prognostic value).
Methods
Source of the population
Patients were identified in the register of MS patients in the Lorraine region of France. The main purpose of this register is to record all incident cases of MS in Lorraine [23,30] and follow them over time according to neurologists’ routine practice [31,32]. On November 1, 2011, 4,717 patients were registered.
Patient sampling
Inclusion criteria were time from MS onset (first signs or symptoms) of at least 5 years [24], a lumbar puncture within 10 years after the MS onset, with complete routine CSF biological data available (CSF OCGBs are stable over time [33-35] thus reflecting status at diagnosis if puncture was performed later), and Barkhof’s criteria available. Only patients with total protein, IgG index and oligoclonal bands available were included in the study. The clinically isolated syndrome (CIS) and radiologically isolated syndrome (RIS) patients were excluded. From the 4,717 patients potentially eligible for the study, 407 patients fulfilled the inclusion criteria (1997-2006) (Figure 1).
The collection of register data was approved by the French Advisory Committee on the Information processing Research in the Field of Health (CCTIRS; reference N°10.258) in May 2010, and the French National Commission for Data Protection and Liberties (CNIL; reference N° 909089) in June 2006. Confidentiality and safety of the data were ensured in accordance with these recommendations. An informed consent for use of patient data was obtained from each participant.
Data collection
For the register, the neurologists collect data at diagnosis and at each following routine consultation. When patients were notified to the register, all information since MS onset was collected retrospectively, and patients were entered in a prospective follow-up.
Data consistency is checked by use of the European Database for MS (EDMUS) software with automatic controls to reduce the frequency of incomplete or incorrect data [36].
For this study, we used demographic data; key episodes in the course of MS, including date of MS onset, date of first and second episodes, and status of recovery from the first episode at the first relapse; Expanded Disability Status Scale (EDSS) score, used to assess MS disability [37], at each visit; and time of assignment of the irreversible disability score, EDSS score 4 (EDSS 4; i.e., limited walking without aid or rest for more than 500 m). MRI findings interpreted by initial Barkhof’s criteria which are: at least one Gadolinium-enhancing lesion or ≥9 T2 lesions, one Juxtacortical lesion, one Infratentorial lesion and three Periventricular lesions; [38] were recorded. As most patients had MRI performed at Nancy University hospital, MRI reading process was consistent for these criteria.
Recovery from the first relapse was classified as incomplete (persistence of neurological signs, corresponding to an EDSS score of at least 2) or complete (absence of neurological signs, an EDSS score of 0 or 1). The onset date of the second neurological episode of MS, which may be a relapse or the onset of the progressive phase, was systematically determined whenever appropriate.
Biological samples and biochemical analyses
All analyses were performed at the biochemistry laboratory of the University Hospital of Nancy or at the biology laboratory of the Regional Hospital of Thionville. Matched CSF and serum were collected in the clinical setting. All samples were immediately transported at room temperature to the lab. Determination of leukocytes count in CSF was assessed using a Nageotte hematocytometer and microscopic observation. The presence of more than 5 cells per mm3 was considered abnormal. Then, CSF were quickly centrifuged at 2,000 × g for 10 min at 4°C and stored at -20°C. The level of CSF total protein was measured by turbidimetry in both laboratories. Concentrations of albumin and IgG were determined in CSF and in serum by automated turbidimetry or nephelemetry, respectively. These parameters were used to calculate IgG index as (CSF IgG/serum IgG) × (serum albumin/CSF albumin). A comparative analysis showed no significant variation of the IgG index between both methods. The threshold value for IgG index was set at 0.60 (personal unpublished data).
The presence of OCGBs in unconcentrated CSF was determined by isoelectric focusing (IEF) followed by immunoblotting [3]. Sensitivity for detecting OCGBs in CSF using this “gold standard” method is higher than 95%, whatever the commercially available IEF apparatus used [1]. A positive control was systematically used in each gel run to determine the reliability of any given run. Cut-off for OCGBs positivity was defined as 2 CSF-restricted IgG bands. Because the presence of OCGBs in CSF remains constant over the course of the disease, results obtained within 10 years after MS onset, where this technique was used, was considered present at diagnosis [33-35].
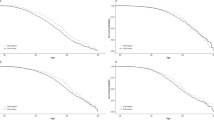
Statistical analysis
Quantitative data are expressed as mean ± SD, median and range, quartiles and extreme values and qualitative data by numbers and percentages. The normality of variables was tested by the Kolmogorov-Smirnov test, skewness and kurtosis. Comparison of 2 groups used chi-square test for categorical variables and Student t test for continuous variables. The time from disease onset to assignment of the irreversible score EDSS 4 was considered the endpoint. Subjects without this score and those who died before the first occurrence of an irreversible EDSS score were censored at the last follow-up. The time to the endpoint was described by Kaplan-Meier estimates. Bivariate analyses involved the log-rank test.
The Cox proportional-hazards regression model was used to assess the predictive value of presence of OCGBs and elevated IgG index on disability progression by multivariate analysis, with adjustment for potential confounding variables: age at disease onset, gender, initial form of MS, incomplete recovery at first relapse, protein level, leukocyte count, IgG index, OCGBs, MRI lesions (Barkhof’s criteria), and time from MS onset.
Also, we defined a treatment variable, with treatment (both immunomodulatory or immunosuppressive therapies be it orally or intravenously administered) as present as soon as the first treatment longer than six months before the time to assignment of irreversible EDSS4 for each patient. We considered that this six months time threshold was the minimal time after which we could estimate the beneficial role of the treatment. We introduced the treatment variable in the multivariate analysis.
Stepwise selection of variables was used with p = 0.20 for entering the model and p = 0.10 for staying in the model. We tested the proportionality assumption and the log linearity hypothesis. Because the proportional-hazards assumption was not verified for some covariates, we used a time-varying variable-extended Cox model [39]. Hazard ratios (HRs) and their 95% confidence intervals (95% CIs) for disability progression (time to EDSS 4) were calculated for parameters and were considered significant at p < 0.05.
Statistical analysis involved SAS v9.3 for Windows (SAS Inst., Cary, NC, USA).
Results
Baseline characteristics are in Table 1. The mean age at MS onset was 33.0 ± 11.1 years. The median time between MS onset and CSF testing was 4.6 years [1.0–7.0]. Among registered patients, those included and not included in the study did not differ in age at onset (p = 0.41) and gender (p = 0.31) but did differ in the initial form of MS (p = 0.01) and incomplete recovery at first relapse (p = 0.02).
During the initial course of MS, 349 patients had RR disease at disease onset and 58 PP disease (Table 1). In all, 142 patients had reached EDSS 4. The median time from MS onset to assignment of irreversible EDSS4 by the Kaplan-Meier method was 4.5 years [2.2–7.2]. In total, 188 (46.2%) had elevated CSF IgG index and 354 (87%) CSF OCGBs. The mean IgG index was 0.6 ± 0.7 and mean CSF total protein level 345.5 ± 219.7 mg/L. The proportion of CSF OCGBs was the same whatever the MS course, namely 87.1% and 86.2% of CSF OCGBs positives in RR and PP patients, respectively.
Table 2 gives the results of bivariate analyses of variables associated with median time from MS onset to EDSS4. Among biological variables, CSF total protein level < 500 mg/L was associated with EDSS 4 (HR 0.66, 95% CI 0.46–0.95). Older age at MS onset (≥29 years) was associated with poor prognosis; for age between 29 and 38 years, the HR was 2.56 (95% CI 1.29–5.07) and between 39 and 49 years, 2.58 (1.27–5.25). Univariate analysis showed no significant association of Barkhof criteria (HR 0.8, 95% CI 0.48–1.4; p = 0.4). Other variables associated with good prognosis were the RR form of MS (HR 0.15, 95% CI 0.10–0.21), female sex (HR 0.45, 95% CI 0.32–0.62) and undergoing a treatment (HR 0.20, 95% CI 0.14–0.28).
The time to assignment of irreversible EDSS 4 did not differ for patients without and with OCGBs (5.4 vs. 4.9 years, p = 0.52) and for patients with and without IgG index < 0.60 (4.9 vs. 5.2 years, p = 0.65). This did not differ when varying the IgG index threshold to < 0,65 (p = 0,73) or to < 0,7 (p = 0,81).
Table 3 presents the results of multivariate analysis with extended Cox regression models and reveals no significant impact of routine CSF biological markers on assignment of EDSS 4. Even when adjusting for major covariates at onset (age) and at diagnosis (sex, initial course of MS, Barkhof’s criteria, treatment), older age at onset (≥50) (HR 2.48, 95% CI 1.11–5.55) and initial PP course (HR 3.12, 95% CI 2.03–4.79) were associated with poor prognosis, while OCGBs (HR 0.76, 95% CI 0.45–1.30) and IgG index (HR 1.36, 95% CI 0.92–2.02) were not.
Discussion
We could not demonstrate any value of CSF IgG index and presence of OCGBs at a mean of 8.9 ± 3.8 years of follow-up for prognosis of disability in MS, which contrasts with previous studies [5-12,18] but is in line with a recent study [40]. Older age at disease onset (≥50 years) and initial PP course of MS were predictors of worsening disability. In contrast with other studies [23,25,27,41,42], gender was not a prognostic factor.
In recent years, several studies have suggested the prognostic value of OCGBs in MS, showing good correlation between disability and presence of OCGBs [9,10,16,43], as well as IgG index [44]. CSF OCGBs are stable over time [33-35], which allowed us to consider it for subjects with late lumbar puncture, as a reflection of the value of this factor at diagnosis. However, whether CSF total protein level and IgG index at the time of lumbar puncture actually reflects their values at diagnosis is uncertain.
Many studies have investigated the prognosis of MS in terms of biological markers [21,40,45]. Most studies have focused on the RR form of MS. The absence of OCGBs and low baseline T2-weighted lesions found on MRI were favourable prognostic factors influencing the clinical response to interferon β treatment in patients with RR MS [16]. Age at disease onset and number of MS attacks during the first 2 years of MS were predictors of the evolution of the disability [46]. Blood levels of gene markers [47], CSF IgM oligoclonal bands [48], the association of intrathecal Ig synthesis and cortical lesions [49], simple detection of intrathecal IgG synthesis [9,44] and initial relapse of RR MS have been studied as prognosis markers of RR MS. Other studies have focused on imaging and motor-evoked potentials [50] or the secondary progressive phase of MS [42].
Another recent study found that the presence of OCGBs and elevated total CSF IgG and protein levels moderately were associated with PP MS but not disease progression [40]. As in our study, for patients who had undergone multiple lumbar punctures, only the earliest puncture was considered, and we found the same percentages for the RR form (85.7%) and PP form (14.3%). However, the study differed from ours in a higher number of subjects, different biological technique for CSF analysis, smaller time from MS onset to lumbar puncture and no multivariate analysis.
In patients with clinically isolated syndromes, the presence of lesions as determined by T2-weighted baseline magnetic resonance imaging (MRI) of the brain or medullar tract increases chances of developing multiple sclerosis. The degree of long-term disability from multiple sclerosis correlates with the volume increase of the lesions seen on the brain MRI in the first five years only [11,24] In our study, the change in volume over time was not taken into account. Therefore, the absence of a prognostic role of baseline MRI considering only the Barkhof-Tintore criteria is not surprising.
For an early prognostic perspective, we entered only covariates assessed at the time of MS onset in the regression model. Compared with the other studies, we were interested in the well-known prognostic markers and new data at MS onset.
End of the 90’s was a milestone in the support of MS. As noted earlier, the biological techniques to detect OCGBs have evolved over time, especially after the 1990s, which must be considered in interpreting results. In recent years, the isoelectric focusing technique of CSF with IgG immunoassays was allowed for detecting chronic inflammatory CSF, especially MS. Here, percentage of OCB negative patients is higher (12.9% for RR and 13.8 for PP) than in previous works [10,51] where percentage oscillated between 3-5%, with maximum 10.6% in Siritho’s work in 2009. It was reported a tendency for lower prevalences in CSF from MS patients in countries in southern of Europe compared to MS patients in northern countries. Although not available in our study, information about the origin of our patients might contribute to explain this atypical result [3,13,52]. Finally, the first eligible criterion, minimal time from disease onset for at least 5 years, considerably decreased the number of patients with CSF test results, because in recent years, the database has had more complete data from CSF tests.
The strengths of our study are that first, we conducted multivariate analysis unlike most studies evaluating the predictive value of routine CSF biological data which used only bivariate analysis [4,12,17,43,49] and included a low number of patients (<100) [9,10,43,47], except for two studies [19,40]. Furthermore, only 2 studies claimed they used adjustment for variables [10,16]. Yet, with our relatively large sample size (n = 407), our results did not show the predictive value of these biological markers. Such differences might explain the previous contradictory results. Second, patients were followed for a median of 8.7 years (6.2–11.0), a long period as compared with other studies [10,46,49,50].
Our study contains some limitations. The main difficulty was the number of missing data relating to CSF, which has several explanations. First, some neurologists believe that CSF data are not important in the diagnosis of MS, particularly if the clinical and radiological criteria leave no doubt. On another hand, for some patients living far from major care center, it was not always possible to perform lumbar puncture. Second, the information might be available but not yet complete for some patients, which led to our excluding data for some patients. Therefore, our cohort of 407 patients could have been even larger, with higher statistical power. Third, we had an exhaustive database, the Lorraine MS register, with data for about 4,700 patients. From the overall register population, patients who did and did not meet the eligibility criteria were comparable in demographic characteristics. Regarding the quality of the data, patient records in the register are regularly updated when patients see their neurologist. However, although they were identified in the register, patients retained in the sample were likely more severe since more frequently diagnosed at hospital center, as our team reported in a previous paper [53]. But as a reflection of the recruitment from the register, there was more heterogeneity in clinical profile, in routine biological markers and in treatments.
Conclusions
In conclusion, our study, involving a large cohort of patients and multivariate analysis, could not demonstrate the value of routine CSF biological markers at MS diagnosis for prognosis of disability progression.
References
Freedman MS, Thompson EJ, Deisenhammer F, Giovannoni G, Grimsley G, Keir G, et al. Recommended standard of cerebrospinal fluid analysis in the diagnosis of multiple sclerosis: a consensus statement. Arch Neurol. 2005;62(6):865–70.
Deisenhammer F, Bartos A, Egg R, Gilhus NE, Giovannoni G, Rauer S, et al. Guidelines on routine cerebrospinal fluid analysis. Report from an EFNS task force. Eur J Neurol. 2006;13(9):913–22.
Link H, Huang YM. Oligoclonal bands in multiple sclerosis cerebrospinal fluid: an update on methodology and clinical usefulness. J Neuroimmunol. 2006;180(1-2):17–28.
Villar LM, Masterman T, Casanova B, Gomez-Rial J, Espino M, Sadaba MC, et al. CSF oligoclonal band patterns reveal disease heterogeneity in multiple sclerosis. J Neuroimmunol. 2009;211(1-2):101–4.
Awad A, Hemmer B, Hartung HP, Kieseier B, Bennett JL, Stuve O. Analyses of cerebrospinal fluid in the diagnosis and monitoring of multiple sclerosis. J Neuroimmunol. 2010;219(1-2):1–7.
Izquierdo G, Angulo S, Garcia-Moreno JM, Gamero MA, Navarro G, Gata JM, et al. Intrathecal IgG synthesis: marker of progression in multiple sclerosis patients. Acta Neurol Scand. 2002;105(3):158–63.
Olsson JE, Link H, Muller R. Immunoglobulin abnormalities in multiple sclerosis. Relation to clinical parameters: disability, duration and age of onset. J Neurol Sci. 1976;27(2):233–45.
Stendahl-Brodin L, Link H. Relation between benign course of multiple sclerosis and low-grade humoral immune response in cerebrospinal fluid. J Neurol Neurosurg Psychiatry. 1980;43(2):102–5.
Avasarala JR, Cross AH, Trotter JL. Oligoclonal band number as a marker for prognosis in multiple sclerosis. Arch Neurol. 2001;58(12):2044–5.
Joseph FG, Hirst CL, Pickersgill TP, Ben Shlomo Y, Robertson NP, Scolding NJ. CSF oligoclonal band status informs prognosis in multiple sclerosis: a case control study of 100 patients. J Neurol Neurosurg Psychiatry. 2009;80(3):292–6.
Rojas JI, Patrucco L, Cristiano E. Oligoclonal bands and MRI in clinically isolated syndromes: predicting conversion time to multiple sclerosis. J Neurol. 2010;257(7):1188–91.
Verjans E, Theys P, Delmotte P, Carton H. Clinical parameters and intrathecal IgG synthesis as prognostic features in multiple sclerosis. Part I J Neurol. 1983;229(3):155–65.
Idiman E, Ozakbas S, Dogan Y, Kosehasanogullari G. The significance of oligoclonal bands in multiple sclerosis: relevance of demographic and clinical features, and immunogenetic backgrounds. J Neuroimmunol. 2009;212(1-2):121–4.
Siritho S, Freedman MS. The prognostic significiance of cerebrospinal fluid in multiple sclerosis. J Neurol Sci. 2009;15(279(1-2):21–5.
Tumani H, Hartung HP, Hemmer B, Teunissen C, Deisenhammer F, Giovannoni G, et al. Cerebrospinal fluid biomarkers in multiple sclerosis. Neurobiol Dis. 2009;35(2):117–27.
Annunziata P, Giorgio A, De Santi L, Zipoli V, Portaccio E, Amato MP, et al. Absence of cerebrospinal fluid oligoclonal bands is associated with delayed disability progression in relapsing-remitting MS patients treated with interferon-beta. J Neurol Sci. 2006;244(1-2):97–102.
Zeman AZJ, Kidd D, McLean BN, Kelly MA, Francis DA, Miller DH, et al. A study of oligoclonal band negative multiple sclerosis. J Neurol Neurosurg Psychiatry. 1996;60:27–30.
Mayringer I, Timeltaler B, Deisenhammer F. Correlation between the IgG index, oligoclonal bands in CSF, and the diagnosis of demyelinating diseases. Eur J Neurol. 2005;12(7):527–30.
Imrell K, Greiner E, Hillert J, Masterman T. HLA-DRB115 and cerebrospinal-fluid-specific oligoclonal immunoglobulin G bands lower age at attainment of important disease milestones in multiple sclerosis. J Neuroimmunol. 2009;210(1-2):128–30.
Rojas JI, Tizio S, Patrucco L, Cristiano E. Oligoclonal bands in multiple sclerosis patients: worse prognosis? Neurol Res. 2012;34(9):889–92.
Gajofatto A, Bongianni M, Zanusso G, Benedetti MD, Monaco S. Are cerebrospinal fluid biomarkers useful in predicting the prognosis of multiple sclerosis patients? Int J Mol Sci. 2011;12(11):7960–70.
Confavreux C, Vukusic S, Moreau T, Adeleine P. Relapses and progression of disability in multiple sclerosis. N Engl J Med. 2000;343(20):1430–8.
Debouverie M, Pittion-Vouyovitch S, Louis S, Guillemin F. Natural history of multiple sclerosis in a population-based cohort. Eur J Neurol. 2008;15(9):916–21.
Brex PA, Ciccarelli O, O’Riordan JI, Sailer M, Thompson AJ, Miller DH. A longitudinal study of abnormalities on MRI and disability from multiple sclerosis. N Engl J Med. 2002;346(3):158–64.
Leibowitz U, Alter M. Clinical factors determining prognosis in multiple sclerosis. Neurology. 1968;18(3):286–7.
Confavreux C, Aimard G, Devic M. Course and prognosis of multiple sclerosis assessed by the computerized data processing of 349 patients. Brain. 1980;103(2):281–300.
Detels R, Clark VA, Valdiviezo NL, Visscher BR, Malmgren RM, Dudley JP. Factors associated with a rapid course of multiple sclerosis. Arch Neurol. 1982;39(6):337–41.
Scalfari A, Neuhaus A, Daumer M, Ebers GC, Muraro PA. Age and disability accumulation in multiple sclerosis. Neurology. 2011;77(13):1246–52.
Vukusic S, Confavreux C. Natural history of multiple sclerosis: risk factors and prognostic indicators. Curr Opin Neurol. 2007;20(3):269–74.
Debouverie M, Pittion-Vouyovitch S, Louis S, Roederer T, Guillemin F. Increasing incidence of multiple sclerosis among women in Lorraine. Eastern France Mult Scler. 2007;13(8):962–7.
Debouverie M, Lebrun C, Jeannin S, Pittion-Vouyovitch S, Roederer T, Vespignani H. More severe disability of North Africans vs Europeans with multiple sclerosis in France. Neurology. 2007;68(1):29–32.
El Adssi H, Debouverie M, Guillemin F. Estimating the prevalence and incidence of multiple sclerosis in the Lorraine region, France, by the capture-recapture method. Mult Scler. 2012;18(9):1244–50.
Cortese I, Capone S, Luchetti S, Grimaldi LM, Nicosia A, Cortese R. CSF-enriched antibodies do not share specificities among MS patients. Mult Scler. 1998;4(3):118–23.
Reiber H, Ungefehr S, Jacobi C. The intrathecal, polyspecific and oligoclonal immune response in multiple sclerosis. Mult Scler. 1998;4(3):111–7.
Walsh MJ, Tourtellotte WW. Temporal invariance and clonal uniformity of brain and cerebrospinal IgG, IgA, and IgM in multiple sclerosis. J Exp Med. 1986;163:41–53.
Confavreux C, Compston DA, Hommes OR, McDonald WI, Thompson AJ. EDMUS, a European database for multiple sclerosis. J Neurol Neurosurg Psychiatry. 1992;55:671–6.
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33(11):1444–52.
Barkhof F, Filippi M, Miller DH, Scheltens P, Campi A, Polman CH, et al. Comparison of MRI criteria at first presentation to predict conversion to clinically definite multiple sclerosis. Brain. 1997;120(Pt 11):2059–69.
Hosmer DW, Lemeshow S, May S. Applied Survival Analysis. 2nd ed. Hoboken: John Wiley & Sons; 2008.
Lourenco P, Shirani A, Saeedi J, Oger J, Schreiber WE, Tremlett H. Oligoclonal bands and cerebrospinal fluid markers in multiple sclerosis: associations with disease course and progression. Mult Scler. 2012;0(0):1–8.
Debouverie M. Gender as a prognostic factor and its impact on the incidence of multiple sclerosis in Lorraine. France J Neurol Sci. 2009;286(1-2):14–7.
Vukusic S, Confavreux C. Prognostic factors for progression of disability in the secondary progressive phase of multiple sclerosis. J Neurol Sci. 2003;206(2):135–7.
Abraira V, Alvarez-Cermeno JC, Arroyo R, Camara C, Casanova B, Cubillo S, et al. Utility of oligoclonal IgG band detection for MS diagnosis in daily clinical practice. J Immunol Methods. 2011;371(1-2):170–3.
Hintzen RQ, Giovannoni G. CSF analysis in suspected MS: do bands aid? Neurology. 2008;70:1059–60.
Cepok S, Jacobsen M, Schock S, Omer B, Jaekel S, Boddeker I, et al. Patterns of cerebrospinal fluid pathology correlate with disease progression in multiple sclerosis. Brain. 2001;124(Pt 11):2169–76.
Binquet C, Quantin C, Le TG, Pagliano JF, Abrahamowicz M, Moreau T. The prognostic value of initial relapses on the evolution of disability in patients with relapsing-remitting multiple sclerosis. Neuroepidemiology. 2006;27(1):45–54.
Hecker M, Paap BK, Goertsches RH, Kandulski O, Fatum C, Koczan D, et al. Reassessment of blood gene expression markers for the prognosis of relapsing-remitting multiple sclerosis. PLoS One. 2011;6(12), e29648.
Mandrioli J, Sola P, Bedin R, Gambini M, Merelli E. A multifactorial prognostic index in multiple sclerosis. Cerebrospinal fluid IgM oligoclonal bands and clinical features to predict the evolution of the disease. J Neurol. 2008;255(7):1023–31.
Calabrese M, Federle L, Bernardi V, Rinaldi F, Favaretto A, Varagnolo MC, et al. The association of intrathecal immunoglobulin synthesis and cortical lesions predicts disease activity in clinically isolated syndrome and early relapsing-remitting multiple sclerosis. Mult Scler. 2012;18(2):174–80.
Bejarano B, Bianco M, Gonzalez-Moron D, Sepulcre J, Goni J, Arcocha J, et al. Computational classifiers for predicting the short-term course of Multiple sclerosis. BMC Neurol. 2011;11:67.
Huttner HB, Schellinger PD, Struffert T, Richter G, Engelhorn T, Bassemir T, et al. MRI criteria in MS patients with negative and positive oligoclonal bands: equal fulfillment of Barkhof’s criteria but different lesion patterns. J Neurol. 2009;256(7):1121–5.
Andreadou E, Chatzipanagiotou S, Constantinides VC, Rombos A, Stamboulis E, Nicolaou C. Prevalence of cerebrospinal fluid oligoclonal IgG bands in Greek patients with clinically isolated syndrome and multiple sclerosis. Clin Neurol Neurosurg. 2013;115:2094–8.
Debouverie M, Laforest L, Van Ganse E, Guillemin F, LORSEP Group. Earlier disability of the patients followed in multiple Sclerosis centers compared to outpatients. Mult Scler. 2009;15(2):251–7.
Acknowledgments
We are indebted to all neurologists taking part in the LORSEP group. We thank other sources of the register: national French hospitalization health care system database, regional health insurance system (CNAMTS main health insurance, MSA agricultural health insurance, RSI social welfare for self-employed workers), and medical records departments of Lorraine hospitals.
Funding
The register is supported by the National Institute for Health and Medical Research (INSERM), Health Ministry of France, LORSEP association and the Lorraine Region.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
MD has done consulting research and/or workshops for Biogen-Idec, Bayer-Schering, Merck-Serono, Novartis, Sanofi-Aventis and Teva Pharma. The organizations mentioned in this statement did not participate in any aspects of the design, execution, analysis, or write-up of this study. FG and MD are coordinators of the Lorraine MS register, which received an unrestricted grant from Merck-Serano. The other authors report no conflicts of interest.
Authors’ contribution
MB carried out the data management and statistical analysis and drafted the manuscript. CL supervised the acquisition of data, the statistical analysis and helped to draft the manuscript. MD conceived of the study, participated in its design and coordination and made substantial contribution to the manuscript. CMA performed the biological analysis and contributed to the interpretation of the result and to the revision of the manuscript. ER CMA performed the biological analysis. FG supervised the design of the study and its coordination and made substantial contribution to the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Becker, M., Latarche, C., Roman, E. et al. No prognostic value of routine cerebrospinal fluid biomarkers in a population-based cohort of 407 multiple sclerosis patients. BMC Neurol 15, 79 (2015). https://doi.org/10.1186/s12883-015-0330-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-015-0330-4