Abstract
Background
Hyperechogenicity of the substantia nigra was recently reported in patients with sporadic ALS with a frequency similar to PD. Data on the diagnostic utility compared to key differential diagnoses of ALS do not exist yet.
Methods
We prospectively enrolled 43 patients with ALS, 29 with myasthenia gravis, 25 patients with inflammatory neuropathy, and 13 with cervical canal stenosis. All patients were examined by a blinded investigator using transcranial B-mode sonography planimetrically measuring hyperechogenic areas of the midbrain representing the substantia nigra.
Results
Mean midbrain hyperechogenic area was increased in ALS compared to non-ALS differentials. ROC analysis revealed only small area under the curve for detecting ALS (AUC: 0.669 [95%CI: 0.56-0.78]; p = 0.006). Highest Youden index was observed for area size of <0.14 cm2 (Youden index: 0.28). Using this cut-off score and that generated from normative data of healthy controls, area size measurements provided a sensitivity of only 46-58% and specificity of 69-83% for detecting ALS. No correlations of hyperechogenic area sizes in ALS patients were found to age, gender, ALS subtype (bulbar versus spinal form), disease duration or ALS-FRS-R score.
Conclusions
Midbrain hyperechogenicity is reproducibly found in ALS patients, but its diagnostic value for discriminating ALS from its key differentials is limited.
Similar content being viewed by others
Background
Transcranial B-mode sonography (TCS) of the midbrain is in the meantime well accepted for the differential diagnosis of Parkinson’s disease (PD) and various movement disorders [1-3]. Nine per cent of healthy 20–80 year old controls also show hyperechogenicity of the substantia nigra (SN) which is considered to be associated with a subclinical functional impairment of the nigrostriatal system [3]. We recently reported a similar high prevalence of hyperechogenecity of the substantia nigra in patients with amyotrophic lateral sclerosis (ALS) [4]. This was independently confirmed very recently [5]. No data exist yet on the diagnostic value in the differential diagnosis of motor neuron diseases (MND) compared to key clinical differentials of myasthenia gravis, inflammatory neuropathies and cervical canal stenosis.
Alteration of the regional iron metabolism is suspected to be the underlying neuropathological correlate of SN hyperechogenicity rather than the neurodegenerative process itself [6]. Post-mortem studies have reported a degeneration of the SN in sporadic ALS [7], which resembles stage 3 of the very recently reported neuropathological classification of Braak and Brettschneider [8,9]. Further preliminary studies reported increased iron content in ALS brain tissue [10]. Neuroimaging studies by the use of PET or SPECT have indeed shown abnormal pre-synaptic and post-synaptic striatal dopaminergic function in ALS patients [11,12].
We here prospectively recruited major differential diagnoses of MNDs to evaluate the diagnostic value of SN hyperechogenicity measured by transcranial sonography.
Methods
Subjects
Patients were recruited at the outpatient clinic of the Department of Neurology of the University Hospital Dresden from 2011 to 2013. These included subjects with definite or probable ALS according to the revised El Escorial criteria, antibody proven myasthenia gravis (MG), inflammatory neuropathies (IN) (including Guillain-Barré syndrome, chronic inflammatory demyelinating polyneuropathy, multifocal motor neuropathy) (clinical diagnosis according to European Federation of Neurological Societies and the Peripheral Nerve Society (EFNS/PNS) [13,14]) and cervical canal stenosis (CCS) (clinical diagnosis according to [15]). The study was approved by the institutional review board (EK 11012012; EK 182062012). Altogether, we included the following 110 subjects: 43 with ALS, 29 with myasthenia gravis, 25 with inflammatory neuropathy and 13 with cervical canal stenosis. Demographic and clinical characteristics of the study cohorts are displayed in Table 1.
Transcranial brain sonography
Data acquisition was performed by a blinded rater. Transcranial B-mode sonography (TCS) was performed by the use of a Toshiba Aplio MX, SSA-780A, with a 3 MHz probe located on the temporal bone window. The technical settings were depth 16 mm, brightness variable, dynamic range 45 dB. Each side was measured in three different planes, one above and one below the orbitomeatal line, parallel to the orbitomeatal line and the mean value was used for further analysis. The ipsilateral hyperechogenic SN was measured planimetrically in the midbrain according to standardized techniques as described by Berg and colleagues [3].
Statistical analyses
Data were prospectively analyzed using the software program SPSS version 19.0 (SPSS Inc., Chicago, IL). Data are displayed as mean ± standard deviation (SD) or numbers (%), significance level was set at P < 0.05 (two-sided). ROC plots including calculation of the area under the curve (AUC) were used to display sensitivity and specificity of TCS measures for detection of ALS. For generation of cut-off values from ROC analysis, we used the Youden index as a measure of the theoretical optimum of test scores. Normal values of SN echogenic size were obtained in healthy controls by calculating the mean + 2 × SD leading to a normal range of <0.20 cm2 as reported previously [4] and perfectly fitting to the literature [3]. For the classification of patients with respect to their SN echogenicity, the mean value of bilateral measurements was used. Statistical comparisons of variables were calculated using χ2 test or one-way ANOVA with Bonferroni post-hoc t-test (see Results sections for details). Spearman’s rank correlation coefficient ρ was used to examine correlations (ρ < 0.3 was considered a weak, ρ = 0.3-0.59 a moderate, ρ ≥ 0.6 a strong correlation).
Results
A temporal bone window sufficient for an adequate sonographic analysis of the SN at least on one side was found in 37 of 43 (86%) ALS patients, 20 of 29 (69%) MG patients, 22 of 25 (88%) IN patients, and 12 of 13 (92%) CCS patients (P = 0.139; χ2 test). In subjects with sufficient temporal acoustic bone windows, mean midbrain hyperechogenic areas were significantly higher in ALS compared non ALS patients (P = 0.006; unpaired two-sided t-test:). Compared to the various differential diagnoses, ALS patients had only significant higher mean SN area compared to MG patients (P = 0.015, Bonferroni adjusted post-hoc t-test), but not to all other patients with no significant differences between the differential diagnoses (one-way ANOVA: F-value = 3.4; P = 0.021; Figure 1B).
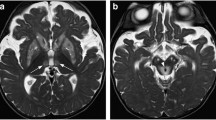
Transcranial sonography (TCS) studies in ALS compared to myasthenia gravis (MG), inflammatory neuropathies (IN) and cervical canal stenosis (CCS). (A) Representative TCS pictures of axial transsections of the brain at midbrain level in one patient with ALS, MG, IN and CCS, respectively. The TCS images show abnormal SN in ALS. In the area of the substantia nigra (SN), a marked hyperechogenicity can be seen. (B) Box plots of SN areas measured by TCS in ALS, MG, IN and CCS patients. The plots show the 10th percentile, first quartile, median, third quartile, and 90th percentile for each parameter. Open circles represent the means. Numbers in parentheses indicate the numbers of patients analyzed. P values are from Bonferroni adjusted post-hoc t-tests. (C) Receiver operating characteristics (ROC) curves displaying the sensitivity and specificity of SN hyperechogenic area for diagnosis of ALS. Insets indicate AUC values, 95% confidence intervals and statistics.
ROC analysis revealing sensitivities and specificities of any particular cut-off value of hyperechogenic SN area size to detect ALS is displayed in Figure 1C. The intervals between cut-off values for area size were between 0.27 cm2 (90th percentile specificity) and 0.07 cm2 (90th percentile sensitivity). The highest Youden index was observed at <0.14 cm2 (Youden index: 0.28). Using the cut-off from normative data from healthy controls of <0.20 cm2 [4], hyperechogenicity was found in 46% (17/37) of ALS patients, in 5% (1/20) of MG patients, in 23% (5/22) of IN patients and in 25% (3/12) of CCS patients, representing a sensitivity of 46% (95%CI: 30-63%) and specificity of 83% (95%CI: 70-91%) to detect ALS in our MND mimics cohort. The sensitivity and specificity values obtained at the maximal Youden index were similar with 58% sensitivity (95%CI: 41-73%) and 69% specificity (95%CI: 55-81%), respectively.
Neither age, gender, MND subtype, ALSFRS-R score, disease duration (r-0.136, p = 0.45) nor pathologically elevated central motor conduction time in magnetic evoked potentials correlated with hyperechogenic SN area.
Discussion
We report data on the diagnostic value of regional midbrain hyperechogenicity determined by TCS in ALS compared to the key differential diagnoses myasthenia gravis, inflammatory neuropathies, and cervical canal stenosis. We showed increased echogenicity of the SN in ALS compared to non ALS differentials, but its diagnostic value is limited, questioning this simple and non-invasive technique as a useful additional technical tool in the differential diagnosis of motor neuron diseases. Hyperechogenic area size in ALS patients did not correlate with age, gender, ALS-FRSR score or disease subtype.
The diagnosis of MND is still done by exclusion of other diseases which have to be considered, as these are for example myasthenia gravis, inflammatory neuropathies and cervical canal stenosis. In some cases this can be particularly difficult in early stages of the disease. Therefore, any diagnostic finding being able to distinguish these challenging differential diagnoses are helpful for the early diagnosis of motor neuron disease. Showing a specificity of >80% using the standard cut-off value TCS seem to be helpful for this purpose, however the sensitivity is rather low (46%). Major limitations of our study are the mono-centric recruitment of patients at a specialized MND centre with a more strongly represented MND patient cohort compared to the mimics cohorts, the rather limited sample size of cervical canal stenosis as an important differential diagnosis the lacking intra-/inter-rater variability measurements.
Our sonography data fits to early pathological studies showing neurodegeneration of the SN region [7] and increased iron content in sporadic ALS brain tissue [10]. Disease spreading to non-motor systems including the midbrain regions was recently reported underlining the hypothesis of a neuronal multisystem disorder [8,9]. Also other neuroimaging techniques revealed functional impairment of the dopaminergic nigro-striatal pathway [11,12]. Recently, hypointense signals in the motor cortex were reported in routine cMRI [16]. In a pilot study using 7 T MRI, this hypointense signal could be localized to deeper cortical layers and – in very preliminary post-mortem analysis – iron depositions (mainly in microglial cells) was found in deeper cortical layers [17]. We do not yet know whether these findings are due to similar neuropathology events as in PD in which the SN hyperechogenicity is due to increased iron content of the midbrain [6].
Conclusion
In summary, substantia nigra hyperechogenecity is reliably and reproducibly observed in ALS patients, but its diagnostic value in discriminating ALS from key ALS mimics is limited. Nevertheless, its value in the diagnostic process of ALS could become one additional cobblestone if one is aware of its limitations.
Ethic committee approval
The study was approved by the local ethics committee of the University of Dresden.
References
Gaenslen A, Unmuth B, Godau J, Liepelt I, Di Santo A, Schweitzer KJ, et al. The specificity and sensitivity of transcranial ultrasound in the differential diagnosis of Parkinson’s disease: a prospective blinded study. Lancet Neurol. 2008;7(5):417–24.
Becker G, Seufert J, Bogdahn U, Reichmann H, Reiners K. Degeneration of substantia nigra in chronic Parkinson’s disease visualized by transcranial color-coded real-time sonography. Neurology. 1995;45(1):182–4.
Berg D, Godau J, Walter U. Transcranial sonography in movement disorders. Lancet Neurol. 2008;7(11):1044–55.
Fathinia P, Hermann A, Reuner U, Kassubek J, Storch A, Ludolph AC. Parkinson’s disease-like midbrain hyperechogenicity is frequent in amyotrophic lateral sclerosis. J Neurol. 2013;260(2):454–7.
Prell T, Schenk A, Witte OW, Grosskreutz J, Gunther A. Transcranial brainstem sonography as a diagnostic tool for amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15(3–4):244–9.
Berg D, Roggendorf W, Schroder U, Klein R, Tatschner T, Benz P, et al. Echogenicity of the substantia nigra: association with increased iron content and marker for susceptibility to nigrostriatal injury. Arch Neurol. 2002;59(6):999–1005.
Kato S, Oda M, Tanabe H. Diminution of dopaminergic neurons in the substantia nigra of sporadic amyotrophic lateral sclerosis. Neuropathol Appl Neurobiol. 1993;19(4):300–4.
Braak H, Brettschneider J, Ludolph AC, Lee VM, Trojanowski JQ, Del Tredici K. Amyotrophic lateral sclerosis-a model of corticofugal axonal spread. Nat Rev Neurol. 2013;9(12):708–14.
Brettschneider J, Del Tredici K, Toledo JB, Robinson JL, Irwin DJ, Grossman M, et al. Stages of pTDP-43 pathology in amyotrophic lateral sclerosis. Ann Neurol. 2013;74(1):20–38.
Kasarskis EJ, Tandon L, Lovell MA, Ehmann WD. Aluminum, calcium, and iron in the spinal cord of patients with sporadic amyotrophic lateral sclerosis using laser microprobe mass spectroscopy: a preliminary study. J Neurol Sci. 1995;130(2):203–8.
Borasio GD, Linke R, Schwarz J, Schlamp V, Abel A, Mozley PD, et al. Dopaminergic deficit in amyotrophic lateral sclerosis assessed with [I-123] IPT single photon emission computed tomography. J Neurol Neurosurg Psychiatry. 1998;65(2):263–5.
Takahashi H, Snow BJ, Bhatt MH, Peppard R, Eisen A, Calne DB. Evidence for a dopaminergic deficit in sporadic amyotrophic lateral sclerosis on positron emission scanning. Lancet. 1993;342(8878):1016–8.
Latov N. Diagnosis of CIDP. Neurology. 2002;59(12 Suppl 6):S2–6.
Van den Bergh PY, Hadden RD, Bouche P, Cornblath DR, Hahn A, Illa I, et al. European Federation of Neurological Societies/Peripheral Nerve Society guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society - first revision. Eur J Neurol. 2010;17(3):356–63.
Muhle C, Metzner J, Weinert D, Falliner A, Brinkmann G, Mehdorn MH, et al. Classification system based on kinematic MR imaging in cervical spondylitic myelopathy. AJNR Am J Neuroradiol. 1998;19(9):1763–71.
Oba H, Araki T, Ohtomo K, Monzawa S, Uchiyama G, Koizumi K, et al. Amyotrophic lateral sclerosis: T2 shortening in motor cortex at MR imaging. Radiology. 1993;189(3):843–6.
Kwan JY, Jeong SY, Van Gelderen P, Deng HX, Quezado MM, Danielian LE, et al. Iron accumulation in deep cortical layers accounts for MRI signal abnormalities in ALS: correlating 7 tesla MRI and pathology. PLoS One. 2012;7(4):e35241.
Acknowledgements
We thank all the patients who participated in this study.
Role of funding
There was no external funding and no sponsor involved in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AH: Conception and design, collection and/or assembly of data, data analysis and interpretation, manuscript drafting. UR: Collection and/or assembly of data, critical revision of manuscript. JS: Collection and/or assembly of data, critical revision of manuscript. PF: Collection and/or assembly of data, data analysis and interpretation, critical revision of manuscript. TL: Collection and/or assembly of data, critical revision of manuscript. JK: Collection and/or assembly of data, data analysis and interpretation, critical revision of manuscript. ML: Collection and/or assembly of data, data analysis and interpretation, critical revision of manuscript. ACL: Idea, data interpretation,critical revision of manuscript. AS: Conception and design, principal investigator, collection and/or assembly of data, data analysis and interpretation, manuscript drafting. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hermann, A., Reuner, U., Schaefer, J. et al. The diagnostic value of midbrain hyperechogenicity in ALS is limited for discriminating key ALS differential diagnoses. BMC Neurol 15, 33 (2015). https://doi.org/10.1186/s12883-015-0280-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-015-0280-x