Abstract
Introduction
Currently, kidney disease is an increasing major health problem worldwide. It is expected to be the 5th ranked cause of death by 2040. If it is early detected, further complication caused by kidney disease will be minimized. An assessment of impaired glomerular filtration rate (eGFR) has potential aids in early identification and treatment of kidney disease. However, in hospital practice instead of using eGFR, direct measurement of serum creatinine level is used for assessing renal function. Hence, this study is aimed to assess the magnitude and associated factors of impaired glomerular filtration rate among admitted patients in Wolkite University Specialized Teaching Hospital (WKUSTH).
Objective
To assess the magnitude and associated factors of impaired glomerular filtration rate in WKUSTH, Ethiopia 2023.
Method
Institutional based cross-sectional study with secondary data was conducted. 338 participants were selected by a convenient sampling technique. Epidata 3.1 version for data entry and SPSS version 20 for data analysis was used. Bivariate analysis was used to screen candidate variables for multivariate analysis. In the multivariate analysis a P-value < 0.05 were considered statistically significant.
Results
The study enrolled 338 patients admitted to WUSTH. Seventy (20.7%) (95% CI: 16.6–25.4%) of them had impaired eGFR according to Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation and Modification of Diet in Renal Disease (MDRD-4). older age (AOR 3.38, 95% CI; 1.31, 8.71), hypertension (AOR 17.8, 95% CI; 7.75, 41.22), anemia (AOR 2.51, 95% CI; 1.11, 5.83) DM (AOR 11.2, 95% CI; 4.11, 30.73), and high BMI (AOR 7.56, 95% CI; 3.16, 18.08), were independently associated with impaired eGFR.
Conclusions
The magnitude of impaired eGFR was prevalent among adult patients admitted to WKUSTH medical ward with different medical conditions. Old age, Hypertension, Diabetes, high body mass index, and Anemia were significantly associated with impaired eGFR both in CKD-EPI and MDRD-4 equation. Estimation of GFR for all hospitalized adults with known CKD risk factors might help in early detection of CKD and prevent complications.
Similar content being viewed by others
Introduction
Globally, the burden of kidney disease is increasing and resulting in an increased hospitalized morbidity and mortality [1]. There are two types of kidney disease: acute, which can appear quickly, and chronic, which can appear gradually over time. Acute renal damage is very common, with a 16% incidence rate identified in hospitalized patients [2]. In the 21st century, chronic kidney disease (CKD) has become one of the leading causes of death and disability [3]. In 2017, the mortality rate of CKD was ranked as the 12th leading cause of death and is expected to rise to 5th ranked by 2040. Kidney disease is also associated with an independent risk factor for morbidity and premature mortality of cardiovascular disease (CVD). Globally, from 1·4 million deaths due to cardiovascular disease, kidney disease was attributed to represent 7·6% of deaths [4]. The complications of kidney disease are not restricted to CVD but also include hypertension, anemia, malnutrition, and mineral and bone disorders [5].
Kidney disease is not only an important public health problem; rather, it also has a big economic burden. It is associated with increased hospitalization, morbidity, early mortality, and productivity loss for patients and their caregivers [6, 7]. Undiagnosed and untreated patients with kidney disease also have a high risk of progression to End Stage Renal Disease (ESRD). The cost of ESRD management is very high because it requires either dialysis or kidney transplantation [8]. In developed countries, treatment of ESRD shares more than 2–3% of their annual healthcare budget [9]. There are about $20,110 to $100,593 annual medical costs per patient for ESRD management in developed countries [6].
About 12–23% of sub-Saharan African (SSA) adults had kidney disease. However, from renal replacement therapy requiring SSA patients, only 1·5% of patients get access due to lack of access and higher costs of dialysis and transplantation [10]. This leads to a high morbidity and mortality rate, low life expectancy, and poor quality of life in SSA [11]. Hence, early detection of kidney disease is required, especially in this resource-limited county, to prevent or delay its progression to ESRD.
The primary biomarker for abnormal kidney function is a Glomerular Filtration Rate (GFR) of < 60 mL/min/1.73 m2 [12]. Measuring GFR is useful in the early detection of kidney disease, identifying the stages of the disease, and monitoring renal functions. It also guides the dosing of drugs, especially for hospitalized patients [13, 14]. However, the advantage of early detection of kidney disease using eGFR has not been sufficiently noted by the patient and even by the stakeholders. In the majority of health institutions, instead of using eGFR, direct measurement of serum creatinine levels is used for assessing renal function tests. However, serum creatinine is raised when there is a substantial reduction in the GFR or when urine elimination is obstructed. Before an increase in serum creatinine is seen, about 50% of renal function must be lost, and it is not able to reveal the disease’s stage [15]. This might be the reason why most patients with kidney disease are unaware of their condition until they develop ESRD, especially in developing countries like Ethiopia. Hence, this study is aimed to assess the magnitude and associated factors of impaired glomerular filtration rate among admitted patients in WKUSTH.
Method and material
Study design, setting and population
An institutional based cross-sectional study was conducted from November 15, 2022, to February 28, 2023, in WKUSTH, which is located in the Southern Nation Nationalities Regional State (SNNP), Gurage Zone, Wolkite, located 158 km southwest of the capital city, Addis Ababa, on the way to Jimma. The hospital situated in Gubreye sub-city, 14 km east of Wolkite town. Currently, WKUSTH is offering outpatient, inpatient, surgical, gynecological, and pediatric services.
Aged 18 years or older patients admitted to the medical wards of WKUSTH during the study period and signed on the consent sheet were included. However, patients on the intensive care unit who were unconscious, younger than 18 years old, amputated patient, pregnant women, admitted due to malnutrition, and morbidly obese patient were excluded. During the study period, 697 patients were admitted to the adult medical ward. From these admitted patients, a total of 338 patients were selected using consecutive sampling technique. The sample size was determined by using a single population proportion formula (N = (Zα/2)2 P (1-P) /d2) with a 32.7% prevalence (P) of impaired glomerular filtration rate among adult hospitalized patients from the previous study conducted in Jimma [16], an assumption of a 95% confidence level, and a 5% margin of error (d). Then the calculated sample size for our study is 338.
Data collection procedures and technique
After detailed information about the study was given and written consent was obtained from all subjects who were included in the study, data were collected using a pretested semi-structured face to face interviewing questionnaire that was developed from the WHO STEPS surveillance manual [17]. The questionnaire includes variables for the assessment of socio-demographics, clinical information and lifestyle behaviors, anthropometrics, blood pressure measurements, and laboratory finding. A trained nurse conducted interviews with patients to gather information on lifestyle behaviors, clinical information, and socio-demographic characteristics.
By examining their medical record, more data was gathered regarding the patient’s comorbidities, such as diabetes mellitus, cardiovascular disease, hypertension, and HIV/AIDS. A history of hypertension, being on antihypertensive medication, or having an average of three readings of systolic and/or diastolic blood pressure greater than 140/90 mm Hg were considered to be indicators of hypertension. All other comorbidities, such as DM, cardiovascular disease, and HIV/AIDS, were defined as present if they were documented in the medical records.
Anthropometrics and blood pressure were measured by trained clinical nurses. Each subject’s height and weight were recorded, and the BMI was computed by dividing the weight in kilograms (kg) by the height in meters (m2). A high BMI was defined as BMI ≥ 25 kg/m2. Since the eGFR equation is inaccurate for comorbid obesity, patients with a BMI ≥ 40 kg/m2 were excluded from our study.
Following the completion of an interview, record review, and the measurement of anthropometric and BP values by a clinical nurse, the laboratory professional conduct the patient. Subsequently, the vein located in the antecubital fossa of the forearm was sterilized using a 70% alcohol solution. A tourniquet was then applied as necessary. Five mL of venous blood samples were collected at any time during the hospitalization using a syringe and needle collection system. Two ml of blood was transferred to EDTA test tube for CBC analysis. CBC was analyzed using the CELL DYNE 1800 hematology, analyzer. Those with hemoglobin value < 12 mg/dl for females and < 13 mg/dl for males were considered as anemic. Three ml of blood was transferred to sterile serum-separating tubes and left to form a clot at room temperature for 30 min. Then the clotted blood samples was centrifuged for 5 min at 4000 revolutions per minutes (rpm) to separate serum from formed elements for biochemical test analysis. The extracted serum was analyzed for Creatinine determination using the Roche Diagnostic Cobas C311 Automated Clinical Chemistry Analyzer by the enzymatic method.
The CKD-EPI Creatinine Eq. (2021) and the four-variable version of the MDRD equation, which was updated in 2006, are used to mathematically estimate serum creatinine-based GFR for all study participants. Those with eGFR < 60 are considered as having impaired eGFR. All laboratory measurements were done following the standard procedures recommended by the manufacturer, and a quality control test was done for all tests before running the sample.
Data quality assurance and management
Data collections were carried out after approval of the research proposal. To ensure the accuracy and reliability of the data, questionnaires and informed consent forms that were originally written in English were translated into the local languages of Amharic. These translations were then retranslated back into English to ensure consistency and precision. Before the actual data collection process, a pretest was conducted on a small portion of the total sample size, specifically 5% (consisting of 17 subjects who met the eligibility criteria), at Atat Hospital.
During the study period, the quality of socio-demographic, anthropometric, and clinical data was ensured through daily checks for completeness and consistency by on-site supervision of data collectors. To uphold confidentiality, a code was utilized to safeguard the test results of study participants, with records securely stored in an undisclosed location. Feedback and necessary corrections were given throughout the daily data collection process.
The laboratory ensured the integrity of the data by following the guidelines provided by the manufacturer and adhering to standard operating procedures throughout the process of specimen collection and Analysis. To avoid any confusion, both the container holding the sample and the corresponding request form were marked with identical identification codes following the collection process. Before any patient sample processed, Roche Diagnostic Cobas C311 Automated Clinical Chemistry Analyzer and CELL DYNE 1800 hematology analyzer was checked for delivering correct result by using dual quality controls (normal and pathological) and the patient result was taken after the controls passed. Calibration is done when new reagent is purchased and the quality control is not passed. All necessary procedures and steps were followed based on the manufacture instructions.
Statistical analysis and procedure
Data were coded and entered into epidata version 3.1 for further data cleaning and to allow consistency and eliminate discrepancies. Then, it was exported to SPSS version 20 software for analysis. Descriptive statistics like frequency, percentages, means, and standard deviations were used to describe the findings. Both bivariate and multivariate logistic regression was done. Bivariate logistic regression analysis was conducted to see the existence of crude association and to select candidate variables. All Variables with a p-value of less than 0.25 in the bivariate analysis were included in multivariate logistic regression. Multivariate logistic regression analysis was done to control possible confounders and to determine factors that may be significantly associated with eGFR. P value < 0.05 was considered statistical significance in the final model.
Ethical considerations
Before any attempt to collect data, approval to conduct the study, ethical clearance was obtained from the ethical review board of Jimma University Institute of Health with a protocol number IRHPGn/576 after approval of the research proposal. A supportive letter was also obtained from Jimma University School of Medical Laboratory to WKUSTH. The study protocol and supportive letter was submitted to WKUSTH and permission to conduct the study was obtained from WKUSTH. Each participant was notified about the purpose of the study, the right to refuse to participate in the study, and the anonymity and confidentiality of the information gathered. A written consent was obtained from the participants after explaining the risk and benefit of the study. The study was carried out in accordance with the 1975 Helsinki declaration, as revised in 2008, and its later amendments or comparable ethical standards.
Result
Socio-demographic characteristics
A total of 338 individuals with a 100% response rate participated, and the proportions of male (51.2%) and female (48.8%) participants were almost similar. The mean age of the study participants was 51.71 (SD = 17.66) years; 44.7% were in the age group above 59 years. Regarding educational status, 163 (48.2%) Couldn’t read and write. While those who had completed college and above were less than 10% (8.6%). About two-third of the participants, 214 (63.3%) were from rural areas, and 155 (45.9%) of them were farmers (Table 1).
Clinical and lifestyle characteristics
The main clinical diagnosis for admission in this study was hypertension (24.9%), followed by anemia (24.0%), DM (15.7%), and cardiac problems (11.2%). Regarding HIV/AIDS status, 10 (3.0%) participants were HIV positive (Table 2).
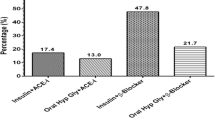
Pattern of impaired eGFR
From the total participants 70 (20.7%) (95% CI: 16.6–25.4%) of them had impaired eGFR according to the CKD-EPI equation and MDRD-4. The mean serum creatinine level of the study participants was 1.078 mg/dl whereas the mean eGFR by MDRD-4 and CKD-EPI of the study subjects were 115.06 and 100.25, respectively. Using the CKD-EPI equation, 1 (0.3%) of study participants had eGFR < 15 ml/min/1.73m2, 30 (8.9%) had eGFR of 15-29.9 ml/min/1.73 m2, 24 (7.1%) had eGFR of 30-44.9 ml/min/1.73m2, and 15 (4.4%) had eGFR of 45-59.9 ml/min/1.73m2. On the other hand, Using MDRD-4 equation, 1 (0.3%) had eGFR < 15 ml/min/1.73m2, 21 (6.2%) had eGFR of 15-29.9 ml/min/1.73m2, 29 (8.6%) had eGFR of 30–44. ml/min/1.73m2, and 19 (5.6%) had eGFR 45-59.9 ml/min/1.73m2 (Fig. 1).
Factors associated with impaired eGFR
Bivariable and multivariable logistic regression was conducted to see the association between dependent and independent variables. Accordingly, on bivariable analysis variables like age > = 60 years (COR 3.79, 95% CI; 2.15,6.69), occupational status (COR, 1.77, 95% CI; 1.04,3.02), educational status (COR, 1.82, 95% CI; 1.06,3.11) Hypertension (COR 14.7, 95%; 95% CI; 7.06,26.00), anemia (COR, 3.76, 95% CI; 2.14,6.60) DM (COR 5.84, 95% CI; 3.11,10.95), heart problem (COR 2.3, 95% CI; 1.1,4.6), alcohol consumption (COR 2.7, 95% CI; 1.24, 5.9), cigarette smoking (COR 3.5, 95% CI; 1.37,8.68), and BMI > = 25 (COR,5.53, 95% CI; 3.21,9.83) were significantly associated with impaired eGFR at P < 0.25 and entered into multivariable analysis. Lastly, in multivariable analysis, older age (AOR 3.38, 95% CI; 1.31, 8.71), hypertension (AOR 17.8, 95% CI; 7.75, 41.22), anemia (AOR 2.51, 95% CI; 1.11, 5.83) DM (AOR 11.2, 95% CI; 4.11, 30.73), and high BMI (AOR 7.56, 95% CI; 3.16, 18.08), were independently associated with impaired eGFR (Table 3).
Discussion
Currently, due to different factors like lifestyle changes and the increasing prevalence of non-communicable chronic diseases like hypertension and DM, kidney disease has become one of the major public health problems worldwide. Especially because of the huge economic burden of ESRD, early detection and prevention of kidney disease is a critical issue. However, the advantage of early detection and prevention of kidney disease has not been sufficiently noted by the patient and even by the stakeholders. From now on, it is commonly unrecognized and leads to further complications.
Our study indicated that seventy (20.7%) (95% CI: 16.6–25.4%) of the study participants had impaired eGFR according to the CKD-EPI equation and MDRD-4. This finding was comparable with a study conducted at Jimma University Medical Center (19.4%), and (19.2%) according to the CKD-EPI equation and MDRD-4, respectively [16], Dessie referral hospital (19.0%) [18], London (17.7%) [19]. However, the result of this finding was lower compared to a study conducted in Spain (28.3%) [20], Germany (27.5%) [21], and Guinea (33%) [22]. This difference might be due to population characteristics, or it might be due to more complex medical patients. Other studies conducted in Uganda 15.3% [23], Canada 8.5% [24], and Brazil 12.7% [25] had reported a lower prevalence of impaired eGFR compared to our study. This difference might be due to differences in sample size and/or population characteristics.
In our study, the prevalence of impaired eGFR using MDRD4 and CKD-EPI equations is equal. This is roughly consistent with the study conducted in Southwest Ethiopia [26] and Jimma University Medical Center [16] which found the highest agreement between MDRD and CKD-EPI equations for GFR estimation. Therefore, in this study area, either CKD-EPI or MDRD can be used to estimate GFR.
In the present study, factors associated with impaired eGFR were older age, hypertension, anemia, DM, and BMI. Accordingly, our results reveal that hypertensive patients had about eighteen times more likely increased risk of having impaired eGFR when compared to patients without hypertension. This finding was in line with previous studies [16, 18, 23, 27, 28].
According to our study, DM was also a risk factor for impaired eGFR. Those having DM have about eleven times more likely increased risk of developing impaired eGFR when compared to patients without DM. This finding was consistent with former studies [18, 23, 25, 29]. In the present study, older age was also independently associated with impaired eGFR. This finding was consistent with prior studies [16, 18, 25, 28]. This is probably due to increased renal risk factors such as DM, hypertension, and heart problems or structural and functional changes in the aging kidneys.
High BMI was associated with impaired eGFR, which showed that patients with a BMI > 25 were 7.56 times more likely to develop impaired eGFR as compared to their counterparts. This finding was similar to a study conducted in Cameroon [30], North-Central Nigeria [29], and Tigray teaching hospitals [31]. This is most probably due to the fact that as BMI increases, renal risk factors such as DM, hypertension, and heart problems will also increase. Anemia was also independently associated with impaired eGFR. This is in line with a study conducted in Kenya [28].
Even though this study has much strength, it has a few limitations. As the study was conducted in only one hospital and the sampling technique was convenient, it may be difficult to represent the whole population of admitted patients. Our study design was a cross-sectional study; being a cross-sectional study by design, we cannot observe a causal relationship between assessed risk factors and eGFR.
Conclusions and recommendations
The magnitude of impaired eGFR among adult patients admitted to a medical ward at WKUSTH was significant. On the other hand, MDRD-4 and CKD-EPI equations deliver comparable results, especially at an estimated GFR less than 60 mL/min per 1.73 m2. Older age, high BMI, anemia, and having comorbidity diseases like hypertension and diabetes mellitus were found to be significantly associated with impaired eGFR. Estimation of GFR for all hospitalized patients might help in the early detection of kidney disease and prevent complications. Despite the fact that many guidelines advocate for the eGFR-based diagnosis of patients, this approach is uncommon in the study region. Hence, policymakers need to design strategies to screen and diagnose kidney disease based on eGFR in hospitalized patients, to enhance health education about risk factors and the advantage of early detection of kidney disease.
Data availability
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body Mass Index
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- CKD:
-
Chronic kidney disease
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetic Mellitus
- eGFR:
-
Estimated glomerular filtration rate
- ESRD:
-
End-stage renal disease
- GFR:
-
Glomerular filtration rate
- HIV:
-
Human immunodeficiency virus
- MDRD :
-
Modification of Diet in Renal Disease
- SSA:
-
Sub-Saharan African
- WKUSTH:
-
Wolkite university specialized teaching hospital
References
Haileamlak A. Chronic kidney disease is on the rise. Ethiop J Health Sci. 2018;28(6):681.
Gonsalez SR, Cortês AL, da Silva RC, Lowe J, Prieto MC, da Silva Lara L. Acute kidney injury overview: from basic findings to new prevention and therapy strategies. Pharmacol Ther. 2019;200:1–12.
Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Supplements. 2022;12(1):7–11.
Luyckx VA, Tonelli M, Stanifer JW. The global burden of kidney disease and the sustainable development goals. Bull World Health Organ. 2018;96(6):414.
Clarke W, Marzinke M. Contemporary practice in clinical chemistry. Academic; 2020.
Elshahat S, Cockwell P, Maxwell AP, Griffin M, O’Brien T, O’Neill C. The impact of chronic kidney disease on developed countries from a health economics perspective: a systematic scoping review. PLoS ONE. 2020;15(3):e0230512.
Schrauben SJ, Chen H-Y, Lin E, Jepson C, Yang W, Scialla JJ, et al. Hospitalizations among adults with chronic kidney disease in the United States: a cohort study. PLoS Med. 2020;17(12):e1003470.
Gbaguidi GN, Houehanou CY, Amidou SA, Vigan J, Houinato DS, Lacroix P. Prevalence of abnormal kidney function in a rural population of Benin and associated risk factors. BMC Nephrol. 2021;22(1):1–9.
Kumela Goro K, Desalegn Wolide A, Kerga Dibaba F, Gashe Fufa F, Wakjira Garedow A, Edilu Tufa B et al. Patient awareness, prevalence, and risk factors of chronic kidney disease among diabetes mellitus and hypertensive patients at Jimma University Medical Center, Ethiopia. BioMed research international. 2019;2019.
Ashuntantang G, Osafo C, Olowu WA, Arogundade F, Niang A, Porter J, et al. Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-saharan Africa: a systematic review. Lancet Global Health. 2017;5(4):e408–17.
Adjei DN, Stronks K, Adu D, Beune E, Meeks K, Smeeth L, et al. Chronic kidney disease burden among African migrants in three European countries and in urban and rural Ghana: the RODAM cross-sectional study. Nephrol Dialysis Transplantation. 2018;33(10):1812–22.
Johnson CA, Levey AS, Coresh J, Levin A, Eknoyan JGL. Clinical practice guidelines for chronic kidney disease in adults: part 1. Definition, disease stages, evaluation, treatment, and risk factors. Am Family Phys. 2004;70(5):869–76.
Girum T, Mesfin D, Bedewi J, Shewangizaw M. The burden of noncommunicable diseases in Ethiopia, 2000–2016: analysis of evidence from global burden of disease study 2016 and global health estimates 2016. International journal of chronic diseases. 2020;2020.
Tegegne B, Demeke T, Amme S, Edmealem A, Ademe S. Knowledge towards prevention and early detection of chronic kidney disease and associated factors among hypertensive patients at a chronic illness clinic of Jimma Town Public Hospitals. BioMed Research International. 2020;2020.
Gounden V, Bhatt H, Jialal I. Renal function tests. 2018.
Adugna T, Merga H, Gudina EK. Impaired glomerular filtration rate, high grade albuminuria and associated factors among adult patients admitted to tertiary hospital in Ethiopia. BMC Nephrol. 2018;19(1):1–11.
Organization WH. WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance. World Health Organization; 2005. Report No.: 9241593830.
Fiseha T, Ahmed E, Chalie S, Gebreweld A. Prevalence and associated factors of impaired renal function and albuminuria among adult patients admitted to a hospital in Northeast Ethiopia. PLoS ONE. 2021;16(2):e0246509.
Annear N, Banerjee D, Joseph J, Harries T, Rahman S, Eastwood J. Prevalence of chronic kidney disease stages 3–5 among acute medical admissions: another opportunity for screening. QJM: Int J Med. 2008;101(2):91–7.
De Francisco A, Fernandez E, Cruz J, Casas M, Gómez-Gerique J, León A, et al. Under-recognized renal insufficiency in hospitalized patients: implications for care. Eur J Intern Med. 2010;21(4):327–32.
Lüders F, Fürstenberg T, Engelbertz C, Gebauer K, Meyborg M, Malyar NM, et al. The impact of chronic kidney disease on hospitalized patients with peripheral arterial disease and critical limb ischemia. Angiology. 2017;68(2):145–50.
Kaba M, Camara M, Béavogui M, Bah A, Fousény D, Kourouma M et al. Risk factors for chronic kidney disease among patients admitted to the medical wards in Conakry. Saudi J Kidney Dis Transplantation. 2016;27(5).
Kalima N, Gabriel B, Muhindo R, Muyingo A. Chronic kidney disease in patients admitted to the medical ward of Mbarara Regional Referral Hospital in southwestern Uganda: prevalence and associated factors. Int J Med Biomedical Res. 2015;4(2):107–16.
Bohlouli B, Tonelli M, Jackson T, Hemmelgam B, Klarenbach S. Risk of hospital-acquired complications in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2016;11(6):956–63.
Pinho NAd S, GVd, Pierin AMG. Prevalence and factors associated with chronic kidney disease among hospitalized patients in a university hospital in the city of São Paulo, SP, Brazil. Brazilian J Nephrol. 2015;37:91–7.
Kebede KM, Abateneh DD, Teferi MB, Asres A. Chronic kidney disease and associated factors among adult population in Southwest Ethiopia. PLoS ONE. 2022;17(3):e0264611.
Rwegerera G, Bayani M, Taolo E, Habte D. The prevalence of chronic kidney disease and associated factors among patients admitted at princess marina hospital. Gaborone Botsw Nigerian J Clin Pract. 2017;20(3):313–9.
Mwenda V, Githuku J, Gathecha G, Wambugu BM, Roka ZG, Ong’or WO. Prevalence and factors associated with chronic kidney disease among medical inpatients at the Kenyatta National Hospital, Kenya, 2018: a cross-sectional study. Pan Afr Med J. 2019;33.
Olanrewaju TO, Aderibigbe A, Popoola AA, Braimoh KT, Buhari MO, Adedoyin OT, et al. Prevalence of chronic kidney disease and risk factors in North-Central Nigeria: a population-based survey. BMC Nephrol. 2020;21(1):1–10.
Hamadou B, Boombhi J, Kamdem F, Fitame A, Amougou SN, Mfeukeu LK, et al. Prevalence and correlates of chronic kidney disease in a group of patients with hypertension in the Savanah zone of Cameroon: a cross-sectional study in Sub-Saharan Africa. Cardiovasc Diagnosis Therapy. 2017;7(6):581.
Bahrey D, Gebremedhn G, Mariye T, Girmay A, Aberhe W, Hika A, et al. Prevalence and associated factors of chronic kidney disease among adult hypertensive patients in Tigray teaching hospitals: a cross-sectional study. BMC Res Notes. 2019;12(1):1–5.
Acknowledgements
The authors are thankful to Jimma University, Wolkite University Specialized Hospital, study participants, data collectors, and supervisors for the support of the overall process of this study.
Funding
This research did not receive any specific grant from any funding agencies.
Author information
Authors and Affiliations
Contributions
B.F. conceived the study, prepared the proposal, analyzed the data, interpreted the findings, and wrote the manuscript. G.A., H.B., and S.A. were involved in data analysis and reviewing of the manuscript. D.A. and N.C. participated in editing and revising subsequent drafts of the paper. All authors reviewed the final version of the manuscript, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Habtu, B.F., Ayele, G., Belay, H. et al. Assessment of impaired glomerular filtration rate and associated factors in South West Ethiopia: a cross-sectional study. BMC Nephrol 25, 259 (2024). https://doi.org/10.1186/s12882-024-03700-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-024-03700-0