Abstract
Background
A better understanding of the association between chronic kidney disease (CKD) and glaucoma is required to optimize clinical outcomes. Therefore, this study aimed to investigate the association of chronic kidney disease (CKD) with new diagnoses of glaucoma over time from January 2009 to December 2019.
Method
This retrospective propensity-matched cohort study utilizing Taiwanese electronic health records examined the incidence of newly diagnosed glaucoma in patients with and without chronic kidney disease (CKD). The exposure variable was the diagnosis of CKD, identified through diagnostic codes. The primary outcome was the incidence of new-onset glaucoma. Subgroup analyses on glaucoma risk included age, gender, comorbidities, glaucoma subtypes, and dialysis status. Statistical analyses included Kaplan–Meier analysis, Cox proportional hazards models, and Poisson regression models, with the associated hazard ratios and confidence intervals reported.
Results
Seven hundred twenty-three thousand two hundred sixteen patients with CKD (42.3% female; mean [SD] age at index, 66.3 [15.6] years) and 723,216 patients without CKD (42.3% female; mean [SD] age at index, 66.3 [15.7]) were recruited. We showed a significantly increased risk of glaucoma irrespective of subtypes in CKD patients compared to those without CKD (HR: 1.29 [CI: 1.26–1.32], p < 0.001). Kaplan–Meier curves revealed a significantly increased glaucoma risk in both the dialytic subtype and non-dialytic CKD patients when compared to their non-CKD counterparts (p < 0.001). We also showed that all genders (aHR 1.17 [CI: 1.13–1.21] for females vs. aHR 1.39 [CI:1.35–1.43] for males), all ages (< = 49: aHR 1.49 [CI: 1.37–1.62]; 50–59: aHR 1.48 [CI: 1.40–1.56]; 60–69: aHR 1.30 [CI: 1.25–1.6]; 70–79: aHR 1.21 [CI: 1.17–1.26]; > 80: aHR 1.29 [CI: 1.21–1.37]); all income brackets and all urbanization status were associated with significantly increased risk of glaucoma from among the CKD cohort when compared to their respective non-CKD cohort (p < 0.001).
Conclusions
Our cohort study spanning 12 years showed an elevated glaucoma risk following a CKD diagnosis compared to a frequency-matched non-CKD cohort. Our findings have relevance for the clinical practice of at-risk CKD patients.
Trial registration
Due to the retrospective nature of the study, no registration was necessary.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is a major public health issue, with recent estimates of 26 million United States adults being affected [1]. Ocular complications like diabetic retinopathy have been described. This is unsurprising given the developmental similarities between the ocular and renal organs [2]. Emerging evidence suggests a link between glaucoma and CKD, potentially due to mechanisms such as renin-angiotensin system dysfunction [3], which can disrupt ocular fluid homeostasis and the blood–brain barrier at the optic nerve head [4] (refer to Supplementary Fig. 1). Other mechanisms include the involvement of inflammatory-related pathways. However, current studies on glaucoma involvement among CKD patients are either limited in size or the study design was not comprehensive enough. For example, Ro et al. relied on the Korean diagnostic code, limiting its generalizability and reproducibility of results among researchers outside of Korea [5]. Such limitations in current studies hinder a more comprehensive understanding of the association between CKD and glaucoma. Glaucoma, a neurodegenerative disease characterized by retinal ganglion cell dysfunction and visual field defects, is a leading cause of blindness worldwide [6] and significantly impacts the quality of life. One study suggested that concordant comorbidities among CKD patients were associated with an increased risk of hospitalization and poorer clinical outcomes if not managed properly [7]. In other words, these findings suggest that early diagnosis and comprehensive care of comorbidities can lead to better clinical outcomes for CKD patients. Therefore, this study aimed to evaluate the associations between CKD and specific comorbidity with potentially severe visual implications (i.e., glaucoma) and to identify factors contributing to glaucoma development, using data from Taiwan's National Health Insurance Research Database (NHIRD) to improve care for at-risk CKD cohorts.
Methods
Database descriptions
Datasets from the Longitudinal Health Insurance Database (LHID) of the NHIRD were utilized. The limitations section will elaborate further on the challenges associated with studies utilizing electronic health records (EHRs) such as the LHID, including classification bias from inaccurate diagnostic codes. Despite these issues, the validity of EHR usage in epidemiological research has been established in previous studies [8]. The NHIRD is a federated database managed by the Taiwan National Health Insurance Administration (NHIA), comprising a randomized sample of one million patients from a population exceeding 21 million enrollees across Taiwan since 2000. The LHID subset contains electronic health records encompassing basic demographics, diagnoses, examinations, and prescriptions obtained from outpatient and inpatient care settings. All data within the LHID are presented in aggregated form, containing statistical summaries of de-identified information. Furthermore, the database has complied with the "Personal Information Protection Act" of Taiwan. Access to the LHID is restricted to researchers affiliated with medical institutions who have obtained prior approval from the NHIA. Studies utilizing the LHID does not contain human participants and are exempt from review by the China Medical University Hospital Institutional Review Board (Taichung, Taiwan). The China Medical University Hospital Institutional Review Board also waived patient consent requirements due to the use of de-anonymized data. This research adhered to the Strengthening the Reporting of Observation Studies in Epidemiology (STROBE) reporting guideline.
Study population and cohort definitions
This was a retrospective, population-based cohort study that recruited 723,216 patients diagnosed with CKD (referred to as the CKD cohort) and an equal number of frequency-matched individuals (723,216) with no previous history of CKD documented (referred to as the non-CKD cohort). The index event for the CKD cohort was an encounter diagnosis of CKD. Inclusion in the CKD cohort was based on relevant clinical encounter diagnosis International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes. Specifically, patients were recruited into our CKD cohort if their CKD diagnosis was present for at least two medical encounters in an outpatient setting or at least one encounter in an inpatient setting (refer to Supplementary Table 1, Supplementary Fig. 2, Supplementary Fig. 3). The study period was from January 1st, 2009, to December 31st, 2015.
Furthermore, we identified dialytic CKD within the CKD cohort with a history of receiving dialysis procedures for at least 3 months or more (refer to Supplementary Table 1).
Our exclusion criteria excluded those with a previous history of glaucoma before the index date, as indicated by the corresponding ICD-10 codes (refer to Supplementary Table 1). Our exclusion criteria also excluded those under 18 years old, patients whose index dates were not between 2009 and 2015, patients with missing demographic data, and patients with no follow-ups. A 1:1 ratio of frequency matching was employed to create a 1:1 match between individuals with CKD with those who did not have a history of CKD. Covariates included in the frequency matching encompassed sex, age, and year of index date.
Baseline covariates and outcome
Demographic characteristics included age (categorized as < = 49, 50–59, 60–60, 70–79 > = 80 years), gender, income and urbanization status (refer to Table 1).
This study used the Taiwanese insurance premium to extrapolate the estimated individual income. Income status was classified into three groups: (1) low income: lower than 17,800 New Taiwan dollar (NT$) per month (US$568); (2) moderate income: 17,800 -43,900 NT$ per month (US$568 -1402); and high income: 43,900 NT$ per month (US$1402). This income classification was based on the minimum monthly income for the year 2012 in Taiwan (set at NT$ 17,800).
The urbanization level of the study participants extracted from the NHIRD in our study was categorized into four subtypes based on various factors calculated by the NHIRD platform. These factors include the population density of the residential area of the individual enrollee and the percentage of residents with at least a form of tertiary education. These four urbanization subtypes were urban (urbanization level 1), sub-urban (urbanization levels 2–3), and rural (urbanization level 4 +).
The primary endpoint was the development of new-onset glaucoma. This was defined as the new (or first-time) encounter diagnosis ICD-10 code of glaucoma or those who received glaucoma-related eye drops within the follow-up period. Our follow-up period was from 2009 to 2019.
Statistical analysis
The characteristics of the study population were described based on CKD status before and after frequency matching. We used a Chi-square test for the categorical variable and a Student T-test for the continuous variables. Individuals were either censored at the end of the study period or upon loss to follow-up, whichever occurred first, for all analyses. The incidence density rate of glaucoma for each cohort was estimated by dividing the number of glaucoma event occurrences by the total follow-up time (per 1000 person-years). The Poisson regression model was also used to assess the CKD patients, the non-CKD control associated incidence rate ratio (IRR) for glaucoma, and 95% confidence intervals (CIs). A Multivariable Cox proportional hazard regression model was conducted to estimate the hazard ratio [9] and 95% CI of developing glaucoma. The multivariable models were adjusted for sex, age, income, urbanization and comorbidities of hypertension, diabetes mellitus, hyperlipidemia, stroke, and dementia. The proportional hazard model assumption was examined using a test of scaled Schoenfeld residuals. In models evaluating the glaucoma risk, results of the test revealed no significant relationship between Schoenfeld residuals for CKD and follow-up time. The cumulative incidence of glaucoma was calculated using the Kaplan-Meir analysis with log-rank test. All hypothesis tests were two-sided, and statistical significance was considered when the P-value was less than 0.05.
Results
Baseline demographics
Seven hundred twenty-three thousand two hundred sixteen patients with CKD (42.3% female; mean [SD] age at index, 66.3 [15.6] years) and 723,216 patients without CKD (52.3% female; mean [SD] age at index, 66.3 [15.7]) were recruited (refer to Table 1). With non-CKD counterparts as reference, there was a greater proportion of CKD patients with hypertension (71.8% of total CKD cases), diabetes (42.3%), hyperlipidemia (44.8%), stroke (12.9%), and dementia (7.16%). In terms of income, 32.6% of the CKD cohort are of low-income level (monthly income < 17,880 NT$), 52.4% had moderate-income level (17,880 NT$-43,990), and 15.1% had high-income level (> 43,900 NT$). Regarding urbanization level [9], 49.9% of the CKD cohort is classified as UL 1, 39.3% as UL 2, 8.65% as UL 3, and 2.2% as UL 4 + . The median follow-up period was 5.35 ± 2.94 years for the CKD cohort and 6.69 ± 2.42 years for the non-CKD cohort.
Covariates and outcomes
According to Table 1, we found a significantly higher number of individuals from the CKD cohort who developed glaucoma of both subtypes (i.e., primary open-angle glaucoma [POAG] or primary closed angle glaucoma [PACG]) within the study period compared to those from the non-CKD cohort (3.28% of total cases from the CKD cohort vs. 2.28% of the total cases from the non-CKD cohort) (p < 0.0001).
Additionally, a significantly higher number of individuals from the CKD cohort received glaucoma-related medications compared to the non-CKD cohort (p < 0.0001). Moreover, a greater number of CKD patients were prescribed two categories of glaucoma medications per prescription compared to non-CKD patients (1127 CKD patients vs. 657 non-CKD patients, respectively) (refer to Table 1). Also, a higher proportion of patients in the CKD cohort using oral carbonic anhydrase inhibitors (CAI) and topical medications containing CAI (topical CAI and β-blocker plus CAI) was found compared to the non-CKD cohort (p < 0.001).
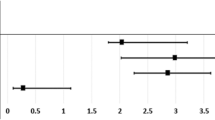
The risk of glaucoma and its subtypes among CKD compared to the non-CKD cohort were analyzed using a combined Poisson Regression model and multivariate Cox proportional hazards regression analysis (See Table 2 and Supplementary Fig. 4). The Cox model showed a significantly increased risk of glaucoma irrespective of subtypes in patients with CKD compared to those without CKD (aHR: 1.29 [CI: 1.26–1.32], p < 0.001). We also showed a significantly increased risk of PACG (aHR: 1.26 [CI: 1.20–1.33], p < 0.001) and POAG (aHR: 1.22 [CI: 1.17–1.28], p < 0.001) among those with CKD compared to those without CKD. Through the Poisson regression, using non-CKD as a reference, our findings also showed that the incident rate ratios (IRRs) for glaucoma development were significantly higher in the CKD group (IRR: 1.79 [CI: 1.76–1.83], p < 0.001) comparatively.
We also analyzed whether the risk of glaucoma was increased when associated with various covariates present among the CKD cohort compared to the non-CKD cohort using a combined Poisson Regression model and multivariate Cox proportional hazards regression analysis (refer to Table 3 and Supplementary Fig. 5). Using non-CKD as reference, we showed an elevated aHR of 1.17 [CI: 1.13–1.21] and IRR of 1.58 [CI: 1.53–1.63] among those that are female; elevated aHR of 1.39 [CI:1.35–1.43] and IRR of 1.97 [CI: 1.92–2.02] among those that are males; elevated aHR (< = 49: aHR 1.49 [CI: 1.37–1.62]; 50–59: aHR 1.48 [CI: 1.40–1.56]; 60–69: aHR 1.30 [CI: 1.25–1.6]; 70–79: aHR 1.21 [CI: 1.17–1.26]; > 80: aHR 1.29 [CI: 1.21–1.37]) and IRR (< = 49: IRR 2.58 [CI: 2.40–277]; 50–59: IRR 2.18 [CI: 2.07–2.29]; 60–69: IRR 1.61 [CI: 1.55–1.67]; 70–79: IRR 1.45 [CI: 1.40–1.50]; > 80: IRR 2.42 [CI: 2.29–2.54]) among all age groups assessed; elevated aHR (< 17,880 NT$: aHR 1.40 [1.34–1.46]; 17,880–43900 NT$: aHR 1.24 [CI: 1.20–1.28]; > 43,900 NT$: aHR 1.20 [CI: 1.14–1.26]) and elevated IRR (< 17,880 NT$: IRR 2.37 [2.29–2.46]; 17,880–43900 NT$: IRR 1.60 [CI: 1.55–1.64]; > 43,900 NT$: IRR 1.48 [CI: 1.41–1.55] in all income brackets; elevated aHR (urbanization level (UL) 1: aHR 1.28 [CI: 1.25–1.33]; UL 2: aHR 1.27 [CI: 1.23–1.32]; UL 3: aHR 1.34 [CI: 1.24–1.45]; UL 4: aHR 1.49 [CI: 1.25–1.78]) and elevated IRR (UL 1: IRR 1.76 [CI: 1.71–1.81]; UL 2: IRR 1.74 [CI: 1.69–1.80]; UL 3: IRR 1.83 [CI: 1.71–1.96]; UL 4: IRR 3.28 [CI: 2.83–3.80]) among all urbanization statuses.
Table 3 and Supplementary Fig. 5 also further demonstrated that individuals with either a history or no history of specific comorbidities of interest were all associated with an increased risk of glaucoma. Comorbidities of interest included hypertension (negative history: aHR 1.47, CI: 1.42–1.53, p < 0.001 and IRR 1.69, CI: 1.64–1.76, p < 0.001 vs. positive history: aHR 1.17, CI: 1.14–1.20, p < 0.001 and IRR 1.27, CI: 1.24–1.30, p < 0.001), diabetes (negative history: aHR 1.27, CI: 1.24–1.31, p < 0.001 and IRR:1.53, CI: 1.49–1.57, p < 0.001 vs. positive history: aHR 1.26, CI: 1.22–1.31, p < 0.001 and IRR: 1.33, CI:1.28–1.38, p < 0.001), hyperlipidemia (negative history: aHR 1.33, CI: 1.30–1.37, p < 0.001 and IRR: 1.83, CI: 1.78–1.88, p < 0.001 vs. positive history: aHR 1.17, CI: 1.14–1.21, p < 0.001 and IRR 1.27, CI: 1.23–1.31, p < 0.001), and stroke (negative history: aHR 1.31, CI: 1.28–1.34, p > 0.001 and IRR: 1.81, CI: 1.78–1.85, p < 0.001 vs. positive history: aHR 1.13, CI: 1.04–1.23, p < 0.001 and IRR 1.31, CI: 1.21–14.2, p < 0.001). Only CKD with a negative history of dementia (aHR 1.31 [CI: 1.28–1.34], p < 0.001 and IRR 1.82 [CI: 1.79–1.86], p < 0.001) showed an increased risk of glaucoma compared to its non-CKD comparators.
With non-CKD as reference, the non-dialytic CKD cohort showed an increased glaucoma risk in terms of aHR (1.22 [CI: 1.20–1.25], p < 0.001) as well as IRR (1.64 [CI: 1.61–167], p < 0.001) (refer to Supplementary Table 2). In terms of the dialytic CKD cohort who received peritoneal dialysis (PD), they showed an increased glaucoma risk in terms of aHR (1.67 [CI: 1.52–1.83], p < 0.001) compared to the non-dialytic CKD cohort and aHR (1.96 [CI: 1.78–2.16]) when compared to the non-CKD cohort. This PD group also reported an IRR of 2.52 (CI: 2.29–2.77, p < 0.001) relating to glaucoma risk compared to the non-CKD cohort. Among the dialytic CKD who received hemodialysis, they showed an aHR of 1.67 ([CI: 1.61–1.73], p < 0.001) and aHR of 1.98 ([CI: 1.91–2.06], p < 0.001) relating to glaucoma risk when compared to the non-dialytic CKD cohort and non-CKD cohort respectively. This HD group also showed an IRR of 3.12 (CI: 3.01–3.23], p < 0.001) relating to glaucoma risk compared to the non-CKD.
Kaplan Meier curves in Fig. 1 indicated an overall increased risk of glaucoma among both the non-dialytic and dialytic CKD patients when compared to the non-CKD patients (p < 0.001).
Discussion
Novel findings
We showed a significantly increased risk of developing OAG and ACG within the CKD cohort compared to the non-CKD cohort. Notably, this increased glaucoma risk persisted among both the dialytic and non-dialytic CKD cohorts. Our combined multivariate Cox proportional hazard regression and Poisson regression models further demonstrated that all genders, all age groups (< = 40, 50–59, 60–69, 70–79, > 80), and all socioeconomic brackets from the CKD cohort were associated with an increased risk for glaucoma compared to their respective non-CKD comparators. Furthermore, an increased risk of glaucoma was observed irrespective of whether CKD patients had a history of comorbidities such as hypertension, hyperlipidemia, stroke, dementia or diabetes.
Clinical implications
Our study significantly contributes to the existing literature by employing rigorous methodology, including long follow-up durations and frequency score matching, to investigate the risk of glaucoma among the CKD cohort. Ours is also one of the largest studies to investigate the association between the risk of developing primary open-angle glaucoma (POAG) and primary angle-closure glaucoma (PACG) subtypes within the chronic kidney disease (CKD) cohort in a population-based study. Using a large dataset enables researchers to elucidate better the real-world epidemiology of glaucoma and its predictive factors among CKD patients. When identifying a condition's causes, ideally one can examine relevant data directly from individual medical records. However, such a retrospective chart review is often time-consuming, limiting the number of patients able to be recruited via this method. Therefore, employing multi-institutional electronic records and utilizing electronic diagnostic codes allows researchers to identify cohorts of CKD patients with glaucoma efficiently. This study design can also be modified to recruit subgroups of the disease of interest and conduct subgroup analyses on covariates of interest. This was one of our strengths, as previous studies, such as the one by Ro et al., did not explore the risks of primary open-angle glaucoma (POAG) and primary angle-closure glaucoma (PACG) subtypes within their CKD group [5]. Furthermore, our study is among the first to analyze glaucoma's associations with dialytic and non-dialytic CKD. Understanding the comorbidities of CKD is important as the effective management of comorbidities among CKD patients has been found to affect their overall clinical outcomes [10].
However, it should be highlighted that there is currently a lack of mention regarding glaucoma-related complications among CKD patients among current guidelines. This gap underscores the need for further research to understand the associations between glaucoma and CKD better. For example, current guidelines for CKD care from the United States (US) and the United Kingdom [11] prioritize the management of complications such as diabetic-related issues [12, 13]. For example, the 2023 US guidelines recommend ophthalmologic screening only for diabetic retinopathy at the time of a type 2 diabetes diagnosis in CKD patients [14]. Therefore, our findings have implications in terms of raising awareness of glaucoma risk for at-risk CKD patients.
It is also worth noting that a higher proportion of patients in the CKD cohort received oral CAI and topical medications containing CAI (seen in both the topical CAI and the β-blocker-CAI hybrid medication) compared to the non-CKD cohort (p < 0.001). This is interesting as the use of such medications among those with impaired renal function is generally done under extreme caution, as it potentially increases the risk of metabolic acidosis and long-term dialysis [15]. Our findings may also highlight the importance of increased awareness regarding the suitability of specific medications, such as CAIs, for CKD patients.
Comparisons to literature
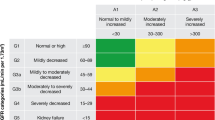
One thousand three hundred eighteen CKD patients were recruited in Ro et al. using diagnostic codes from a Korean electronic health registry [5]. Ro et al. reported an increased risk for open-angle glaucoma (OAG) among CKD patients (HR: 1.546 [CI: 1.363–1.754], p < 0.001). They also found an increased risk of OAG among both their mild cases and advanced cases of CKD, as well as an increased OAG risk among females and those 40 years and older. They also found increased OAG in rural areas (p < 0.001) and lower income (p < 0.001). Their findings complemented our own. One of the similarities between our study design and that of Ro et al. pertained to the primary outcome [5]. Both studies utilized diagnostic codes related to glaucoma and glaucoma-related medications to identify new incident glaucoma among CKD patients. One major difference was that our study utilized internationally recognized ICD diagnostic codes. Unfortunately, diagnostic codes have limitations, such as the inability to determine the eGFR levels. Additionally, we could not assess glaucoma-related ophthalmic parameters such as visual fields. Zhu et al. hinted towards the implications of such limitations. Zhu et al. was a cross-sectional study investigating the risks of major eye diseases, including glaucoma, among CKD patients. Major differences between their study and ours included its cross-sectional nature and the use of actual measurements of eGFR and ophthalmological parameters like cup-to-disc ratio to assess glaucoma risk among CKD patients [16]. Using such a study design, Zhu et al. found no significant association between CKD and glaucoma. This is a factor that future studies should explore further.
We also showed an increased risk of glaucoma among dialytic CKD patients compared to their non-CKD comparators. Interestingly, there is a lack of consensus concerning the association between glaucoma and dialysis. Lim et al. was another retrospective cohort study conducted using a similar electronic health registry. However, the primary difference between their study and ours was that Lim et al. recruited end-stage renal disease patients (ESRD) receiving dialysis and propensity-matched controls without dialysis to investigate their risk for glaucoma. In contrast, our study recruited CKD patients, which encompassed those with End-Stage Renal Disease (ESRD). Such a design by our study allows for a more comprehensive investigation into the effects of CKD on glaucoma risk. Another point to note was that Lim et al. demonstrated an increased risk of closed-angle glaucoma (ACG) among dialytic ESRD patients (HR: 1.550, 95% CI: 1.074–2.239) [17]. However, contrary to our findings, Lim et al. did not observe an increased risk of OAG among their dialysis patients. One possible reason for their results is the variation in study periods. Lim et al. recruited Taiwanese ESRD patients up to the year 2013, while our study included CKD patients up to 2017. This is an important difference as there has been a steady increase in the prevalence of myopia and high myopia over the years, linked in part to the increasing urbanization of Taiwanese society [18]. Furthermore, myopia and high myopia have been associated with an elevated risk of OAG [19].
Regarding gender, our study's aHRs and IRRs for glaucoma were higher in males than females. This contrasts with other studies [5, 17], which identified an increase in glaucoma risk primarily among females. Gender-related factors like ocular axial length may partially explain these findings [20], as axial length has been found to affect the autoregulatory function of the eye in terms of intraocular pressure.
Regarding income and urbanization, ours aligned with Ro et al., who reported an increased risk among those of lower income and in rural areas. Such findings may be due to lower-income individuals being more likely to maintain a less balanced diet, which could contribute to increased glaucoma risk [21, 22]. Additionally, individuals from higher-income brackets residing in urban areas are more likely to attain higher levels of education, potentially leading to increased eye strain in this subgroup. This, in turn, may contribute to their increased glaucoma risk [23]. Our findings emphasize the need to be aware that CKD patients, regardless of their income level, may be at an increased risk of developing glaucoma.
Another finding was the lower magnitude of aHRs and IRRs associated with the glaucoma development among CKD patients with comorbidities compared to those without such a history. This contrasts with findings from Lim et al. [17]. Given that our study is retrospective and relies on diagnostic codes, it is plausible that the clinical severity, duration and history of receiving treatment (e.g. antihypertensives and statins) for the comorbidities studied may have influenced our results obtained [24,25,26,27].
Limitations
Limitations of our study include the retrospective design and reliance on diagnostic codes that could possibly introduce misclassification bias or the inability to incorporate clinical parameters like proteinuria and eGFR levels [17]. Other unaccounted confounders include ethnicity [28], renal transplant history [29], smoking history as well as medication histories like statins and steroids [27, 29, 30]. Future prospective studies that incorporate laboratory and clinical measurements, such as cup-to-disc ratio, proteinuria, and eGFR, as well as additional subgroup analysis of other covariates like renal transplant history, smoking history, and systemic medication history, can better confirm our findings regarding the association between CKD and glaucoma.
Conclusion
This study demonstrated increased glaucoma risk within our CKD cohort compared to our frequency-matched non-CKD cohort. The implications of these findings include raising awareness among clinicians about the risk of glaucoma in CKD patients, as well as providing valuable real-world data that may influence the gradual refinement of guidelines regarding the care of CKD patients.
Availability of data and materials
The Taiwan National Health Insurance Research Database (NHIRD) is a fully deidentified database that adheres to all the relevant national privacy laws of Taiwan, including the “Personal Information Protection Act” of Taiwan. This database is managed by the NHIRD administrators, and access to it is granted to tertiary medical centres in Taiwan, including our teams. Due to privacy restrictions, data from the NHIRD database is not publicly available. However, the population-level aggregate and deidentified data supporting the findings of this study are openly accessible upon reasonable request to the NHIRD administrators through their website (https://nhird.nhri.edu.tw) or by contacting the NHIRD administrators directly (nhird@nhri.org.tw). Alternatively, the corresponding author may also be contacted (doctoraga@gmail.com).
References
Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl (2011). 2022;12(1):7–11.
Izzedine H, Bodaghi B, Launay-Vacher V, Deray G. Eye and kidney: from clinical findings to genetic explanations. J Am Soc Nephrol. 2003;14(2):516–29.
Kochumon S, Hasan A, Al-Rashed F, Sindhu S, Thomas R, Jacob T, et al. Increased Adipose Tissue Expression of IL-23 Associates with Inflammatory Markers in People with High LDL Cholesterol. Cells. 2022;11(19).
Holappa M, Vapaatalo H, Vaajanen A. Many Faces of Renin-angiotensin System - Focus on Eye. Open Ophthalmol J. 2017;11:122–42.
Ro JS, Moon JY, Park TK, Lee SH. Association between chronic kidney disease and open-angle glaucoma in South Korea: a 12-year nationwide retrospective cohort study. Sci Rep. 2022;12(1):3423.
Lin Y, Jiang B, Cai Y, Luo W, Zhu X, Lin Q, et al. The Global Burden of Glaucoma: Findings from the Global Burden of Disease 2019 Study and Predictions by Bayesian Age-Period-Cohort Analysis. J Clin Med. 2023;12(5).
Tonelli M, Wiebe N, Guthrie B, James MT, Quan H, Fortin M, et al. Comorbidity as a driver of adverse outcomes in people with chronic kidney disease. Kidney Int. 2015;88(4):859–66.
Chen Md CY, Kuo Md HT, Hsu Md AY, Lin Md CJ, Hsia Md NY, Tien Md PT, et al. Prevalence of uveitis in syphilis patients in Taiwan. Emerg Microbes Infect. 2024;13:2290836.
Anikina E, Wagner SK, Liyanage S, Sullivan P, Pavesio C, Okhravi N. The Risk of Sympathetic Ophthalmia after Vitreoretinal Surgery. Ophthalmol Retina. 2022;6(5):347–60.
Li Y, Barve K, Cockrell M, Agarwal A, Casebeer A, Dixon SW, et al. Managing comorbidities in chronic kidney disease reduces utilization and costs. BMC Health Serv Res. 2023;23(1):1418.
Angeles-Han ST, Ringold S, Beukelman T, Lovell D, Cuello CA, Becker ML, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Screening, Monitoring, and Treatment of Juvenile Idiopathic Arthritis-Associated Uveitis. Arthritis Care Res (Hoboken). 2019;71(6):703–16.
Gaitonde DY, Cook DL, Rivera IM. Chronic Kidney Disease: Detection and Evaluation. Am Fam Physician. 2017;96(12):776–83.
Forbes A, Gallagher H. Chronic kidney disease in adults: assessment and management. Clin Med (Lond). 2020;20(2):128–32.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 12. Retinopathy, neuropathy, and foot care: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S203-s215.
Wang YC, Ling XC, Tsai WH, Liu JS, Kuo KL. Risks of Topical Carbonic Anhydrase Inhibitors in Glaucoma Patients With Chronic Kidney Disease: A Nationwide Population-Based Study. Am J Ophthalmol. 2023;253:49–55.
Zhu Z, Liao H, Wang W, Scheetz J, Zhang J, He M. Visual Impairment and Major Eye Diseases in Chronic Kidney Disease: The National Health and Nutrition Examination Survey, 2005–2008. Am J Ophthalmol. 2020;213:24–33.
Lim CC, Lee CY, Huang FC, Huang JY, Hung JH, Yang SF. Risk of glaucoma in patients receiving hemodialysis and peritoneal dialysis: A nationwide population-based cohort study. Int J Environ Res Public Health. 2020;17(18):6774.
Tsai TH, Liu YL, Ma IH, Su CC, Lin CW, Lin LL, et al. Evolution of the Prevalence of Myopia among Taiwanese Schoolchildren: A Review of Survey Data from 1983 through 2017. Ophthalmology. 2021;128(2):290–301.
Chen SJ, Lu P, Zhang WF, Lu JH. High myopia as a risk factor in primary open angle glaucoma. Int J Ophthalmol. 2012;5(6):750–3.
Zhou S, Burkemper B, Pardeshi AA, Apolo G, Richter G, Jiang X, et al. Racial and Ethnic Differences in the Roles of Myopia and Ocular Biometrics as Risk Factors for Primary Open-Angle Glaucoma. Invest Ophthalmol Vis Sci. 2023;64(7):4.
Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371(9609):340–57.
Ng Yin Ling C, Lim SC, Jonas JB, Sabanayagam C. Obesity and risk of age-related eye diseases: a systematic review of prospective population-based studies. International Journal of Obesity. 2021;45(9):1863–85.
Wong TY, Foster PJ, Johnson GJ, Seah SK. Education, socioeconomic status, and ocular dimensions in Chinese adults: the Tanjong Pagar Survey. Br J Ophthalmol. 2002;86(9):963–8.
Dharmadhikari S, Lohiya K, Chelkar V, Kalyani VK, Dole K, Deshpande M, et al. Magnitude and determinants of glaucoma in type II diabetics: A hospital based cross-sectional study in Maharashtra. India Oman J Ophthalmol. 2015;8(1):19–23.
Wang S, Bao X. Hyperlipidemia, Blood Lipid Level, and the Risk of Glaucoma: A Meta-Analysis. Invest Ophthalmol Vis Sci. 2019;60(4):1028–43.
Horwitz A, Klemp M, Jeppesen J, Tsai JC, Torp-Pedersen C, Kolko M. Antihypertensive Medication Postpones the Onset of Glaucoma: Evidence From a Nationwide Study. Hypertension. 2017;69(2):202–10.
Yuan Y, Xiong R, Wu Y, Ha J, Wang W, Han X, et al. Associations of statin use with the onset and progression of open-angle glaucoma: a systematic review and meta-analysis. EClinicalMedicine. 2022;46: 101364.
Rong SS, Chen LJ, Pang CP. Myopia genetics-the Asia-pacific perspective. Asia Pac J Ophthalmol (Phila). 2016;5(4):236–44.
Moon JJ, Kim YW, Oh BL, Han K, Kim DK, Joo KW, et al. Nationwide Glaucoma incidence in end stage renal disease patients and kidney transplant recipients. Sci Rep. 2021;11(1):7418.
Pérez-de-Arcelus M, Toledo E, Martínez-González M, Martín-Calvo N, Fernández-Montero A, Moreno-Montañés J. Smoking and incidence of glaucoma: The SUN Cohort. Medicine (Baltimore). 2017;96(1): e5761.
Funding
This study is supported in part by China Medical University Hospital (DMR-111–105; DMR-112–087; DMR-113–009). We are grateful to the Health Data Science Center,
China Medical University Hospital for providing administrative, technical and funding support. The funders had no role in the study design, data collection and analysis, the decision to publish, or manuscript preparation. No additional external funding was received for this study.
Author information
Authors and Affiliations
Contributions
AYH, YCS, CJL, HSC, YYT wrote and edited the paper's main text. AYH, YCS, CJL, HSC, YYT participated in the study design and drafting of the paper. AYH, YCS, CJL, HSC, YYT designed, discussed, edited, and guided the overall process of the paper. AYH, YCS, CJL, HSC, YYT contributed to the drafting of the paper. AYH, YCS, CJL, HSC, YYT contributed to the study's design. AYH, YCS, CJL, HSC, YYT provided valuable insight and contributed to the drafting of the paper. All authors (AYH, YCS, CJL, HSC, YYT) contributed equally to the manuscript revisions. All authors (AYH, YCS, CJL, HSC, YYT) approved the final version of the manuscript and agreed to be held accountable for the content therein.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study adhered to the tenets of the Declaration of Helsinki. As the Taiwan National Health Insurance database is comprised of de-identified data, the requirement of written consent from study participants was deemed unnecessary and waived by the Ethics Research Committee. Institutional Review Board approval was also not required because de-identified data were used for this retrospective analysis.
As the Taiwan National Health Insurance database comprises of de-identified data and this study utilized such data only in a retrospective nature, written informed consent requirement was waived by the China Medical University Hospital Institutional Review Board.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hsu, A.Y., Shao, YC., Lin, CJ. et al. Evaluating the risk of new-onset glaucoma in chronic kidney disease patients: a nationwide cohort study. BMC Nephrol 25, 263 (2024). https://doi.org/10.1186/s12882-024-03698-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-024-03698-5