Abstract
Rationale & objective
Glomerulonephritis (GN) is a leading cause of chronic kidney disease (CKD). Major adverse cardiovascular events (MACE) are prolific in CKD. The risk of MACE in GN cohorts is multifactorial. We investigated the prognostic significance of routine cardiac biomarkers, Troponin I and N-terminal pro-BNP (NT-proBNP) in predicting MACE within 5 years of GN diagnosis.
Study Design
Retrospective cohort study.
Setting & participants
Data were obtained from TriNetX, a global federated health research network of electronic health records (EHR).
Exposure or predictor
Biomarker thresholds: Troponin I: 18 ng/L, NT-proBNP: 400 pg/mL.
Outcomes
Primary outcome: Incidence of major adverse cardiovascular events (MACE). Secondary outcome: was the risk for each individual component of the composite outcome.
Analytical Approach
1:1 propensity score matching using logistic regression. Cox proportional hazard models were used to assess the association of cardiac biomarkers with the primary and secondary outcomes, reported as Hazard Ratio (HR) and 95% confidence intervals (CI). Survival analysis was performed which estimates the probability of an outcome over a 5-year follow-up from the index event.
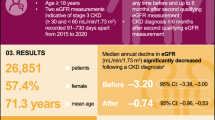
Results
Following PSM, 34,974 and 18,218 patients were analysed in the Troponin I and NTproBNP cohorts, respectively. In the Troponin I all cause GN cohort, 3,222 (9%) developed composite MACE outcome HR 1.79; (95% CI, 1.70, 1.88, p < 0.0001). In the NTproBNP GN cohort, 1,686 (9%) developed composite MACE outcome HR 1.99; (95% CI, 1.86, 2.14, p < 0.0001).
Limitations
The data are derived from EHR for administrative purposes; therefore, there is the potential for data errors or missing data.
Conclusions
In GN, routinely available cardiac biomarkers can predict incident MACE. The results suggest the clinical need for cardiovascular and mortality risk profiling in glomerular disease using a combination of clinical and laboratory variables.
Similar content being viewed by others
Introduction
Chronic Kidney disease (CKD) is a global health economic burden and contributes to premature mortality. In 2017, CKD was ranked as the 12th leading cause of death, with Cardiovascular Disease (CVD) deaths attributed to CKD representing 4·6% of total mortality [1]. CKD is a chronic systemic pro-inflammatory state contributing to vascular and myocardial remodelling, atherosclerosis, vascular calcification and complex dyslipidaemia [2, 3]. Importantly, CKD is an independent risk factor for CVD [4], with the risk of cardiovascular (CV) events more clinically significant than the development of kidney failure in those with CKD [5].
Glomerulonephritis (GN) is one of the leading causes of CKD [6]. Patients with GN have a higher absolute risk of developing CVD [7]. The risk of CVD in GN is multifactorial, including exposure to immunosuppressive medication which can increase likelihood of developing CVD [8]. Furthermore, there is emerging evidence of the pro-inflammatory consequences of GN and the development of a unique cardiovascular phenotype [9]. Following diagnosis, patients with GN may initially have a stable level of renal function alongside significant proteinuria, an independent risk factor for CVD [10].
Given the multifactorial relationship between GN and the development of CV complications, patients diagnosed with GN must be appropriately monitored for their risk of CVD. The study aimed to investigate the prognostic significance of routinely measured circulating plasma cardiac biomarkers such as Troponin I or N-terminal pro-BNP (NT-proBNP) in predicting major adverse cardiovascular events (MACE) within 5 years of diagnosis of GN in a global federated research network database (TriNetX).
Methods
Study Design
A retrospective cohort study was based on anonymised data from TriNetX, a global federated health research network that provides anonymised access to electronic health records (EHR). The TriNetX database of longitudinal data includes demographics with laboratory and mortality data derived from the EHR of large healthcare organisations (HCOs). The dataset represents the Global Collaborative Network of 113 healthcare organisations of > 140 million patients, primarily in North America and Western Europe. The diagnosis has been standardised to the International Statistical Classification of Diseases and Related Health Problems 10th Revision, Clinical Modification (ICD-10CM) [11], allowing the accurate identification of disease cohorts. More information on TriNetX can be found online (https://trinetx.com/about-trinetx/). The data used in this analysis were accessed on 10th March 2024.
Building cohorts in TriNetX
All patients with a diagnosis of a Primary GN (as coded by ICD-10CM: N00-N08 in their EHR); IgA nephropathy (IgAN); membranous nephropathy (MN); focal segmental glomerulosclerosis (FSGS); or minimal change disease (MCD) were included. A full list of ICD-10CM codes used is shown in Appendix Table 1. At the time of the search, all 113 HCOs in the Research Network had data available for all cause GN and subtypes and laboratory data for Troponin I and NTproBNP.
According to biomarker-specific thresholds, two cohorts were generated for analysis.
-
1.
Troponin I cohorts stratified as Troponin I ≥ 18 ng/L or < 18 ng/L.
-
2.
NT-proBNP cohorts stratified as ≥ 400.00 pg/mL or ˂400.00 pg/mL, respectively.
Cardiac biomarkers were the first reported result within three months of GN diagnosis. The specific thresholds reflect the National Institute of Health and Care Excellence (NICE) guideline for diagnosing heart failure (NTproBNP). Troponin I is an approximation of the 99th percentile across all clinical assay platforms [12].
Demographic data on age and gender were collected, as well as common CV risk factors by ICD-10CM codes, including hypertensive diseases (I10-I16), ischaemic heart disease (IHD) (ICD-10CM: I20-I25), heart failure (ICD-10CM: I50), diabetes mellitus (E08-E13) and smoking status (F17 nicotine dependence). Data was also collected on common cardiovascular medication; beta blockers, antilipemic agents, ace inhibitors, angiotensin II inhibitors, aspirin, clopidogrel, diuretics, finerenone, eplerenone, spironolactone. Laboratory results for estimated glomerular filtration rate (eGFR utilising Modification of Diet in Renal Disease (MDRD) formula)), proteinuria (microalbumin mg/g) and cholesterol (mg/dL) were extracted from the database. Laboratory values were the first reported within three months of GN diagnosis.
Index Event
The diagnosis of a primary GN with a cardiac biomarker measured within 3 months (NTproBNP or Troponin I) following the diagnosis was used as the index event. The index event whereby a patient meets the criteria for inclusion could be up to 20 years before the data search date.
Follow-up and clinical outcome
The primary outcome was the incidence of any MACE that occurred between 1 day after the index event and five years follow-up. MACE was defined as a composite of IHD (ICD-10CM: I20-I25), angina (ICD-10CM: I20), acute myocardial infarction (AMI) (MI ICD-10CM: I21), heart failure (ICD-10CM: I50), atrial fibrillation or flutter (ICD-10CM: I48), ischaemic stroke (ICD-10CM: I63), and all-cause mortality (death). Patients who incurred a MACE 5-years prior to the index event were excluded. The secondary outcome was the risk for each component of the composite outcome.
Statistical analysis
All statistical analyses were performed on the TriNetX online platform. All participants had been enrolled to the database between the years 2010–2024.
As a continuous variable, age was expressed as mean and standard deviation (S.D.) and tested for differences with an independent-sample t-test. The demographic and CV risk factor data were expressed as absolute frequencies and percentages and tested for differences with the chi-squared test.
Prior to analysis, cohorts were 1:1 propensity score matched (PSM) [13] for baseline demographics CV risk factors, CV medications, proteinuria and cholesterol. PSM was performed using the online TriNetX platform. The platform uses ‘greedy nearest-neighbour matching’ with a caliper of 0.1 pooled standard deviations and a difference between propensity scores ≤ 0.1. Covariate balance between groups was assessed using standardised mean differences (SMDs) and included in appendix results, SMD between cohorts < 0.1 is considered well-matched.
Following PSM, Cox proportional hazard models were used to assess the association of cardiac biomarkers with the primary and secondary outcomes at 5-year follow-ups.
Results are reported as hazard ratio HR) with 95% confidence intervals and Kaplan-Meier survival curves with log-rank tests. No imputations were made for missing data. Censoring was applied, and a patient was removed (censored) from the analysis after the last event in their electronic record. Statistical analysis was performed using the’ Analytics’ functionality on TriNetX, which used the R Survival package v3.2-3. A p-value < 0.05 was accepted as the level of statistical significance.
Exploratory analysis
We performed 3 additional exploratory analyses to understand:
-
1.
The CV risk of patients with GN beyond that attributed to traditional risk factors.
-
2.
The prognostic significance of combining NTproBNP and Troponin I in a single analysis.
-
3.
The prognostic significance of NTproBNP by excluding troponin I and vice-versa.
The first exploratory analysis aimed to study the CV risk of patients with GN beyond that attributed and acknowledged by traditional risk factors such as demographics, comorbidities, CV medication and level of renal function.
We investigated the risk of the primary and secondary outcome in the all-cause GN cohort only following 1:1 PSM, including the same variables as the main analysis with the addition of eGFR.
In the second analysis, we aimed to determine the prognostic utility of a combined biomarker approach, with NTproBNP and Troponin I stratified by their respective thresholds.
In the final analysis, we aimed to determine the prognostic significance of each biomarker (stratified by specific thresholds above) in a population where the alternate biomarker had been reduced.
Both these analyses were performed on the all-cause GN group only following 1:1 PSM including the same variables as the main analysis with the addition of renal function as detailed above. These further 2 exploratory analyses were performed to account for the potential overlap in the populations were NTproBNP and Troponin I are reported.
Data Access
The data used in this analysis were accessed on the TriNetX online research platform. To gain access to this data a request can be made to TriNetX (https://live.trinetx.com/), although costs may be incurred, and a data sharing agreement must be in place. As a federated research network, studies using TriNetX do not require research ethical approval as no patient’s identifiable information is received.
Results
Demographics
Troponin I
A total of 48,541 patients with all-cause GN were identified. Prior to propensity score matching (PSM), patients with Troponin I ≥ 18 ng/L were older, a higher proportion of males and a greater prevalence of ischaemic heart disease (IHD), heart failure (HF) and diabetes mellitus. A summary of the PSM characteristics may be found in Appendix Table 2. Following PSM, 34,974 patients were included in the analysis (mean patient age 59.4 SD 17; 48% male). 82% of the cohort patients had hypertension, 31% IHD and 24% HF. Beta-blockers and diuretics were the most common CV medication prescribed at 59%. Across the sub-group analysis, the mean age and CV risk factor profile reflected a similar pattern to all-cause GN. Following PSM, troponin I median and standard deviation (SD) was 75.5 ng/L ± 47.3 vs. 13.6 ng/L ± 1.8, both cohorts (Troponin I < 18 ng/L vs. Troponin I≥18ng/L) were well matched for age, gender and CV risk factors, with no statistically significant differences between groups. A breakdown of patient selection is shown in the study flow diagram. (Fig. 1)
NT-proBNP
In total, 34,841 patients with all-cause GN were identified. Prior to PSM, patients with NTproBNP ≥ 400 pg/ml were older, a higher proportion male and a greater prevalence of hypertension, IHD and HF. A summary of the PSM characteristics may be found in Appendix Table 3. Following PSM, 18,218 patients were included in the analysis (mean age 60 (SD 17.8); 50% male). Of the all-cause GN cohort, 31.6% had pre-existing HF, 22% IHD and 55% were diabetic. The sub-group analysis of primary GN in this cohort again had similar CV risk factor profiles to all-cause GN. Following PSM NTproBNP median SD was 1204pg/ml ± 803 vs. 183 pg/ml ± 108, both cohorts (NTproBNP < 400 pg/ml vs. NTproBNP ≥400 pg/ml) were well matched for age, gender and CV risk factors, with no statistically significant differences between groups. A breakdown of patient selection is shown in the study flow diagram. (Fig. 1)
Table 1 displays the included patient demographics following PSM and CV risk profile for all GN cohorts.
Clinical outcomes
Troponin I
Within all-cause GN cohort, 13,625 of the 34,974 patients had 5-year follow-up data available from the time of the index event. Of those, 6,222 developed the primary composite outcome. Of these 3,222 (9% of all-cause GN cohort) had a Troponin I above the 18 ng/L threshold. This equated to a HR of 1.79 (95% CI, 1.70, 1.88, p-value < 0.0001). When considering the secondary outcome, of the individual components of the primary composite outcome, an increased Troponin I was associated with a statistically significant increased risk of all-cause mortality HR 1.53 (95% CI, 1.47, 1.59); stroke HR1.27 (95% CI, 1.17, 1.38); HF HR 1.81 (95% CI, 1.71, 1.91); acute myocardial infarction (AMI) HR 1.79 (95% CI, 1.68, 1.93); angina pectoris HR 1.33 (95% CI, 1.22, 1.46) and IHD HR 1.62 (95% CI, 1.53, 1.71) (Fig. 2). Only atrial fibrillation and flutter as secondary outcomes did not reach the level of statistical significance.
An increased cardiac Troponin I above the 18ng/L threshold was associated with a statistically significant increased risk of the composite primary outcome in all GN sub-groups: IgA nephropathy (IgAN) HR1.75 (95% CI, 1.61, 1.90); membranous nephropathy (MN) HR 1.79 (95% CI, 1.64, 1.94); focal segmental glomerulosclerosis (FSGS) HR 1.71 (95% CI, 1.58, 1.87) and minimal change disease (MCD) HR 1.71 (95% CI, 1.58, 1.86). In the GN sub-groups, the most significant risk associated with an increased cardiac Troponin I was the development of heart failure over the 5 years of follow-up: IgAN HR 1.87 (95% CI, 1.66, 2.10); MN HR 1.90 (95% CI, 1.73, 2.09); FSGS HR 1.84 (95% CI, 1.67, 2.01). Conversely, the risk of AMI correlated most significantly with troponin in MCD HR 1.87 (95% CI, 1.67, 2.01) (Appendix Table 4).
NT-proBNP
Within all-cause GN cohort, 7,116 of the 18,218 patients had 5-year follow-up data available from the time of the index event. Of those, 3,023 developed the primary composite outcome. Of these 1,686 (9% of all-cause GN cohort) had a NTproBNP above the 400 pg/ml threshold. This equated to a HR of 1.99 ((95% CI, 1.86, 2.14, p-value < 0.0001). When considering the secondary outcome, of the individual components of the primary composite outcome, an increased NTproBNP was associated with a statistically significant increased risk of all-cause mortality HR 2.49 (95% CI, 2.33, 2.66); stroke HR 1.49 (95% CI, 1.23, 1.70)); atrial fibrillation and flutter HR 1.96 (95% CI, 1.76, 2.17)); heart failure HR 2.26 (95% CI, 2.08, 2.44); AMI HR 1.91 (95% CI, 1.71, 2.13); and IHD HR 1.83 (95% CI, 1.69, 1.99) (Fig. 3). Only angina pectoris as a secondary outcome did not reach the level of statistical significance.
An increased NTproBNP above the 400 pg/ml threshold was associated with a statistically significant increased risk of the composite primary outcome in all GN sub-groups: IgAN HR 1.84 (95% CI, 1.62, 2.09); MN HR 1.91 (95% CI, 1.68, 2.18); FSGS HR 1.88 (95% CI, 1.65, 2.14) and MCD HR 1.77 (95% CI, 1.56, 2.00). In the GN sub-groups, the most significant risk associated with an increased NTproBNP was HF, over the 5 years of follow-up in: IgAN HR 2.46 (95% CI, 2.11, 2.86) and MN HR 2.43 (95% CI, 2.08, 2.84). A NTproBNP ≥400 pg/ml was most significantly associated with all-cause mortality in FSGS HR 2.406 (95% CI, 2.13, 2.70) and MCD HR 2.41 (95% CI, 2.14, 2.71) (Appendix Table 5).
Kaplan - Meier survival analysis (KM) was produced excluding patients with outcome prior to the time window. This analysis highlights that MACE and its components increase the risk of mortality for GN including the sub-group analysis of primary GN (Fig. 4).
Exploratory analysis- adjusted for baseline CKD
Troponin I
In an exploratory analysis, 12,872 of the 33,822 patients had 5-year follow-up data available from the time of the index event. Of those, 5,896 developed the primary composite outcome. Of these, 3,016 (9% of all-cause GN cohort) had a Troponin I above the 18 ng/L threshold. This equated to a HR of 1.76 (95% CI, 1.67,1.86, p-value < 0.0001). When considering the secondary outcome, an increased Troponin I was statistically significant for all components of MACE all-cause mortality HR 1.48 (95% CI, 1.42, 1.54); stroke HR 1.25 (95% CI, 1.15, 1.37); heart failure HR 1.77 (95% CI, 1.67, 1.87); atrial fibrillation and flutter HR 1.44 (1.34, 1.54); AMI HR 1.76 (95% CI, 1.65, 1.89); angina pectoris HR 1.35 (95% CI, 1.23, 1.48) and IHD HR 1.56 (95% CI, 1.48, 1.65) (Fig. 5 and Appendix Table 7).
NTproBNP
In our exploratory analysis, 6,333 of the 16,730 patients had 5-year follow-up data available from the time of the index event. Of those, 2,735 developed the primary composite MACE outcome. Of these, 1,500 (9% of all cause GN cohort) had a NTproBNP above the 400 pg/ml threshold. This equated to a HR of 1.99 (95% CI, 1.85, 2.15, p-value < 0.0001). When considering the secondary outcome, an increased NTproBNP was associated with a statistically significant increased risk of all-cause mortality HR 2.41 (95% CI, 2.25, 2.57) ); stroke HR 1.45(95% CI, 1.26, 1.67) ); heart failure HR 2.32 (95% CI, 2.14, 2.52) ; AMI HR 1.90 (95% CI, 1.69, 2.13) ); and IHD HR 1.78 (95% CI, 1.63, 1.94) (Fig. 6). Only angina pectoris as a secondary outcome did not reach the level of statistical significance (Appendix Table 8).
Table 2 displays the included patient demographics following PSM CV risk profile and eGFR for all GN cohorts.
A summary of the PSM characteristics may be found in Appendix Table 6.
Exploratory analysis – combined NTproBNP and troponin I
In our exploratory analysis of all cause GN with Troponin I and NTproBNP combined, 736 of the 2,318 patients had 5-year follow-up data available from the time of the index event. Of those, 327 developed the primary composite MACE outcome. Of these, 176 (7.6% of all cause GN cohort) had Troponin I and NTproBNP above threshold. This equated to a HR of 2.79 (95% CI, 2.24, 3.48, p-value 0.002). When considering the secondary outcome, statistically significant increased risk was not demonstrated for three of the components of MACE; IHD HR 2.47 (95% CI, 1.96, 3.11,p-value 0.003), AMI HR 3.08 (95% CI, 2.30, 4.12, p-value 0.018), HF HR 2.81 (95% CI, 2.25, 3.51, p-value 0.002). Secondary outcomes that did not meet statistical significance; angina HR 1.69 (95% CI, 1.18, 2.41, p-value 0.893), AF and flutter HR 1.86 (95% CI, 1.38, 2.51, p-value 0.154)stroke HR 1.29 (95% CI, 0.91, 1.81. p-value 0.719), all-cause mortality HR 2.68 (95% CI, 2.25, 3.19, p-value 0.858).
Exploratory analysis – alternate biomarker excluded
In our exploratory analysis of all cause GN with NTproBNP excluded, 11,339 of the 27,674 patients had 5-year follow-up data available from the time of the index event. Of those, 4,958 developed the primary composite MACE outcome. Of these, 2,608 (9.4% of all cause GN cohort) had a Troponin I above the 18 ng/L threshold. This equated to a HR of 1.81 (95% CI, 1.72, 1.92, p-value < 0.0001). When considering the secondary outcome, statistically significant increased risk was demonstrated for each component of MACE; IHD HR 1.69 (95% CI, 1.59, 1.80,p-value < 0.0001), Angina HR 1.48 (95% CI, 1.32, 1.66, p-value < 0.0001), AMI HR 1.91 (95% CI, 1.76, 2.07, p-value < 0.0001), HF HR 1.94 (95% CI, 1.82, 2.07, p-value < 0.0001), AF and flutter HR 1.61 (95% CI, 1.48, 1.75, p-value 0.003), stroke HR 1.28 (95% CI, 1.16, 1.42. p-value 0.05), all-cause mortality HR 1.51 (95% CI, 1.44, 1.58, p -value < 0.0001).
In our exploratory analysis of all cause GN with Troponin I excluded, 5,250 of the 13,376 patients had 5-year follow-up data available from the time of the index event. Of those, 2,183 developed the primary composite MACE outcome. Of these, 1,244 (9.3% of all cause GN cohort) had a NTproBNP above the 400 pg/ml threshold. This equated to a HR of 1.95(95% CI, 1.79, 2.12, p < 0.0001). When considering the secondary outcome, statistically significant increased risk was demonstrated for each component of MACE apart from angina;
IHD HR 1.72 (95% CI, 1.55, 1.90,p-value < 0.0001), AMI HR 1.67 (95% CI, 1.47, 1.91, p-value 0.006), HF HR 2.27 (95% CI, 2.06, 2.50, p-value < 0.0001), AF and flutter HR 2.09 (95% CI, 1.84, 2.38, p-value < 0.0001), stroke HR 1.52 (95% CI, 1.28, 1.79. p-value 0.01), all-cause mortality HR 2.41 (95% CI, 2.23, 2.60, p-value < 0.0001), angina HR 1.36 (95% CI, 1.15, 1.61, p-value 0.7521).
Discussion
This analysis highlights that routine clinical laboratory cardiac biomarkers, frequently utilised in healthcare settings, can predict incident MACE in patients with GN. Across all GN and sub-groups of primary GN, a raised NT-proBNP and/or Troponin I produced a statistically significant correlation with incident MACE. The exploratory analyses adjusted for baseline CKD demonstrates the CV risk of patients with GN is present beyond the effects conferred by pre-existing traditional risk factors of baseline renal function, in addition to exploring the prognostic significance of a combined biomarker approach.
Multiple studies have recognised the association between circulating plasma cardiac biomarkers and risk of future CV complications in GN patients, however, at present, biomarker monitoring is not a part of standard routine practice for the GN population [14,15,16,17]. Our study confirms, in a large study population reflective of real-world clinical use, that Troponin I and NT-proBNP, readily available laboratory tests, provide valuable results that can aid the management of patients with GN.
Proteinuria is synonymous with a GN diagnosis and the correlation between proteinuria and CVD has long been established [18, 19]. For example, Lee et al. [20] conducted a retrospective study of two renal registries analysing patients with biopsy proven membranous nephropathy. One of the measured outcomes was Cardiovascular event (CVE). The study showed a dichotomous pattern of CVE; early events when significant proteinuria and later events over two years since diagnosis not associated with proteinuria. MN disease activity at the time of CVE was a significant independent risk factor HR 2.1, (95% CI, 1.1,4.3) [20]. This highlights that in GN cohorts the pathophysiology leading to CVE can be considered multifactorial; early risk associated with acute immunomodulatory changes and subsequent long-term risk from the GN triggering atherosclerotic pathways.
Ordonez et al. [21] highlighted the increased risk of coronary heart disease associated with nephrotic syndrome (NS) however, we are yet to make significant progress in quantifying and reducing this risk in our GN cohorts. Analysis of data from American electronic health records, The Kaiser Permanente NS Study [22] demonstrated the risk of MACE when comparing a cohort of primary nephrotic patients against a matched adult cohort (adults without diabetes mellitus, NS, or nephrotic range proteinuria). The primary NS cohort demonstrated over a 2.5-fold higher adjusted rate of incident AMI compared with matched controls, adjusted, 2.58 (95% CI, 1.89 to 3.52) [22].
We continue to understand better the pathogenesis of CVD in CKD and the critical role of endothelial dysfunction that may be specific to GN alongside traditional risk factors such as hypertension and dyslipidaemia [23,24,25]. Biomarkers associated with endothelial dysfunction are present in GN cohorts. Salmito et al. [25] demonstrated a correlation between syndecan-1, a biomarker of endothelial glycocalyx damage, and proteinuria in a cohort of patients with NS. A longitudinal study of patients with FSGS by Zhang et al. [26] showed that the endothelial biomarkers von Willebrand factor and soluble vascular cell adhesion molecule-1 remained elevated despite clinical remission. This study has demonstrated that Troponin I and NTproBNP, validated laboratory tests widely used in clinical practice, can predict the risk of MACE in GN.
NS is associated with dyslipidaemia, including significant hypertriglyceridemia. Persistent dyslipidaemia can exert ‘lipid nephrotoxicity’ [27], which is multifactorial and perpetuates the progression of CKD and subsequent increased risk of CVD [28]. The lipidome of NS patients shows evident dysregulated lipid metabolism, including High-density lipoprotein (HDL) dysfunction. HDL has cardioprotective, antioxidant properties that enhance endothelial function but is dysfunctional in those with CVD disease associated with CKD [3]. Although HDL levels can be measured, no demonstratable threshold can be correlated with increased risk of MACE as we have demonstrated with Troponin I and NTproBNP. There is emerging evidence that the pro-inflammatory process of dyslipidaemia associated with CVD precedes the onset of established CKD [29].
In addition, previous studies in IgAN, the commonest primary GN [30], have aimed to appreciate better and highlight the risk of MACE in this cohort. Based on registry data, Jarrick et al. [31] conducted a retrospective longitudinal analysis of IgAN patients in Sweden. Compared to age and gender-matched cohorts IgAN patients had an increased risk of developing IHD with an adjusted HR 1.86 (95% CI,1.63–2.13). Sagi et al. [32] performed echocardiography prospectively on a cohort of IgAN patients and discovered that the left ventricular mass index could be utilised to predict the risk of mortality, major CV events, and end-stage renal disease. Utilising echocardiography to risk stratify patients requires much more infrastructure and cost compared to routine clinical laboratory measures circulating plasma biomarkers, such as Troponin I and NTproBNP.
The mainstay of treatment for GN is to achieve disease remission using immunosuppressing medication. Patients are frequently exposed to similar levels of immune-modulating medication as transplant patients. Results show that these drugs in themselves can contribute to the development of CV complications [33, 34]. Calcineurin inhibitors (CNI) are common kidney transplant immunosuppression but are also prescribed for GN treatment. CNI has been associated with hypertension in transplant recipients through endothelial dysfunction and oxidative stress; new onset diabetes post-transplantation is also associated with CNI [35,36,37]. Furthermore, glucocorticoids remain an inherent feature in treatment protocols for GN. Due to the relapsing nature of many GN diagnoses the steroid exposure of a patient can be very significant. Glucocorticoids are associated with hyperglycaemia, hypertension and dyslipidaemia, all well-established risk factors for CVD [38,39,40].
A study by Hutton et al. [41] based on a prospective Canadian cohort of 2544 patients aimed to examine the hypothesis that the risk of CVD over 3 years in CKD patients with GN is higher than in those with non-GN causes of CKD. The results showed that patients with GN-CKD have a high 8.7% absolute 3-year risk of CVD. However, when the PSM with prior CV risk factors and level of kidney function, the Hazard ratio was 1.0141.The first exploratory analysis, reported here, for MACE events adjusted for baseline CKD disproves this theory.
Given the prevalence of GN and CKD and its direct correlation with MACE outcomes, we must identify those individuals at most risk of MACE to address their modifiable risk factors. By virtue of a diagnosis of GN, patients will require frequent monitoring of blood tests. A method can be developed by testing readily available cardiac biomarkers to calculate CV mortality and risk profiling in patients with glomerular disease using a combination of clinical and laboratory variables.
Strengths and limitations
This study reports a large retrospective cohort of the prognostic significance of routinely measured cardiac biomarkers. The study is based on a large multi-million patient database from participating healthcare organisations. As such the study is reflective of clinical practice. The biomarkers evaluated are already used in clinical practice and can be measured easily in hospital diagnostic laboratories.
While real-world data reflects clinical practice, the retrospective study means the cohorts are not randomised or controlled. However, using a quasi-experimental approach with PSM replicates a randomised control trial within observational data, somewhat mitigating the risk [42]. External validity of the results is limited to the database being studied, this study primarily includes primarily includes participants from North America and Western Europe. The data are derived from electronic health records for administrative purposes; therefore, there is the potential for data errors or missing data. Patients/data may also be lost to follow-up if a patient moves healthcare organisation which could potentially skew covariate distribution and outcomes.
PSM balanced cohorts for age, gender, and CV risk factors. However, omitting socio-economic data such as deprivation indices and family history could bias the results.
Conclusion
Routinely available cardiac biomarkers can predict incident MACE in patients with GN. The results suggest the clinical need for CV mortality and morbidity risk profiling in patients with glomerular disease using a combination of clinical and laboratory variables.
Patient number for pre and post Propensity score matching (PSM) number for Troponin I and NTproBNP all cause GN cohorts. Figure showing the number of patients before and after PSM was applied for all cause GN cohort. Troponin I and NTproBNP cohorts have been separated into their biomarker thresholds for analysis
Data availability
All data supporting the results reported in the article can be found within the manuscript and the appendix.
References
Global. Regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2020;395(10225):709–33.
Jankowski J, Floege J, Fliser D, Böhm M, Marx N. Cardiovascular Disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation. 2021;143(11):1157–72.
Vaziri ND. Dyslipidemia of chronic renal failure: the nature, mechanisms, and potential consequences. Am J Physiol Ren Physiol. 2006;290(2):F262–272.
Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on kidney in cardiovascular disease, high blood pressure research, clinical cardiology, and epidemiology and prevention. Circulation. 2003;108(17):2154–69.
Levey AS, Eckardt KU, Tsukamoto Y, et al. Definition and classification of chronic kidney disease: a position statement from kidney disease: improving global outcomes (KDIGO). Kidney Int. 2005;67(6):2089–100.
Registry UR, UK Renal Registry. (2022) UK renal registry 24th annual report – data to 31/12/2020. Vol 20232022.
Canney M, Gunning HM, Zheng Y, et al. The risk of cardiovascular events in individuals with primary glomerular diseases. Am J Kidney Dis. 2022;80(6):740–50.
Miller LW. Cardiovascular toxicities of immunosuppressive agents. Am J Transpl. 2002;2(9):807–18.
Ferro CJ, Mark PB, Kanbay M, et al. Lipid management in patients with chronic kidney disease. Nat Rev Nephrol. 2018;14(12):727–49.
Klausen K, Borch-Johnsen K, Feldt-Rasmussen B, et al. Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension, and diabetes. Circulation. 2004;110(1):32–5.
World Health O. ICD-10: international statistical classification of diseases and related health problems : tenth revision. 2nd ed. Geneva: World Health Organization; 2004.
Medicine TIFoCCaL. High-Sensitivity* Cardiac Troponin I and T Assay Analytical Characteristics Designated by Manufacturer. IFCC Committee on Clinical Applications of Cardiac Bio-Markers (C-CB) v052022. Available online https://ifcc.web.insd.dk/media/479435/high-sensitivity-cardiac-troponin-i-and-t-assay-analytical-characteristics-designated-by-manufacturer-v052022.pdf.
Guo S, Fraser MW. Propensity score analysis: statistical methods and applications; 2014.
Bansal N, Zelnick L, Go A, et al. Cardiac biomarkers and risk of Incident Heart failure in chronic kidney disease: the CRIC (chronic renal insufficiency cohort) study. J Am Heart Assoc. 2019;8(21):e012336.
Savoj J, Becerra B, Kim JK, et al. Utility of cardiac biomarkers in the setting of kidney disease. Nephron. 2019;141(4):227–35.
Scheven L, de Jong PE, Hillege HL, et al. High-sensitive troponin T and N-terminal pro-B type natriuretic peptide are associated with cardiovascular events despite the cross-sectional association with albuminuria and glomerular filtration rate. Eur Heart J. 2012;33(18):2272–81.
Provenzano M, Andreucci M, De Nicola L, et al. The role of prognostic and predictive biomarkers for assessing Cardiovascular risk in chronic kidney Disease patients. Biomed Res Int. 2020;2020:2314128.
Stehouwer CDA, Smulders YM. Microalbuminuria and risk for cardiovascular disease: analysis of potential mechanisms. J Am Soc Nephrol. 2006;17(8):2106–11.
Weinstock Brown W, Keane WF. Proteinuria and cardiovascular disease. Am J Kidney Dis. 2001;38(4 Suppl 1):S8–13.
Lee T, Derebail VK, Kshirsagar AV, et al. Patients with primary membranous nephropathy are at high risk of cardiovascular events. Kidney Int. 2016;89(5):1111–8.
Ordoñez JD, Hiatt RA, Killebrew EJ, Fireman BH. The increased risk of coronary heart disease associated with nephrotic syndrome. Kidney Int. 1993;44(3):638–42.
Go AS, Tan TC, Chertow GM, et al. Primary nephrotic syndrome and risks of ESKD, Cardiovascular events, and death: the kaiser permanente nephrotic syndrome study. J Am Soc Nephrol. 2021;32(9):2303–14.
Mackinnon B, Deighan CJ, Norrie J, Boulton-Jones JM, Sattar N, Fox JG. The link between circulating markers of endothelial function and proteinuria in patients with primary glomerulonephritis. Clin Nephrol. 2005;63(3):173–80.
Salmon AH, Satchell SC. Endothelial glycocalyx dysfunction in disease: albuminuria and increased microvascular permeability. J Pathol. 2012;226(4):562–74.
Salmito FT, de Oliveira Neves FM, Meneses GC, de Almeida Leitão R, Martins AM, Libório AB. Glycocalyx injury in adults with nephrotic syndrome: association with endothelial function. Clin Chim Acta. 2015;447:55–8.
Zhang Q, Zeng C, Fu Y, Cheng Z, Zhang J, Liu Z. Biomarkers of endothelial dysfunction in patients with primary focal segmental glomerulosclerosis. Nephrol (Carlton). 2012;17(4):338–45.
Moorhead JF, Chan MK, El-Nahas M, Varghese Z. Lipid nephrotoxicity in chronic progressive glomerular and tubulo-interstitial disease. Lancet. 1982;2(8311):1309–11.
Agrawal S, Zaritsky JJ, Fornoni A, Smoyer WE. Dyslipidaemia in nephrotic syndrome: mechanisms and treatment. Nat Rev Nephrol. 2018;14(1):57–70.
Zeng W, Beyene HB, Kuokkanen M, et al. Lipidomic profiling in the strong heart study identified American indians at risk of chronic kidney disease. Kidney Int. 2022;102(5):1154–66.
Schena FP, Nistor I. Epidemiology of IgA nephropathy: a global perspective. Semin Nephrol. 2018;38(5):435–42.
Jarrick S, Lundberg S, Sundström J, Symreng A, Warnqvist A, Ludvigsson JF. Immunoglobulin a nephropathy and ischemic heart disease: a nationwide population-based cohort study. BMC Nephrol. 2021;22(1):165.
Sági B, Késői I, Vas T, Csiky B, Nagy J, Kovács TJ. Left ventricular myocardial mass index associated with cardiovascular and renal prognosis in IgA nephropathy. BMC Nephrol. 2022;23(1):285.
Birdwell KA, Park M. Post-transplant cardiovascular disease. Clin J Am Soc Nephrol. 2021;16(12):1878–89.
Jardine AG, Gaston RS, Fellstrom BC, Holdaas H. Prevention of cardiovascular disease in adult recipients of kidney transplants. Lancet. 2011;378(9800):1419–27.
Jardine AG. Assessing the relative risk of cardiovascular disease among renal transplant patients receiving tacrolimus or cyclosporine. Transpl Int. 2005;18(4):379–84.
Calò LA, Davis PA, Giacon B, et al. Oxidative stress in kidney transplant patients with calcineurin inhibitor-induced hypertension: effect of ramipril. J Cardiovasc Pharmacol. 2002;40(4):625–31.
Heisel O, Heisel R, Balshaw R, Keown P. New onset diabetes mellitus in patients receiving calcineurin inhibitors: a systematic review and meta-analysis. Am J Transpl. 2004;4(4):583–95.
Ng MK, Celermajer DS. Glucocorticoid treatment and cardiovascular disease. Heart. 2004;90(8):829–30.
Walker BR. Glucocorticoids and cardiovascular disease. Eur J Endocrinol. 2007;157(5):545–59.
Lim CC, Choo JCJ, Tan HZ, et al. Changes in metabolic parameters and adverse kidney and cardiovascular events during glomerulonephritis and renal vasculitis treatment in patients with and without diabetes mellitus. Kidney Res Clin Pract. 2021;40(2):250–62.
Hutton HL, Levin A, Gill J, Djurdjev O, Tang M, Barbour SJ. Cardiovascular risk is similar in patients with glomerulonephritis compared to other types of chronic kidney disease: a matched cohort study. BMC Nephrol. 2017;18(1):95.
Stuart BL, Grebel LE, Butler CC, Hood K, Verheij TJM, Little P. Comparison between treatment effects in a randomised controlled trial and an observational study using propensity scores in primary care. Br J Gen Pract. 2017;67(662):e643–9.
Acknowledgements
Not applicable.
Funding
This work was supported by the Wellcome Trust [219574/Z/19/Z]; and the Faculty of Health and Life Sciences, University of Liverpool.
Author information
Authors and Affiliations
Contributions
ED: leading contributor to manuscript and data interpretation. PA: Guidance on using TrinetX and data outputs. BB, GL, LO: contributed to conception and design of work. GM, AR: conception and design of work, interpretation of data and manuscript editingAll authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
As a federated research network, studies using TriNetX do not require research ethical approval as no patient’s identifiable information is received.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Davies, E.M., Buckley, B.J.R., Austin, P. et al. Routine cardiac biomarkers for the prediction of incident major adverse cardiac events in patients with glomerulonephritis: a real-world analysis using a global federated database. BMC Nephrol 25, 233 (2024). https://doi.org/10.1186/s12882-024-03667-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-024-03667-y