Abstract
Background
Cerebral small vessel disease can be identified using magnetic resonance imaging, and includes white matter hyperintensities, lacunar infarcts, cerebral microbleeds, and brain atrophy. Cerebral small vessel disease and chronic kidney disease share many risk factors, including hypertension. This study aims to explore an association between chronic kidney disease and cerebral small vessel disease, and also to explore the role of hypertension in this relationship.
Methods
With a cross sectional study design, data from 390 older adults was retrieved from the general population study Good Aging in Skåne. Chronic kidney disease was defined as glomerular filtration rate < 60 ml/min/1,73m2. Associations between chronic kidney disease and magnetic resonance imaging markers of cerebral small vessel disease were explored using logistic regression models adjusted for age and sex. In a secondary analysis, the same calculations were performed with the study sample stratified based on hypertension status.
Results
In the whole group, adjusted for age and sex, chronic kidney disease was not associated with any markers of cerebral small vessel disease. After stratification by hypertension status and adjusted for age and sex, we observed that chronic kidney disease was associated with cerebral microbleeds (OR 1.93, CI 1.04–3.59, p-value 0.037), as well as with cortical atrophy (OR 2.45, CI 1.34–4.48, p-value 0.004) only in the hypertensive group. In the non-hypertensive group, no associations were observed.
Conclusions
In this exploratory cross-sectional study, we observed that chronic kidney disease was associated with markers of cerebral small vessel disease only in the hypertensive subgroup of a general population of older adults. This might indicate that hypertension is an important link between chronic kidney disease and cerebral small vessel disease. Further studies investigating the relationship between CKD, CSVD, and hypertension are warranted.
Similar content being viewed by others
Background
Cerebral small vessel disease (CSVD) includes pathologies of the small vessels in the brain, including small arteries, arterioles, venules, and capillaries. These pathologies are diagnosed and identified on magnetic resonance imaging (MRI) as white matter hyperintensities (WMHs), lacunar infarcts, cerebral microbleeds (CMBs), brain atrophy, recent small subcortical infarcts, and perivascular spaces. CSVD is an important cause of cognitive decline, dementia, stroke, and functional impairment [1, 2]. Although the prevalence of CSVD varies between studies, it increases with age and is very common in the older population [3, 4]. For example, the prevalence of CMBs has been estimated to increase from 7% in people 45–50 years to 36% in people ≥ 80 years [5]. The prevalence of lacunar infarcts has been estimated to increase from 22% at age 75 years to 32% at age 80 years [6].
Chronic kidney disease (CKD) is related to age, and it is– like CSVD– also prevalent in the older population [7]. Previously, we and others have shown an association between CKD and cognitive impairment [8, 9]. In our previous work, we found a longitudinal association between CKD and the development of impairment in processing speed [10]. Processing speed and executive function seem to be more affected by CSVD, compared to other cognitive domains [11, 12]. The kidney and the brain share similar low vascular resistance mechanisms, presumably making both organs sensible to hypertension [13, 14]. CKD is related to other vascular diseases, such as myocardial infarction and intermittent claudication [15, 16]. These findings suggest that an association between CKD and CSVD is possible.
Studies investigating the relationship between CKD and CSVD have found mixed results. In a pooled meta-analysis published in 2023 (n = 57 030), Xiao et al. [17] found CKD (eGFR < 60 ml/min/1,73m2) to be associated with WMHs (CI 1.05–1.86), lacunar infarcts (CI 1.18–1.92), and CMBs (CI 1.26–1.90), but not with perivascular spaces (CI 0.77–1.88). Similar results were noted in another pooled meta-analysis (n = 10 534) [18], where low eGFR was associated with WMHs, lacunar infarcts, CMBs, and silent cerebral infarction. Interestingly, in another meta-analysis (n = 20 379), Makin et al. [19] found lacunar infarcts not to be associated with CKD (defined as eGFR < 60 ml/min/1,73m2 or presence of albuminuria). In summary, CKD was associated with WMHs and CMBs in two large meta-analyses. One large meta-analysis found an association between CKD and lacunar infarcts, while another did not. There are relatively few studies that have investigated the relationship between CKD and brain atrophy. Vogels et al. [20] identified 3 studies investigating an association between eGFR and brain atrophy, in which all studies found such an association. Since previous studies investigating a relationship between CKD and markers of CSVD have found conflicting results, and studies investigating the relationship between CKD and brain atrophy are lacking, further studies investigating the relationship between CKD and CSVD are indicated.
CKD and CSVD share many of the same risk factors, including hypertension [13]. The prevalence of hypertension has been estimated to be as high as 65% in individuals ≥ 60 years of age [21]. This probably makes hypertension the most common treatable risk factor of both CKD and CSVD, and therefore the most important. The aims of this study were to explore an association between CKD and CSVD, as well as the role of hypertension in this possible association.
Methods
Study population
All data used in this cross-sectionally designed study was collected from the ongoing population-based cohort study “Good Aging in Skåne” (GÅS), conducted at the Department of Geriatric Medicine, Skåne University Hospital in Malmö, Sweden [22]. GÅS is part of the “Swedish National study on Aging and Care” (SNAC) [23]. In GÅS, participants ≥ 60 years of age have randomly been recruited from the population register since 2001. Participants represent the general, older population from the south part of Sweden. Participants in the GÅS study are invited to be examined every 3–6 years, depending on age, until death. The survey includes physical and medical examination, medical history, interview, anthropometrics, neuropsychological testing, blood sampling, and self-reported questionnaires. New participants have been recruited continuously to the GÅS study, following the same procedure as described above. A more thorough description of GÅS has been presented elsewhere [22].
A subgroup of 407 participants underwent MRI examination between March 2016 to March 2018. Out of these, 17 had missing blood samples, leaving 390 participants in this study.
Kidney function
Participants are invited for re-examinations in a nonfasted state every 3–6 years. Cryopreserved blood samples were collected from the nearest examination prior to the MRI examination (mean 738 (SD 366) days. Cystatin C (cysC) and creatinine (crea) were later analyzed at the Skåne University Hospital laboratory in Malmö. CysC was analyzed using Gentians reagent with a Beckman Coulter LX20 [24], crea was analyzed using a modified Jaffe method with a Beckman Coulter LX20 traceable to isotope-dilution mass spectrometry (IDMS).
CKD is often defined as estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73m2 [25] based on the well-established and reliable chronic kidney disease epidemiology collaboration (CKD-EPI) formula, in which consideration is taken for age and sex [26]. Calculations can be made based on crea, cysC or both (crea/cysC). In this study, mean eGFR from crea/cysC was used to assess eGFR in non-underweight participants [27]. Having a body mass index (BMI) < 23 was defined as being underweight [28]. To minimize bias, the same formula was used to calculate eGFR based only on cysC in underweight participants [29]. CKD was defined as having an eGFR of < 60 ml/min/1.73m2. Normal kidney function was defined as having an eGFR ≥ 60 ml/min/1.73m2.
Neuroradiology
MRI was performed in the Radiology Department at Skåne University Hospital in Malmö, using a 3 Tesla MRI (General Electric discovery MR 750w). The MRI examination included axial diffusion-weighted images (DWI), axial T2-weighted fluid-attenuated inversion recovery (T2 FLAIR), and axial susceptibility-weighted angiography (SWAN). An experienced neuroradiologist examined all 407 MRI examinations systematically, blinded for clinical information. The MRI examination has been described in more detail elsewhere [30].
FLAIR sequences were used to assess WMHs. The Fazekas scale [31] was used to grade the presence of WMHs, where a score of ≥ 2 was considered pathological and representative of pathological presence of WMHs.
Lacunar infarcts were defined as having ≥ 1 ischemic infarction (< 1.0 cm) in the deep white matter, the basal ganglia or pons [32].
CMBs were defined as having ≥ 1 small (0,2 − 0,5 cm) hypointense lesion [32], using the SWAN sequence.
Cortical atrophy was defined as presence of at least one of the following entities: Global cortical atrophy (GCA) ≥ 1 according to the Pasquier scale [33], Koedam score ≥ 1 [34], and/or presence of frontal/frontotemporal/temporal atrophy (visually assessed by an experienced neuroradiologist).
The composite CSVD variable was constituted of a modified version of the cerebral small vessel disease (SVD) score, presented by Staals et al. in 2014 [35]. Presence of CSVD according to the composite CSVD variable was defined as presence of at least one of the following: Fazekas scale ≥ 2, ≥ 1 lacunar infarct, and/or ≥ 1 CMB.
The modified STRIVE variable was constituted of a modified version of the Standards for reporting vascular changes on neuroimaging (STRIVE), presented by Wardlaw et al. in 2013 [36]. Presence of CSVD according to the modified STRIVE variable was defined as presence of at least one of the following: Fazekas scale ≥ 2, ≥ 1 lacunar infarct, ≥ 1 CMB, cortical atrophy, and/or central atrophy. Presence of central atrophy was visually assessed by an experienced neuroradiologist.
Hypertension
A history of hypertension was assessed by a physician from medical history and medical record for an ICD-10 diagnosis of primary or secondary hypertension. Current use of antihypertensive treatment was documented using Anatomical Therapeutic Chemical (ATC) codes (antihypertensive agents ATC02, diuretics TC03, beta-blockers ATC07, calcium antagonists ATC08, and renin-angiotensin-system inhibitors ATC09). Medical records were also reviewed in retrospect for an ICD-10 diagnosis of primary or secondary hypertension diagnosed any time before the MRI examination.
Statistics
Binary logistic regression models were used to explore associations between CKD (eGFR < 60 ml/min/1.73 m2) and the presence of WMHs, lacunar infarcts, CMBs, cortical atrophy, composite CSVD, and modified STRIVE.
First, we estimated the logistic models without covariates. Kidney function and CSVD are affected by age and sex. Therefore, to minimize confounding, we also estimated the logistic models including these covariates.
In a secondary analysis the sample was stratified by hypertension status. Binary logistic models were used to explore associations between CKD and the presence of WMHs, lacunar infarcts, CMBs, cortical atrophy, composite CSVD, and modified STRIVE. Due to limited sample size, adjustments to mitigate confounding were made including only age and sex in the statistical models. The results are presented in Table 1.
All statistical analyses were performed using the software IBM SPSS version 27. The statistical significance level was set at 5%.
Results
A description of the characteristics of the study sample stratified based on kidney function is presented in Table 2. In Table 3, the study sample was stratified by hypertension status.
Compared to participants with normal kidney function (eGFR ≥ 60 ml/min/1.73m2), participants with CKD (eGFR < 60 ml/min/1.73m2) more often had WMHs (39.4% vs. 28.0%), lacunar infarcts (10.6% vs. 7.4%), CMBs (36.2% vs. 24.7%), and cortical atrophy (59.6% vs. 47.6%). The criteria for CSVD according to the composite CSVD variable and the modified STRIVE variable, were also more often met in the group with CKD compared to the group with normal kidney function (61.7% vs. 47.3% and 85.1% vs. 77.4%, respectively). This is presented in Table 2.
The results from both the unadjusted and adjusted models are presented in Table 4. Unadjusted, we observed that CKD was associated with WMHs, CMBs and cortical atrophy, as well as with the composite CSVD variable. However, after adjusting the statistical models for age and sex, none of the associations between CKD and CSVD remained significant.
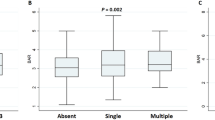
Results of the stratified analyses are shown in Table 1. No association was observed between CKD and CSVD in the non-hypertensive group. In the hypertensive group, adjusted for age and sex, we observed that CKD was associated with CMBs (OR 1.93, CI 1.04–3.59, p-value 0.037), as well as with cortical atrophy (OR 2.45, CI 1.34–4.48, p-value 0.004).
Discussion
We have explored the association between CKD and CSVD in a general population cohort of older adults. All markers of CSVD were more prevalent in the CKD group compared to those with normal kidney function. We observed that CKD was associated with CMBs and cortical atrophy in the hypertensive group. No statistically significant associations were observed in the non-hypertensive group.
Results in previous studies
Previous studies have reported mixed findings regarding an association between CKD and CMBs, though recent pooled meta-analyses support such a connection [17, 18]. Kim et al. [37] found that the level of eGFR impairment was associated to the burden of CMBs, which also is supported by other studies (Shima et al. [38], Van Overbeek et al. [39]). In contrary to our findings, Kim, Shima and van Overbeek all found the link between eGFR and CMBs to be independent of hypertension. In regard to this seemingly inconsistency, a few differences between these studies can be highlighted. Kim et al. used the modification of diet in renal disease (MDRD) formula to estimate eGFR. MDRD is associated with less accuracy compared to the CKD-EPI formula [40], increasing the risk of misclassification of subjects based on kidney function in this study. The participants in the study performed by Shima et al. had more advanced CKD compared to the participants in this study, which represents a relatively healthy older population. The study by Van Overbeek et al. had a longitudinal setting, investigating CKD and progression of CMBs over time.
Not all studies have found an association between CKD and CMBs. Akoudad et al. [41] found no association between eGFR and CMBs. A possible explanation to this could be that lobar CMBs were overrepresented in their material. Lobar CMBs have a stronger association to cerebral amyloid angiopathy than to arteriosclerosis. Neither did Sedaghat et al. [42] find any association between decline in eGFR and incident CMBs over time, with or without adjustments made for hypertension in their regression models. In another recent longitudinal study, Jiménez-Balado et al. [43] also found no association between decline in eGFR and incident CMBs. Even though the estimation of GFR in these two latter studies were measured from creatinine alone, increasing the risk of overestimation of eGFR, the mean eGFR of the participants in both these studies were high, almost 80 ml/min/1.73m2, representing relatively healthy populations. It is possible that the follow-up time of 5 and 4 years, respectively, in these two studies was too short to find any associations between decline in eGFR and incident CMBs.
Compared to CKD and CMBs, less is known regarding the connection between CKD and brain atrophy. Similar to our findings, Yakushiji et al. [44] found CKD (eGFR < 60 ml/min/1.73m2) to be associated with cerebral atrophy. Chang et al. [45] found mild CKD (defined as eGFR < 90 ml/min/1.73m2) to be associated with reduced gray matter volume and cortical thickness in a group of older participants. In contrast to our findings, the connection between CKD and brain atrophy found by both Yakushiji and Chang were independent of hypertension. In another study by Ikram et al. [46], no association between eGFR and cerebral atrophy was found. In all these studies comparing CKD to cerebral atrophy, eGFR was based on creatinine alone, which risks overestimating GFR and making the results more difficult to interpret.
The role of hypertension
In this study, we observed that CKD was associated with CMBs and cortical atrophy in the hypertensive group. In the non-hypertensive group, no association between CKD and CSVD was observed.
Both the brain and the kidneys are high energy consuming organs, dependent on a high, continuous, and stable blood flow. The vascular resistance in the kidney and the brain are low compared to other organs, resulting in a greater exposure of their vascular beds to pulsatile pressure. This presumably make both the kidney and the brain sensitive to hypertension [13, 14]. Hypertension is strongly related to damage in the microvasculature of the kidneys (hypertensive nephrosclerosis), one of the most common pathways leading to end stage renal disease [25]. Whether CKD is a cause of hypertension or vice versa is not clear and has long been a matter of debate. The matter is not resolved, but there is recent evidence that gives support to the latter claim [47].
Hypertension is also strongly related to CSVD [1], including both CMBs [30] and brain atrophy [48]. A recent longitudinal trial from the Framingham Heart Study, showed that hypertension in mid to late life preceded development of CMBs later in life [49]. Another recent longitudinal study found that diastolic hypertension preceded progression in CVSD [50]. Zhang et al. [51] found an association between reduction in white matter blood flow and WMHs, and hypertension has been associated with reduction in global and regional cerebral blood flow [52]. These arguments indicate that hypertension most likely contributes to the development of CSVD.
Hypertension is heavily associated with arterial stiffness [53]. Arterial stiffness is also associated with CSVD [54, 55], as well as with CKD [56]. Arterial stiffness is associated with elevated pulse wave velocity and elevated pulsatile pressure [53]. The vascular beds of the kidney and the brain are, as mentioned above, proposed as particularly vulnerable to increased pulsatile pressure. Hypertension is also associated with endothelial dysfunction (ED) [57]. ED is related to CKD [58], as well as to CSVD [59]. An association between CKD and markers of CSVD was observed only in the hypertensive group in this study. A hypothesis regarding the pathophysiology behind this association is that hypertension-related damage to the microvasculature of the kidney and the brain is responsible. This hypertension-related damage could depend on elevated pulsatile pressure, or hypertension-related ED, or both.
Hence, an explanation to the associations between CKD and markers of CSVD observed only in the hypertensive group in this study, could be hypertension-related damage to the small vessels in both the kidney and the brain, resulting in impairment in eGFR, as well as CSVD.
Renal contribution to development of CSVD
Hypertension is related to reduction in function of the blood-brain barrier [60]. A possible implication of renal dysfunction on CSVD in hypertensive subjects could be that a history of hypertension, with a following reduction in the blood-brain barrier function, leaves the brain more susceptible to damage from fluid and electrolyte imbalances linked to CKD [61].
The results in a recent longitudinal mouse study by Lau et al. [62] rises yet another theory. Lau et al. showed that CKD leads to disruption of the blood-brain barrier independently of hypertension. Since CKD was related to CMBs and cortical atrophy only in the hypertensive group in this study, it is possible that the combination of CKD and hypertension, both capable of damaging the blood-brain barrier, resulted in brain damage, but that CKD alone in this relatively healthy population, did not.
Finally, CKD has been associated with arterial stiffness independently of hypertension [56], and to ED independently of blood pressure [63]. Hypothetically, this could imply that CKD is indirectly involved in the development of hypertension and the development of CSVD, through the development of arterial stiffness and/or ED.
Definition of CKD
GFR has in most previous studies been estimated using the CKD-EPI formula. The most common proteins used to estimate GFR in the CKD-EPI formula are crea and cysC. The use of crea, cysC or a combination of crea/cysC in the formula varies among studies, although the use of crea alone seems to be most common. The use of crea for estimating GFR can be problematic since crea is directly related to muscle mass. In the older population, where loss of muscle mass and sarcopenia is common, crea often overestimates GFR [29]. In a recent large review (n = 23 667), Zou et al. found that the use of CKD-EPI based on cysC to estimate GFR was associated with less bias compared to the use of crea or crea/cysC, while the use of crea/cysC provided the highest accuracy [64]. A previous study of the GÅS cohort has found a significant amount of variation between eGFR based on cysC compared to crea using the CKD-EPI-formula (≥ 10% variation was found in 65%, and > 30% variation was found in 19% of the participants) [65]. Low body weight is associated with low muscle mass in older people [66]. In the older population underweight is commonly defined as BMI < 23 [28]. Since using crea/cysC to estimate GFR provided the highest accuracy in the review of Zou et al., eGFR was based on crea/cysC in the non-underweight participants. To minimize bias and overestimation of GFR in underweight participants, eGFR was based on cysC alone in participants with BMI < 23.
In this study, GFR was estimated from cysC alone in underweight participants. There are studies that have found cysC to be a risk factor of CSVD independent of eGFR based on creatinine [17], which theoretically could bias eGFR based on cysC in the underweight of this study. The cause of the association between cysC and CSVD independent of eGFR based on creatinine is not fully understood. CSVD-related release of microvesicles containing cysC has been proposed [67]. Grubb et al. introduced the term shrunken pore syndrome (SPS) in 2015 [68]. In SPS, small molecules such as crea, are assumed to be more easily excreted in the glomeruli of the kidneys compared to larger molecules, such as cysC. SPS is associated with elevated proteins associated with atherosclerosis [69]. To truly determine cysC as a risk factor of CSVD independent of GFR, GFR should not be estimated indirectly through measurement of endogenous substances, but directly by assessing GFR based on excretion of exogenous substances, such as iohexol. To the knowledge of the authors, this has not yet been performed.
A sensitivity analysis was made where all statistical models were re-run with GFR estimated using the CKD-EPI formula based on crea/cysC in all 390 participants (results not shown). When eGFR was based on crea/cysC in all participants, the number of subjects with CKD status decreased from 94 to 87. All estimates and CI:s in the statistical models remained similar. With the statistical significance level set at 5%, all previous associations remained, except for an association that was lost between CKD and CMBs in the hypertensive group adjusted for age and sex (p-value 0.063). It is likely that an association was harder to observe due to the smaller CKD group and dilution of the group with normal kidney function by subjects that, in reality, had CKD.
Definition of CSVD
WMHs, lacunar infarcts, CMBs, and brain atrophy are commonly regarded as components of CSVD [1, 36]. WMHs, lacunar infarcts, and CMBs are focal lesions, and their definitions do not vary significantly between studies. Brain atrophy can be global or focal, and especially global atrophy represents the outcome of a more diffuse process. The definition of brain atrophy varies extensively, making comparisons between studies more difficult. Brain atrophy can be measured using different visual scales, as the Pasquier scale or the Koedam score. Brain atrophy can also be assessed using automatic brain tissue segmentation (for example of gray matter or of white matter) [70]. In addition, the pathophysiological geneses behind brain atrophy are diverse, and different pathological processes in the central nervous system can lead to brain atrophy. Common pathologies leading to brain atrophy are CSVD and Alzheimer´s disease. Alzheimer´s disease typically leads to atrophy of the medial temporal lobe and/or the parietal lobe. The localizations of brain atrophy as part of CSVD is less studied, but seem to include global cerebral atrophy [71]. Examples of other pathologies that can lead to brain atrophy are excessive alcohol use, Parkinson´s disease, multiple sclerosis, and sleep disorder [70, 72].
Clinical implications
Since this was a cross-sectional designed exploratory study, no causal relationships could be established. We observed that eGFR was associated with markers of CSVD in the older hypertensive population. Hypertension is an important risk factor of CSVD, and CSVD is heavily linked to major disorders, such as dementia and stroke. The findings of this study emphasize the importance of assessment and management of hypertension in older individuals with CKD.
Strengths and weaknesses
Strengths of this study include representation of the general, older population, a relatively large sample size compared to other MRI studies, and use of the same experienced neuroradiologist to ensure consistency in the evaluation of the MRI images. Previous studies investigating inter-rater reliability regarding markers of CSVD on MRI, have found a high inter-rater reliability regarding assessment of WMHs, CMBs, and cortical atrophy according to Pasquier scale and the Koedam score [73,74,75,76], and a moderate to high inter-rater reliability regarding lacunar infarcts [77].
Another strength of this study includes the use of both crea and cysC to accurately estimate GFR using the reliable CKD-EPI formula, as well as the consideration taken to underweight participants, by estimating GFR only on cysC in this group to minimize bias.
We acknowledge that this study had limitations. An association between CKD and markers of CSVD was observed only in the hypertensive group in this study, and we cannot rule out hypertension as a potential confounder in this relationship. This was, however, an exploratory study. Further studies are warranted to further explore the relationship between CKD, CSVD, and hypertension.
Perivascular spaces and recent small subcortical infarcts are in many studies considered entities of CSVD. Recent small subcortical infarcts are included in the SVD score, and perivascular spaces are included in both the SVD score and in STRIVE [35, 36]. Perivascular spaces and small subcortical infarct were not measured, and therefore a modified version of the SVD score (composite CSVD) and a modified version of STRIVE (modified STRIVE) were created. This could limit the comparability of our findings with other studies.
Compared to those with normal kidney function, the group with CKD were slightly older, and they also had a greater burden of cardiovascular risk factors and events, such as hypertension, diabetes, smoking, coronary artery disease, and heart failure (see Table 2), which most likely contributed to the difference in CSVD burden between the groups.
The logistic regression models were adjusted for age and sex. The number of CSVD related outcomes in the group with CKD was relatively small (see Table 2), and therefore no adjustments for further potential covariates were performed. We acknowledge that the small prevalence of some of the lesions could have prevented us from observing associations between CSVD and CKD because of lack of power. This is especially true regarding lacunar infarcts, where only 10 cases were observed in the CKD group.
The vast majority of subjects in this study had an eGFR ≥ 60 ml/min/1.73m2(76%), representing normal kidney function (eGFR mean = 70.9 ml/min/1.73m2, eGFR median = 71.6 ml/min/1.73m2, eGFR 25 percentile = 60.6 ml/min/1.73m2, eGFR 75 percentile = 81.9 ml/min/1.73m2). The use of eGFR as a continuous variable could potentially have allowed the exploration of a dose-dependent relationship between eGFR and the severity of CSVD. However, since the vast majority of subjects in this study had normal kidney function, to avoid extrapolation, the variable representing kidney function was kept binary.
Another limitation of this study is that the blood samples were not taken at the MRI examination. To investigate this issue, we performed a sensitivity analysis to identify the CKD status at the next study visit after the MRI visit. The mean time from the MRI examination until the following blood sampling was 605 (SD 399) days. GFR was estimated in the same procedure as above. 212 (52,1%) out of the 407 participants who underwent MRI, continued attending visits in the GÅS study. Out of these 212 participants, 28 (13.2%) had missing GFR status in the following GÅS visit. The vast majority, 147 (69.3%) participants, remained stable in their group based on eGFR. 7 (3.3%) participants went from CKD to normal kidney function, and 30 (14.2%) went from normal kidney function to CKD. We do not know if CKD in these cases appeared before or after the MRI examination. Presumably, some of the participants who had been classified as having normal kidney function, could have had developed CKD before the MRI examination. Therefore, the observed associations between CKD and CSVD in this study could be underestimated.
Conclusions
We observed an association between CKD and markers of CSVD (CMBs and cortical atrophy) in the general older hypertensive population. In the general older non-hypertensive population, no associations between CKD and any markers of CSVD were observed. Our findings might indicate that hypertension is a link between CKD and CSVD. Further studies investigating the relationship between CKD, CSVD, and hypertension are warranted.
Data availability
All data in this study was based on the GÅS dataset. The GÅS dataset is restricted and not publicly available. The data can be obtained by the co-author and GÅS research leader professor Sölve Elmståhl by reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CKD-EPI:
-
Chronic kidney disease epidemiology collaboration
- CMBs:
-
Cerebral microbleeds
- CSVD:
-
Cerebral small vessel disease
- DBP:
-
Diastolic blood pressure
- DWI:
-
Diffusion-weighted images
- ED:
-
Endothelial dysfunction
- eGFR:
-
Estimated glomerular filtration rate
- IDMS:
-
Isotope-dilution mass spectrometry
- GCA:
-
Global cortical atrophy
- GFR:
-
Glomerular filtration rate
- GÅS:
-
Good aging in Skåne
- MRI:
-
Magnetic resonance imaging
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- SNAC:
-
Swedish national study on aging and care
- SPS:
-
Shrunken pore syndrome
- STRIVE:
-
Standards for reporting vascular changes on neuroimaging
- SVD:
-
Cerebral small vessel disease
- SWAN:
-
Susceptibility-weighted angiography
- T2 FLAIR:
-
T2-weighted fluid-attenuated inversion recovery
- WMHs:
-
White matter hyperintensities
References
Li Q, Yang Y, Reis C, Tao T, Li W, Li X, Zhang JH. Cerebral small Vessel Disease. Cell Transpl. 2018;27(12):1711–22.
Cannistraro RJ, Badi M, Eidelman BH, Dickson DW, Middlebrooks EH, Meschia JF. CNS small vessel disease: a clinical review. Neurology. 2019;92(24):1146–56.
Romero JR. Simple interventions: A Clue to Tackle Cerebral Small Vessel Disease. Stroke. 2022;53(9):2868–9.
Mu R, Qin X, Guo Z, Meng Z, Liu F, Zhuang Z, Zheng W, Li X, Yang P, Feng Y, et al. Prevalence and consequences of Cerebral Small Vessel diseases: a cross-sectional study based on Community people Plotted against 5-Year age strata. Neuropsychiatr Dis Treat. 2022;18:499–512.
Poels MM, Vernooij MW, Ikram MA, Hofman A, Krestin GP, van der Lugt A, Breteler MM. Prevalence and risk factors of cerebral microbleeds: an update of the Rotterdam scan study. Stroke. 2010;41(10 Suppl):103–6.
Nylander R, Fahlstrom M, Rostrup E, Kullberg J, Damangir S, Ahlstrom H, Lind L, Larsson EM. Quantitative and qualitative MRI evaluation of cerebral small vessel disease in an elderly population: a longitudinal study. Acta Radiol. 2018;59(5):612–8.
Zhang QL, Rothenbacher D. Prevalence of chronic kidney disease in population-based studies: systematic review. BMC Public Health. 2008;8:117.
Berger I, Wu S, Masson P, Kelly PJ, Duthie FA, Whiteley W, Parker D, Gillespie D, Webster AC. Cognition in chronic kidney disease: a systematic review and meta-analysis. BMC Med. 2016;14(1):206.
Mansson T, Overton M, Pihlsgard M, Elmstahl S. Impaired kidney function is associated with lower cognitive function in the elder general population. Results from the good aging in Skane (GAS) cohort study. BMC Geriatr. 2019;19(1):360.
Mansson T, Elmstahl S. Processing speed is affected by early impairment in kidney function in the general elder population. BMC Nephrol. 2021;22(1):314.
Dey AK, Stamenova V, Turner G, Black SE, Levine B. Pathoconnectomics of cognitive impairment in small vessel disease: a systematic review. Alzheimers Dement. 2016;12(7):831–45.
Sachdev PS, Blacker D, Blazer DG, Ganguli M, Jeste DV, Paulsen JS, Petersen RC. Classifying neurocognitive disorders: the DSM-5 approach. Nat Rev Neurol. 2014;10(11):634–42.
Lau WL, Huisa BN, Fisher M. The cerebrovascular-chronic kidney disease connection: perspectives and mechanisms. Transl Stroke Res. 2017;8(1):67–76.
O’Rourke MF, Safar ME. Relationship between aortic stiffening and microvascular disease in brain and kidney: cause and logic of therapy. Hypertension. 2005;46(1):200–4.
Jankowski J, Floege J, Fliser D, Bohm M, Marx N. Cardiovascular Disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation. 2021;143(11):1157–72.
Arinze NV, Gregory A, Francis JM, Farber A, Chitalia VC. Unique aspects of peripheral artery disease in patients with chronic kidney disease. Vasc Med. 2019;24(3):251–60.
Xiao C-Y, Ma Y-H, Ou Y-N, Zhao B, Hu H-Y, Wang Z-T, Tan L. Association between kidney function and the Burden of Cerebral Small Vessel Disease: an updated Meta-analysis and systematic review. Cerebrovasc Dis 2023:1–11.
Liu Y, Lv P, Jin H, Cui W, Niu C, Zhao M, Fan C, Teng Y, Pan B, Peng Q, et al. Association between low estimated glomerular filtration rate and risk of Cerebral Small-Vessel diseases: a Meta-analysis. J Stroke Cerebrovasc Dis. 2016;25(3):710–6.
Makin SD, Cook FA, Dennis MS, Wardlaw JM. Cerebral small vessel disease and renal function: systematic review and meta-analysis. Cerebrovasc Dis. 2015;39(1):39–52.
Vogels SC, Emmelot-Vonk MH, Verhaar HJ, Koek HL. The association of chronic kidney disease with brain lesions on MRI or CT: a systematic review. Maturitas. 2012;71(4):331–6.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, et al. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
Ekström H, Elmståhl S. Pain and fractures are independently related to lower walking speed and grip strength: results from the population study Good Ageing in Skåne / Pain and fractures are independently related to lower walking speed and grip strength: results from the population study good ageing in Skåne. Acta Orthop 2006(6):902.
Lagergren M, Fratiglioni L, Hallberg IR, Berglund J, Elmstahl S, Hagberg B, Holst G, Rennemark M, Sjolund BM, Thorslund M, et al. A longitudinal study integrating population, care and social services data. The Swedish National study on aging and care (SNAC). Aging Clin Exp Res. 2004;16(2):158–68.
Legrand H, Werner K, Christensson A, Pihlsgård M, Elmståhl S. Prevalence and determinants of differences in cystatin C and creatinine-based estimated glomerular filtration rate in community-dwelling older adults: a cross-sectional study. BMC Nephrol. 2017;18(1):350.
Kidney Disease. Improving global outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the evaluation and management of chronic kidney disease. Kidney inter Suppl. 2013;3:1–150.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Inker LA, Schmid CH, Tighiouart H, Eckfeldt JH, Feldman HI, Greene T, Kusek JW, Manzi J, Van Lente F, Zhang YL, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012;367(1):20–9.
Porter Starr KN, Bales CW. Excessive body weight in older adults. Clin Geriatr Med. 2015;31(3):311–26.
Nankivell BJ, Nankivell LFJ, Elder GJ, Gruenewald SM. How unmeasured muscle mass affects estimated GFR and diagnostic inaccuracy. EClinicalMedicine 2020, 29–30:100662.
Elmstahl S, Ellstrom K, Siennicki-Lantz A, Abul-Kasim K. Association between cerebral microbleeds and hypertension in the Swedish general population good aging in Skane study. J Clin Hypertens (Greenwich). 2019;21(8):1099–107.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149(2):351–6.
Offenbacher H, Fazekas F, Schmidt R, Koch M, Fazekas G, Kapeller P. MR of cerebral abnormalities concomitant with primary intracerebral hematomas. AJNR Am J Neuroradiol. 1996;17(3):573–8.
Pasquier F, Leys D, Weerts JG, Mounier-Vehier F, Barkhof F, Scheltens P. Inter- and intraobserver reproducibility of cerebral atrophy assessment on MRI scans with hemispheric infarcts. Eur Neurol. 1996;36(5):268–72.
Koedam EL, Lehmann M, van der Flier WM, Scheltens P, Pijnenburg YA, Fox N, Barkhof F, Wattjes MP. Visual assessment of posterior atrophy development of a MRI rating scale. Eur Radiol. 2011;21(12):2618–25.
Staals J, Makin SD, Doubal FN, Dennis MS, Wardlaw JM. Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology. 2014;83(14):1228–34.
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, Lindley RI, O’Brien JT, Barkhof F, Benavente OR, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12(8):822–38.
Kim SH, Shin DW, Yun JM, Lee JE, Lim JS, Cho BL, Kwon HM, Park JH. Kidney dysfunction and cerebral microbleeds in neurologically healthy adults. PLoS ONE. 2017;12(2):e0172210.
Shima H, Ishimura E, Naganuma T, Yamazaki T, Kobayashi I, Shidara K, Mori K, Takemoto Y, Shoji T, Inaba M, et al. Cerebral microbleeds in predialysis patients with chronic kidney disease. Nephrol Dial Transpl. 2010;25(5):1554–9.
van Overbeek EC, Staals J, van Oostenbrugge RJ. Decreased kidney function relates to progression of cerebral microbleeds in lacunar stroke patients. Int J Stroke. 2016;11(6):695–700.
McFadden EC, Hirst JA, Verbakel JY, McLellan JH, Hobbs FDR, Stevens RJ, O’Callaghan CA, Lasserson DS. Systematic review and metaanalysis comparing the Bias and Accuracy of the modification of Diet in Renal Disease and chronic kidney disease epidemiology collaboration equations in community-based populations. Clin Chem. 2018;64(3):475–85.
Akoudad S, Sedaghat S, Hofman A, Koudstaal PJ, van der Lugt A, Ikram MA, Vernooij MW. Kidney function and cerebral small vessel disease in the general population. Int J Stroke. 2015;10(4):603–8.
Sedaghat S, Ding J, Eiriksdottir G, van Buchem MA, Sigurdsson S, Ikram MA, Meirelles O, Gudnason V, Levey AS, Launer LJ. The AGES-Reykjavik Study suggests that change in kidney measures is associated with subclinical brain pathology in older community-dwelling persons. Kidney Int. 2018;94(3):608–15.
Jimenez-Balado J, Riba-Llena I, Pizarro J, Palasi A, Penalba A, Ramirez C, Maisterra O, Espinel E, Ramos N, Pujadas F, et al. Kidney function changes and their relation with the progression of cerebral small vessel disease and cognitive decline. J Neurol Sci. 2020;409:116635.
Yakushiji Y, Nanri Y, Hirotsu T, Nishihara M, Hara M, Nakajima J, Eriguchi M, Nishiyama M, Hara H, Node K. Marked cerebral atrophy is correlated with kidney dysfunction in nondisabled adults. Hypertens Res. 2010;33(12):1232–7.
Chang CY, Lin CC, Tsai CF, Yang WC, Wang SJ, Lin FH, Fuh JL. Cognitive impairment and hippocampal atrophy in chronic kidney disease. Acta Neurol Scand. 2017;136(5):477–85.
Ikram MA, Vernooij MW, Hofman A, Niessen WJ, van der Lugt A, Breteler MM. Kidney function is related to cerebral small vessel disease. Stroke. 2008;39(1):55–61.
Staplin N, Herrington WG, Murgia F, Ibrahim M, Bull KR, Judge PK, Ng SYA, Turner M, Zhu D, Emberson J, et al. Determining the relationship between blood pressure, kidney function, and chronic kidney disease: insights from genetic epidemiology. Hypertension. 2022;79(12):2671–81.
Newby D, Winchester L, Sproviero W, Fernandes M, Wang D, Kormilitzin A, Launer LJ, Nevado-Holgado AJ. Associations between Brain volumes and cognitive tests with hypertensive Burden in UK Biobank. J Alzheimers Dis. 2021;84(3):1373–89.
Petrea RE, O’Donnell A, Beiser AS, Habes M, Aparicio H, DeCarli C, Seshadri S, Romero JR. Mid to Late Life Hypertension trends and Cerebral Small Vessel Disease in the Framingham Heart Study. Hypertension. 2020;76(3):707–14.
Jimenez-Balado J, Riba-Llena I, Maisterra O, Pizarro J, Palasi A, Pujadas F, Mundet X, Vinyoles E, Delgado P. Ambulatory blood pressure levels in the prediction of progression of Cerebral Small Vessel Disease. J Am Geriatr Soc. 2020;68(10):2232–9.
Zhang D, Zhang J, Zhang B, Zhang J, He M. Association of blood pressure, White Matter lesions, and Regional Cerebral Blood Flow. Med Sci Monit. 2021;27:e929958.
Nobili F, Rodriguez G, Marenco S, De Carli F, Gambaro M, Castello C, Pontremoli R, Rosadini G. Regional cerebral blood flow in chronic hypertension. A correlative study. Stroke. 1993;24(8):1148–53.
Safar ME, Asmar R, Benetos A, Blacher J, Boutouyrie P, Lacolley P, Laurent S, London G, Pannier B, Protogerou A, et al. Interaction between Hypertension and arterial stiffness. Hypertension. 2018;72(4):796–805.
Zhai FF, Ye YC, Chen SY, Ding FM, Han F, Yang XL, Wang Q, Zhou LX, Ni J, Yao M, et al. Arterial stiffness and cerebral small Vessel Disease. Front Neurol. 2018;9:723.
Ellstrom K, Abul-Kasim K, Siennicki-Lantz A, Elmstahl S. Associations of carotid artery flow parameters with MRI markers of cerebral small vessel disease and patterns of brain atrophy. J Stroke Cerebrovasc Dis. 2023;32(3):106981.
Safar ME, London GM, Plante GE. Arterial stiffness and kidney function. Hypertension. 2004;43(2):163–8.
Vanhoutte PM, Shimokawa H, Tang EH, Feletou M. Endothelial dysfunction and vascular disease. Acta Physiol (Oxf). 2009;196(2):193–222.
Roumeliotis S, Mallamaci F, Zoccali C. Endothelial dysfunction in chronic kidney Disease, from Biology to Clinical outcomes: a 2020 Update. J Clin Med 2020, 9(8).
Bai T, Yu S, Feng J. Advances in the role of endothelial cells in Cerebral Small Vessel Disease. Front Neurol. 2022;13:861714.
Setiadi A, Korim WS, Elsaafien K, Yao ST. The role of the blood-brain barrier in hypertension. Exp Physiol. 2018;103(3):337–42.
Arnold R, Issar T, Krishnan AV, Pussell BA. Neurological complications in chronic kidney disease. JRSM Cardiovasc Dis. 2016;5:2048004016677687.
Lau WL, Nunes ACF, Vasilevko V, Floriolli D, Lertpanit L, Savoj J, Bangash M, Yao Z, Shah K, Naqvi S, et al. Chronic kidney Disease increases cerebral microbleeds in Mouse and Man. Transl Stroke Res. 2020;11(1):122–34.
Seliger SL, Salimi S, Pierre V, Giffuni J, Katzel L, Parsa A. Microvascular endothelial dysfunction is associated with albuminuria and CKD in older adults. BMC Nephrol. 2016;17(1):82.
Zou LX, Sun L, Nicholas SB, Lu Y, K SS, Hua R. Comparison of bias and accuracy using cystatin C and creatinine in CKD-EPI equations for GFR estimation. Eur J Intern Med. 2020;80:29–34.
Legrand H, Werner K, Christensson A, Pihlsgard M, Elmstahl S. Prevalence and determinants of differences in cystatin C and creatinine-based estimated glomerular filtration rate in community-dwelling older adults: a cross-sectional study. BMC Nephrol. 2017;18(1):350.
Hao R, Guo H. Anorexia, undernutrition, weight loss, Sarcopenia, and cachexia of aging. Eur Rev Aging Phys Activity. 2012;9(2):119–27.
Kanhai DA, de Kappelle KDF. LJ, Kappelle Lj Fau - Uiterwaal CSPM, Uiterwaal Cs Fau - van der Graaf Y, van der Graaf Y Fau - Pasterkamp G, Pasterkamp G Fau - Geerlings MI, Geerlings Mi Fau - Visseren FLJ, Visseren FL: Extracellular vesicle protein levels are related to brain atrophy and cerebral white matter lesions in patients with manifest vascular disease: the SMART-MR study. (2044–6055 (Print)).
Grubb A, Lindstrom V, Jonsson M, Back SE, Ahlund T, Rippe B, Christensson A. Reduction in glomerular pore size is not restricted to pregnant women. Evidence for a new syndrome: ‘Shrunken pore syndrome’. Scand J Clin Lab Invest. 2015;75(4):333–40.
Almen MS, Bjork J, Nyman U, Lindstrom V, Jonsson M, Abrahamson M, Vestergren AS, Lindhe O, Franklin G, Christensson A, et al. Shrunken pore syndrome is Associated with increased levels of atherosclerosis-promoting proteins. Kidney Int Rep. 2019;4(1):67–79.
Zhao L, Lee A, Fan YH, Mok VCT, Shi L. Magnetic resonance imaging manifestations of cerebral small vessel disease: automated quantification and clinical application. Chin Med J (Engl). 2020;134(2):151–60.
Nitkunan A, Lanfranconi S, Charlton RA, Barrick TR, Markus HS. Brain atrophy and cerebral small vessel disease: a prospective follow-up study. Stroke. 2011;42(1):133–8.
Litak J, Mazurek M, Kulesza B, Szmygin P, Litak J, Kamieniak P, Grochowski C. Cerebral Small Vessel Disease. Int J Mol Sci 2020, 21(24).
Li X, Yuan J, Qin W, Yang L, Yang S, Li Y, Hu W. Higher total cerebral small Vessel Disease Burden was Associated with mild cognitive impairment and overall cognitive dysfunction: a propensity score-matched case-control study. Front Aging Neurosci. 2021;13:695732.
Fan Y, Xu Y, Shen M, Guo H, Zhang Z. Total cerebral small Vessel Disease Burden on MRI correlates with cognitive impairment in outpatients with Amnestic disorders. Front Neurol. 2021;12:747115.
Goldstein ED, Badi MK, Hasan TF, Lesser ER, Hodge DO, Lin MP, Meschia JF. Cerebral small Vessel Disease Burden and all-cause mortality: Mayo Clinic Florida familial cerebrovascular diseases Registry. J Stroke Cerebrovasc Dis. 2019;28(12):104285.
Rhodius-Meester HFM, Benedictus MR, Wattjes MP, Barkhof F, Scheltens P, Muller M, van der Flier WM. MRI visual ratings of Brain Atrophy and White Matter hyperintensities across the Spectrum of Cognitive decline are differently affected by age and diagnosis. Front Aging Neurosci. 2017;9:117.
Roob G, Schmidt R, Kapeller P, Lechner A, Hartung HP, Fazekas F. MRI evidence of past cerebral microbleeds in a healthy elderly population. Neurology. 1999;52(5):991–4.
Acknowledgements
The authors are grateful to all participants and all staff members in the GÅS project. A special acknowledgement to Ole Larsen for management of data from the GÅS study.
Funding
The project Good Aging in Skåne, part of the Swedish National Study on Aging and Care (www.snac.org) was supported by the Swedish Ministry of Health and Social Affairs, the County of Region Skåne and the Swedish Research Council under grant no. 2017 − 01613; 521-2013-8604.
Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
The study design was set up by TM, AR and SE. KA-K examined and interpretated the MRI images. TM performed the statistical analyses. The manuscript was drafted by TM. AR, KE, SE and KA-K revised the manuscript critically. All authors contributed to the intellectual discussion and gave approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The GÅS study is conducted in accordance with the Declaration of The Code of Ethics of the World Medical Association (Declaration of Helsinki). The study was approved by the Regional Ethics Review Board, Lund University (2015/859). All participants received written information. Informed consent for participation in the study was obtained from either the participants or, when necessary, from relatives.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Månsson, T., Rosso, A., Ellström, K. et al. Chronic kidney disease and its association with cerebral small vessel disease in the general older hypertensive population. BMC Nephrol 25, 93 (2024). https://doi.org/10.1186/s12882-024-03528-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-024-03528-8