Abstract
Background
Hereditary renal hypouricemia (RHUC) is a heterogenous disorder characterized by defective uric acid (UA) reabsorption resulting in hypouricemia and increased fractional excretion of UA. RHUC is an important cause of exercise-induced acute kidney injury (EIAKI), nephrolithiasis and posterior reversible encephalopathy syndrome (PRES). We present here an unusual case of a patient with RHUC who presented with recurrent EIAKI and had two heterozygous mutations in the SLC2A9 gene.
Case presentation
A 43-year old man was admitted to our clinic because of bilateral loin pain, nausea and sleeplessness for 3 days after strenuous exercise. The laboratory results revealed increased levels of blood urea nitrogen (BUN) (15 mmol/l) and serum creatinine (Scr) (450 μmol/l), while the UA level was extremely low at 0.54 mg/dl, and his fractional excretion of urate (FE-UA) was 108%. The patient had an episode of acute kidney injury after playing soccer approximately 20 years ago, and on routine physical examination, his UA was less than 0.50 mg/dl. In view of the marked hypouricemia and high FE-UA, a diagnosis of RHUC was suspected, which led us to perform mutational screening of the SLC22A12 and SLC2A9 genes. DNA sequencing revealed no mutation in SLC22A12 gene, but two heterozygous mutations in the SLC2A9 gene.
Conclusions
This is a rare report of a patient with RHUC2 due to the mutation of SLC2A9. And this unique symptom of EIAKI and decreased or normal serum concentrations of UA warrant more attention as an early cue of RHUC.
Similar content being viewed by others
Background
RHUC is a rare hereditary disease caused by impaired urate transport: reduced urate reabsorption and/or increased secretion [1, 2]. The incidence of renal hypouricemia has been reported to be 0.15% to 0.72% [3]. Two types of RHUC have been described. RHUC1 is caused by mutations in the SLC22A12 gene(OMIN #220,150), while RHUC2 is caused by mutations in the SLC2A9 gene(OMIN #612,076). More than 150 RHUC patients with mutations in the SLC22A12 gene have been described all over the world, with the majority belonging to the Asian population. The highest reported frequencies far have been 2.30–2.37% in Japan and 0.4% in Korea, with the specific mutation sites identified as c.774G > A (p.W258X) and c.269G > A (p.R90H), respectively. However, RHUC1 patients have also been documented in other ethnic groups, including Arab, Iraqi Jews, Caucasians, and Roma, as well as in geographically non-contiguous countries. Notably, the c.1245_1253del and c.1400C > T variants have unexpectedly high prevalence of 1.92% and 5.56%, respectively, among the Roma population in five regions spanning the Czech Republic, Slovakia, and Spain. These findings highlight the uneven geographical and ethnic distribution of SLC22A12 mutations, necessitating consideration in non-Asian patients [4, 5]. Whereas only approximately 20 cases of RHUC2 have been reported worldwide [6,7,8]. Patient ethnicity is diverse and includes Japanese, Chinese, Ashkenazi-Jewish, Anglo-Saxon, Greek, and Czech; to date, only few Caucasian families with a SLC2A9 mutation have been reported [9]. RHUC2 exhibits a broader clinical variability compared to RHUC1 [10]: UA levels observed in heterozygous patients with SLC2A9 mutations are similar to those with compound heterozygous and/or homozygous SLC22A12 mutations. However, compound heterozygous and/or homozygous RHUC2 patients have significantly lower serum UA levels, approaching zero, and markedly higher renal excretion, exceeding 100% [2, 11]. On the other hand, heterozygous RHUC2 family relatives exhibit normal levels of UA [12, 13].
Here we report an unusual case of a patient with RHUC2 who presented with recurrent EIAKI and had two heterozygous mutations in the SLC2A9 gene.
Case presentation
A 43‐year‐old man was admitted because of bilateral loin pain, nausea and sleeplessness for 3 days after strenuous exercise, but without oliguria, hematuria or myalgia. There was no history of nephrolithiasis, and family history was unremarkable. He took regular antihypertensive drug amlodipine. He had no smoking history and wasn’t exposed to known chemicals or solvents. On admission, his blood pressure was 167/103 mmHg. The other physical examination was unremarkable.
The laboratory results revealed increased levels of BUN (15 mmol/l) and Scr (450 μmol/l), while the UA level was extremely low at 32 μmol/l(0.54 mg/dl) (normal range 3.50–8.50 mg/dl). His creatine kinase (CK), lactate dehydrogenase (LDH) and complete blood count were all normal. 24-h urinary protein was 0.39 g (normal range < 150 mg), urinary protein/creatinine ratio was 417 mg/g (normal range < 200 mg/g), urinary albumin/creatinine ratio was 260 mg/g (normal range < 30 mg/g), urine β2 microglobulin was 0.57 mg/l (normal range < 0.2 mg/l). The patient’s FE-UA was 108%. Urinalysis showed no glucose, red blood cells or casts. Serologic parameters were all within normal range, including complement, antinuclear antibody (ANA), double-stranded DNA (dsDNA), antineutrophil cytoplasmic antibody (ANCA), anti-glomerular basement membrane (GBM) antibodies, and hepatitis B and C antibody. His renal ultrasound showed normal-size kidneys with no evidence of obstruction (right:125*65 mm, left:115*65 mm).
Within one week, his renal function started to recover spontaneously, and urinalysis showed no protein. Based on the above results, no kidney biopsy was performed.
The patient recalled that he had an episode of acute kidney injury after playing soccer approximately 20 years ago. At that time, his Scr was up to 900 μmol/l, and returned to normal range within one month without dialysis.
On a previous admission, his Scr was 65 μmol/l, BUN was 5 mmol/l, UA was less than 30 μmol/l(0.50 mg/dl).
None of his family members had hypouricemia during routine biochemistry examination (including his parents and his sister).
In view of the marked hypouricemia and high FE-UA, a diagnosis of RHUC was suspected, which led us to perform mutational screening of the SLC22A12 and SLC2A9 genes. However, only the patient but not other family members received the genetic test per the patient’s and his sister’s request.
DNA sequencing revealed no mutation in SCL22A22 gene, but two heterozygous mutations in the SLC2A9 gene.
Copy number variation(CNV) analysis of the next generation sequencing(NGS) data suggested a deletion of exon 4 and 5 in the SLC2A9 gene. A length of 146 bp heterozygous deletion (chr4:9,982,216–9,982,361) in exon 5 of the SLC2A9 gene was verified by qPCR-SYBR Green I method. Moreover, there was a heterozygous nonsense mutation (c.944G > A, pTrp315Stop) that introduced a premature “stop” codon located in exon 7 of the SLC2A9 gene (Fig. 1). These mutations have not been reported previously.
DNA sequencing for the mutations. The patient carried two heterogeneous mutations in SLC2A9 gene. a. CNV analysis suggested a deletion of exon 4 and 5 in the SLC2A9 gene. b. A length of 146 bp heterozygous deletion (chr4:9,982,216–9,982,361) in exon 5 of the SLC2A9 gene was verified by qPCR-SYBR Green I method. c.A heterozygous nonsense mutation (c.944G > A, pTrp315Stop) in exon 7
Two months after his discharge from the hospital, his renal function was improved remarkably (Scr recovered to 75 μmol/l), suggesting recovery of the kidneys from AKI (Fig. 2).
Discussion and conclusion
There are two types of RHUC. RHUC1 is caused by mutations in the gene SLC22A12 that encodes a renal urate-anion exchanger named urate transporter 1(URAT1) [1, 14]. URAT1 is the first identified renal urate-anion transporter, which is mainly expressed in the apical side of the proximal tubule, and is responsible for a large portion of proximal urate reabsorption [1]. RHUC2 is caused by mutations in the SLC2A9 gene, which encodes a high-capacity glucose and urate transporter, named glucose transporter 9 (GLUT9) [15]. GLUT9 is expressed in human kidney proximal tubule epithelial cells. Two GLUT9 variants have been identified: the GLUT9S and GLUT9L [2, 8, 15, 16]. GLUT9L is localized to the basolateral side and GLUT9S to the apical side [17]. The GLUT9L has been suggested to be the only transporter that mediates the efflux of the urate from the cells across the basolateral membrane [11]. Whereas urate absorption from the tubular lumen into the cells is mediated by URAT1, GLUT9S and possibly other apical transporters [18].
Patients with homozygous mutations in SLC22A12 typically have serum UA concentrations below 59.5 μmol/l(1.0 mg/dl) and a partial urate reabsorption defect with FE-UA between 40 and 90%. In contrast, the loss of function mutations in SLC2A9 precludes all urate from exiting the cells from basal lateral membrane, thus completely blocking urate absorption. The net effect is that the value of FE-UA is greater than 100%, the values above 100% reflecting urate secretion. So loss-of-function mutations in SLC2A9 cause more severe hypouricemia and render patients more vulnerable for complications, such as nephrolithiasis, EIAKI and PRES [9].
Nephrolithiasis and EIAKI are reported to have a prevalence of 8.5% and 6.5% in patients with RHUC based on mutational screening [11, 19]. PRES was only described in 3 patients with EIAKI due to RHUC till now [20,21,22]. Acute kidney disease associated with renal hypouricemia was first described in 1989 by Erley et al. [23].The relative risk was assessed in a study of 13 patients presenting with AKI following exercise, three of whom (23%) had RHUC [24]. A retrospective investigation described 54 patients’ clinical features of EIAKI associated with RHUC. The study revealed that the majority of patients were males, with a male: female ratio of 8:1. During follow-up, 13 patients (24%) developed recurrent AKI [25].
There is a difference in the occurrence rate of AKI between RHUC1 and RHUC2. In RHUC1, the loss of URAT1 function results in partial UA absorption defect. In RHUC2, the heterozygous GLUT9 mutation causes hypouricemia due to haploinsufficiency rather than a dominant negative effect. Homozygous GLUT9 mutations lead to severe hypouricemia through loss-of-function mutations and completely block the efflux of UA, preventing its absorption by all apical transporters, including URAT1. Therefore, reports indicate that heterozygous RHUC2 patients exhibit UA levels similar to those with URAT1 mutations, while homozygous and/or compound heterozygous patients have lower serum UA levels (close to 0 mg/dL) and higher FE-UA (> 100%), compared with 13% in those with heterozygous GLUT9 mutations and 40 to 90% in patients with homozygous loss of URAT1 [6, 11] (Table 1).
When AKI occurs in patients with RHUC after strenuous exercise, the initial symptoms are often abdominal pain and nausea/vomiting, usually occurring within 6–12 h after exercise. In addition, during the onset of AKI, the blood UA level may be close to normal due to kidney dysfunction, so it may not attract enough attention of clinicians. The prevention of AKI in RHUC includes avoiding strenuous exercise and ensuring sufficient fluid intake after exercise. Supportive treatment is important after AKI attack. The prognosis of RHUC-associated AKI is benign, only a few patients required hemodialysis, while recurrent AKI may lead to chronic kidney disease (CKD) in some patients [25, 26]. Therefore, early recognition and treatment are important to improve the renal outcome.
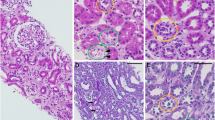
The mechanism by which RHUC causes EIAKI remains controversial. Firstly, oxidative stress from reactive oxygen species generated during exercise leads to renal vasoconstriction, ischemia, oxidant injury [27], resulting in reduced glomerular filtration rate and ATN; However, there were no differences observed in oxidative stress markers between RHUC patients and healthy participants before and after exercise [28]. Secondly, during exercise, increased UA production leads to UA excretion stress and precipitation in the tubules, as occurs in tumor lysis syndrome or UA nephropathy. Although Erley's description confirms the histological correlation between uric acid nephropathy and acute renal failure, further reports have not substantiated this finding. In fact, most kidney biopsies reveal acute tubular injury without intratubular UA deposition [23, 25, 29] (Table 2).Thirdly, a study analyzed the purine metabolism in RHUC patients and found that, compared to healthy participants, RHUC patients exhibited a rapid decrease in blood xanthine concentration and a significant increase in urinary xanthine concentration after exercise. The decrease in blood xanthine, which serves as a salvage pathway substrate, can reduce ATP resynthesis, resulting in the loss of renal tubular ATP and EIAKI [28]. Fourthly, reduced clearance of urate-coupled anions as a result of loss-of-function mutations of either URAT1 or GLUT9 may exert toxic effects on renal proximal tubules, leading to toxic ATN [11]. Furthermore, in patients with EIAKI, it was observed through CT scans performed after the administration of iv contrast agents that there were patchy, wedge-shaped, and high-density areas in both kidneys due to delayed excretion of the contrast agent. This phenomenon may be attributed to transient renal segmental ischemia caused by renal vascular spasm. These findings suggest that renal vascular spasm during exercise may lead to a similar ischemia–reperfusion-like kidney injury following physical activity [24, 30].
SLC2A9 was first identified as a novel member of the facilitative glucose transporter family in 2000 by Phay et al. [33]. In 2008, Matsuo et al. [8] identified two loss-of-function heterozygous mutations in SLC2A9 that caused RHUC by decreased urate reabsorption on both apical and basolateral sides of the proximal renal tubules. To date, 18 patients with EIAKI caused by SLC2A9 mutation have been reported, most of them have homozygous or compound heterozygous mutations (72.2%, 13/18 and 22.2%, 4/18, respectively) (Table 3).
Patients should be advised to avoid strenuous exercise and ensure an adequate intake of fluids after physical activity. On another note, a study involving five participants who took 300 mg of allopurinol daily for five consecutive days and underwent physical fitness testing (PFT) revealed that allopurinol could prevent EIAKI and exercise-induced UA excretion [41]. Furthermore, Frank et al. [42] and Sasaki et al. [43] successfully treated three patients with UA kidney stones and renal hypouricemia using allopurinol, resulting in stone dissolution and preventing further stone formation.
In the present case, the patient was shown to carry two heterozygous mutations in the GLUT9 gene, including a length of 146 bp CNV (chr4:9,982,216–9,982,361) in exon 5 and c.944G > A (p.Trp315Stop) nonsense mutation in exon 7. Although these mutations have not been reported in previous genetic studies on RHUC, they are very likely the cause that leads to the deficiency in urate reabsorption in our patients. CNV is a form of structural variation, corresponding to relatively large regions of the genome that have been deleted or duplicated on certain chromosomes. For example, in this case, 146 bp heterozygous deletion variations were found in exon 5 in the GLUT9 gene. Moreover, DNA sequencing of SLC2A9 identified a novel heterozygous nonsense mutation, c.944G > A in exon 7 (p.Trp315Stop), which may result in prematurely truncated GLUT9 protein in the patient. If combined these heterozygous mutations with the patient’s clinical feature, it overwhelmingly likely led to the malfunction of the GLUT9 protein. Because other family members were unavailable for the genetic study, we couldn’t get a conclusion that these heterozygous mutations were compound heterozygous mutations. Because this patient’s parents and sister do not have clinical hypouricemia, according to the autosomal recessive mode of inheritance, we speculated that this patient had a compound heterozygous mutation in the GLUT9 gene. These mutations have not been published to date.
A limitation of this case is the lack of the genetic test results from his family members.
This is a report of a patient with RHUC2 due to the mutation of SLC2A9, which encodes GLUT9. In clinical practice, the diagnosis of RHUC should be considered in patients manifesting symptoms of recurrent AKI and decreased or normal serum concentrations of UA, particularly after strenuous exercise.
Availability of data and materials
All data collected from this patient were obtained from Huashan Hospital and are available in this paper.
Abbreviations
- RHUC:
-
Hereditary renal hypouricemia
- UA:
-
Uric acid
- EIAKI:
-
Exercise-induced acute kidney injury
- PRES:
-
Posterior reversible encephalopathy syndrome
- BUN:
-
Blood urea nitrogen
- Scr:
-
Serum creatinine
- FE-UA:
-
Fractional excretion of urate
- CK:
-
Creatine kinase
- LDH:
-
Lactate dehydrogenase
- ANA:
-
Antinuclear antibody
- dsDNA:
-
Double-stranded DNA
- ANCA:
-
Antineutrophil cytoplasmic antibody
- GBM:
-
Glomerular basement membrane
- URAT1:
-
Urate transporter 1
- GLUT9:
-
Glucose transporter 9
- PFT:
-
Physical fitness testing
References
A E, H K, Chairoungdua A, Shigeta Y, Jutabha P, Cha SH, et al. Molecular identification of a renal urate anion exchanger that regulates blood urate levels. Nature. 2002;417(6887):447–447.
Stiburkova B, Taylor J, Marinaki AM, Sebesta I. Acute kidney injury in two children caused by renal hypouricaemia type 2. Pediatr Nephrol. 2012;27(8):1411–5.
Hisatome I, Ogino K, Kotake H, Ishiko R, Saito M, Hasegawa J, Mashiba H, Nakamoto S. Cause of persistent hypouricemia in outpatients. Nephron. 1989;51(1):13–6.
Stiburkova B, Gabrikova D, Cepek P, Simek P, Kristian P, Cordoba-Lanus E, et al. Prevalence of URAT1 allelic variants in the Roma population. Nucleosides Nucleotides Nucleic Acids. 2016;35(10–12):529–35.
Stiburkova B, Bohata J, Pavelcova K, Tasic V, Plaseska-Karanfilska D, Cho SK, et al. Renal hypouricemia 1: rare disorder as common disease in Eastern Slovakia Roma population. Biomedicines. 2021;9(11):1607.
Jeannin G, Chiarelli N, Gaggiotti M, Ritelli M, Maiorca P, Quinzani S, Verzeletti F, Possenti S, Colombi M, Cancarini G. Recurrent exercise-induced acute renal failure in a young Pakistani man with severe renal hypouricemia and SLC2A9 compound heterozygosity. BMC Med Genet. 2014;15:3.
Zhou Z, Ma L, Zhou J, Song Z, Zhang J, Wang K, et al. Renal hypouricemia caused by novel compound heterozygous mutations in the SLC22A12 gene: a case report with literature review. BMC Med Genet. 2018;19(1):142.
Matsuo H, Chiba T, Nagamori S, Nakayama A, Domoto H, Phetdee K, et al. Mutations in glucose transporter 9 gene SLC2A9 cause renal hypouricemia. Am J Hum Genet. 2008;83(6):744–51.
Windpessl M, Ritelli M, Wallner M, Colombi M. A Novel Homozygous SLC2A9 Mutation Associated with Renal-Induced Hypouricemia. Am J Nephrol. 2016;43(4):245–50.
Mancikova A, Krylov V, Hurba O, Sebesta I, Nakamura M, Ichida K, et al. Functional analysis of novel allelic variants in URAT1 and GLUT9 causing renal hypouricemia type 1 and 2. Clin Exp Nephrol. 2016;20(4):578–84.
Dinour D, Gray NK, Campbell S, Shu X, Sawyer L, Richardson W, et al. Homozygous SLC2A9 mutations cause severe renal hypouricemia. J Am Soc Nephrol. 2010;21(1):64–72.
Stiburkova B, Ichida K, Sebesta I. Novel homozygous insertion in SLC2A9 gene caused renal hypouricemia. Mol Genet Metab. 2011;102(4):430–5.
Toyoda Y, Cho SK, Tasic V, Pavelcova K, Bohata J, Suzuki H, et al. Identification of a dysfunctional exon-skipping splice variant in GLUT9/SLC2A9 causal for renal hypouricemia type 2. Front Genet. 2022;13:1048330.
Ichida K, Hosoyamada M, Hisatome I, Enomoto A, Hikita M, Endou H, et al. Clinical and molecular analysis of patients with renal hypouricemia in Japan-influence of URAT1 gene on urinary urate excretion. J Am Soc Nephrol. 2004;15(1):164–73.
Vitart V, Rudan I, Hayward C, Gray NK, Floyd J, Palmer CN, et al. SLC2A9 is a newly identified urate transporter influencing serum urate concentration, urate excretion and gout. Nat Genet. 2008;40(4):437–42.
Caulfield MJ, Munroe PB, O’Neill D, Witkowska K, Charchar FJ, Doblado M, et al. SLC2A9 is a high-capacity urate transporter in humans. PLoS Med. 2008;5(10):e197.
Augustin R, Carayannopoulos MO, Dowd LO, Phay JE, Moley JF, Moley KH. Identification and characterization of human glucose transporter-like protein-9 (GLUT9): alternative splicing alters trafficking. J Biol Chem. 2004;279(16):16229–36.
Dinour D, Gray NK, Ganon L, Knox AJ, Shalev H, Sela BA, et al. Two novel homozygous SLC2A9 mutations cause renal hypouricemia type 2. Nephrol Dial Transplant. 2012;27(3):1035–41.
Park JH, Jo YI, Lee JH. Renal effects of uric acid: hyperuricemia and hypouricemia. Korean J Intern Med. 2020;35(6):1291–304.
Fujinaga S, Ito A, Nakagawa M, Watanabe T, Ohtomo Y, Shimizu T. Posterior reversible encephalopathy syndrome with exercise-induced acute kidney injury in renal hypouricemia type 1. Eur J Pediatr. 2013;172(11):1557–60.
Shima Y, Nozu K, Nozu Y, Togawa H, Kaito H, Matsuo M, et al. Recurrent EIARF and PRES with severe renal hypouricemia by compound heterozygous SLC2A9 mutation. Pediatrics. 2011;127(6):e1621–5.
Mou LJ, Jiang LP, Hu Y. A novel homozygous GLUT9 mutation cause recurrent exercise-induced acute renal failure and posterior reversible encephalopathy syndrome. J Nephrol. 2015;28(3):387–92.
Erley CM, Hirschberg RR, Hoefer W, Schaefer K. Acute renal failure due to uric acid nephropathy in a patient with renal hypouricemia. Klin Wochenschr. 1989;67(5):308–12.
Ishikawa I, Sakurai Y, Masuzaki S, Sugishita N, Shinoda A, Shikura N. Exercise-induced acute renal failure in 3 patients with renal hypouricemia. Nihon Jinzo Gakkai Shi. 1990;32(8):923–8.
Ohta T, Sakano T, Igarashi T, Itami N, Ogawa T, Group ARFAwRHR. Exercise-induced acute renal failure associated with renal hypouricaemia: results of a questionnaire-based survey in Japan. Nephrol Dial Transplant. 2004;19(6):1447–53.
Coca SG, Singanamala S, Parikh CR. Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int. 2012;81(5):442–8.
Paller MS, Hoidal JR, Ferris TF. Oxygen free radicals in ischemic acute renal failure in the rat. J Clin Invest. 1984;74(4):1156–64.
Miyamoto D, Sato N, Nagata K, Sakai Y, Sugihara H, Ohashi Y, et al. Analysis of purine metabolism to elucidate the pathogenesis of acute kidney injury in renal hypouricemia. Biomedicines. 2022;10(7):1584.
Ohta T, Sakano T, Ogawa T, Kato J, Awaya Y, Kihara H, Kinoshita Y. Exercise-induced acute renal failure with renal hypouricemia: a case report and a review of the literature. Clin Nephrol. 2002;58(4):313–6.
Tadokoro T, Tamura Y, Mohri M. Exercise-induced acute kidney injury. QJM. 2022;115(1):47–8.
Numabe A, Tsukada H, Sugimoto T, Ono H, Hirao S, Abe M, Yagi S. A case of acute renal failure in a patient with idiopathic hypouricemia. Nihon Jinzo Gakkai Shi. 1992;34(7):841–5 Japanese.
Wang C, Wang J, Liu S, Liang X, Song Y, Feng L, et al. Idiopathic renal hypouricemia: A case report and literature review. Mol Med Rep. 2019;20(6):5118–24.
Phay JE, Hussain HB, Moley JF. Cloning and expression analysis of a novel member of the facilitative glucose transporter family, SLC2A9 (GLUT9). Genomics. 2000;66(2):217–20.
Shen H, Feng C, Jin X, Mao J, Fu H, Gu W, et al. Recurrent exercise-induced acute kidney injury by idiopathic renal hypouricemia with a novel mutation in the SLC2A9 gene and literature review. BMC Pediatr. 2014;14:73.
Androvitsanea A, Stylianou K, Maragkaki E, Tzanakakis M, Stratakis S, Petrakis I, et al. Vanishing urate, acute kidney injury episodes and a homozygous SLC2A9 mutation. Int Urol Nephrol. 2015;47(6):1035–6.
Zhou Y, Zhou YC, Liu ZH, Wu Y. Hypouricemia and exercise-induced acute kidney injury. J Nephrol Dialy Transplant. 2016;25(06):579–83.
Claverie-Martin F, Trujillo-Suarez J, Gonzalez-Acosta H, Aparicio C, Justa Roldan ML, Stiburkova B, et al. URAT1 and GLUT9 mutations in Spanish patients with renal hypouricemia. Clin Chim Acta. 2018;481:83–9.
Wang C, Li HX, Ding JJ, Qi C, Zhu GH, Liao PL, Huang L, Wang XW. A pedigree report of renal hypouricemia caused by SLC2A9 mutation and literature review. J Clin Nephrol. 2021;21(10):877–81.
Maalouli C, Dahan K, Devresse A, Gillion V. Mutation in the SLC2A9 Gene: A New Family with Familial Renal Hypouricemia Type 2. Case Rep Nephrol. 2021;2021:4751099.
Kaynar K, Güvercin B, Şahin M, Turan N, Açíkyürek F. A novel mutation in a patient with familial renal hypouricemia type 2. Nefrologia (Engl Ed). 2022;42(3):347–50.
Yeun JY, Hasbargen JA. Renal hypouricemia: prevention of exercise-induced acute renal failure and a review of the literature. Am J Kidney Dis. 1995;25(6):937–46.
Frank M, Many M, Sperling O. Familial renal hypouricaemia: two additional cases with uric acid lithiasis. Br J Urol. 1979;51(2):88–91.
Sasaki M, Takenawa J, Kanamaru H. A case of idiopathic hypouricemia due to augmented renal tubular secretion of uric acid. Nihon Hinyokika Gakkai Zasshi. 1986;77(8):1349–52.
Acknowledgements
All authors thank the patient and his family for their support.
Funding
Chuangming Hao was supported by the National Natural Science Foundation of China project (grant numbers 81930120 and 82370689).
Author information
Authors and Affiliations
Contributions
JZ, MZ, QHX, NXX, MXL, MZ, CMH were all directly involved in the care of this patient. JZ and MZ collected the data necessary for analysis and wrote the initial draft of the paper. QHX, NXX, MXL and MZ contributed to the data analysis and interpretation. CMH was responsible for revising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
The patient received all information regarding this case report. Written informed consent for publication in BMC Nephrology was obtained from the patient. A copy of the consent form is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, J., Zhang, M., Xie, Q. et al. Recurrent exercise-induced acute kidney injury associated with hypouricemia: a case report and literature review. BMC Nephrol 24, 384 (2023). https://doi.org/10.1186/s12882-023-03378-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-023-03378-w